Cone Beam Computed Tomography in the Assessment of the Effectiveness of Physical Therapy with the Use of the Electromagnetic Field Combined with Light Radiation Emitted by LEDs in the Treatment of Inflammation of the Paranasal Sinuses—A Case Study
Abstract
1. Introduction
2. Aim of Study
3. Material and Methods
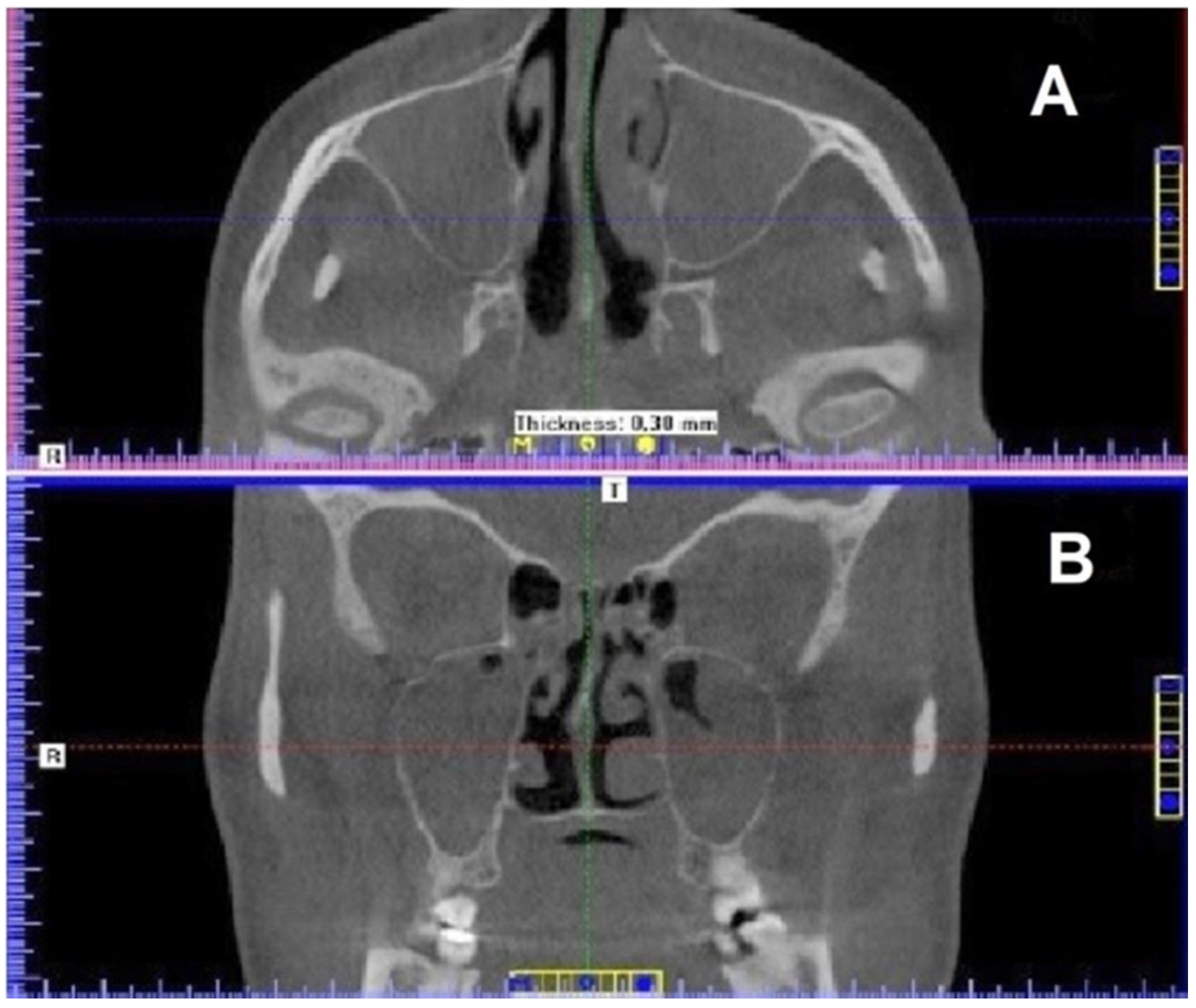
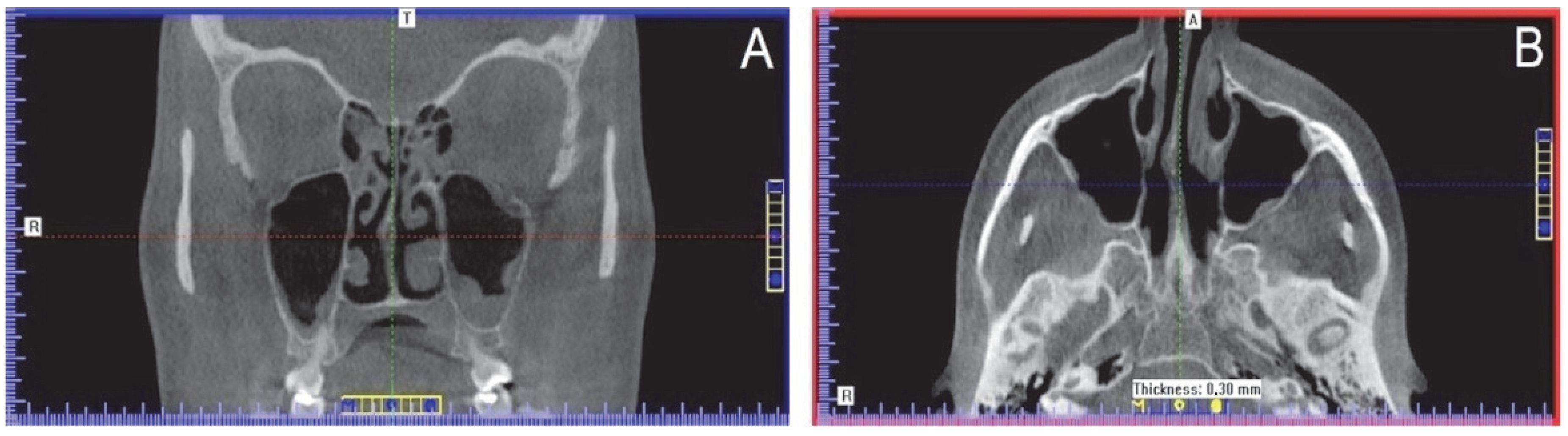
4. Results
5. Discussion
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| ELF-EMF | Extremely Low Frequency—Electromagnetic Field |
| LED | Light Emitting Diode |
| IR | infrared light |
| R | red light |
References
- Jager, L.; Rammelsberg, P.; Reiser, M. Bildgebende Diagnostik der Normalanatomie des Temporomandibulargelenks. Radiologe 2001, 41, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Young, H.M.; Sun Park, C.K.; Chau, O.W.; Lee, T.Y.; Gaede, S. Technical Note: Volumetric computed tomography for radiotherapy simulation and treatment planning. J. Appl. Clin. Med. Phys. 2021, 22, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Howerton, W.B., Jr.; Mora, M.A. Advancements in digital imaging. What is new and on the horizon? J. Am. Dent. Assoc. 2008, 139 (Suppl. 3), S20–S24. [Google Scholar] [CrossRef]
- Loubele, M.; Bogaerts, R.; Van Dijck, E.; Pauwels, R.; Vanheusden, S.; Suetens, P.; Marchal, G.; Sanderink, G.; Jacobs, R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacialis applications. Eur. J. Radiol. 2009, 71, 461–468. [Google Scholar] [CrossRef]
- Bargan, S.; Merrill, R.; Tetradis, S. Cone beam computed tomography imaging in the evaluation of the temporomandibular joint. J. Calif Dent Assoc. 2010, 38, 33–39. [Google Scholar]
- Anjos Pontual, M.L.; Freire, J.S.; Barbosa, J.M.; Frazão, M.A.; dos Anjos Pontual, A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac. Radiol. 2012, 41, 24–29. [Google Scholar] [CrossRef]
- Phothikhun, S.; Suphanantachat, S.; Chuenchompoonut, V.; Nisapakultorn, K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J. Periodontol. 2012, 83, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.A.; Drage, N.A.; Davies, J.; Thomas, D.W. Effective dose from cone beam CT examinations in dentistry. Brit. J. Radiol. 2009, 82, 35–40. [Google Scholar] [CrossRef]
- Loubbele, M.; Jacobs, R.; Maes, F.; Denis, K.; White, S.; Coudyzer, W.; Lambrichts, I.; van Steenberghe, D.; Suetens, P. Image quality vs. radiation dose of four cone beam computed tomography scaners. Dentomaxillofac. Radiol. 2008, 37, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Scarfe, W.C.; Farman, A.G. What is cone-beam CK and how does it work? Dent Clin. N. Am. 2008, 52, 707–730. [Google Scholar] [CrossRef]
- Calderhead, R.G.; Won-Serk, K.; Ohshiro, T.; Trelles, M.A.; Vasily, D.B. Adjunctive 830 nm light-emitting diode therapy can improve the results following aesthetic procedures. Laser Ther. 2015, 24, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Barolet, D.B. Light-emitting diodes (LEDs) in dermatology. Semin Cutan Med. Surg. 2008, 27, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Paolillo, F.R.; Borghi-Silva, A.; Parizotto, N.A.; Curachi, C.; Bagnato, V.S. New treatment of cellulite with infrared-LED illumination applied during high-intensity treadmill training. J. Cosmet Laser Ther. 2011, 13, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Russell, B.A.; Kellett, N.; Reilly, L.R. A study to determine the efficacy of combination LED light therapy (633nm and 830nm) in facial skin rejuvenation. J. Cosmet Laser Ther. 2005, 7, 196–200. [Google Scholar] [CrossRef] [PubMed]
- von Felbert, V.; Kernland-Lang, K.; Hoffmann, G.; Wienert, V.; Simon, D.; Hunziker, T. Irradiation with water-filtered infrared A plus visible light improves cutaneous scleroderma lesions in a series of cases. Dermatology 2011, 222, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Pall, M.L. Electromagnetic fields act via activation of voltage-gated calcium channels to produce beneficial or adverse effects. J. Cell Mol. Med. 2013, 17, 958–965. [Google Scholar] [CrossRef]
- Fan, W.; Qian, F.; Ma, Q.; Zhang, P.; Chen, T.; Chen, C.; Zhang, Y.; Deng, P.; Zhou, Z.; Yu, Z. 50 Hz electromagnetic field exposure promotes proliferation and cytokine production of bone marrow mesen-chymal stem cells. Int. J. Clin. Exp. Med. 2015, 8, 7394–7404. [Google Scholar]
- Pilla, A.; Fitzsimmons, R.; Muehsam, D.; Wu, J.; Rohde, C.; Casper, D. Electromagnetic fields as first messenger in biological signaling: Application to calmodulin-dependent signaling in tissue repair. Biochim. Biophys. Acta 2011, 1810, 1236–1245. [Google Scholar] [CrossRef]
- Marcinkowska-Gapińska, A.; Nawrocka-Bogusz, H. Analysis of the magnetic field influence on the rheological properties of healthy person’s blood. BioMed Res. Int. 2013, 2013, 490410. [Google Scholar] [CrossRef]
- Vianale, G.; Reale, M.; Amerio, P.; Stefanachi, M.; Di Luzio, S.; Muraro, R. Extremely low frequency electromagnetic field enhances human keratinocyte cell growth and decreases pro-inflammatory chemokine production. Br. J. Dermatol. 2008, 158, 1189–1196. [Google Scholar] [CrossRef]
- Patruno, A.; Amerio, P.; Pesce, M.; Vianale, G.; Di Luzio, S.; Tulli, A.; Franceschelli, S.; Grilli, A.; Muraro, R.; Reale, M. Extremely low frequency electromagnetic fields modulate expression of inducible nitric oxide syn-thase, endothelial nitric oxide synthase and cyclooxygenase–2 in the human keratinocyte cell line HaCaT: Potential therapeutic effects in wound healing. Br. J. Dermatol. 2010, 162, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.L.; Teli, T.; Harrison, B.S. Effect of electromagnetic field on cyclic adenosine monophosphate (cAMP) in a human mu-opioid receptor cell model. Electromagn Biol Med. 2016, 35, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Lietz-Kijak, D.; Ardan, R. Physiotherapeutic reduction of orofacial pain using extremely low-frequency electromagnetic field and light-emitting diode therapy-a pilot study. Pain Res. Manag. 2022, 2022, 3115154. [Google Scholar] [CrossRef] [PubMed]
- Kopacz, Ł.; Ciosek, Ż.; Gronwald, H.; Skomro, P.; Ardan, R.; Lietz-Kijak, D. Comparative analysis of the influence of selected physical factors on the level of pain in the course of temporomandibular joint disorders. Pain Res. Manag. 2020, 2020, 1036306. [Google Scholar] [CrossRef] [PubMed]
- Cieślar, G.; Mrowiec, J.; Kasperczyk, S.; Sieroń-Stoltny, K.; Sieroń, A. Analgesic effect of simultaneous exposure to infrared laser radiation and μT magnetic field in rats. In Mechanisms for Low-Light Therapy III; Hamblin, M.R., Waynant, R.W., Anders, J., Eds.; SPIE: Bellingham, WA, USA, 2008; Volume 6846, pp. 74–80. [Google Scholar]
- Gualdi, G.; Costantini, E.; Reale, M.; Amerio, P. Wound repair and extremely low frequency-electromagnetic field: Insight from in vitro study and potential clinical application. Int J. Mol. Sci. 2021, 22, 5037. [Google Scholar] [CrossRef] [PubMed]
- Pasek, J.; Pasek, T.; Sieroń-Stołtny, K.; Cieślar, G.; Sieroń, A. Electromagnetic fields in medicine–The state of art. Electromagn. Biol. Med. 2016, 35, 170–175. [Google Scholar] [CrossRef]
- Gordon, G.A. Designed electromagnetic pulsed therapy: Clinical applications. J. Cell Physiol. 2007, 212, 579–582. [Google Scholar] [CrossRef]
- Nelson, F.R.; Zvirbulis, R.; Pilla, A.A. Non-invasive electromagnetic field therapy produces rapid and substantial pain reduction in early knee osteoarthritis: A randomized double-blind pilot study. Rheumatol. Int. 2013, 33, 2169–2173. [Google Scholar] [CrossRef]
- Pesce, M.; Patruno, A.; Speranza, L.; Reale, M. Extremely low frequency electromagnetic field and wound healing: Implication of cytokines as biological mediators. Eur. Cytokine Netw. 2013, 24, 1–10. [Google Scholar] [CrossRef]
- Cieślar, G.; Rozmus-Kuczia, I.; Łatka, U.; Matyszkiewicz, B.; Krzeszkowiak, T.; Mrowiec, J.; Sieroń-Stołtny, K.; Sieroń, A. Estimation of clinical efficacy of Viofor JPS System Magnetic & Light Therapy–device for magnetostimulation connected with light energy in the treatment of degenerative and inflammatory diseases of joints. Balneol. Pol. 2004, 46, 42–58. [Google Scholar]
- Lietz-Kijak, D.; Kijak, E.; Śliwiński, Z.; Opalko, K. The use of physiotherapy in the regeneration of periapical bone structures of the teeth, prepared to load the prosthetic. Adv. Hyg. Exper. Med. 2013, 67, 643–647. [Google Scholar] [CrossRef] [PubMed]
- Ghogomu, N.; Kern, R. Chronic rhinosinusitis: The rationale for current treatments. Expert Rev. Clin. Immunol. 2017, 13, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Guilemany, J.M.; Alobid, I.; Mullo, J. Controversies in the treatment of chronic rhinosinusitis. Expert Rev. Respir Med. 2010, 4, 463–477. [Google Scholar] [CrossRef] [PubMed]
- Sedaghat, A.R. Chronic Rhinosinusitis. Am. Fam Physician. 2017, 96, 500–506. [Google Scholar] [PubMed]
- Rosenfeld, R.M.; Piccirillo, J.F.; Chandrasekhar, S.S.; Brook, I.; Kumar, A.K.; Kramper, M.; Orlandi, R.R.; Palmer, J.N.; Patel, Z.M.; Peters, A.; et al. Clinical practice guideline (update): Adult sinusitis. Otolaryngol. Head Neck Surg. 2015, 152 (Suppl. 2), S1–S39. [Google Scholar] [CrossRef]
- Mullol, J.; Obando, A.; Pujols, L.; Alobid, I. Corticosteroid treatment in chronic rhinosinusitis: The possibilities and the limits. Immunol Allergy Clin. N. Am. 2009, 29, 657–668. [Google Scholar] [CrossRef]
- Pasek, J.; Misiak, A.; Mucha, R.; Pasek, T.; Sieroń, A. New possibilities in physical therapy-magnetolaserotherapy. Physioter. Pol. 2008, 8, 1–10. [Google Scholar]
- Sieroń, A.; Pasek, J.; Mucha, R. Magnetic field and light energy in medicine and rehabilitation-magnetoledotherapy. Balneol. Pol. 2007, 49, 1–7. [Google Scholar]
- Pasek, J.; Pasek, T.; Sieroń, A. Some practical recommendations in the use of magnetic fields and light in physical medicine. Acta Bio-Opt. Inform. Med. 2007, 13, 284–285. [Google Scholar]
- Orien, A.; Pasek, J.; Mucha, R. Low-energy light in medicine and rehabilitation. Rehabil. Pract. 2007, 2, 25–27. [Google Scholar]
- Sieroń, A.; Cieślar, G.; Krawczyk-Krupka, A.; Biniszkiewicz, T.; Bilska, A.; Adamek, M. Application of Magnetic Fields in Medicine, 2nd ed.; Į-Medica Press: Bielsko, Biała, 2002. [Google Scholar]
- Reddy, G.K. Biological basis and clinical role of low-intensity lasers in biology and medicine. J. Clin. Laser Med. Surg. 2004, 22, 141–150. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kijak, K.; Cieślar, G.; Kowacka, M.; Skomro, P.; Gronwald, H.; Garstka, A.; Lietz-Kijak, D. Cone Beam Computed Tomography in the Assessment of the Effectiveness of Physical Therapy with the Use of the Electromagnetic Field Combined with Light Radiation Emitted by LEDs in the Treatment of Inflammation of the Paranasal Sinuses—A Case Study. Int. J. Environ. Res. Public Health 2022, 19, 13570. https://doi.org/10.3390/ijerph192013570
Kijak K, Cieślar G, Kowacka M, Skomro P, Gronwald H, Garstka A, Lietz-Kijak D. Cone Beam Computed Tomography in the Assessment of the Effectiveness of Physical Therapy with the Use of the Electromagnetic Field Combined with Light Radiation Emitted by LEDs in the Treatment of Inflammation of the Paranasal Sinuses—A Case Study. International Journal of Environmental Research and Public Health. 2022; 19(20):13570. https://doi.org/10.3390/ijerph192013570
Chicago/Turabian StyleKijak, Konrad, Grzegorz Cieślar, Małgorzata Kowacka, Piotr Skomro, Helena Gronwald, Adam Garstka, and Danuta Lietz-Kijak. 2022. "Cone Beam Computed Tomography in the Assessment of the Effectiveness of Physical Therapy with the Use of the Electromagnetic Field Combined with Light Radiation Emitted by LEDs in the Treatment of Inflammation of the Paranasal Sinuses—A Case Study" International Journal of Environmental Research and Public Health 19, no. 20: 13570. https://doi.org/10.3390/ijerph192013570
APA StyleKijak, K., Cieślar, G., Kowacka, M., Skomro, P., Gronwald, H., Garstka, A., & Lietz-Kijak, D. (2022). Cone Beam Computed Tomography in the Assessment of the Effectiveness of Physical Therapy with the Use of the Electromagnetic Field Combined with Light Radiation Emitted by LEDs in the Treatment of Inflammation of the Paranasal Sinuses—A Case Study. International Journal of Environmental Research and Public Health, 19(20), 13570. https://doi.org/10.3390/ijerph192013570








