Enumeration of the Public Health Workforce in New York State: Workforce Changes in the Wake of COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Analysis
3. Results
3.1. Participants
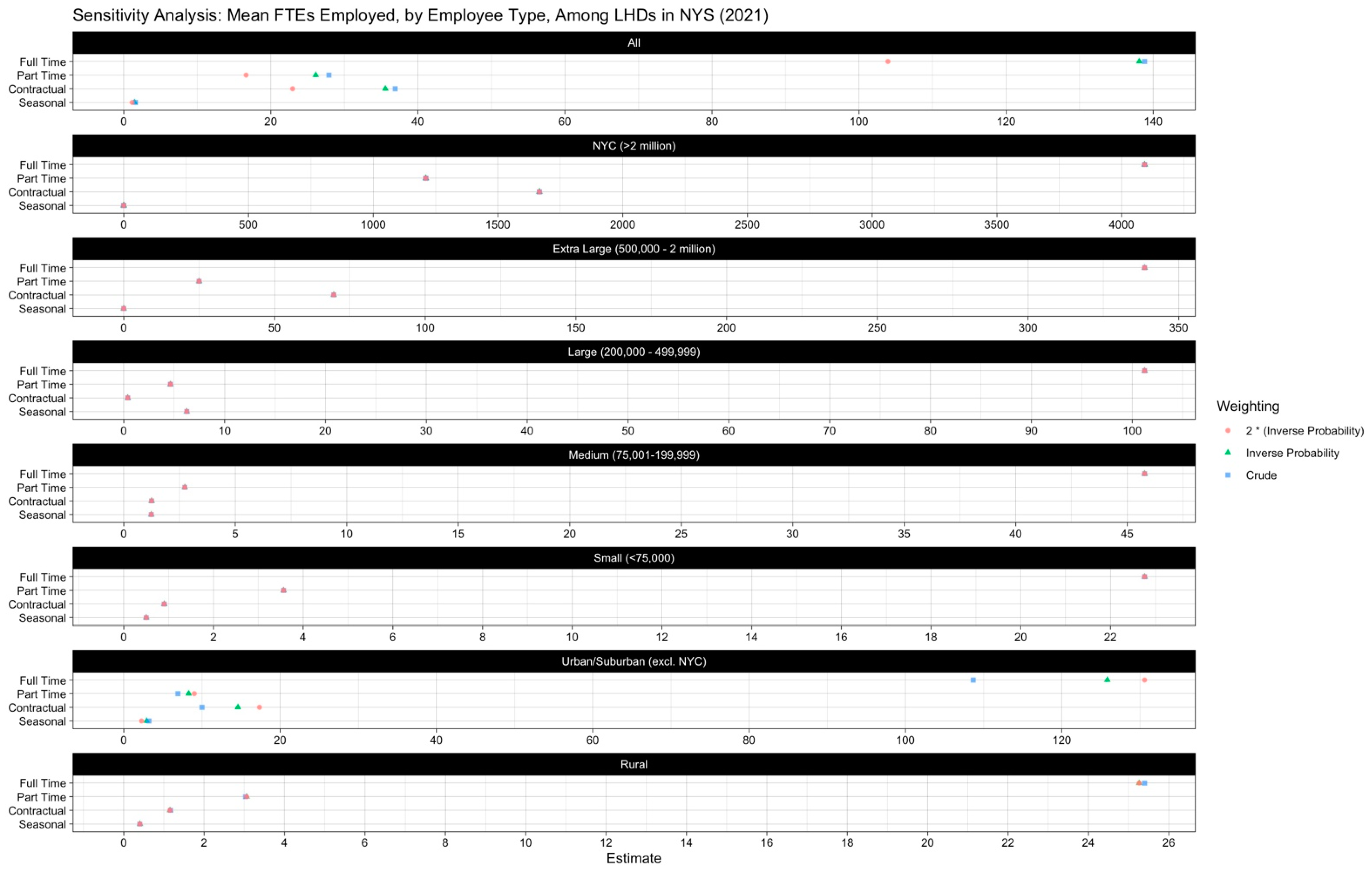
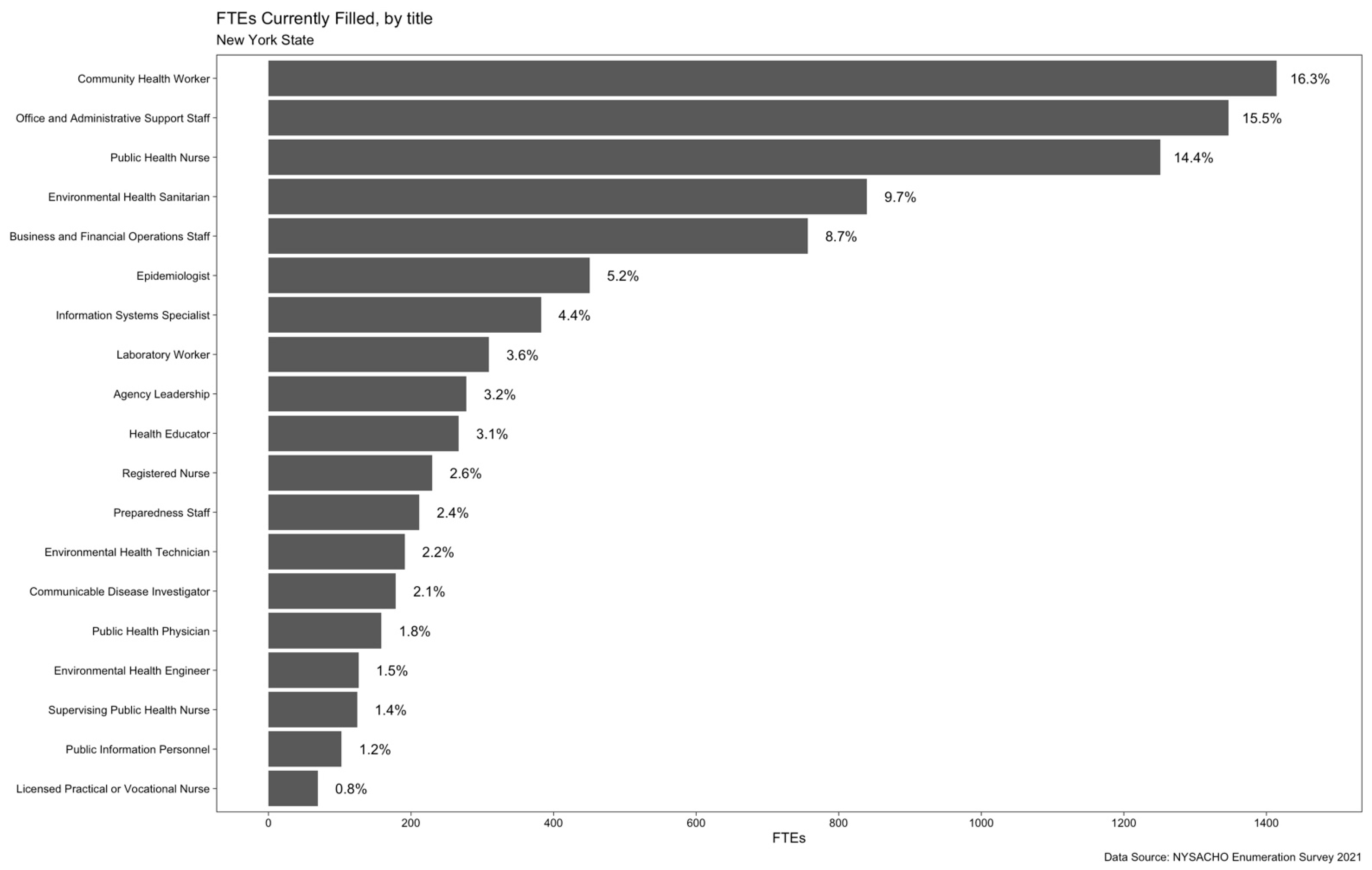
3.2. Workforce Size, Type and Composition
3.3. Changes over Time
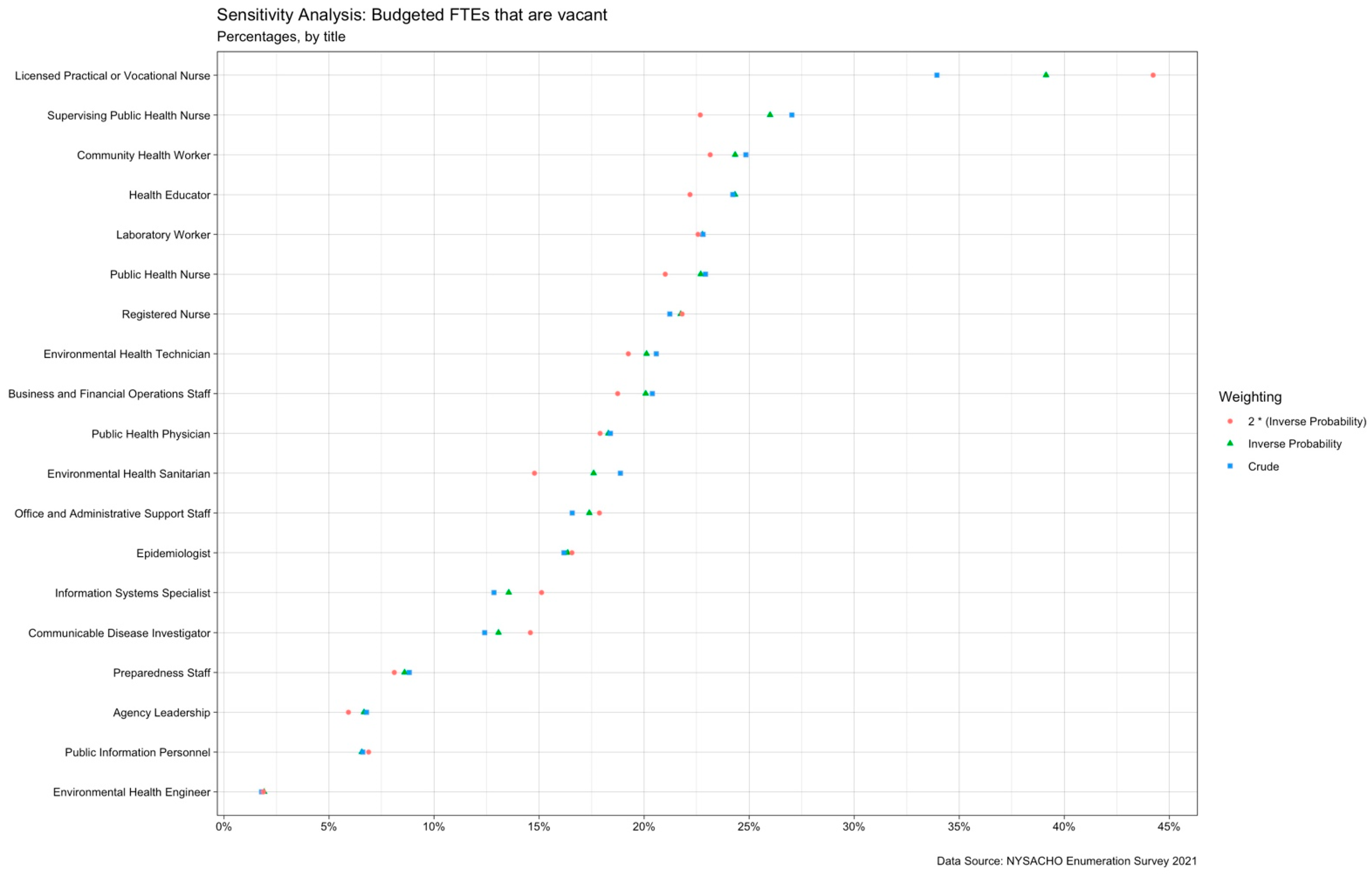
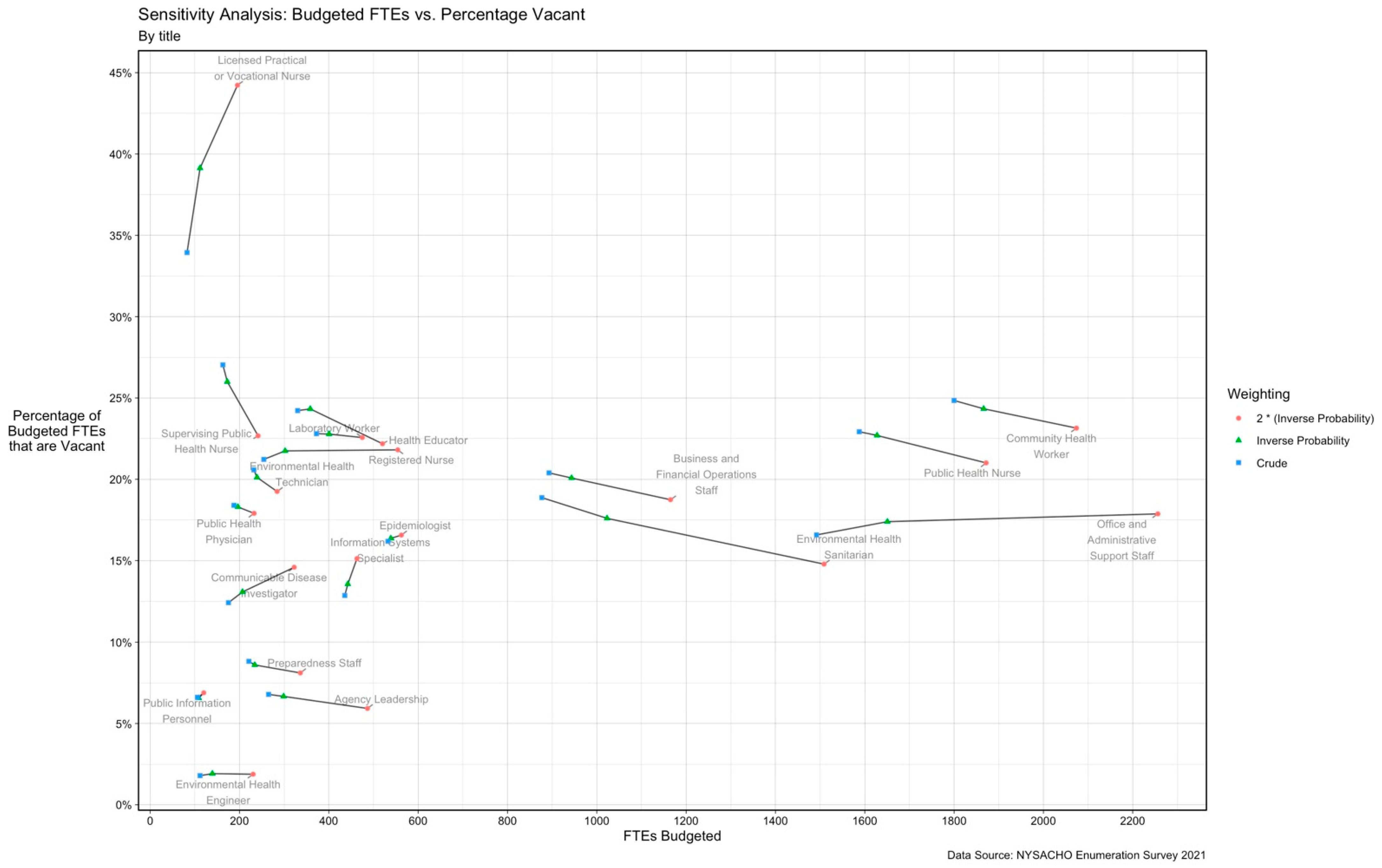
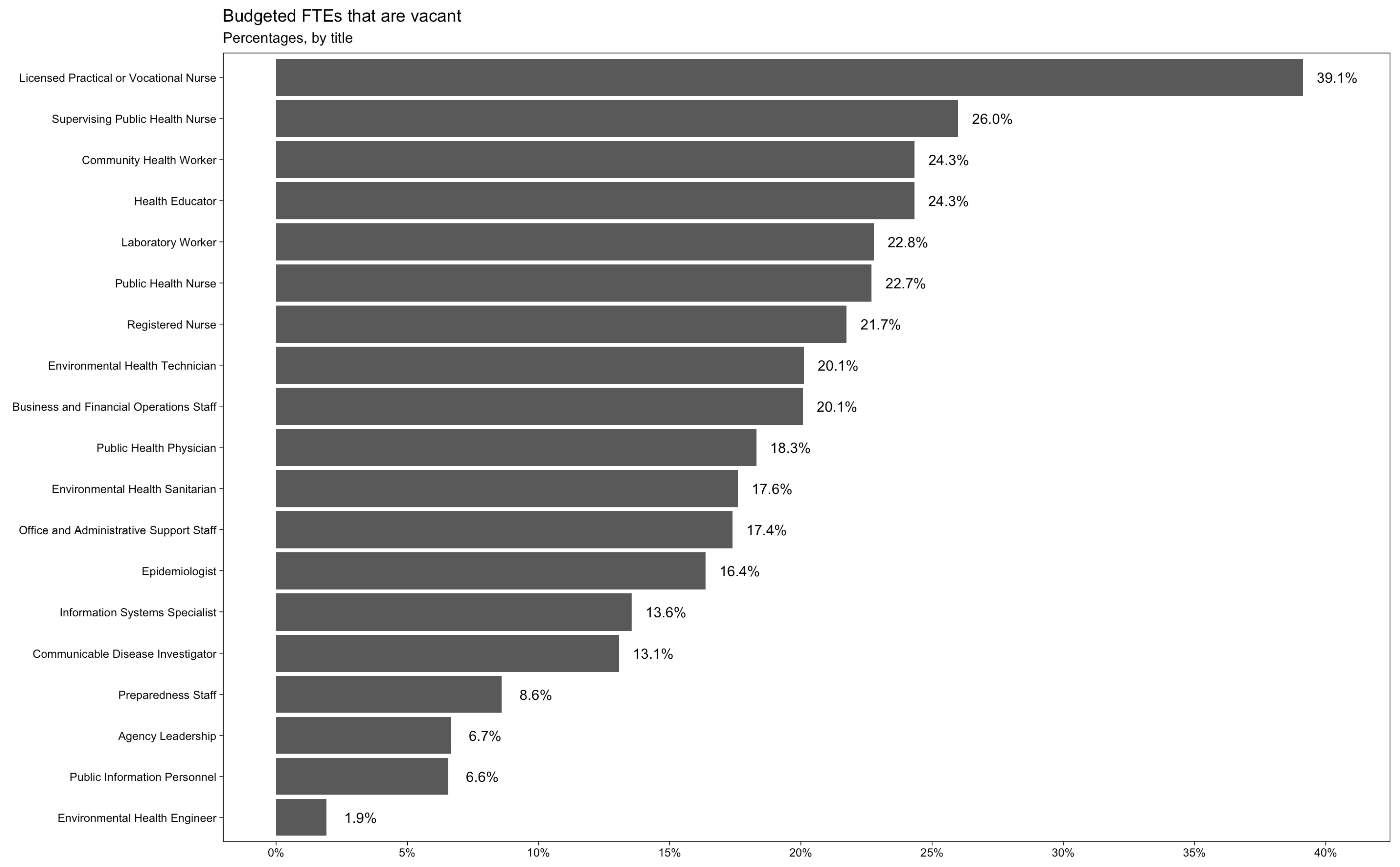
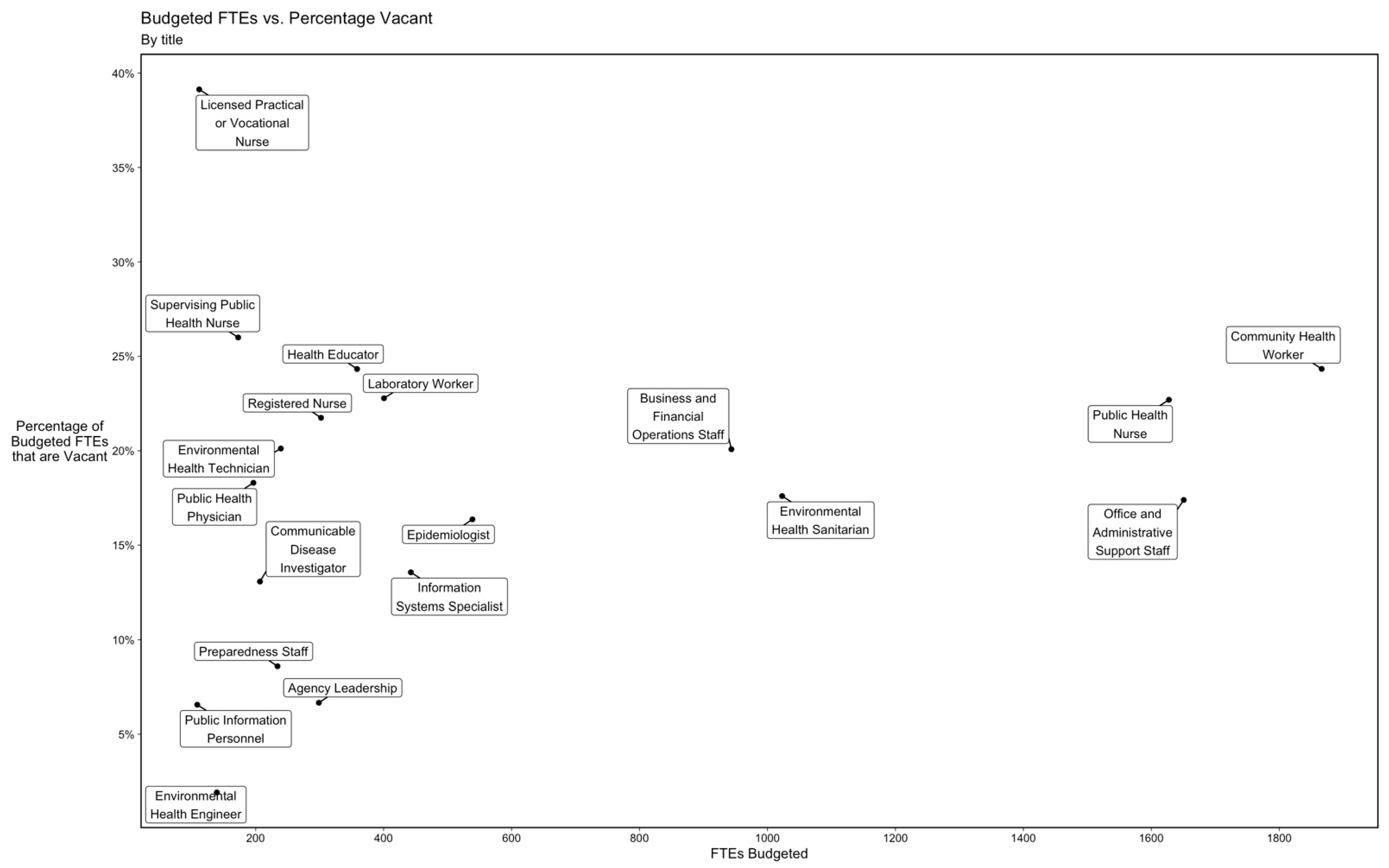
3.4. Workforce Vacancies
3.5. RecruitmentChallenges
4. Discussion
4.1. Sufficient Number of Staff
4.2. Composition of Staff
4.3. Applicability, Strengths, and Limitations of the Survey
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Bipartisan Policy Center. Public Health Forward: Modernizing the US Public Health System. Washington, DC, USA. December 2021. Available online: https://bipartisanpolicy.org/report/public-health-forward/ (accessed on 15 June 2022).
- NACCHO. 2019 Profile Study: Changes in Local Health Department Workforce and Finance Capacity since 2008. Research Brief, May 2020. Available online: https://www.naccho.org/uploads/downloadable-resources/2019-Profile-Workforce-and-Finance-Capacity.pdf (accessed on 15 June 2022).
- Dinkin, P.; Kumar, P.; Laboissiere, M.; Lurie, E.; Parthasarthy, R.; Willson, M. Care for the Caretakers: Building the Global Public Health Workforce. McKinsey & Company. 2022. Available online: https://www.mckinsey.com/industries/public-and-social-sector/our-insights/care-for-the-caretakers-building-the-global-public-health-workforce (accessed on 30 September 2022).
- DeSalvo, K.; Hughes, B.; Bassett, M.; Benjamin, G.; Fraser, M.; Galea, S.; Garcia, J.; Howard, J. Public Health COVID-19 Impact Assessment: Lessons Learned and Compelling Needs. Perspectives, Expert Voices in Health and Health Care. National Academy of Medicine. 7 April 2021. Available online: Nam.edu/TransformingHealth (accessed on 18 April 2022).
- New York State Department of Health. New York State Statewide COVID-19 Fatalities by County. Available online: https://health.data.ny.gov/Health/New-York-State-Statewide-COVID-19-Fatalities-by-Co/xymy-pny5 (accessed on 25 August 2022).
- Public Health Law, NY: Article 6, State Aid to Cities and Counties. The New York State Senate. Published 22 September 2014. Available online: https://www.nysenate.gov/legislation/laws/PBH/A6 (accessed on 12 October 2022).
- General Municipal Law, NY: Article 2, General Municipal Finances § 3-C Limit upon Real Property Tax Levies by Local Governments. The New York State Senate. Published 19 April 2019. Available online: https://www.nysenate.gov/legislation/laws/GMU/3-C (accessed on 12 October 2022).
- Lav, I.J.; Leachman, M. State Limits on Property Taxes Hamstring Local Services and Should Be Relaxed or Repealed. Center on Budget and Policy Priorities. Published 18 July 2018. Available online: https://www.cbpp.org/research/state-budget-and-tax/state-limits-on-property-taxes-hamstring-local-services-and-should-be (accessed on 12 October 2022).
- Beck, A.J.; Boulton, M.L.; Coronado, F. Enumeration of the Governmental Public Health Workforce. Am. J. Prev. Med. 2014, 47 (Suppl. 3), S306–S313. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.J.; Coronado, F.; Boulton, M.L.; Merrill, J.A. Public Health Enumeration Working Group. The public health workforce taxonomy: Revisions and recommendations for implementation. J. Public Health Manag. Pract. 2018, 24, E1–E11. [Google Scholar] [CrossRef] [PubMed]
- Sumaya, C.V. Enumeration and composition of the public health workforce: Challenges and strategies. Am. J. Public Health 2012, 102, 469–474. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 18 April 2022).
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Wickham, H.; Bryan, J. Readxl: Read Excel Files. R Package Version 1.4.0. 2022. Available online: https://CRAN.R-project.org/package=readxl (accessed on 18 April 2022).
- Firke, S. Janitor: Simple Tools for Examining and Cleaning Dirty Data. R Package Version 2.1.0. 2021. Available online: https://CRAN.R-project.org/package=janitor (accessed on 18 April 2022).
- Wickham, H.; Seidel, D. Scales: Scale Functions for Visualization. R Package Version 1.2.0. 2022. Available online: https://CRAN.R-project.org/package=scales (accessed on 18 April 2022).
- NYSACHO. Support the Prepare Act: Public Health Reinvestment and Emergency Pandemic Adaptability, Readiness and Efficiency. Available online: https://www.nysacho.org/news/the-prepare-act-public-health-reinvestment-and-emergency-pandemic-adaptability-readiness-and-efficiency/ (accessed on 17 August 2022).
- Carlin, M.; Ensign, K.; Person, C.; Kittle, A.; Meadows, K. State of the Public Health Workforce: Trends and Challenges Leading up to the COVID-19 Pandemic. J. Public Health Manag. Pract. 2021, 27, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.; Thomas, S.; Williams, D.; Kennedy, J.; Burke, S. Implications for health system reform, workforce recovery and rebuilding in the context of the Great Recession and COVID-19: A case study of workforce trends in Ireland 2008–2021. Hum. Resour. Health 2022, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rechel, B.; Jakubowski, E.; McKee, M.; Nolte, E. Organization and Financing of Public Health Services in Europe: Country reports [Internet]; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2018; (Health Policy Series, No. 49.). Available online: https://www.ncbi.nlm.nih.gov/books/NBK507325/ (accessed on 20 September 2022).
- Watts, R.; Bowles, D.; Fisher, C.; Li, I. Public health job advertisements in Australia and New Zealand: A changing landscape. Aust. N. Z. J. Public Health 2019, 43, 522–528. [Google Scholar] [CrossRef] [PubMed]
- McGinnis, S.; Robertson, D.; Moore, J. Enumeration of the Local Public Health Workforce in New York: 2006; Center for Health Workforce Studies, School of Public Health, SUNY Albany: Rensselaer, NY, USA, 2008; Available online: https://www.chwsny.org/wp-content/uploads/2008/01/lphenumeration20082006_final_reduced2.pdf (accessed on 15 June 2022).
- Sim, F.; Lock, K.; McKee, M. Maximizing the contribution of the public health workforce: The English experience. Bull. World Health Organ. 2007, 85, 935–940. [Google Scholar] [CrossRef] [PubMed]
| LHDs in NYS | NACCHO 2019 Survey Participants | NYSACHO 2021 Survey Participants | |
|---|---|---|---|
| Size of Population Served | |||
| NYC (>2 million) | 1 | 1 | 1 |
| Extra Large (500,000–2 million) | 5 | 3 | 3 |
| Large (250,000–499,999) | 8 | 5 | 8 |
| Medium (75,001–249,999) | 18 | 13 | 17 |
| Small (<75,000) | 26 | 15 | 23 |
| Service Level | |||
| Full Service LHDs | 36 | 24 | 32 |
| Partial Service LHDs | 22 | 13 | 20 |
| Urbanicity | |||
| NYC | 1 | 1 | 1 |
| Urban/Suburban (w/o NYC) | 25 | 16 | 22 |
| Rural | 32 | 20 | 29 |
| Region | |||
| Capital Region | 8 | 5 | 8 |
| Central New York | 5 | 5 | 5 |
| Finger Lakes | 9 | 7 | 7 |
| Long Island | 2 | 1 | 1 |
| Mid-Hudson | 7 | 3 | 6 |
| Mohawk Valley | 6 | 3 | 5 |
| New York City | 1 | 1 | 1 |
| North Country | 7 | 5 | 7 |
| Southern Tier | 8 | 4 | 7 |
| Western New York | 5 | 3 | 5 |
| Full Time | Part Time | Contractual | Seasonal | |
|---|---|---|---|---|
| Overall | 138.1 (6–4092) | 26.1 (0–1211) | 35.6 (0–1666) | 1.5 (0–38) |
| Size of Population Served | ||||
| NYC (>2 million) | 4091.9 | 1210.6 | 1666.0 | 0 |
| Extra Large (500,000–2 million) | 338.7 (210–585) | 25.0 (1–65) | 69.7 (0–209) | 0.0 (0–0) |
| Large (200,000–499,999) | 101.2 (30–163) | 4.6 (0–13) | 0.4 (0–1) | 6.2 (0–38) |
| Medium (75,001–199,999) | 45.8 (10–89) | 2.7 (0–18) | 1.2 (0–8) | 1.2 (0–21) |
| Small (<75,000) | 22.8 (6–87) | 3.6 (0–40) | 0.9 (0–5) | 0.5 (0–10) |
| Urbanicity | ||||
| Urban/Suburban (excl. NYC) | 125.8 (16–585) | 8.3 (0–65) | 14.6 (0–209) | 2.9 (0–38) |
| Rural | 25.3 (6–87) | 3.1 (0–40) | 1.2 (0–8) | 0.4 (0–10) |
| NACCHO 2019 | NYSACHO 2021 | Difference | % Change | n | |
|---|---|---|---|---|---|
| Overall | |||||
| All Respondents | 8960 | 9111 | 151 | 2% | 34 |
| Size of Population Served | |||||
| NYC (>2 million) | 6956 | 6968 | 12 | 0% | 1 |
| Extra Large (500,000–2 million) | 265 | 484 | 219 | 83% | 1 |
| Large (200,000–499,999) | 721 | 561 | −160 | −22% | 5 |
| Medium (75,001–199,999) | 612 | 643 | 31 | 5% | 13 |
| Small (<75,000) | 407 | 455 | 49 | 12% | 14 |
| Employee Type | NACCHO 2019 | NYSACHO 2021 | Difference | % Change |
|---|---|---|---|---|
| Full Time | 6428.0 | 4751.0 | −1677.4 | −26% |
| Part Time | 1347.6 | 1225.0 | −123.0 | −9% |
| Contractual | 13.7 | 1686.0 | 1672.8 | 12,210% |
| Seasonal | 58.4 | 32.0 | −26.4 | −45% |
| Budgeted | Vacant | Vacancy Rate | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Population | n | 2019 | 2021 | Change | 2019 | 2021 | Change | 2019 | 2021 | Change |
| All Respondents | 34 | 10,198.00 | 11,318.40 | 1120.40 | 1237.60 | 2207.10 | 969.5 | 12.10% | 19.50% | 7.40% |
| NYC (>2 million) | 1 | 8110.00 | 8893.10 | 783.1 | 1154.00 | 1924.70 | 770.7 | 14.20% | 21.60% | 7.40% |
| Extra Large (500,000–2 million) | 1 | 281 | 520 | 239 | 16 | 36 | 20 | 5.70% | 6.90% | 1.20% |
| Large (200,000–499,999) | 5 | 755.5 | 678 | −77.5 | 34.5 | 117 | 82.5 | 4.60% | 17.30% | 12.70% |
| Medium (75,001–199,999) | 13 | 631.7 | 712.2 | 80.5 | 19.9 | 69.5 | 49.6 | 3.20% | 9.80% | 6.60% |
| Small (<75,000) | 14 | 419.8 | 515.1 | 95.3 | 13.2 | 59.9 | 46.7 | 3.10% | 11.60% | 8.50% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michaels, I.; Pirani, S.; Fleming, M.; Arana, M.M.; D’Angelo, E.; Dyer-Drobnack, C.; DiManno, M.; Ravenhall, S.; Gloria, C.T. Enumeration of the Public Health Workforce in New York State: Workforce Changes in the Wake of COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 13592. https://doi.org/10.3390/ijerph192013592
Michaels I, Pirani S, Fleming M, Arana MM, D’Angelo E, Dyer-Drobnack C, DiManno M, Ravenhall S, Gloria CT. Enumeration of the Public Health Workforce in New York State: Workforce Changes in the Wake of COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(20):13592. https://doi.org/10.3390/ijerph192013592
Chicago/Turabian StyleMichaels, Isaac, Sylvia Pirani, Molly Fleming, Mayela M. Arana, Emily D’Angelo, Cristina Dyer-Drobnack, Margaret DiManno, Sarah Ravenhall, and Christian T. Gloria. 2022. "Enumeration of the Public Health Workforce in New York State: Workforce Changes in the Wake of COVID-19" International Journal of Environmental Research and Public Health 19, no. 20: 13592. https://doi.org/10.3390/ijerph192013592
APA StyleMichaels, I., Pirani, S., Fleming, M., Arana, M. M., D’Angelo, E., Dyer-Drobnack, C., DiManno, M., Ravenhall, S., & Gloria, C. T. (2022). Enumeration of the Public Health Workforce in New York State: Workforce Changes in the Wake of COVID-19. International Journal of Environmental Research and Public Health, 19(20), 13592. https://doi.org/10.3390/ijerph192013592









