Herbal Decoctions for the Levels of Sulfur Dioxide, Benzopyrene, and Mycotoxin from Traditional Korean Medicine Clinics: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Standards and Reagents
2.3. Experimenting Methods
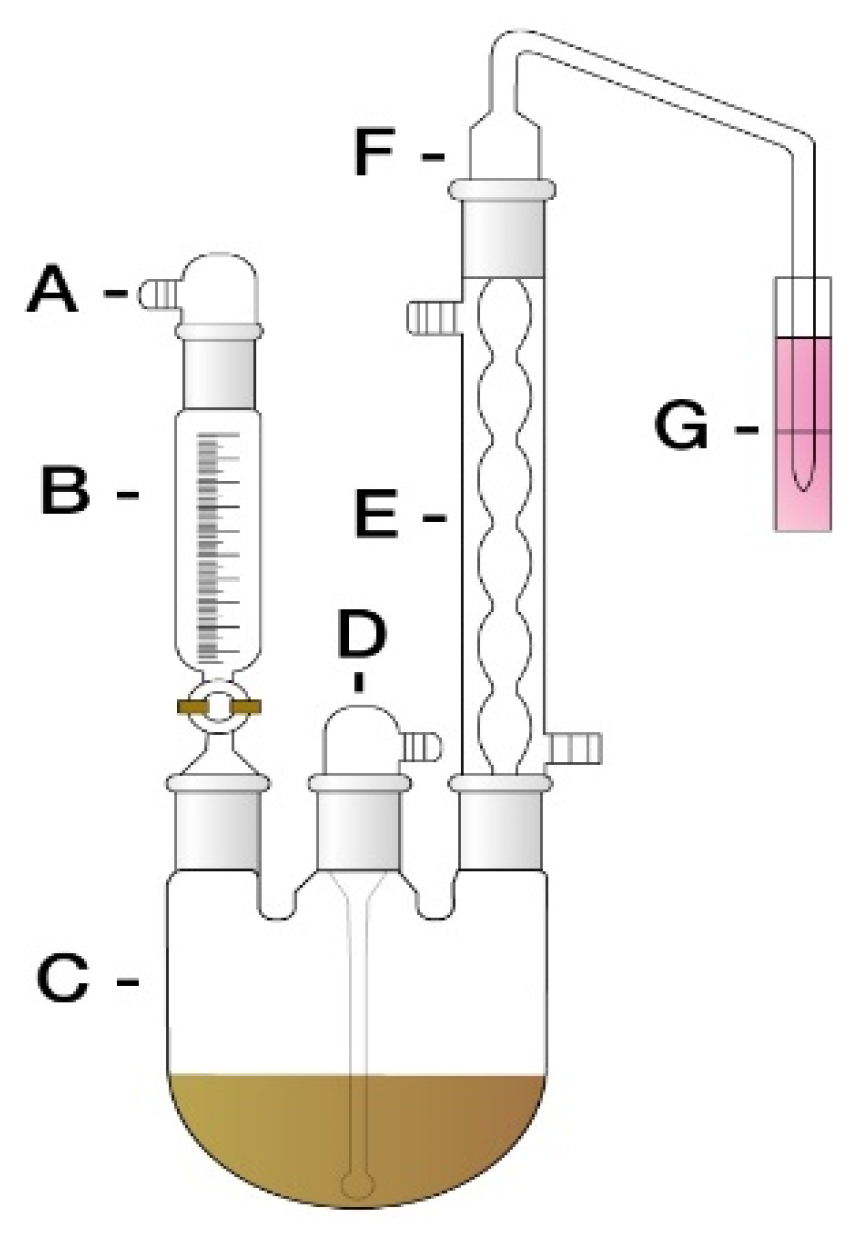
2.3.1. Pre-Treatment of Samples
2.3.2. Analysis Instrument and Analysis Conditions
2.4. Validation of the Test Method
2.4.1. Recovery Rate
2.4.2. Detection Limit (LOD), and Quantitation Limit (LOQ) of the Analytical Equipment
2.5. Test Criteria
3. Results
3.1. Sulfur Dioxide (SO2)
3.2. Mycotoxin
3.3. Benzopyrene
4. Discussion
Limitation of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Herbal Medicine Market Share, Analysis (2029) | COVID-19 Impact. Available online: https://www.fortunebusinessinsights.com/herbal-medicine-market-106320 (accessed on 5 September 2022).
- Welz, A.N.; Emberger-Klein, A.; Menrad, K. Why People Use Herbal Medicine: Insights from a Focus-Group Study in Germany. BMC Complement. Altern. Med. 2018, 18, 92. [Google Scholar] [CrossRef]
- Luo, L.; Wang, B.; Jiang, J.; Fitzgerald, M.; Huang, Q.; Yu, Z.; Li, H.; Zhang, J.; Wei, J.; Yang, C.; et al. Heavy Metal Contaminations in Herbal Medicines: Determination, Comprehensive Risk Assessments, and Solutions. Front. Pharmacol. 2021, 11, 595335. [Google Scholar] [CrossRef] [PubMed]
- Chien, M.-Y.; Yang, C.-M.; Chen, C.-H. Organochlorine Pesticide Residue in Chinese Herbal Medicine. J. Pestic. Sci. 2022, 47, 30–34. [Google Scholar] [CrossRef] [PubMed]
- De Lima, C.M.S.; Fujishima, M.A.T.; de Lima, B.P.; Mastroianni, P.C.; de Sousa, F.F.O.; da Silva, J.O. Microbial Contamination in Herbal Medicines: A Serious Health Hazard to Elderly Consumers. BMC Complement. Med. Ther. 2020, 20, 17. [Google Scholar] [CrossRef] [PubMed]
- Javed, A.; Naeem, I.; Benkerroum, N.; Riaz, M.; Akhtar, S.; Ismail, A.; Sajid, M.; Khan, M.T.; Ismail, Z. Occurrence and Health Risk Assessment of Aflatoxins through Intake of Eastern Herbal Medicines Collected from Four Districts of Southern Punjab—Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 9531. [Google Scholar] [CrossRef]
- Posadzki, P.; Watson, L.; Ernst, E. Contamination and Adulteration of Herbal Medicinal Products (HMPs): An Overview of Systematic Reviews. Eur. J. Clin. Pharmacol. 2013, 69, 295–307. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry Sulfur Dioxide | Medical Management Guidelines | Toxic Substance Portal | ATSDR. Available online: https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=249&toxid=46 (accessed on 9 October 2022).
- New Jersey Department of Health. Right to Know Hazardous Substance Fact Sheet; New Jersey Department of Health: Trenton, NJ, USA, 2017.
- Food and Drug Administration Chemical Hazards | FDA. Available online: https://www.fda.gov/animal-veterinary/biological-chemical-and-physical-contaminants-animal-food/chemical-hazards (accessed on 9 October 2022).
- Tschinkel, P.F.S.; Melo, E.S.P.; Pereira, H.S.; Silva, K.R.N.; Arakaki, D.G.; Lima, N.V.; Fernandes, M.R.; Leite, L.C.S.; Melo, E.S.P.; Melnikov, P.; et al. The Hazardous Level of Heavy Metals in Different Medicinal Plants and Their Decoctions in Water: A Public Health Problem in Brazil. Biomed Res. Int. 2020, 2020, 1465051. [Google Scholar] [CrossRef]
- Zhou, X.; Li, C.-G.; Chang, D.; Bensoussan, A. Current Status and Major Challenges to the Safety and Efficacy Presented by Chinese Herbal Medicine. Medicines 2019, 6, 14. [Google Scholar] [CrossRef]
- WHO. WHO Global Report on Traditional and Complementary Medicine 2019; WHO: Luxembourg, 2019.
- Noviana, E.; Indrayanto, G.; Rohman, A. Advances in Fingerprint Analysis for Standardization and Quality Control of Herbal Medicines. Front. Pharmacol. 2022, 13, 853023. [Google Scholar] [CrossRef]
- Jeong, H.I.; Han, J.-E.; Shin, B.-C.; Jang, S.B.; Won, J.-H.; Han Kim, K.; Sung, S.-H. Monitoring of Heavy Metals and Pesticide Residues of Herbal Decoctions in Traditional Korean Medicine Clinics in Korea. Int. J. Environ. Res. Public Health 2022, 19, 8523. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. The 2017 Korean Medicine Utilization and Herbal Medicine Consumption Survey. Available online: https://www.koms.or.kr/board/researchReport/view.do?post_no=46&menu_no=21 (accessed on 1 April 2022).
- Ministry of Food and Drug Safety. The Korean Pharmacopoeia; Ministry of Food and Drug Safety: North Chungcheong, Korea, 2022.
- Lafeuille, J.-L.; Lefevre, S.; Achouri, D. Determination of Added Sulfites in Dried Garlic with a Modified Version of the Optimized Monier-Williams Method. J. AOAC Int. 2007, 90, 1090–1097. [Google Scholar] [CrossRef] [PubMed]
- Warner, C.R.; Daniels, D.H.; Joe, F.L.; Fazio, T. Reevaluation of Monier-Williams Method for Determining Sulfite in Food. J. Assoc. Off. Anal. Chem. 1986, 69, 3–5. [Google Scholar] [CrossRef]
- Turner, N.W.; Bramhmbhatt, H.; Szabo-Vezse, M.; Poma, A.; Coker, R.; Piletsky, S.A. Analytical Methods for Determination of Mycotoxins: An Update (2009–2014). Anal. Chim. Acta 2015, 901, 12–33. [Google Scholar] [CrossRef] [PubMed]
- Gazioglu, I.; Tekkeli, S.E.K. Development and Validation of a HPLC Method for the Determination of Benzo(a)Pyrene in Human Breast Milk. Food Sci. Biotechnol. 2017, 26, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.I.; Kim, K.H.; Won, J.H.; Sung, G.U.; Kim, J.W.; Han, J.; Sung, A.D.M.; Park, E.J.; Sung, S.H. Development of Hazardous Materials Management Standard for Decoction Type of Personalized Herbal Medicine. J. Pharmacopunct. 2020, 23, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Chang-Seob, S.; Dae-Sun, H.; Jun-Kyoung, L.; Hye-Kyung, H.; Jin-Mi, C.; Young-Ran, U.; Seol, J.; Hyeun-Kyoo, S. Concentration of Heavy Metals, Residual Pesticides and Sulfur Dioxide before/after a Decoction—In Prescription Consist of Sipjeondaebo-Tang. J. Korean Oriental. Med. 2009, 30, 108–117. [Google Scholar]
- Yu, I.S.; Lee, J.S.; Kim, S.D.; Kim, Y.H.; Park, H.W.; Ryu, H.J.; Lee, J.H.; Lee, J.M.; Jung, K.; Na, C.; et al. Monitoring Heavy Metals, Residual Agricultural Chemicals and Sulfites in Traditional Herbal Decoctions. BMC Complement. Altern. Med. 2017, 17, 154. [Google Scholar] [CrossRef]
- Huang, B.; Chen, Q.; Wang, L.; Gao, X.; Zhu, W.; Mu, P.; Deng, Y. Aflatoxin B1 Induces Neurotoxicity through Reactive Oxygen Species Generation, DNA Damage, Apoptosis, and S-Phase Cell Cycle Arrest. Int. J. Mol. Sci. 2020, 21, 6517. [Google Scholar] [CrossRef]
- World Health Organization. Aflatoxins: Some Naturally Occurring Substances: Food Items and Constituents, Heterocyclic Aromatic Amines and Mycotoxins. IARC Monogr. Eval. Carcinog. Risks Hum. 1993, 56, 245–395. [Google Scholar]
- Ikeagwulonu, R.C.; Onyenekwe, C.C.; Oshim, I.O.; Olise, N.A.; Odeyemi, O.; Ojidei, C.K. Investigation of the Levels of Total Aflatoxin in Herbal Traditional Medicines from Selected Vendors Dealers in South-Eastern Nigeria. J. Adv. Med. Pharm. Sci. 2020, 22, 26–31. [Google Scholar] [CrossRef][Green Version]
- Ravindra, K.; Sokhi, R.; van Grieken, R. Atmospheric Polycyclic Aromatic Hydrocarbons: Source Attribution, Emission Factors and Regulation. Atmos. Environ. 2008, 42, 2895–2921. [Google Scholar] [CrossRef]
- Korea Food & Drug Administration. Criteria and Method of Benzopyrene for Herbal; Korea Food & Drug Administration: Osong, Korea, 2009.
- Human Health Risk Assessment | US EPA. Available online: https://www.epa.gov/risk/human-health-risk-assessment (accessed on 1 April 2022).
- Herbal Medicinal Products | European Medicines Agency. Available online: https://www.ema.europa.eu/en/human-regulatory/herbal-medicinal-products (accessed on 1 April 2022).
- World Health Organization. WHO Guidelines for Assessing Quality of Herbal Medicines with Reference to Contaminants and Residues; World Health Organization: Geneva, Switzerland, 2007.
- Segalstad, S.H. International IT Regulations and Compliance: Quality Standards in the Pharmaceutical and Regulated Industries; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2008; p. 324. [Google Scholar]
- Pharmaceutical Inspection Cooperation Scheme. Annual Report 2019; Pharmaceutical Inspection Cooperation Scheme: Geneva, Switzerland, 2020. [Google Scholar]
| Instrument | Analysis Condition (Waters, USA 2475 FLD, Alliance 2695) |
|---|---|
| Column | Xbridge C18 (4.6 × 250 mm, 5 μm) |
| Mobile phase | Water·Methanol·Acetonitrile (60:25:15) |
| Flow rate | 1.0 mL/min |
| Injection volume | 10 μL |
| Post-column derivatization system | Post Column Reaction Module (PBPB) |
| Detector | Fluorescence (Ex: 365 nm Em: 435 nm) |
| Instrument | Analysis Condition (Waters, USA 2475 FLD, Alliance 2695) |
|---|---|
| Column | PAH C18 (4.6 × 250 mm, 5 μm) |
| Mobile phase | Acetonitrile·Water (8:2) |
| Flow rate | 1.0 mL/min |
| Injection volume | 10 μL |
| Detector | Fluorescence (Ex: 294 nm Em: 404 nm) |
| 7.5 ppm | 15 ppm | 30 ppm | 60 ppm | |
|---|---|---|---|---|
| Recovery rate (%) | 84.3 ± 5.0 | 88.3 ± 5.0 | 88.7 ± 3.1 | 90.3 ± 5.5 |
| 5 ppb | 10 ppb | 20 ppb | ||
|---|---|---|---|---|
| Recovery rate (%) | Aflatoxin B1 | 88.3 ± 6.2 | 91.7 ± 6.9 | 96.8 ± 5.5 |
| Aflatoxin B2 | 84.6 ± 1.2 | 89.3 ± 5.2 | 96.2 ± 6.8 | |
| Aflatoxin G1 | 79.7 ± 3.7 | 89.6 ± 9.4 | 89.8 ± 5.0 | |
| Aflatoxin G2 | 78.6 ± 3.2 | 82.7 ± 3.0 | 82.8 ± 2.3 | |
| Benzopyrene | 3-Methylcholanthrene | |
|---|---|---|
| Recovery rate (%) | 105.3 ± 7.4 | 84.2 ± 6.3 |
| Limit of Detection (ppm) | Limit of Quantitation (ppm) | |
|---|---|---|
| Aflatoxin B1 | 0.07 | 0.24 |
| Aflatoxin B2 | 0.05 | 0.18 |
| Aflatoxin G1 | 0.07 | 0.22 |
| Aflatoxin G2 | 0.05 | 0.15 |
| Limit of Detection (ppm) | Limit of Quantitation (ppm) | |
|---|---|---|
| Benzopyrene | 0.025 | 0.077 |
| Herbal Decoctions | TKM Clinics (ppm) | TKM Hospitals (ppm) | External Herbal Dispensaries (ppm) |
|---|---|---|---|
| Galgeun-tang | 0.000 | 0.000 | 0.000 |
| Kangwhalyupung-tang | 0.000 | 0.000 | 0.000 |
| Dangguisu-san | 0.000 | 0.000 | 0.000 |
| Dokhwalgisaeng-tang | ND | ND | ND |
| Banhasasim-tang | ND | ND | 0.000 |
| Bangpungtongseong-san | ND | ND | ND |
| Bojungikgi-tang | ND | ND | ND |
| Sipjeondaebo-tang | ND | ND | ND |
| Ssanghwa-tang | ND | ND | ND |
| Ojeok-san | ND | ND | ND |
| Test criteria | ≤30 ppm | ≤30 ppm | ≤30 ppm |
| Herbal Decoctions | Aflatoxin B1 (ppb) | Aflatoxin B2 (ppb) | Aflatoxin G1 (ppb) | Aflatoxin G2 (ppb) | Total Aflatoxin (ppb) | |
|---|---|---|---|---|---|---|
| TKM Clinics | Galgeun-tang | ND | ND | ND | 0.05 | 0.05 |
| Kangwhalyupung-tang | ND | ND | 0.04 | 0.02 | 0.05 | |
| Dangguisu-san | ND | 0.01 | 0.12 | 0.02 | 0.15 | |
| Dokhwalgisaeng-tang | ND | 0.00 | 0.05 | 0.03 | 0.08 | |
| Banhasasim-tang | ND | ND | ND | ND | ND | |
| Bangpungtongseong-san | ND | ND | ND | 0.03 | 0.03 | |
| Bojungikgi-tang | ND | ND | 0.29 | ND | 0.29 | |
| Sipjeondaebo-tang | ND | 0.01 | 0.05 | ND | 0.06 | |
| Ssanghwa-tang | ND | ND | 0.03 | 0.93 | 0.96 | |
| Ojeok-san | ND | ND | ND | ND | ND | |
| TKM Hospitals | Galgeun-tang | ND | ND | ND | ND | ND |
| Kangwhalyupung-tang | ND | ND | ND | ND | ND | |
| Dangguisu-san | ND | ND | ND | ND | ND | |
| Dokhwalgisaeng-tang | ND | 0.04 | 0.05 | ND | 0.09 | |
| Banhasasim-tang | ND | ND | ND | ND | ND | |
| Bangpungtongseong-san | ND | ND | ND | ND | ND | |
| Bojungikgi-tang | ND | ND | ND | ND | ND | |
| Sipjeondaebo-tang | ND | 0.02 | 0.11 | ND | 0.12 | |
| Ssanghwa-tang | ND | ND | 0.05 | ND | 0.05 | |
| Ojeok-san | ND | ND | 0.06 | ND | 0.07 | |
| External Herbal Dispensaries | Galgeun-tang | ND | ND | ND | ND | ND |
| Kangwhalyupung-tang | ND | ND | ND | ND | ND | |
| Dangguisu-san | ND | ND | ND | ND | ND | |
| Dokhwalgisaeng-tang | ND | ND | ND | ND | ND | |
| Banhasasim-tang | ND | ND | ND | ND | ND | |
| Bangpungtongseong-san | ND | ND | ND | ND | ND | |
| Bojungikgi-tang | ND | ND | ND | ND | ND | |
| Sipjeondaebo-tang | ND | ND | ND | ND | ND | |
| Ssanghwa-tang | ND | ND | ND | ND | ND | |
| Ojeok-san | ND | ND | ND | ND | ND | |
| Test criteria | ≤15 ppb of total aflatoxin and ≤10 ppb of aflatoxin B1 | |||||
| Herbal Decoctions | TKM Clinics (ppb) | TKM Hospitals (ppb) | External Herbal Dispensaries (ppb) |
|---|---|---|---|
| Galgeun-tang | ND | ND | ND |
| Kangwhalyupung-tang | ND | ND | ND |
| Dangguisu-san | ND | ND | ND |
| Dokhwalgisaeng-tang | ND | ND | ND |
| Banhasasim-tang | ND | ND | ND |
| Bangpungtongseong-san | ND | ND | ND |
| Bojungikgi-tang | ND | ND | ND |
| Sipjeondaebo-tang | ND | ND | ND |
| Ssanghwa-tang | ND | ND | ND |
| Ojeok-san | ND | ND | ND |
| Test criteria | ≤5 ppb | ≤5 ppb | ≤5 ppb |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, H.I.; Han, J.-E.; Shin, B.-C.; Jang, S.; Won, J.-H.; Kim, K.H.; Sung, S.-H. Herbal Decoctions for the Levels of Sulfur Dioxide, Benzopyrene, and Mycotoxin from Traditional Korean Medicine Clinics: A Preliminary Study. Int. J. Environ. Res. Public Health 2022, 19, 13595. https://doi.org/10.3390/ijerph192013595
Jeong HI, Han J-E, Shin B-C, Jang S, Won J-H, Kim KH, Sung S-H. Herbal Decoctions for the Levels of Sulfur Dioxide, Benzopyrene, and Mycotoxin from Traditional Korean Medicine Clinics: A Preliminary Study. International Journal of Environmental Research and Public Health. 2022; 19(20):13595. https://doi.org/10.3390/ijerph192013595
Chicago/Turabian StyleJeong, Hye In, Ji-Eun Han, Byung-Cheul Shin, Soobin Jang, Jae-Hee Won, Kyeong Han Kim, and Soo-Hyun Sung. 2022. "Herbal Decoctions for the Levels of Sulfur Dioxide, Benzopyrene, and Mycotoxin from Traditional Korean Medicine Clinics: A Preliminary Study" International Journal of Environmental Research and Public Health 19, no. 20: 13595. https://doi.org/10.3390/ijerph192013595
APA StyleJeong, H. I., Han, J.-E., Shin, B.-C., Jang, S., Won, J.-H., Kim, K. H., & Sung, S.-H. (2022). Herbal Decoctions for the Levels of Sulfur Dioxide, Benzopyrene, and Mycotoxin from Traditional Korean Medicine Clinics: A Preliminary Study. International Journal of Environmental Research and Public Health, 19(20), 13595. https://doi.org/10.3390/ijerph192013595





