The Effects of Individual Characteristics of the Naval Personnel on Sleepiness and Stress during Two Different Watchkeeping Schedules
Abstract
1. Introduction
2. Materials and Methods
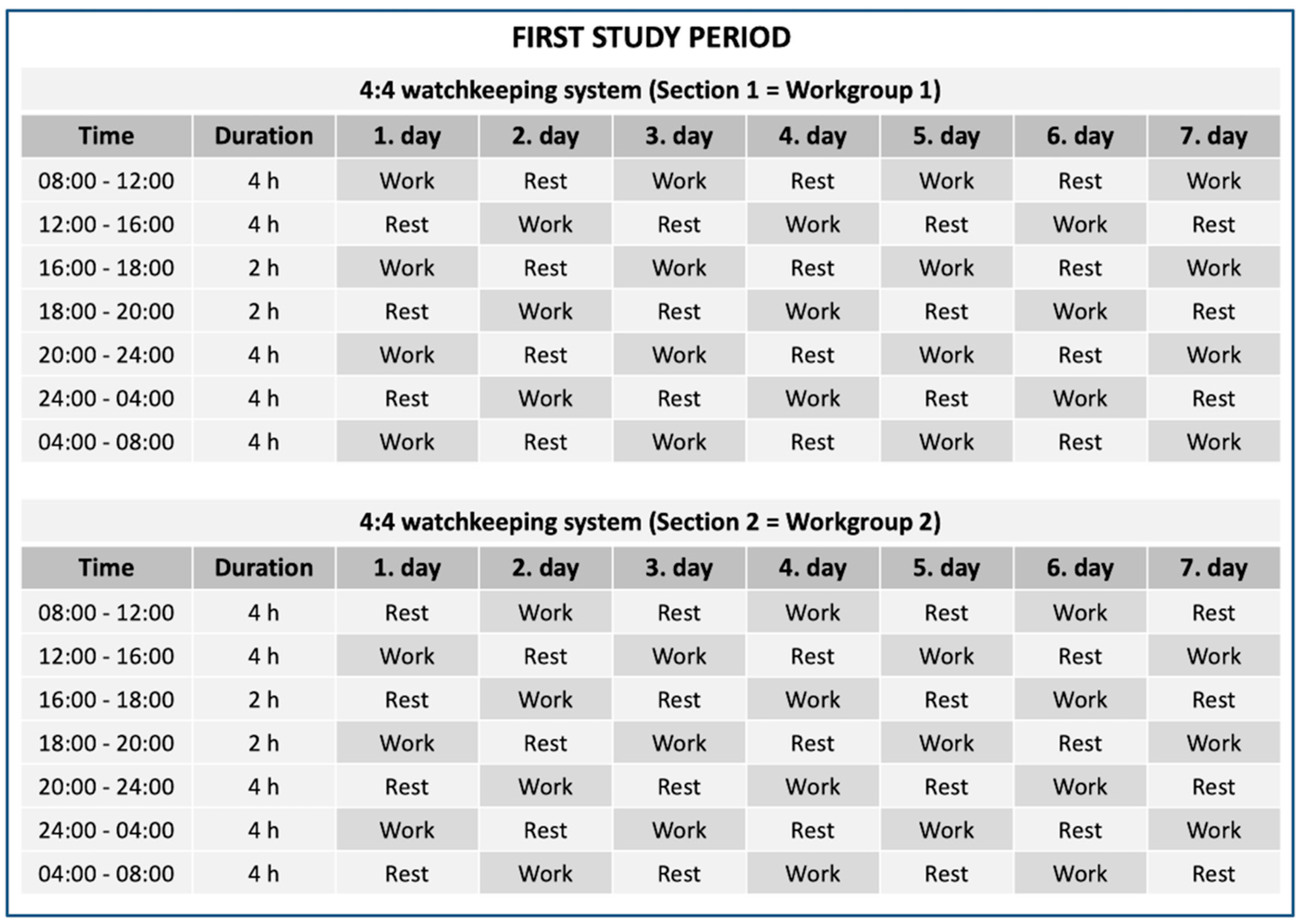
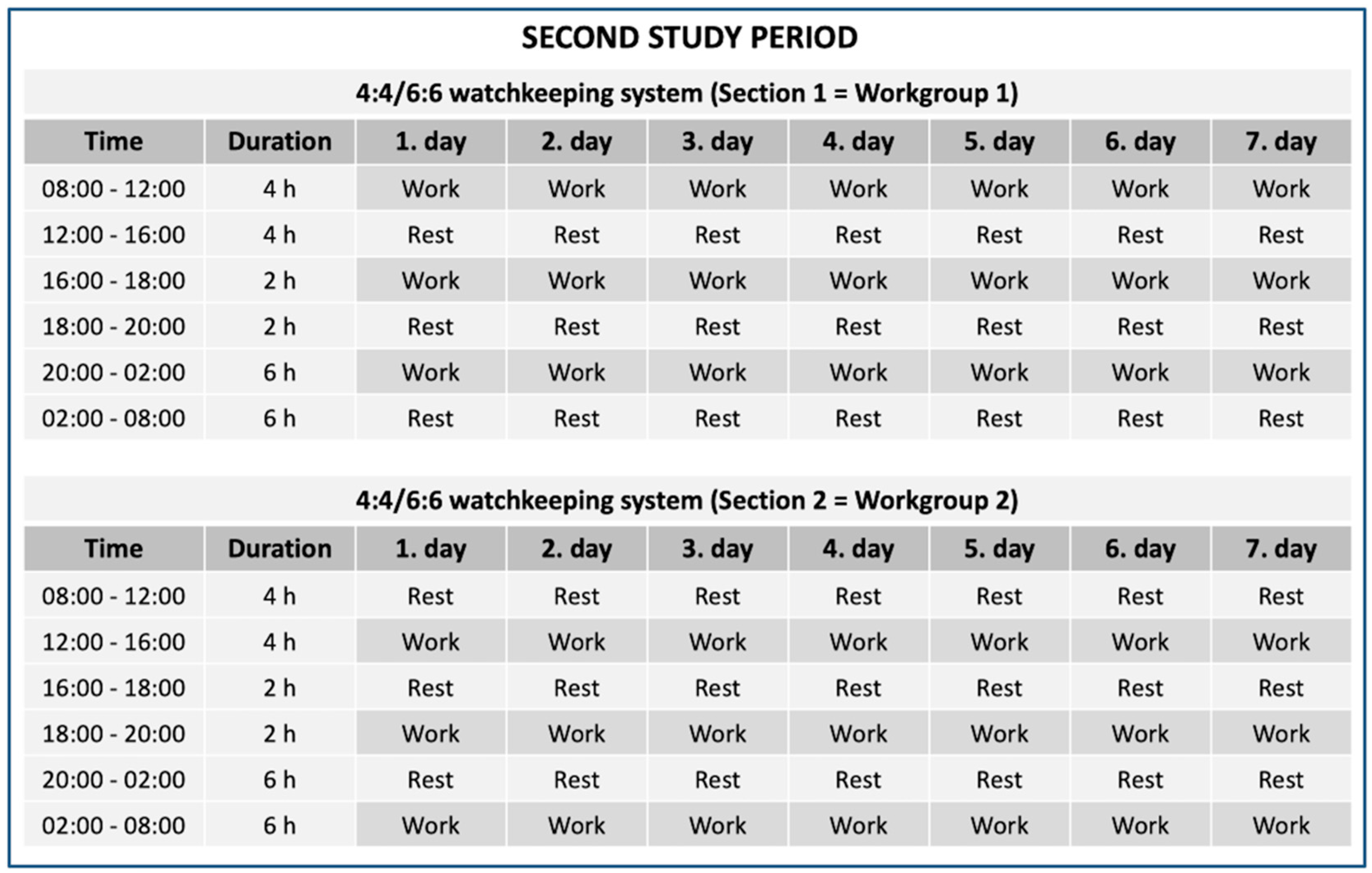
2.1. Study Design on Board
2.2. Participant Characteristics
2.3. Measurements on Board the Navy Missile Patrol Boat
2.3.1. The Karolinska Sleepiness Scale (KSS)
2.3.2. Salivary AA, Cor, IgA and DHEA
2.3.3. Orthostatic Test
2.3.4. Cognitive Tests (SART, N-Back)
2.3.5. Heart Rate Variability (HRV)
2.4. Statistics
3. Results
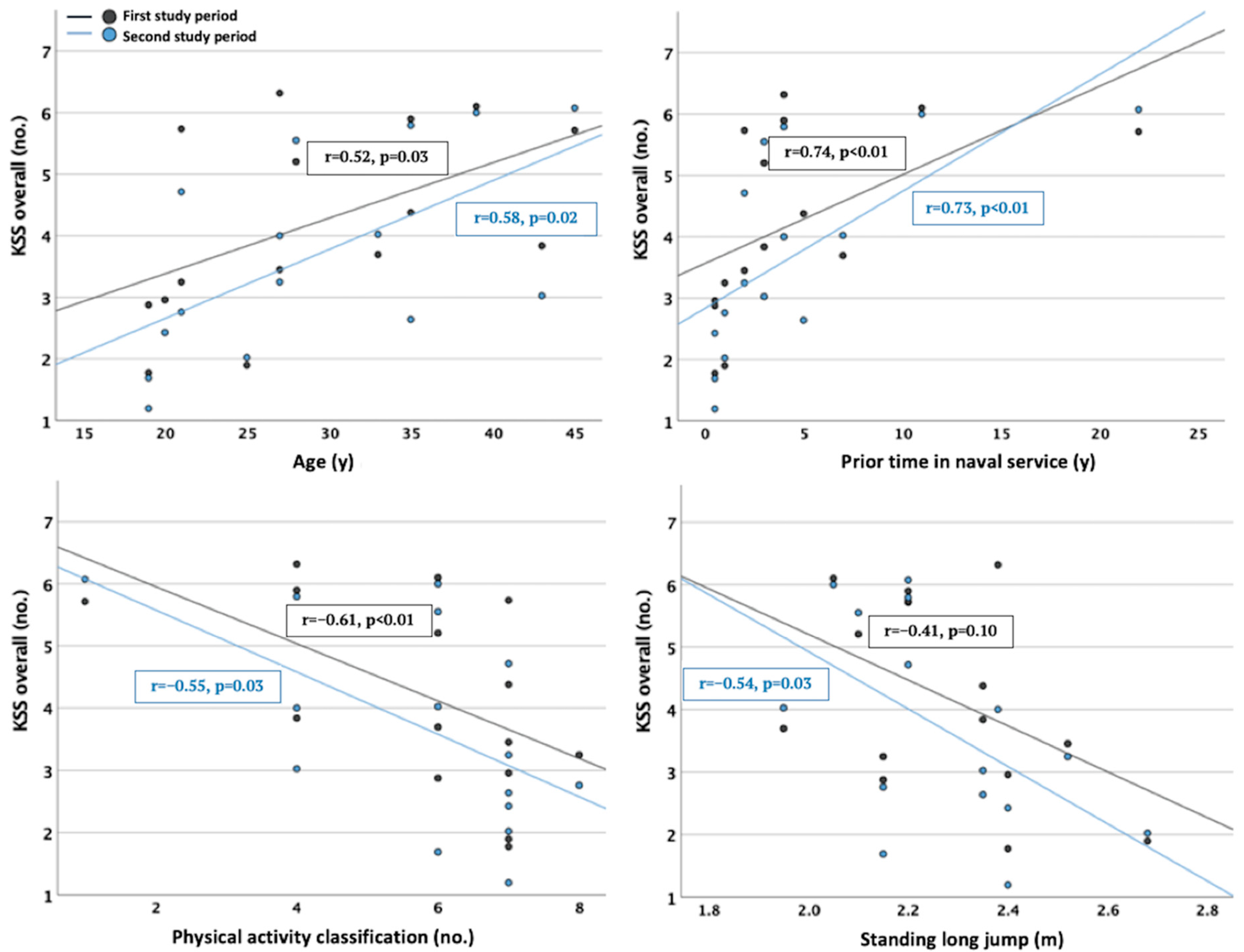
3.1. The Most Distinct Associations between Sleepiness, Fatigue, Stress Responses and Individual Characteristics
3.2. Associations regarding Physical Fitness and Body Composition
3.3. Associations regarding Blood Biomarkers
3.4. Associations regarding Psychological Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kyröläinen, H.; Häkkinen, K.; Kautiainen, H.; Santtila, M.; Pihlainen, K.; Häkkinen, A. Physical fitness, BMI and sickness absence in male military personnel. Occup. Med. 2008, 58, 251–256. [Google Scholar] [CrossRef]
- Middleton, K.J.; Carr, A.J. The identification of combat survivability tasks associated with naval vessel damage in maritime environments. Appl. Ergon. 2017, 59, 27–33. [Google Scholar] [CrossRef]
- Brown, P.; Fallowfield, J.L. Physical Employment Standards for UK Royal Navy Personnel: A Survey of Tasks That Require Muscle Strength and Endurance. Mil. Med. 2019, 184, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Bilzon, J.L.; Scarpello, E.G.; Smith, C.V.; Ravenhill, N.A.; Rayson, M.P. Characterization of the metabolic demands of simulated shipboard Royal Navy fire-fighting tasks. Ergonomics 2001, 44, 766–780. [Google Scholar] [CrossRef]
- Kettunen, O.; Kyröläinen, H.; Santtila, M.; Vasankari, T. Physical fitness and volume of leisure time physical activity relate with low stress and high mental resources in young men. J. Sports Med. Phys. Fitness 2014, 54, 545–551. [Google Scholar]
- Kettunen, O.; Kyröläinen, H.; Santtila, M.; Vuorimaa, T.; Vasankari, T.J. Greater levels of cardiorespiratory and muscular fitness are associated with low stress and high mental resources in normal but not overweight men. BMC Public Health 2016, 16, 788. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef] [PubMed]
- Teisala, T.; Mutikainen, S.; Tolvanen, A.; Rottensteiner, M.; Leskinen, T.; Kaprio, J.; Kolehmainen, M.; Rusko, H.; Kujala, U.M. Associations of physical activity, fitness, and body composition with heart rate variability-based indicators of stress and recovery on workdays: A cross-sectional study. J. Occup. Med. Toxicol. 2014, 9, 16. [Google Scholar] [CrossRef]
- Mujica-Parodi, L.R.; Renelique, R.; Taylor, M.K. Higher body fat percentage is associated with increased cortisol reactivity and impaired cognitive resilience in response to acute emotional stress. Int. J. Obes. 2009, 33, 157–165. [Google Scholar] [CrossRef]
- WHO Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 19 August 2022).
- Hoeyer, J.L.; Hansen, H.L. Obesity among Danish seafarers. Int. Marit. Health 2005, 56, 48–55. [Google Scholar]
- Hansen, H.L.; Hjarnoe, L.; Jepsen, J.R. Obesity continues to be a major health risk for Danish seafarers and fishermen. Int. Marit. Health 2011, 62, 98–103. [Google Scholar] [PubMed]
- Oldenburg, M.; Harth, V.; Jensen, H.J. Overview and prospect: Food and nutrition of seafarers on merchant ships. Int. Marit. Health 2013, 64, 191–194. [Google Scholar] [CrossRef] [PubMed]
- 2018 Department of Defense Health Related Behaviors Survey (HRBS). Available online: https://www.rand.org/pubs/research_reports/RR4222.html (accessed on 19 August 2022).
- Gregg, M.A.; Jankosky, C.J. Physical readiness and obesity among male U.S. Navy personnel with limited exercise availability while at sea. Mil. Med. 2012, 177, 1302–1307. [Google Scholar] [CrossRef]
- Sanden, S.; Johnsen, B.H.; Eid, J.; Sommerfelt-Pettersen, J.; Koefoed, V.; Størksen, R.; Røsseland, A.; Neteland, H.O.; Wetteland, P.I.; Wilhelmsen, E.V. Mental readiness for maritime international operation: Procedures developed by Norwegian navy. Int. Marit. Health 2014, 65, 93–97. [Google Scholar] [CrossRef][Green Version]
- Allen, P.; Wadsworth, E.; Smith, A. Seafarers’ fatigue: A review of the recent literature. Int. Marit. Health 2008, 59, 81–92. [Google Scholar] [PubMed]
- Wadsworth, E.J.; Allen, P.H.; McNamara, R.L.; Smith, A.P. Fatigue and health in a seafaring population. Occup. Med. 2008, 58, 198–204. [Google Scholar] [CrossRef]
- Roberts, S.E.; Jaremin, B.; Chalasani, P.; Rodgers, S.E. Suicides among seafarers in UK merchant shipping, 1919–2005. Occup. Med. 2010, 60, 54–61. [Google Scholar] [CrossRef][Green Version]
- Oldenburg, M.; Jensen, H.J.; Latza, U.; Baur, X. Seafaring stressors aboard merchant and passenger ships. Int. J. Public Health 2009, 54, 96–105. [Google Scholar] [CrossRef]
- Kenny, D.T.; Cooper, C.L. Introduction: Occupational stress and its management. Int. J. Stress Manag. 2003, 10, 275–279. [Google Scholar] [CrossRef]
- Ritonja, J.; Aronson, K.J.; Matthews, R.W.; Boivin, D.B.; Kantermann, T. Working Time Society consensus statements: Individual differences in shift work tolerance and recommendations for research and practice. Ind. Health 2019, 57, 201–212. [Google Scholar] [CrossRef] [PubMed]
- De la Fuente-Solana, E.I.; Suleiman-Martos, N.; Velando-Soriano, A.; Cañadas-De la Fuente, G.R.; Herrera-Cabrerizo, B.; Albendín-García, L. Predictors of burnout of health professionals in the departments of maternity and gynaecology, and its association with personality factors: A multicentre study. J. Clin. Nurs. 2021, 30, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Strahler, J.; Mueller, A.; Rosenloecher, F.; Kirschbaum, C.; Rohleder, N. Salivary alpha-amylase stress reactivity across different age groups. Psychophysiology 2010, 47, 587–595. [Google Scholar] [CrossRef]
- Hellhammer, D.H.; Wüst, S.; Kudielka, B.M. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 2009, 34, 163–171. [Google Scholar] [CrossRef]
- Afrisham, R.; Aberomand, M.; Soliemanifar, O.; Kooti, W.; Ashtary-Larky, D.; Alamiri, F.; Najjar-Asl, S.; Khaneh-Keshi, A.; Sadegh-Nejadi, S. Levels of salivary immunoglobulin A under psychological stress and its relationship with rumination and five personality traits in medical students. Eur. J. Psychiat. 2016, 30, 41–53. [Google Scholar]
- Izawa, S.; Sugaya, N.; Shirotsuki, K.; Yamada, K.C.; Ogawa, N.; Ouchi, Y.; Nagano, Y.; Suzuki, K.; Nomura, S. Salivary dehydroepiandrosterone secretion in response to acute psychosocial stress and its correlations with biological and psychological changes. Biol. Psychol. 2008, 79, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Deinzer, R.; Kleineidam, C.; Stiller-Winkler, R.; Idel, H.; Bachg, D. Prolonged reduction of salivary immunoglobulin A (sIgA) after a major academic exam. Int. J. Psychophysiol. 2000, 37, 219–232. [Google Scholar] [CrossRef]
- Jemmott, J.B.; Magloire, K. Academic stress, social support, and secretory immunoglobulin A. J. Pers. Soc. Psychol. 1988, 55, 803. [Google Scholar] [CrossRef] [PubMed]
- Lowe, G.; Urquhart, J.; Greenman, J.; Lowe, G. Academic stress and secretory immunoglobulin A. Psychol. Rep. 2000, 87, 721–722. [Google Scholar] [CrossRef]
- Kim, H.G.; Cheon, E.J.; Bai, D.S.; Lee, Y.H.; Koo, B.H. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef]
- Vrijkotte, T.G.; van Doornen, L.J.; de Geus, E.J. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension 2000, 35, 880–886. [Google Scholar] [CrossRef]
- Hynynen, E.; Konttinen, N.; Kinnunen, U.; Kyröläinen, H.; Rusko, H. The incidence of stress symptoms and heart rate variability during sleep and orthostatic test. Eur. J. Appl. Physiol. 2011, 111, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Shattuck, N.L.; Matsangas, P. Psychomotor vigilance performance predicted by Epworth Sleepiness Scale scores in an operational setting with the United States Navy. J. Sleep Res. 2015, 24, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Matsangas, P.; Shattuck, N.L. Sleep quality, occupational factors, and psychomotor vigilance performance in the U.S. Navy sailors. Sleep 2020, 43, zsaa118. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Boros, S. The effect of physical activity on sleep quality: A systematic review. Eur. J. Physiother. 2021, 23, 11–18. [Google Scholar] [CrossRef]
- Hulsegge, G.; Loef, B.; van Kerkhof, L.W.; Roenneberg, T.; van der Beek, A.J.; Proper, K.I. Shift work, sleep disturbances and social jetlag in healthcare workers. J. Sleep Res. 2019, 28, e12802. [Google Scholar] [CrossRef]
- Reinberg, A.; Ashkenazi, I. Internal desynchronization of circadian rhythms and tolerance to shift work. Chronobiol. Int. 2008, 25, 625–643. [Google Scholar] [CrossRef]
- Gander, P.; O’Keeffe, K.; Santos-Fernandez, E.; Huntington, A.; Walker, L.; Willis, J. Fatigue and nurses’ work patterns: An online questionnaire survey. Int. J. Nurs. Stud. 2019, 98, 67–74. [Google Scholar] [CrossRef]
- Härmä, M.; Hakola, T.; Kandolin, I.; Sallinen, M.; Virkkala, J.; Bonnefond, A.; Mutanen, P. A controlled intervention study on the effects of a very rapidly forward rotating shift system on sleep-wakefulness and well-being among young and elderly shift workers. Int. J. Psychophysiol. 2006, 59, 70–79. [Google Scholar] [CrossRef]
- Arulanandam, S.; Tsing, G.C. Comparison of alertness levels in ship crew. An experiment on rotating versus fixed watch schedules. Int. Marit. Health 2009, 60, 6–9. [Google Scholar]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef]
- Akerstedt, T.; Knutsson, A.; Westerholm, P.; Theorell, T.; Alfredsson, L.; Kecklund, G. Mental fatigue, work and sleep. J. Psychosom. Res. 2004, 57, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Kaida, K.; Takahashi, M.; Akerstedt, T.; Nakata, A.; Otsuka, Y.; Haratani, T.; Fukasawa, K. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin. Neurophysiol. 2006, 117, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Lutzhoft, M.; Dahlgren, A.; Kircher, A.; Thorslund, B.; Gillberg, M. Fatigue at sea in Swedish shipping: A field study. Am. J. Ind. Med. 2010, 53, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Robertson, I.H.; Manly, T.; Andrade, J.; Baddeley, B.T.; Yiend, J. ‘Oops!’: Performance correlates of everyday attentional failures in traumatic brain injured and normal subjects. Neuropsychologia 1997, 35, 747–758. [Google Scholar] [CrossRef]
- Jaeggi, S.M.; Buschkuehl, M.; Perrig, W.J.; Meier, B. The concurrent validity of the N-back task as a working memory measure. Memory 2010, 18, 394–412. [Google Scholar] [CrossRef]
- Konstabel, K.; Lönnqvist, J.E.; Walkowitz, G.; Konstabel, K.; Verkasalo, M. The ‘Short Five’ (S5): Measuring personality traits using comprehensive single items. Eur. J. Personal. 2012, 26, 13–29. [Google Scholar] [CrossRef]
- Losoi, H.; Turunen, S.; Wäljas, M.; Helminen, M.; Öhman, J.; Julkunen, J.; Rosti-Otajärvi, E. Psychometric Properties of the Finnish Version of the Resilience Scale and its Short Version. Psychol. Community Health 2013, 2, 1–10. [Google Scholar] [CrossRef]
- Myllylä, M.; Kyröläinen, H.; Ojanen, T.; Ruohola, J.P.; Heinonen, O.J.; Vahlberg, T.; Parkkola, K.I. Effects of operational assessment of the 4:4 and 4:4/6:6 watch systems on sleepiness, fatigue, and stress responses during patrolling on a navy missile patrol boat. Chronobiol. Int. 2022, 39, 1233–1241. [Google Scholar] [CrossRef]
- Bourdillon, N.; Schmitt, L.; Yazdani, S.; Vesin, J.M.; Millet, G.P. Minimal Window Duration for Accurate HRV Recording in Athletes. Front. Neurosci. 2017, 11, 456. [Google Scholar] [CrossRef]
- Axelrod, S.; Lishner, M.; Oz, O.; Bernheim, J.; Ravid, M. Spectral analysis of fluctuations in heart rate: An objective evaluation of autonomic nervous control in chronic renal failure. Nephron 1987, 45, 202–206. [Google Scholar] [CrossRef]
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front. Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef] [PubMed]
- Härmä, M.; Ilmarinen, J.; Knauth, P.; Rutenfranz, J.; Hänninen, O. Physical training intervention in female shift workers: I. The effects of intervention on fitness, fatigue, sleep, and psychosomatic symptoms. Ergonomics 1988, 31, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Park, S.M. Association of muscle mass and fat mass with insulin resistance and the prevalence of metabolic syndrome in Korean adults: A cross-sectional study. Sci. Rep. 2018, 8, 2703. [Google Scholar] [CrossRef] [PubMed]
- Nykänen, T.; Pihlainen, K.; Kyröläinen, H.; Fogelholm, M. Associations of nutrition and body composition with cardiovascular disease risk factors in soldiers during a 6-month deployment. Int. J. Occup. Med. Environ. Health 2020, 33, 457–466. [Google Scholar] [CrossRef]
- Mudali, S.; Dobs, A.S. Effects of testosterone on body composition of the aging male. Mech. Ageing Dev. 2004, 125, 297–304. [Google Scholar] [CrossRef]
- Crichton, G.E.; Elias, M.F.; Davey, A.; Sullivan, K.J.; Robbins, M.A. Higher HDL cholesterol is associated with better cognitive function: The Maine-Syracuse study. J. Int. Neuropsychol. Soc. 2014, 20, 961–970. [Google Scholar] [CrossRef]
- Jackson, J.J.; Thoemmes, F.; Jonkmann, K.; Lüdtke, O.; Trautwein, U. Military training and personality trait development: Does the military make the man, or does the man make the military? Psychol. Sci. 2012, 23, 270–277. [Google Scholar] [CrossRef]
| FIRST STUDY PERIOD | SECOND STUDY PERIOD | |||||
|---|---|---|---|---|---|---|
| n | Range | Mean (SD) | n | Range | Mean (SD) | |
| Age (y) | 17 | 19–45 | 29 (8) | 16 | 19–45 | 29 (9) |
| Prior time in naval service (y) | 17 | 0.5–22.0 | 4.2 (5.4) | 16 | 0.5–22.0 | 4.8 (5.6) |
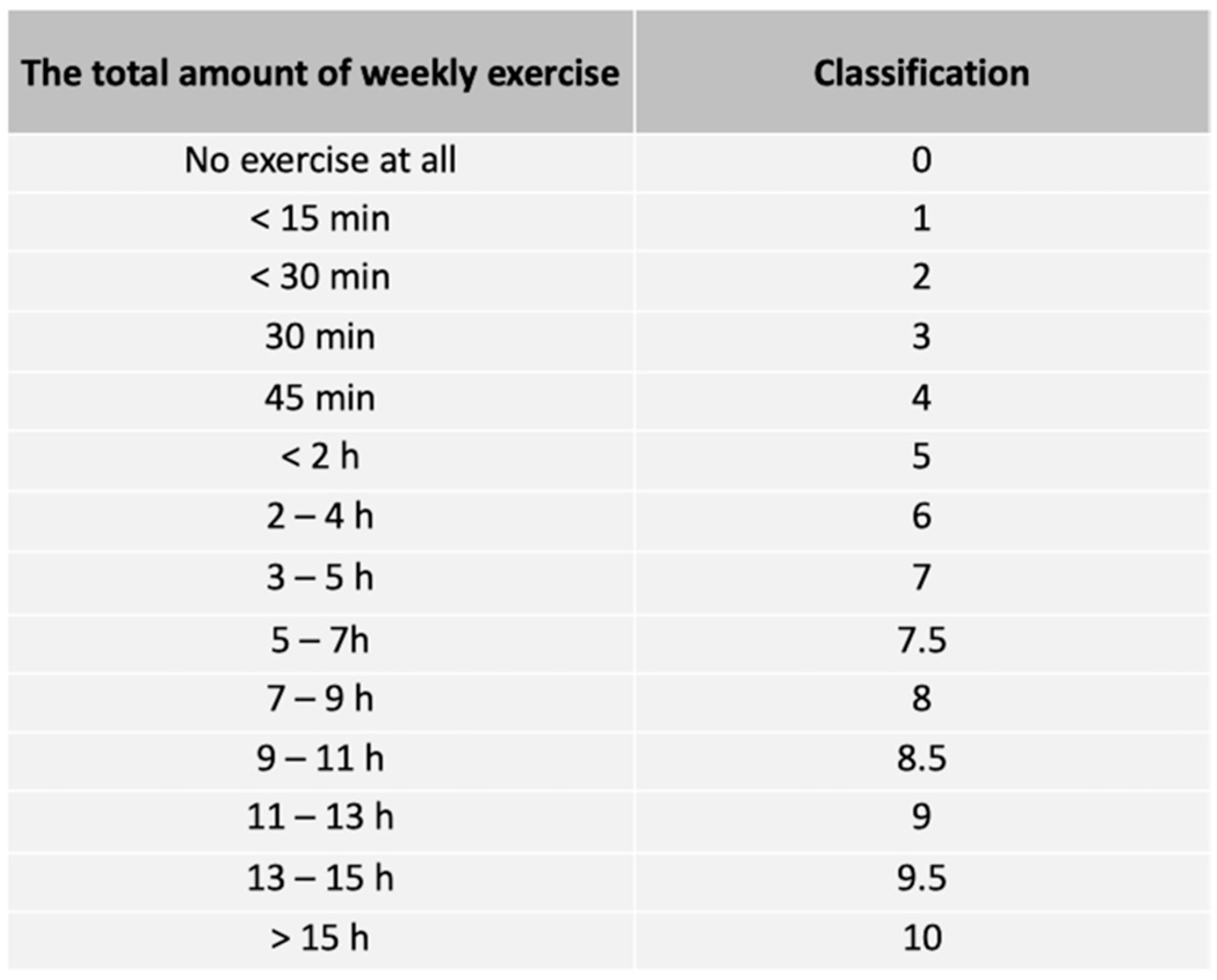
| Physical activity classification (no.) | 17 | 1–8 | 6 (2) | 16 | 1–8 | 6 (2) |
| Body composition | ||||||
| Height (m) | 16 | 1.65–1.87 | 1.79 (0.05) | 15 | 1.65–1.87 | 1.80 (0.05) |
| Body mass (kg) | 16 | 62.8–102.1 | 82.8 (8.7) | 15 | 62.8–102.1 | 83.8 (8.4) |
| Body mass index (kg/m2) | 16 | 19.9–32.0 | 25.9 (3.0) | 15 | 19.9–32.0 | 25.9 (3.0) |
| Body fat percentage (%) | 16 | 7.7–34.4 | 20.0 (6.8) | 15 | 7.7–34.4 | 20.3 (7.0) |
| Skeletal muscle mass (kg) | 16 | 32.8–42.8 | 37.5 (3.1) | 15 | 32.8–42.8 | 37.7 (3.0) |
| Fat mass (kg) | 16 | 4.8–31.2 | 16.9 (6.9) | 15 | 4.8–31.2 | 17.4 (7.1) |
| Waist circumference (cm) | 11 | 67–113 | 91 (12) | 12 | 67–113 | 91 (11) |
| Physical fitness | ||||||
| Push-ups (reps/min) | 17 | 22–68 | 41 (11) | 16 | 22–68 | 40 (11) |
| Sit-ups (reps/min) | 17 | 22–62 | 45 (10) | 16 | 22–62 | 44 (10) |
| Standing long jump (m) | 17 | 1.95–2.68 | 2.29 (0.19) | 16 | 1.95–2.68 | 2.29 (0.19) |
| 12-min run test (m) | 17 | 2030–3010 | 2628 (293) | 16 | 2030–3010 | 2634 (277) |
| MVCupper (kg) | 11 | 84–124 | 106 (11) | 12 | 81–124 | 104 (12) |
| MVClower (kg) | 11 | 323–531 | 444 (59) | 12 | 292–531 | 432 (71) |
| SMBT (m) | 11 | 5.10–8.02 | 6.57 (0.80) | 12 | 5.10–8.02 | 6.50 (0.80) |
| Blood biomarkers | ||||||
| FPG (mmol/l) | 11 | 5.2–6.1 | 5.5 (0.2) | 12 | 5.0–6.1 | 5.5 (0.3) |
| FPI (mU/l) | 11 | 5.0–17.0 | 8.3 (4.0) | 12 | 5.0–17.0 | 8.5 (3.9) |
| HbA1c (mmol/mol) | 11 | 29.0–36.0 | 31.9 (2.0) | 12 | 29.0–36.0 | 32.2 (2.0) |
| TC (mmol/l) | 11 | 3.2–6.3 | 4.8 (0.9) | 12 | 3.2–6.3 | 4.8 (0.9) |
| LDL-C (mmol/l) | 11 | 1.2–4.6 | 3.0 (0.9) | 12 | 1.2–4.6 | 3.0 (0.9) |
| HDL-C (mmol/l) | 11 | 1.1–2.0 | 1.5 (0.3) | 12 | 1.1–2.0 | 1.5 (0.3) |
| TES (nmol/l) | 11 | 8.7–24.0 | 15.7 (4.8) | 12 | 8.7–24.0 | 15.4 (4.7) |
| IGF-1 (nmol/l) | 11 | 11.2–23.8 | 18.0 (4.2) | 12 | 11.2–23.8 | 18.2 (4.1) |
| Psychological factors | ||||||
| S5: Extraversion (no.) | 11 | −12–12 | 3 (10) | 11 | −21–12 | 1 (11) |
| S5: Neuroticism (no.) | 11 | −31–3 | −17 (10) | 11 | −29–3 | −15 (9) |
| S5: Openness (no.) | 11 | −6–31 | 10 (12) | 11 | −6–31 | 11 (11) |
| S5: Agreeableness (no.) | 11 | −4–26 | 12 (10) | 11 | −4–26 | 11 (10) |
| S5: Conscientiousness (no.) | 11 | 4–32 | 19 (9) | 11 | 4–27 | 17 (8) |
| RS14 (no.) | 11 | 62–95 | 79 (11) | 11 | 62–94 | 77 (9) |
| Before measurement periods | ||||||
| Sleep/day, last 3 days (h) | 16 | 5.5–8.0 | 7.0 (0.7) | 15 | 6.0–8.8 | 7.5 (0.7) |
| Sleep/day, last 1 day (h) | 16 | 6.5–9.0 | 7.4 (0.7) | 15 | 5.0–10.0 | 7.0 (0.8) |
| FIRST STUDY PERIOD | SECOND STUDY PERIOD | ||||
|---|---|---|---|---|---|
| KSS | sAA, sCOR, sIgA, sDHEA | HRV | KSS | HRV | |
| Age | •KSS (overall) r = 0.52 * •KSS (02–04 h) r = 0.54 * | •sDHEA r = 0.55 * °sAA r = −0.52 * | •LF(SU) r = −0.59 * | •KSS (overall) r = 0.58 * •KSS (16–18 h) r = 0.58 * •KSS (02–04 h) r = 0.50 * | - |
| Prior time in naval service | •KSS (overall) r = 0.74 ** •KSS (16–18 h) r = 0.71 ** •KSS (02–04 h) r = 0.70 ** | •sDHEA r = 0.61 ** | •SDNN(ST) r = −0.60 * •TP(ST) r = −0.55 * | •KSS (overall) r = 0.73 ** •KSS (16–18 h) r = 0.67 ** •KSS (02–04 h) r = 0.65 ** | •LF/FH(SU) r = 0.56 * |
| Physical activity classification | °KSS (overall) r = −0.61 ** °KSS (16–18 h) r = −0.56 * °KSS (02–04 h) r = −0.61 ** | - | - | °KSS (overall) r = −0.55 * °KSS (16–18 h) r = −0.54 * | °LF/HF(SU) r = −0.69 ** |
| Standing long jump | °KSS (16–18 h) r = −0.48 * | - | °SDNN(ST) r = 0.55 * | °KSS (overall) r = −0.54 * °KSS (16–18 h) r = −0.61 * | °HRmean(ST) r = −0.55 * °RMSSD(ST) r = 0.65 ** |
| FIRST STUDY PERIOD | SECOND STUDY PERIOD | |||||
|---|---|---|---|---|---|---|
| sAA, sCOR, sIgA, sDHEA | SART, N-Back | HRV | sAA, sCOR, sIgA, sDHEA | SART, N-Back | HRV | |
| Push-ups | - | - | - | °sCOR r = −0.55 * | - | - |
| Sit-ups | - | - | - | - | °SART RT r = −0.52 * | - |
| MVCupper | °sAA r = −0.75 ** | - | - | - | - | °LF/HF (SU) r = −0.67 * |
| MVClower | - | °SART Errors r = −0.63 * °SART RT r = −0.65 * | - | - | - | - |
| SMBT | - | - | - | - | °SART RT r = −0.63 * | - |
| 12-min run test | - | - | •LF (ST) r = −0.64 * | - | °SART RT r = −0.56 * | - |
| BMI | - | - | •TP (SU) r = −0.62 * | - | - | - |
| WC | - | •N-Back Total hits r = −0.66 * | •LF (SU) r = −0.77 ** •TP (SU) r = −0.83 ** | - | - | - |
| BFP | - | - | •LF (SU) r = −0.78 ** •TP (SU) r = −0.75 ** | - | - | - |
| FATM | - | - | •LF (SU) r = −0.81 ** •TP (SU) r = −0.74 ** | - | - | °TP (SU) r = 0.55 * |
| SMM | - | - | - | •sAA r = 0.63 * | °N-Back Total hits r = 0.56 * | - |
| FIRST STUDY PERIOD | SECOND STUDY PERIOD | |||||
|---|---|---|---|---|---|---|
| sAA, sCOR, sIgA, sDHEA | SART, N-Back | HRV | sAA, sCOR, sIgA, sDHEA | SART, N-Back | HRV | |
| FPG | - | •N-Back Total hits r = −0.63 * | •LF (SU) r = −0.80 ** •TP (SU) r = −0.91 ** •SDNN (ST) r = −0.72 * •RMSSD (ST) r = −0.71 * | •sCOR r = 0.59 * | - | - |
| FPI | •sAA r = 0.71 * | - | •RMSSD (SU) r = −0.68 * •HF (SU) r = −0.73 * •TP (SU) r = −0.75 * | - | - | - |
| HbA1c | - | - | - | - | - | •LF/HF (SU) r = 0.58 * |
| TC | - | - | - | - | - | •LF (ST) r = −0.67 * |
| LDL-C | - | - | - | - | - | •LF (ST) r = −0.59 * •LF/HF (ST) r = 0.68 * |
| HDL-C | - | °SART Errors r = −0.66 * °SART RT r = −0.64 * | - | - | °N-Back Total hits r = 0.60 * | °HRmean (ST) r = −0.63 * °LF (ST) r = 0.61 * |
| TES | - | °SART Errors r = −0.81 ** °SART RT r = −0.77 ** | °HF (SU) r = 0.64 * °LF/HF (ST) r= −0.78 * | - | - | °SDNN (SU) r = 0.67 * °RMSSD ( SU) r = 0.65 * |
| IGF-1 | - | - | - | - | - | °LF/HF (SU) r = −0.69 * |
| FIRST STUDY PERIOD | SECOND STUDY PERIOD | ||||
|---|---|---|---|---|---|
| KSS | HRV | sAA, sCOR, sIgA, sDHEA | SART, N-Back | HRV | |
| S5: Extraversion | °KSS (16–18 h) r = −0.60 * | - | - | - | - |
| S5: Neuroticism | - | - | - | - | °SDNN(SU) r = 0.87 ** °RMSSD(SU) r = 0.87 ** °LF(SU) r = 0.68 * |
| S5: Openness | - | - | - | °SART RT r = −0.64 * | °LF/HF(ST) r = −0.68 * |
| S5: Agreeableness | - | °LF (SU) r = 0.72 * | °sCOR r = −0.62 * | •N-Back Errors r = 0.61 * | - |
| RS14 | - | •LF/FH (SU) r = 0.68 * | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myllylä, M.; Kyröläinen, H.; Ojanen, T.; Ruohola, J.-P.; Heinonen, O.J.; Simola, P.; Vahlberg, T.; Parkkola, K.I. The Effects of Individual Characteristics of the Naval Personnel on Sleepiness and Stress during Two Different Watchkeeping Schedules. Int. J. Environ. Res. Public Health 2022, 19, 13451. https://doi.org/10.3390/ijerph192013451
Myllylä M, Kyröläinen H, Ojanen T, Ruohola J-P, Heinonen OJ, Simola P, Vahlberg T, Parkkola KI. The Effects of Individual Characteristics of the Naval Personnel on Sleepiness and Stress during Two Different Watchkeeping Schedules. International Journal of Environmental Research and Public Health. 2022; 19(20):13451. https://doi.org/10.3390/ijerph192013451
Chicago/Turabian StyleMyllylä, Mikko, Heikki Kyröläinen, Tommi Ojanen, Juha-Petri Ruohola, Olli J. Heinonen, Petteri Simola, Tero Vahlberg, and Kai I. Parkkola. 2022. "The Effects of Individual Characteristics of the Naval Personnel on Sleepiness and Stress during Two Different Watchkeeping Schedules" International Journal of Environmental Research and Public Health 19, no. 20: 13451. https://doi.org/10.3390/ijerph192013451
APA StyleMyllylä, M., Kyröläinen, H., Ojanen, T., Ruohola, J.-P., Heinonen, O. J., Simola, P., Vahlberg, T., & Parkkola, K. I. (2022). The Effects of Individual Characteristics of the Naval Personnel on Sleepiness and Stress during Two Different Watchkeeping Schedules. International Journal of Environmental Research and Public Health, 19(20), 13451. https://doi.org/10.3390/ijerph192013451





