How Psychosocial Safety Climate Helped Alleviate Work Intensification Effects on Presenteeism during the COVID-19 Crisis? A Moderated Mediation Model
Abstract
1. Introduction
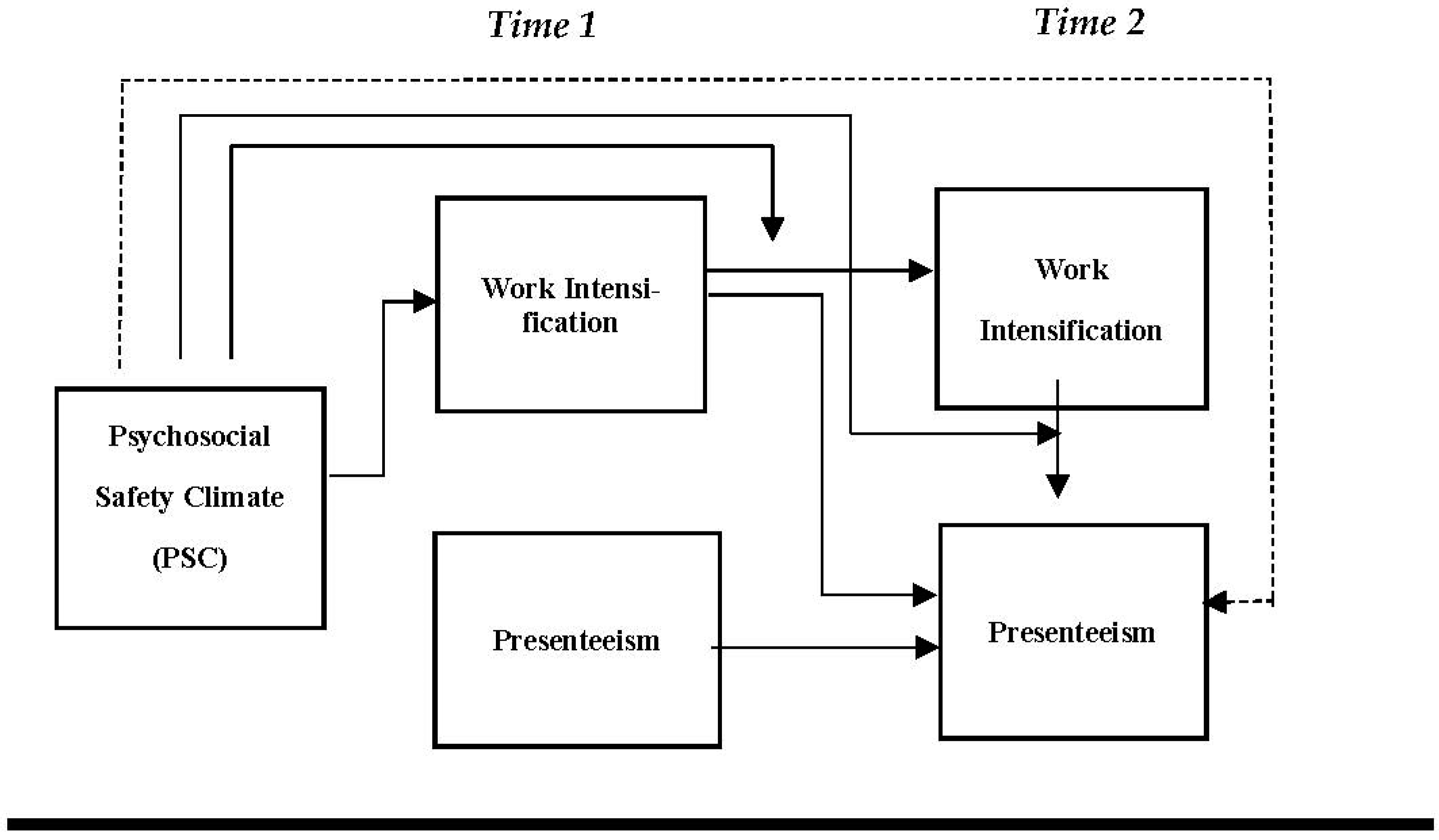
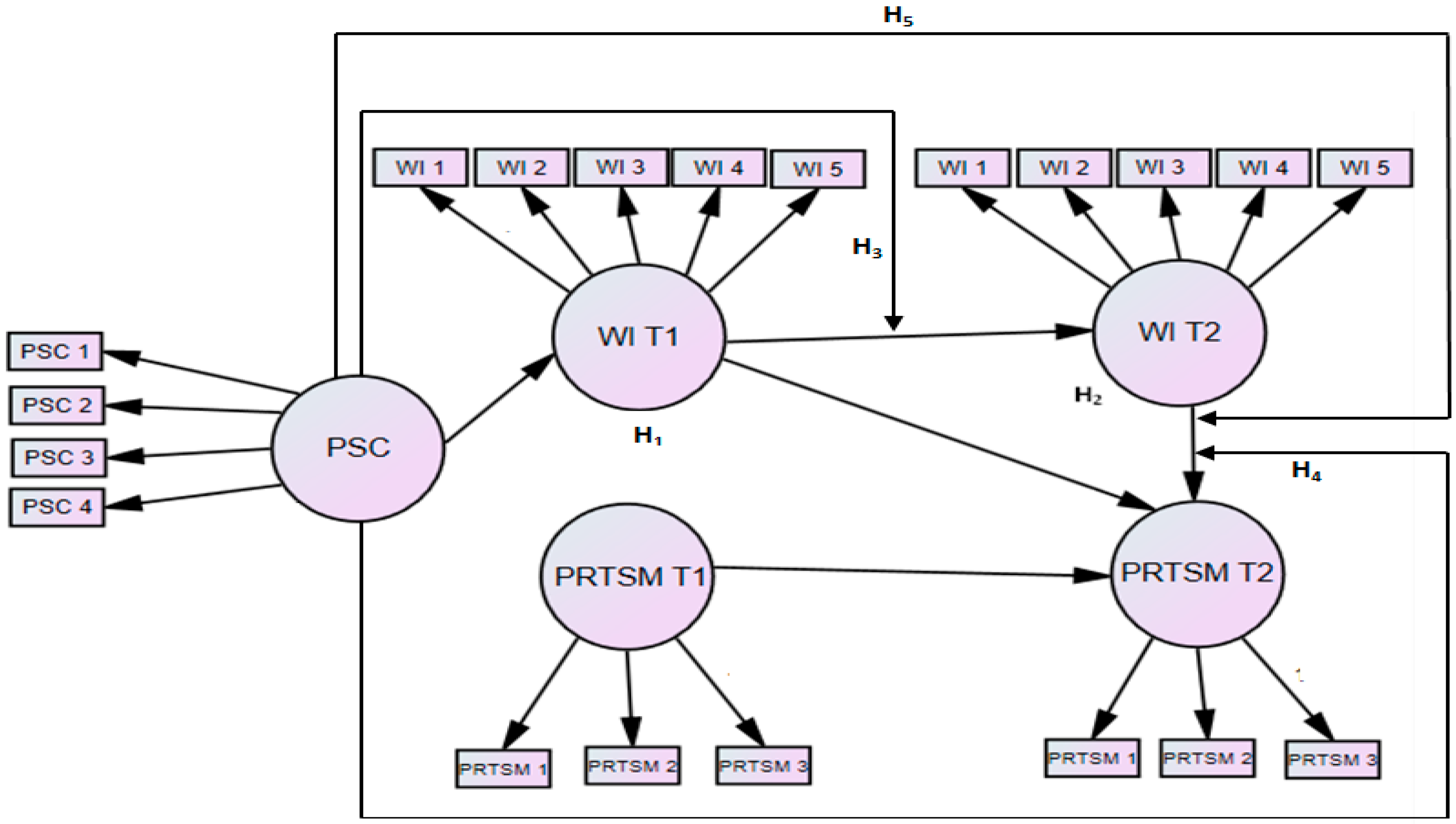
- Investigate the precursor role of PSC by examining its indirect effect on PRTSM at time 2 (PRTSM T2) via WI at time 1 (WI T1).
- Explore a moderated mediation model by testing the moderating role of PSC on the relationship: A. between WI T1 and WI at time 2 (WI T2). B. between WI T2 and PRTSM T2, C. the indirect effect of WI T1 on PRTSM T2. To our knowledge, there is no study that examined such a relationship.
2. Materials and Methods
2.1. Samples and Participants
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Results of Confirmatory Factor Analysis
3.1.1. Measurement Model
3.1.2. Structural Model
4. Discussion
Study Strengths, Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Havaei, F.; Ma, A.; Staempfli, S.; MacPhee, M. Nurses’ Workplace Conditions Impacting Their Mental Health during COVID-19: A Cross-Sectional Survey Study. Healthcare 2021, 9, 84. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.; Peter, E.; Killackey, T.; Maciver, J. The “nurse as hero” discourse in the COVID-19 pandemic: A poststructural discourse analysis. Int. J. Nurs. Stud. 2021, 117, 103887. [Google Scholar] [CrossRef] [PubMed]
- Buheji, M.; Buhaid, N. Nursing human factor during COVID-19 pandemic. Int. J. Nurs. Sci. 2020, 10, 12–24. [Google Scholar] [CrossRef]
- Wankhade, P.; Stokes, P.; Tarba, S.; Rodgers, P. Work intensification and ambidexterity-the notions of extreme and ‘everyday’experiences in emergency contexts: Surfacing dynamics in the ambulance service. Public Manag. Rev. 2020, 22, 48–74. [Google Scholar] [CrossRef]
- Kubicek, B.; Paškvan, M.; Korunka, C. Development and validation of an instrument for assessing job demands arising from accelerated change: The intensification of job demands scale (IDS). Eur. J. Work. Organ. Psychol. 2015, 24, 898–913. [Google Scholar] [CrossRef]
- Bunner, J.; Prem, R.; Korunka, C. How work intensification relates to organization-level safety performance: The mediating roles of safety climate, safety motivation, and safety knowledge. Front. Psychol. 2018, 9, 2575. [Google Scholar] [CrossRef]
- Hu, Q.; Schaufeli, W.B.; Taris, T.W. How are changes in exposure to job demands and job resources related to burnout and engagement? A longitudinal study among Chinese nurses and police officers. Stress Health 2017, 33, 631–644. [Google Scholar] [CrossRef]
- Demerouti, E.; Le Blanc, P.M.; Bakker, A.B.; Schaufeli, W.B.; Hox, J. Present but sick: A three-wave study on job demands, presenteeism and burnout. Career Dev. Int. 2009, 14, 50–68. [Google Scholar] [CrossRef]
- Kinman, G.; Grant, C. Presenteeism during the COVID-19 pandemic: Risks and solutions. Oxf. Univ. Press Behalf Soc. Occup. Med. 2020, 71, 243–244. [Google Scholar] [CrossRef]
- Johns, G. Presenteeism in the workplace: A review and research agenda. J. Organ. Behav. 2010, 31, 519–542. [Google Scholar] [CrossRef]
- Karanika-Murray, M.; Biron, C. The health-performance framework of presenteeism: Towards understanding an adaptive behaviour. Hum. Relat. 2020, 73, 242–261. [Google Scholar] [CrossRef]
- Pilette, P.C. Presenteeism in nursing: A clear and present danger to productivity. JONA J. Nurs. Adm. 2005, 35, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Tori, K.; Dinh, T.T.H.; Mather, C. Healthcare Professional Presenteeism during a COVID-19 Outbreak in an Australian Rural Healthcare Environment: A Case Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8336. [Google Scholar] [CrossRef] [PubMed]
- Koopman, C.; Pelletier, K.R.; Murray, J.F.; Sharda, C.E.; Berger, M.L.; Turpin, R.S.; Hackleman, P.; Gibson, P.; Holmes, D.M.; Bendel, T. Stanford presenteeism scale: Health status and employee productivity. J. Occup. Environ. Med. 2002, 44, 14–20. [Google Scholar] [CrossRef]
- Mosteiro-Díaz, M.P.; Baldonedo-Mosteiro, M.; Borges, E.; Baptista, P.; Queirós, C.; Sánchez-Zaballos, M.; Felli, V.; Abreu, M.; Silva, F.; Franco-Correia, S. Presenteeism in nurses: Comparative study of Spanish, Portuguese and Brazilian nurses. Int. Nurs. Rev. 2020, 67, 466–475. [Google Scholar] [CrossRef]
- Becher, H.; Dollard, M. Psychosocial Safety Climate and Better Productivity in Australian Workplaces—Cost, Productivity, Presenteeism and Abseteeism; Safe Work Australia: Canberra, Australia; University of South Australia: Canberra, Australia, 2016; p. 39. [Google Scholar]
- Li, Y.; Zhang, J.; Wang, S.; Guo, S. The effect of presenteeism on productivity loss in nurses: The mediation of health and the moderation of general self-efficacy. Front. Psychol. 2019, 10, 1745. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Ferreira, P.C.S.; Griep, R.H.; Rotenberg, L. Association between Presenteeism, Psychosocial Aspects of Work and Common Mental Disorders among Nursing Personnel. Int. J. Environ. Res. Public Health 2020, 17, 6758. [Google Scholar] [CrossRef]
- Van Der Feltz-Cornelis, C.M.; Varley, D.; Allgar, V.L.; De Beurs, E. Workplace stress, presenteeism, absenteeism, and resilience amongst university staff and students in the COVID-19 lockdown. Front. Psychiatry 2020, 11, 1284. [Google Scholar] [CrossRef]
- McGregor, A.; Magee, C.A.; Caputi, P.; Iverson, D. A job demands-resources approach to presenteeism. Career Dev. Int. 2016, 21, 402–418. [Google Scholar] [CrossRef]
- Yi, J.-S.; Kim, H. Factors related to presenteeism among South Korean workers exposed to workplace psychological adverse social behavior. Int. J. Environ. Res. Public Health 2020, 17, 3472. [Google Scholar] [CrossRef]
- Ruhle, S.; Breitsohl, H.; Aboagye, E.; Baba, V.; Biron, C.; Leal, C.C.; Dietz, C.; Ferreira, A.I.; Gerich, J.; Johns, G.; et al. “To work, or not to work, that is the question”—Recent trends and avenues for research on presenteeism. Eur. J. Work. Organ. Psychol. 2020, 29, 344–363. [Google Scholar] [CrossRef]
- Liu, B.; Lu, Q.; Zhao, Y.; Zhan, J. Can the psychosocial safety climate reduce ill-health presenteeism? Evidence from Chinese healthcare staff under a dual information processing path lens. Int. J. Environ. Res. Public Health 2020, 17, 2969. [Google Scholar] [CrossRef] [PubMed]
- Dollard, M.F.; Bakker, A.B. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J. Occup. Organ. Psychol. 2010, 83, 579–599. [Google Scholar] [CrossRef]
- Law, R.; Dollard, M.F.; Tuckey, M.R.; Dormann, C. Psychosocial safety climate as a lead indicator of workplace bullying and harassment, job resources, psychological health and employee engagement. Accid. Anal. Prev. 2011, 43, 1782–1793. [Google Scholar] [CrossRef]
- Dollard, M.F.; McTernan, W. Psychosocial safety climate: A multilevel theory of work stress in the health and community service sector. Epidemiol. Psychiatr. Sci. 2011, 20, 287–293. [Google Scholar] [CrossRef]
- Idris, M.A.; Dollard, M.F. A multi-level study of psychosocial safety climate, challenge and hindrance demands, employee exhaustion, engagement and physical health. In Psychosocial Factors at Work in the Asia Pacific; Springer: Berlin/Heidelberg, Germany, 2014; pp. 127–143. [Google Scholar]
- Yulita, M.I.; Dollard, M. Psychosocial safety climate: Past, present, and future research In Psychosocial Factors at Work in the Asia Pacific; Springer: Cham, Switzerland, 2016; pp. 89–134. [Google Scholar]
- Mansour, S.; Tremblay, D.-G. How can we decrease burnout and safety workaround behaviors in health care organizations? The role of psychosocial safety climate. Pers. Rev. 2019, 48, 528–550. [Google Scholar] [CrossRef]
- Chowdhury, S.K.; Endres, M.L. The impact of client variability on nurses’ occupational strain and injury: Cross-level moderation by safety climate. Acad. Manag. J. 2010, 53, 182–198. [Google Scholar] [CrossRef]
- Mansour, S. Psychosocial Safety Climate (PSC). In Handbook on Management and Employment Practices; Springer: Berlin/Heidelberg, Germany, 2022; pp. 459–479. [Google Scholar] [CrossRef]
- Dollard, M.F.; Opie, T.; Lenthall, S.; Wakerman, J.; Knight, S.; Dunn, S.; Rickard, G.; Mac Leod, M. Psychosocial safety climate as an antecedent of work characteristics and psychological strain: A multilevel model. Work Stress 2012, 26, 385–404. [Google Scholar] [CrossRef]
- Hall, G.B.; Dollard, M.F.; Winefield, A.H.; Dormann, C.; Bakker, A.B. Psychosocial safety climate buffers effects of job demands on depression and positive organizational behaviors. Anxiety Stress Coping 2013, 26, 355–377. [Google Scholar] [CrossRef]
- Mansour, S.; Nogues, S.; Tremblay, D.-G. Psychosocial safety climate as a mediator between high-performance work practices and service recovery performance: An international study in the airline industry. Int. J. Hum. Resour. Manag. 2021, 5, 1–35. [Google Scholar] [CrossRef]
- Dollard, M.F. The PSC-4; A Short PSC Tool. In Psychosocial Safety Climate; Springer: Berlin/Heidelberg, Germany, 2019; pp. 385–409. [Google Scholar] [CrossRef]
- Cho, H.; Sagherian, K.; Steege, L.M. Hospital nursing staff perceptions of resources provided by their organizations during the COVID-19 pandemic. Workplace Health Saf. 2021, 69, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Kang, M.; Hong, H.C. Sickness presenteeism in shift and non-shift nurses: Using the fifth Korean working conditions survey. Int. J. Environ. Res. Public Health 2021, 18, 3236. [Google Scholar] [CrossRef] [PubMed]
- Freeling, M.; Rainbow, J.G. Painting a picture of nurse presenteeism: A multi-country integrative review: Nurse presenteeism: An integrative review. Int. J. Nurs. Stud. 2020, 109, 103659. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E. Conservation of resources: A new attempt at conceptualizing stress. Am. Psychol. 1989, 44, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Weick, K. Sensemaking in Organizations; Sage Publications: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Christianson, M.K.; Barton, M.A. Sensemaking in the time of COVID-19. J. Manag. Stud. 2020, 58, 572–576. [Google Scholar] [CrossRef]
- Sagherian, K.; Steege, L.M.; Cobb, S.J.; Cho, H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J. Clin. Nurs. 2020, 5, 1–14. [Google Scholar] [CrossRef]
- Meirun, T.; Bano, S.; Javaid, M.U.; Arshad, M.Z.; Shah, M.U.; Rehman, U.; Parvez, Z.A.; Ilyas, M. Nuances of COVID-19 and Psychosocial Work Environment on Nurses’ Wellbeing: The Mediating Role of Stress and Eustress in Lieu to JD-R Theory. Front. Psychol. 2020, 11, 570236. [Google Scholar] [CrossRef]
- Idris, M.A.; Dollard, M.F.; Winefield, A.H. Integrating psychosocial safety climate in the JD-R model: A study amongst Malaysian workers. SA J. Ind. Psychol. 2011, 37, 29–39. [Google Scholar] [CrossRef]
- Garrick, A.; Mak, A.S.; Cathcart, S.; Winwood, P.C.; Bakker, A.B.; Lushington, K. Psychosocial safety climate moderating the effects of daily job demands and recovery on fatigue and work engagement. J. Occup. Organ. Psychol. 2014, 87, 694–714. [Google Scholar] [CrossRef]
- Oshio, T.; Tsutsumi, A.; Inoue, A.; Suzuki, T.; Miyaki, K. The reciprocal relationship between sickness presenteeism and psychological distress in response to job stressors: Evidence from a three-wave cohort study. J. Occup. Health 2017, 59, 552–561. [Google Scholar] [CrossRef]
- Zadow, A.J.; Dollard, M.F.; Dormann, C.; Landsbergis, P. Predicting new major depression symptoms from long working hours, psychosocial safety climate and work engagement: A population-based cohort study. BMJ Open 2021, 11, e044133. [Google Scholar] [CrossRef] [PubMed]
- Dollard, M.F.; Dormann, C.; Tuckey, M.R.; Escartín, J. Psychosocial safety climate (PSC) and enacted PSC for workplace bullying and psychological health problem reduction. Eur. J. Work. Organ. Psychol. 2017, 26, 844–857. [Google Scholar] [CrossRef]
- Hobfoll, S.E. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Appl. Psychol. 2001, 50, 337–421. [Google Scholar] [CrossRef]
- Van Woerkom, M.; Bakker, A.B.; Nishii, L.H. Accumulative job demands and support for strength use: Fine-tuning the job demands-resources model using conservation of resources theory. J. Appl. Psychol. 2016, 101, 141–150. [Google Scholar] [CrossRef]
- Wright, T.A.; Hobfoll, S.E. Commitment, psychological well-being and job performance: An examination of conservation of resources (COR) theory and job burnout. J. Bus. Manag. 2004, 9, 389–406. [Google Scholar]
- Mansour, S.; Tremblay, D.-G. Workload, generic and work–family specific social supports and job stress: Mediating role of work–family and family–work conflict. Int. J. Contemp. Hosp. Manag. 2016, 28, 1778–1804. [Google Scholar] [CrossRef]
- Miraglia, M.; Johns, G. Going to work ill: A meta-analysis of the correlates of presenteeism and a dual-path model. J. Occup. Health Psychol. 2016, 21, 261–283. [Google Scholar] [CrossRef]
- Loh, M.Y.; Idris, M.A.; Dollard, M.F.; Isahak, M. Psychosocial safety climate as a moderator of the moderators: Contextualizing JDR models and emotional demands effects. J. Occup. Organ. Psychol. 2018, 91, 620–644. [Google Scholar] [CrossRef]
- Mansour, S.; Tremblay, D.-G. Work–family conflict/family–work conflict, job stress, burnout and intention to leave in the hotel industry in Quebec (Canada): Moderating role of need for family friendly practices as “resource passageways”. Int. J. Hum. Resour. Manag. 2018, 29, 2399–2430. [Google Scholar] [CrossRef]
- Mansour, S.; Tremblay, D.-G. The mediating role of work engagement between psychosocial safety climate and organisational citizenship behaviours: A study in the nursing and health sector in Quebec. Int. J. Hum. Resour. Dev. Manag. 2018, 18, 51–71. [Google Scholar] [CrossRef]
- Halbesleben, J.R.B.; Neveu, J.-P.; Paustian-Underdahl, S.C.; Westman, M. Getting to the “COR” understanding the role of resources in conservation of resources theory. J. Manag. 2014, 40, 1334–1364. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Conservation of resource caravans and engaged settings. J. Occup. Organ. Psychol. 2011, 84, 116–122. [Google Scholar] [CrossRef]
- Hobfoll, S.; De Jong, J. The course and limitations of natural recovery from trauma: The centrality of threats to attachment and safety and their Reinstatement. Facil. Resil. Recovery Follow. Trauma. Events 2014, 1, 69–89. [Google Scholar]
- Manapragada, A.; Bruk-Lee, V.; Thompson, A.H.; Heron, L. When safety climate is not enough: Examining the moderating effects of psychosocial hazards on nurse safety performance. J. Adv. Nurs. 2019, 75, 1207–1218. [Google Scholar] [CrossRef]
- Sonnentag, S.; Venz, L.; Casper, A. Advances in recovery research: What have we learned? What should be done next? J. Occup. Health Psychol. 2017, 22, 365–380. [Google Scholar] [CrossRef]
- Mauno, S.; Kubicek, B.; Minkkinen, J.; Korunka, C. Antecedents of intensified job demands: Evidence from Austria. Empl. Relat. Int. J. 2019, 4, 691–707. [Google Scholar] [CrossRef]
- Idris, M.A.; Dollard, M.F.; Tuckey, M.R. Psychosocial safety climate as a management tool for employee engagement and performance: A multilevel analysis. Int. J. Stress Manag. 2015, 22, 183–206. [Google Scholar] [CrossRef]
- Nauman, S.; Raja, U.; Haq, I.U.; Bilal, W. Job demand and employee well-being. Pers. Rev. 2019, 48, 1150–1168. [Google Scholar] [CrossRef]
- Weick, K.E.; Sutcliffe, K.M.; Obstfeld, D. Organizing and the process of sensemaking. Organ. Sci. 2005, 16, 409–421. [Google Scholar] [CrossRef]
- Maitlis, S.; Lawrence, T.B. Triggers and enablers of sensegiving in organizations. Acad. Manag. J. 2007, 50, 57–84. [Google Scholar] [CrossRef]
- Wang, F.; Pollock, K.E.; Hauseman, C. School principals’ job satisfaction: The effects of work intensification. Can. J. Educ. Adm. Policy 2018, 185, 73. [Google Scholar]
- Griffin, M.A.; Curcuruto, M. Safety climate in organizations. Annu. Rev. Organ. Psychol. Organ. Behav. 2016, 3, 191–212. [Google Scholar] [CrossRef]
- Taylor, J.A.; Davis, A.L.; Shepler, L.J.; Lee, J.; Cannuscio, C.; Zohar, D.; Resick, C. Development and validation of the fire service safety climate scale. Saf. Sci. 2019, 118, 126–144. [Google Scholar] [CrossRef]
- Maitlis, S.; Sonenshein, S. Sensemaking in crisis and change: Inspiration and insights from Weick (1988). J. Manag. Stud. 2010, 47, 551–580. [Google Scholar] [CrossRef]
- Maitlis, S.; Christianson, M. Sensemaking in organizations: Taking stock and moving forward. Acad. Manag. Ann. 2014, 8, 57–125. [Google Scholar] [CrossRef]
- Newman, A.; Donohue, R.; Eva, N. Psychological safety: A systematic review of the literature. Hum. Resour. Manag. Rev. 2017, 27, 521–535. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Gagnon, M.; Perron, A.; Dufour, C.; Marcogliese, E.; Pariseau-Legault, P.; Wright, D.K.; Martin, P.; Carnevale, F.A. Blowing the whistle during the first wave of COVID-19: A case study of Quebec nurses. J. Adv. Nurs. 2022, 1–15. [Google Scholar] [CrossRef]
- Marceau, M.; Ledoux, I.; Lavoie, S.; Douma, N.B.; Mailhot-Bisson, D.; Gosselin, É. Exploration of the occupational and personal dimensions impacted by the COVID-19 pandemic for nurses: A qualitative analysis of survey responses. J. Adv. Nurs. 2022, 78, 2150–2164. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural equation modeling with AMOS, EQS, and LISREL: Comparative approaches to testing for the factorial validity of a measuring instrument. Int. J. Test. 2001, 1, 55–86. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Edwards, J.R.; Lambert, L.S. Methods for integrating moderation and mediation: A general analytical framework using moderated path analysis. Psychol. Methods 2007, 12, 1–22. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Cohen, A.; Abedallah, M. The mediating role of burnout on the relationship of emotional intelligence and self-efficacy with OCB and performance. Manag. Res. Rev. 2015, 38, 2–28. [Google Scholar] [CrossRef]
- Berthelsen, H.; Ertel, M.; Geisler, M.; Muhonen, T. Validating the Psychosocial Safety Climate Questionnaire–integration of findings from cognitive interviews in Germany and Sweden. Scand. J. Work. Organ. Psychol. 2019, 4, 9. [Google Scholar] [CrossRef]
- Alshamsi, A.I.; Santos, A.; Thomson, L. Psychosocial Safety Climate moderates the effect of demands of hospital accreditation on healthcare professionals: A longitudinal study. Front. Health Serv. 2022, 2, 824619. [Google Scholar] [CrossRef]
- Arbuckle, J.L. IBM SPSS Amos 20 User’s Guide; Amos Development Corporation, SPSS Inc.: Chicago, IL, USA, 2011; pp. 226–229. [Google Scholar]
- Hayes, A.F. An index and test of linear moderated mediation. Multivar. Behav. Res. 2015, 50, 1–22. [Google Scholar] [CrossRef]
- Choo, C. The knowing organization: How organizations use information to construct meaning, create knowledge and make decisions. Int. J. Inf. Manag. 1996, 16, 329–340. [Google Scholar] [CrossRef]
- Brunetto, Y.; Saheli, N.; Dick, T.; Nelson, S. Psychosocial safety climate, psychological capital, healthcare SLBs’ wellbeing and innovative behaviour during the COVID 19 pandemic. Public Perform. Manag. Rev. 2021, 1, 1–22. [Google Scholar] [CrossRef]
- Afsharian, A.; Zadow, A.; Dollard, M.F. Psychosocial safety climate from two different cultural perspectives in the Asia pacific: Iran and Australia hospitals. In Psychosocial Factors at Work in the Asia Pacific; Springer: Berlin/Heidelberg, Germany, 2016; pp. 187–201. [Google Scholar] [CrossRef]
- Dollard, M.F.; Bailey, T. Building psychosocial safety climate in turbulent times: The case of COVID-19. J. Appl. Psychol. 2021, 106, 951–964. [Google Scholar] [CrossRef]
- Havermans, B.M.; Brouwers, E.P.M.; Hoek, R.J.A.; Anema, J.R.; van der Beek, A.J.; Boot, C.R.L. Work stress prevention needs of employees and supervisors. BMC Public Health 2018, 18, 642. [Google Scholar] [CrossRef]
- Idris, M.A.; Dollard, M.F.; Coward, J.; Dormann, C. Psychosocial safety climate: Conceptual distinctiveness and effect on job demands and worker psychological health. Saf. Sci. 2012, 50, 19–28. [Google Scholar] [CrossRef]
- Seddighi, H.; Dollard, M.F.; Salmani, I. Psychosocial safety climate of employees during the COVID-19 pandemic in Iran: A policy analysis. Disaster Med. Public Health Prep. 2020, 16, 438–444. [Google Scholar] [CrossRef]
- Rainbow, J.G.; Steege, L.M. Presenteeism in nursing: An evolutionary concept analysis. Nurs. Outlook 2017, 65, 615–623. [Google Scholar] [CrossRef]

| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1 | ||||||||||
| 2. Hours’type | 0.10 | 1 | |||||||||
| 3. Department | −0.08 | −0.06 | 1 | ||||||||
| 4. Seniority | 0.52 ** | 0.14 * | −0.09 | 1 | |||||||
| 5. PSC | 2.63 | 0.91 | 0.10 | −0.07 | −0.02 | 0.06 | 0.79 | ||||
| 6. WI T1 | 4.21 | 0.73 | −0.03 | 0.06 | 0.02 | −0.06 | −0.31 ** | 0.88 | |||
| 7. WI T2 | 2.92 | 1.26 | −0.03 | −0.01 | 0.03 | −0.09 | −0.06 | 0.15 ** | 0.85 | ||
| 8. PRTSM T1 | 4.09 | 0.74 | −0.01 | 0.04 | 0.05 | −0.00 | −0.23 ** | 0.25 ** | 0.11 * | 0.79 | |
| 9. PRTSM T2 | 3.21 | 1.45 | 0.01 | 0.10 | 0.11 * | −0.02 | −0.08 | 0.14 * | 0.17 ** | 0.23 ** | 0.86 |
| Variables | Items | Loading | AVE |
|---|---|---|---|
| WI T1 | Since the COVID-Crisis: | 0.60 | |
| 1. It is increasingly rare to have enough time for work tasks | 0.80 | ||
| 2. It is increasingly harder to take time for breaks. | 0.78 | ||
| 3.The time between the more intense work phases has decreased. | 0.84 | ||
| 4. One has more often to do two or three things at once (such as eating lunch, writing emails, and talking on the phone). | 0.80 | ||
| 5. Ever more work has to be completed by fewer and fewer employees | 0.63 | ||
| WI T2 | Since the COVID-Crisis: | 0.50 | |
| 1. It is increasingly rare to have enough time for work tasks | 0.74 | ||
| 2. It is increasingly harder to take time for breaks. | 0.83 | ||
| 3.The time between the more intense work phases has decreased. | 0.66 | ||
| 4. One has more often to do two or three things at once (such as eating lunch, writing emails, and talking on the phone). | 0.72 | ||
| 5. Ever more work has to be completed by fewer and fewer employees | 0.57 | ||
| PSC | 1. Senior management shows support for stress prevention through involvement and commitment. | 0.81 | 0.52 |
| 2. Senior management considers employee psychological health to be as important as productivity. | 0.53 | ||
| 3. There is good communication here about psychological safety issues which affect me. | 0.89 | ||
| 4. In my organization, the prevention of stress involves all levels of the organization. | 0.59 | ||
| PRTSM T1 | 1. Despite having my (health problem), I was able to finish hard tasks in my work. | 0.67 | 0.58 |
| 2. At work, I was able to focus on achieving my goals despite my (health problem). | 0.88 | ||
| 3. Despite having my (health problem), I felt energetic enough to complete all my work. | 0.72 | ||
| PRTSM T2 | 1. Despite having my (health problem), I was able to finish hard tasks in my work. | 0.69 | 0.69 |
| 2. At work, I was able to focus on achieving my goals despite my (health problem). | 0.94 | ||
| 3. Despite having my (health problem), I felt energetic enough to complete all my work. | 0.84 |
| Path | β | p-Value | Bootstrapping Bias-Corrected Percentile Method 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| PSC on PRTSM T2 via WI T1 | −0.06 | <0.01 | 0.11 | −0.01 |
| WI T1 on PRTSM T2 via WI T2 | 0.02 | <0.02 | 0.03 | 0.06 |
| Independent Variables | Dependent Variable: WI T2 (X→M, H3) | |||||
|---|---|---|---|---|---|---|
| Low PSC (≤8, High Risk) | Moderate PSC (>8–12, Moderate Risk) | High PSC (Low Risk, >12, Low Risk) | ||||
| Β | CR | Β | CR | Β | CR | |
| 1. Age | −0.001 ns | −0.01 ns | −0.06 ns | −0.51 | 0.36 ns | 0.22 |
| 2. Hours’type | 0.04 ns | 0.18 | 0.04 ns | 0.15 | 0.11 ns | −0.23 |
| 3. Department | −0.20 ns | −1.5 | 0.12 ns | 0.78 | −0.16 ns | −0.72 |
| 4. Seniority | −0.13 ns | −1.65 | −0.07 ns | −0.75 | −0.05 ns | −0.50 |
| 5. WI T1 | 0.48 ** | 2.77 | 0.12 ns | 0.70 | 0.05 ns | 0.31 |
| R² | 0.17 ** | 0.02 | 0.08 | |||
| Independent Variables | Dependent Variable: PRSTSM T2 (M→Y, H4) | |||||
| 1. Age | −0.20 ns | 1.27 | −0.13 ns | −1.33 | 0.20 ns | 1.37 |
| 2. Type of hours | 0.20 ns | 0.60 | 0.37 * | 1.92 | 0.31 ns | 0.79 |
| 3. Department | 0.07 ns | 0.36 | 0.15 ns | 1.23 | 0.02 ns | 0.11 |
| 4. Seniority | −0.001 ns | −0.01 | −0.02 ns | −0.24 | −0.02 ns | −0.22 |
| 5. PRSTSM T1 | 0.45 ** | 2.64 | 0.29 * | 2.28 | 0.45 ns | 2.64 |
| 6. WI T2 | 0.38 ** | 2.11 | 0.17 * | 1.95 | −0.02 ns | −0.24 |
| R² | 0.15 * | 0.14 | 0.11 | |||
| Low PSC (≤8, High Risk) | Moderate PSC (>8–12, Moderate Risk) | High PSC (Low Risk, >12, Low Risk) | ||||||
|---|---|---|---|---|---|---|---|---|
| β | Bootstrapping Bias-corrected percentile method 95% CI | β | Bootstrapping Bias-corrected percentile method 95% CI | β | Bootstrapping Bias-corrected percentile method 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||
| 0.19 *** | 0.02 | 0.55 | 0.02 ns | −0.03 | 0.12 | −0.001 ns | 0.06 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansour, S.; Faisal Azeem, M.; Dollard, M.; Potter, R. How Psychosocial Safety Climate Helped Alleviate Work Intensification Effects on Presenteeism during the COVID-19 Crisis? A Moderated Mediation Model. Int. J. Environ. Res. Public Health 2022, 19, 13673. https://doi.org/10.3390/ijerph192013673
Mansour S, Faisal Azeem M, Dollard M, Potter R. How Psychosocial Safety Climate Helped Alleviate Work Intensification Effects on Presenteeism during the COVID-19 Crisis? A Moderated Mediation Model. International Journal of Environmental Research and Public Health. 2022; 19(20):13673. https://doi.org/10.3390/ijerph192013673
Chicago/Turabian StyleMansour, Sari, Malik Faisal Azeem, Maureen Dollard, and Rachael Potter. 2022. "How Psychosocial Safety Climate Helped Alleviate Work Intensification Effects on Presenteeism during the COVID-19 Crisis? A Moderated Mediation Model" International Journal of Environmental Research and Public Health 19, no. 20: 13673. https://doi.org/10.3390/ijerph192013673
APA StyleMansour, S., Faisal Azeem, M., Dollard, M., & Potter, R. (2022). How Psychosocial Safety Climate Helped Alleviate Work Intensification Effects on Presenteeism during the COVID-19 Crisis? A Moderated Mediation Model. International Journal of Environmental Research and Public Health, 19(20), 13673. https://doi.org/10.3390/ijerph192013673








