Effect of Nucleic Acid Screening Measures on COVID-19 Transmission in Cities of Different Scales and Assessment of Related Testing Resource Demands—Evidence from China
Abstract
1. Introduction
2. Materials and Methods
2.1. Concept Definition
2.2. Model Building Assumptions
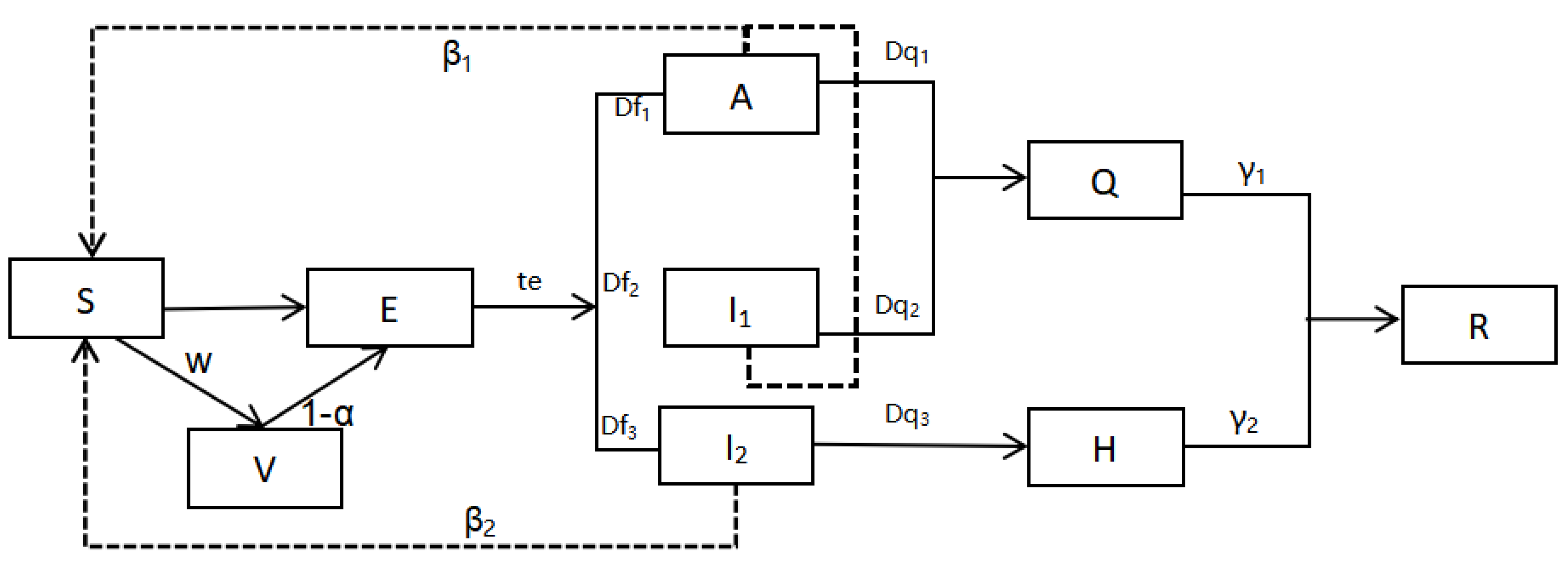
2.3. Epidemiological Model
2.4. Scenario Construction
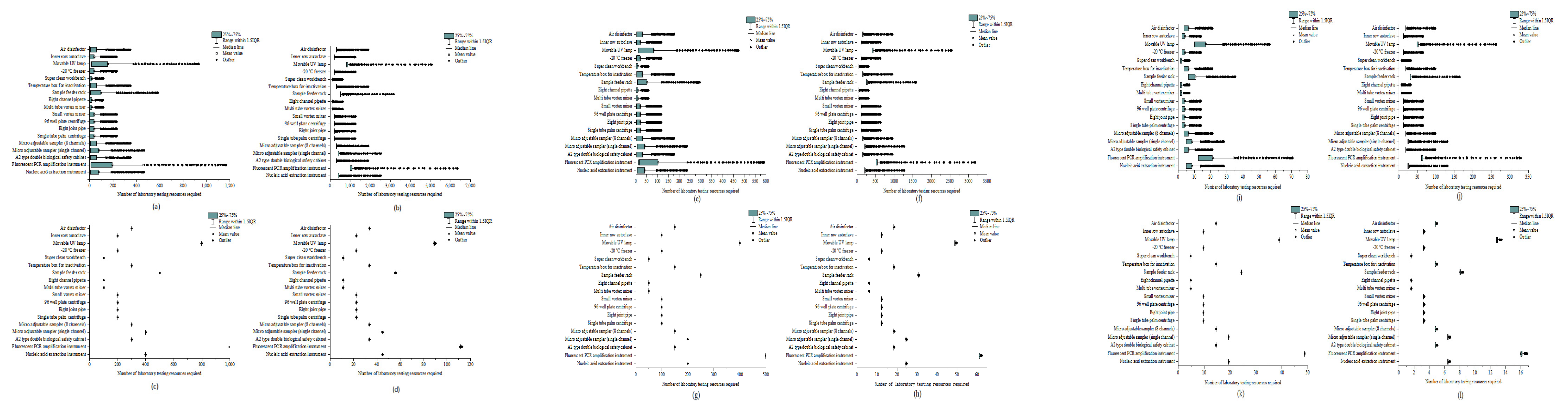
2.5. Laboratory Testing Related Resource Parameters
2.6. Model Validation
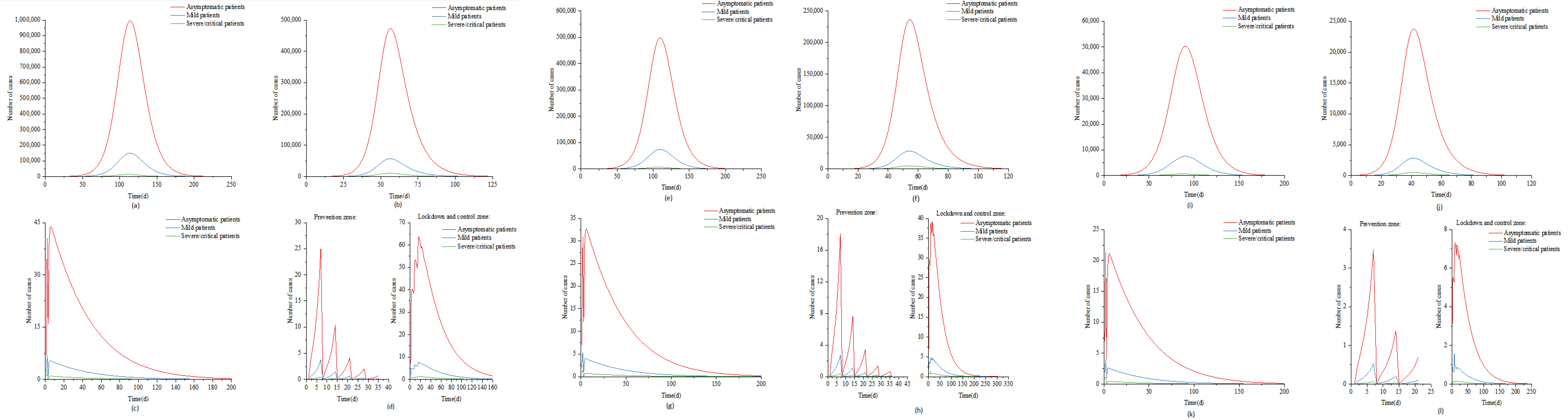
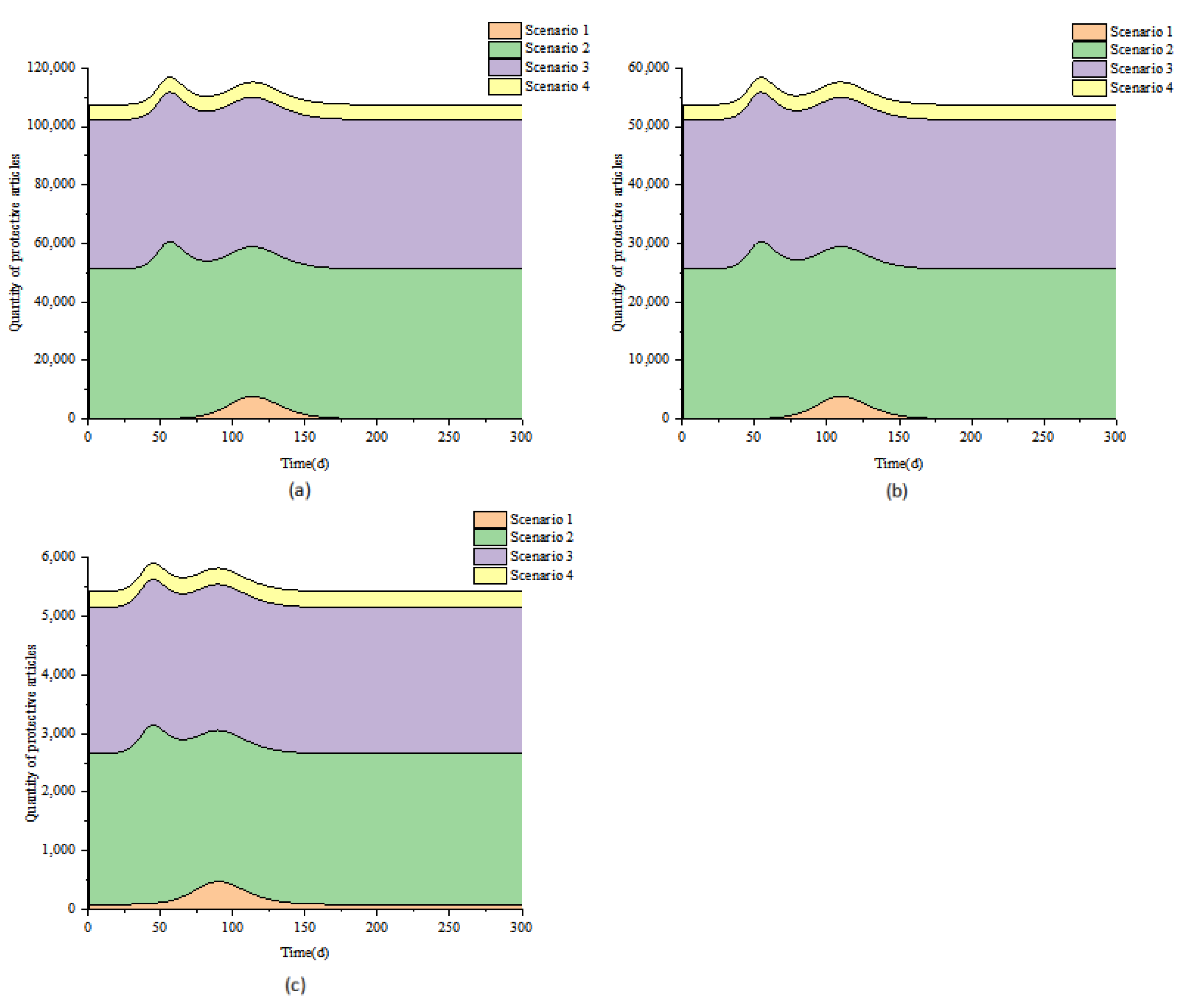
3. Results
3.1. Scenario 1
3.2. Scenario 2
3.3. Scenario 3
3.4. Scenario 4
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baidu. Real-Time Big Data Report on COVID-19 Outbreak. 15 April 2022. Available online: https://voice.baidu.com/act/newpneumonia/newpneumonia/?from=osari_pc_3 (accessed on 14 August 2022).
- Liu, M.Y.; Qi, F.F.; Bao, L.L. Research progress of vaccines against SARS-CoV-2 variant Omicron. Adv. Biochem. Biophys. 2022, 49, 7. [Google Scholar]
- Dergaa, I.; Abdelrahman, H.J.; Varma, A.; Yousfi, N.; Souissi, A.; Ghram, A.; Hammad, A.S.; Mus, E.; Taheri, M.; Irandoust, K.; et al. COVID-19 Vaccination, Herd Immunity and The Transition Toward Normalcy: Challenges with The Upcoming Sports Events. Ann. Appl. Sport Sci. 2021, 9, e1032. [Google Scholar] [CrossRef]
- Simonsson, O.; Flodin, P.; Sidorchuk, A.; Marchetti, L.; Awil, F.; Castro, R.; Niemi, M.E. Effects of the COVID-19 pandemic and previous pandemics, epidemics and economic crises on mental health: A systematic review. BJPsych Open 2022, 8, e181. [Google Scholar]
- He, C.Y.; Wen, Y.C.; Chang, Y.L.; Geng, X.X. Measurement and Analysis of the COVID-19 Epidemic Impact on China’s Economy. J. Quant. Tech. Econ. 2020, 37, 3–22. [Google Scholar]
- Bastiampillai, T.; Allison, S.; Looi, J.C.L.; Licinio, J.; Wong, M.L.; Perry, S.W. The COVID-19 pandemic and epidemiologic insights from recession-related suicide mortality. Mol. Psychiatry 2020, 25, 3445–3447. [Google Scholar] [CrossRef]
- Hubei CDC. Personnel Health Management Measures in Key Domestic Areas. 10 August 2022. Available online: www.hbgstv.com/p/58578.html (accessed on 14 August 2022).
- Yao, S.T.; He, Z.Q.; Xu, S.J.; Gao, Y.D.; Yang, Y.C.; Dong, Z.L.; Li, Y.L.; Li, L.; Han, J.Z. Investigation and Analysis of a School Cluster Epidemic of COVID-19 in Longchuan County, Yunnan Province. Shanghai Prev. Med. 2022, 30, 1–6. [Google Scholar]
- Sun, Z.; Chen, J.F.; Liu, M.W.; Kao, Q.J.; Kong, Q.X. Epidemiological characteristics of 42 clustered outbreaks of COVID-19 in Hangzhou. Shanghai Prev. Med. 2022, 34, 265–267. [Google Scholar]
- Hu, M.; Yue, Y.; Wang, L.; Du, X.B.; Feng, J.; Cheng, Y.; Chi, X.L. Analysis of the first local clustered epidemic caused by the COVID-19 Omicron variant in Chengdu. Chin. J. Prev. Med. 2022, 23, 346–350. [Google Scholar]
- Gong, X.H.; Mao, S.H.; Kong, D.C.; Xiao, W.J.; Zheng, Y.X.; Zhu, Y.Y.; Lin, S.; Yu, X.; Cui, P.; Jiang, X.J.; et al. Epidemiological investigation on a cluster of COVID-19 in a public place in Shanghai. Chin. Public Health 2021, 37, 1071–1076. [Google Scholar]
- Wang, H.B.; Zhang, W.Z.; Meng, T.Y. Investigation and Analysis of a COVID-19 Family Cluster Epidemic in a District of Beijing. Cap. Public Health 2022, 16, 188–191. [Google Scholar]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Respiratory Branch of Chinese Medical Association, Chinese Medical Doctor Association Respiratory Physician Branch. Guidelines for the diagnosis, treatment and prevention of 2019-nCoV in Chinese adults. Chin. Med. J. 2021, 101, 1293–1356. [Google Scholar]
- Willan, J.; King, A.J.; Jeffery, K.; Bienz, N. Challenges for NHS hospitals during COVID-19 epidemic. BMJ. 2020, 368, m1117. [Google Scholar] [CrossRef]
- Fallucchi, F.; Faravelli, M.; Quercia, S. Fair allocation of scarce medical resources inthe time of COVID-19: What do people think? J. Med. Ethics 2020, 47, 3–6. [Google Scholar] [CrossRef]
- Weng, F.; Yao, H.S. Discussion on the Rationality of the Calculation Standard of the Demand for Medical Protective Materials During the Prevention and Control of COVID-19. China Med. Devices 2021, 36, 142–145. [Google Scholar]
- Hong, H.; Shi, H.B.; Jiang, H.B.; Gu, X.M.; Chen, Y.; Ding, K.Q.; Xu, G.Z. Effectiveness evaluation of COVID-19 prevention and control measures in Ningbo based on infectious disease dynamics model. Chin. J. Epidemiol. 2020, 41, 1606–1610. [Google Scholar]
- Wei, Y.Y.; Guan, J.X.; Zhao, Y.; Shen, S.P.; Chen, F. SEIR dynamic model assists in tracing the origin of the spread of COVID-19 in Xinfadi, Beijing and evaluating the effect of prevention and control. Chin. J. Epidemiol. 2020, 41, 1772–1776. [Google Scholar]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 395, 689–697. [Google Scholar] [CrossRef]
- Rainisch, G.; Undurraga, E.A.; Chowell, G. A dynamic modeling tool for estimating healthcare demand from the COVID-19 epidemic and evaluating population-wide interventions. Int. J. Infect. Dis. 2020, 96, 376–383. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, T.; Yang, Y.; Chen, F.Y.; Dai, P.X.; Jia, M.M.; Leng, Z.W.; Ma, L.B.; Yang, J.; Qi, W.R.; et al. Assessment of Laboratory Testing and Preventive Control Resource Needs for the COVID-19 Pandemic. Chin. J. Epidemiol. 2021, 42, 983–991. [Google Scholar]
- Ryu, S.; Gao, H.; Wong, J.Y.; Shiu, E.Y.C.; Xiao, J.; Fong, M.W.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings International Travel-Related Measures. Emerg. Infect. Dis. 2020, 26, 961–966. [Google Scholar] [CrossRef]
- Xiao, J.; Shiu, E.Y.; Gao, H.Z.; Wong, J.Y.; Fong, M.W.; Ryu, S.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings Personal Protective and Environmental Measures. Emerg. Infect. Dis. 2020, 26, 967–975. [Google Scholar] [CrossRef]
- Aleta, A.; David, M.C.; Piontti, A.P.Y.; Ajelli, M.; Litvinova, M.; Chinazzi, M.; Dean, N.E.; Halloran, M.E.; Longini, I.M., Jr.; Merler, S.; et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020, 4, 964–971. [Google Scholar] [CrossRef]
- Li, X.N.; Huang, Y.; Wang, W.; Jing, Q.L.; Zhang, C.H.; Qin, P.Z.; Guan, W.J.; Gan, L.; Li, Y.L.; Liu, W.H.; et al. Efficacy of inactivated SARS-CoV-2 vaccines against the Delta variant infection in Guangzhou: A test-negative case-control real-world study. Emerg. Microbes Infect. 2021, 10, 1751–1759. [Google Scholar] [CrossRef]
- Chen, J.L.; Jin, M.L.; Wang, X.; Yang, X.J.; Zhang, N.; Liu, F.N.; Liu, R.; Guo, J.P.; Chen, Y.; Wang, C.J. Analysis of COVID-19 Epidemic Trend Based on SVEPIUHDR Infectious Disease Dynamics Model. Chin. J. Epidemiol. 2021, 42, 1341–1346. [Google Scholar]
- He, X.; Lau, E.H.Y.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Author Correction: Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 1491–1493. [Google Scholar] [CrossRef]
- Wei, Y.Y.; Zhao, Y.; Chen, F.; Shen, H.B. Principles of dynamics model and its application in forecasting the epidemics and evaluation the efforts of prevention and control interventions. Chin. J. Prev. Med. 2020, 54, 602–607. [Google Scholar]
- Du, M.; Liu, M.; Liu, J. Progress in research of epidemiologic feature and control of SARS-CoV-2 Delta variant. Chin. J. Epidemiol. 2021, 42, 1774–1779. [Google Scholar]
- Wang, J.; Dong, Y. The spread and prevention of COVID-19 based on SEI_(i)RD model. J. Syst. Simul. 2022, 34, 1532–1546. [Google Scholar]
- Zhang, Y.; Liu, Y.; Yao, R.X.; Zha, Y.X.; Liu, Q.; Li, R.Z.; Zhang, L.; Wang, Z.; Xu, X.Y.; Zhong, B. Analysis of length of hospital stay in 365 patients with novel coronavirus pneumonia (COVID-19) based on a multilevel model. Modern Prev. Med. 2020, 47, 4210–4213, 4224. [Google Scholar]
- Zhang, M.; Xiao, J.; Deng, A.; Zhang, Y.; Zhuang, Y.; Hu, T.; Li, J.; Tu, H.; Li, B.; Zhou, Y.; et al. Transmission Dynamics of an Outbreak of the COVID-19 Delta Variant B.1.617.2—Guangdong Province, China, May—June 2021. China CDC Wkly. 2021, 3, 584–586. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.; Kleynhans, J.; von Gottberg, A.; McMorrow, M.L.; Wolter, N.; Bhiman, J.N.; Moyes, J.; du Plessis, M.; Carrim, M.; Buys, A.; et al. SARS-CoV-2 incidence, transmission and reinfection in a rural and an urban setting: Results of the PHIRST-C cohort study, South Africa, 2020–2021. Lancet Infect Dis. 2022, 22, 821–834. [Google Scholar] [CrossRef]
- Hu, S.; Wang, W.; Wang, Y.; Litvinova, M.; Luo, K.; Ren, L.; Sun, Q.; Chen, X.; Zeng, G.; Li, J.; et al. Infectivity, susceptibility, and risk factors associated with SARS-CoV-2 transmission under intensive contact tracing in Hunan. China Nat. Commun. 2021, 12, 1533. [Google Scholar] [CrossRef]
- National Bureau of Statistics of the People’s Republic of China. China Health Statistical Yearbook; China Statistics Press: Beijing, China, 2022. [Google Scholar]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Dattani, S.; Roser, M. Coronavirus Pandemic (COVID-19). 22 March 2022. Available online: https://ourworldindata.org/coronavirus (accessed on 14 August 2022).
- Comprehensive Team of the State Council’s Joint Prevention and Control Mechanism for COVID-19. Notice on Issuing Regional COVID-19 Nucleic Acid Testing Organization Implementation Guidelines (Third Edition). 22 March 2022. Available online: https://www.henan.gov.cn/2022/03-22/2418914.html (accessed on 14 August 2022).
- Worby, C.J.; Chang, H.H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat. Commun. 2020, 11, 4049. [Google Scholar] [CrossRef]
- Hussein, N.R.; Naqid, I. Strict social distancing measures helped early control of SARS-CoV-2 spread in Duhok city, Iraq. J. Infect. Dev. Ctries 2022, 16, 1370–1371. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, B.; Yuan, J.; Tao, Y. The impact of social distancing and epicenter lockdown on the COVID-19 epidemic in mainland China: A data-driven SEIQR model study. medRxiv 2020. [Google Scholar] [CrossRef]
- Fong, M.W.; Gao, H.Z.; Wong, J.Y.; Xiao, J.; Shiu, E.Y.C.; Ryu, S.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings Social Distancing Measures. Emerg. Infect. Dis. 2020, 26, 976–984. [Google Scholar] [CrossRef]
- Zhu, Q.R.; Sun, M.S.; Yang, W.D. Assessment of Impact of COVID-19 Epidemic on China’s Economy: An Empirical Study Based on GTAP Model. Stat. Decis. 2020, 2020, 91–96. [Google Scholar]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 27 February 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/who-china-jointmissionon-covid-19-final-report (accessed on 14 August 2022).
- Wang, Q.; Shi, N.; Huang, J.; Yang, L.; Cui, T.; Ai, J.; Ji, H.; Xu, K.; Ahmad, T.; Bao, C.; et al. Cost-Effectiveness of Public Health Measures to Control COVID-19 in China: A Microsimulation Modeling Study. Front. Public Health 2022, 9, 726690. [Google Scholar] [CrossRef]
- Zhang, T.; Wu, H.T.; Wang, L.H.; Yang, W.Z. Research on rapid assessment of COVID-19 medical resource needs based on scenario simulation. Chin. J. Epidemiol. 2020, 41, 1390–1395. [Google Scholar]
- Lyu, Y.L.; Rong, S.J.; Sun, F.; Xiang, C.; Li, J.Y. Management of an emergency sample collection team under the setting of whole-community severe acute respiratory syndrome coronavirus 2 nucleic acid testing. Int. Health 2022, 7, ihac057. [Google Scholar] [CrossRef]
- López-Seguí, F.; Estrada-Cuxart, O.; Mitjà, I.V.O.; Hernández-Guillamet, G.; Prat-Gil, N.; Maria-Bonet, J.; Isnard-Blanchar, M.; Moreno-Millan, N.; Blanco, I.; Vilar-Capella, M.; et al. A Cost-Benefit Analysis of the COVID-19 Asymptomatic Mass Testing Strategy in the North Metropolitan Area of Barcelona. Int. J. Environ. Res. Public Health 2021, 18, 7028. [Google Scholar] [CrossRef]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.Y.; Chen, L.; Wang, M. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef]
- General Office of National Health Commission. Notice on printing and distributing the diagnosis and treatment plan for novel coronavirus pneumonia (Trial Version 9). 14 March 2022. Available online: http://www.gov.cn/zhengce/zhengceku/2022-03/15/content_5679257.htm (accessed on 14 August 2022).
- Comprehensive Team of the State Council’s Joint Prevention and Control Mechanism for COVID-19.Notice on Issuing the Implementation Guidelines (Second Edition) for the Organization of COVID-19 Nucleic Acid Testing for All Staff. 14 September 2021. Available online: http://www.gov.cn/xinwen/2021-09/14/content_5637134.htm (accessed on 14 August 2022).
| Parameter Name | Meaning | Model Value | Sources |
|---|---|---|---|
| w | Daily vaccination rate | 0.005~0.015 | Parameter estimation |
| α | Vaccine Protection Rate | 0.14 (1 dose) | Reference [27] |
| ρ | Probability of an exposed person becoming an infected person | 0.50 | Reference [28] |
| β1 | Infection index of asymptomatic infected persons and mild confirmed cases | 4.46 (3.40~5.50) | References [29,30] |
| β2 | Infection index of severe/critical confirmed cases | 6.50 (5.00~8.00) | Reference [31] |
| γ1 | The recovery rate of asymptomatic infections and mild confirmed cases | 0.17 | Reference [32] |
| γ2 | The recovery rate of severe/critical confirmed cases | 0.06 | Reference [33] |
| te | The rate at which exposed persons progress to infected persons (reciprocal of incubation period) | 1/4.40 | Reference [34] |
| Df1 | The proportion of asymptomatic infections | 0.85 | Reference [35] |
| Df2 | The proportion of mild confirmed cases | 0.1275 | Reference [36] |
| Df3 | The proportion of severe/critical confirmed cases | 0.0225 | Reference [36] |
| Dq1 | Time from the discovery of asymptomatic infection to isolation(d) | 1 | Parameter estimation |
| Dq2 | Time from the discovery of mild confirmed cases to their isolation(d) | 1 | Parameter estimation |
| Dq3 | Time from the discovery of severe/critical confirmed cases to their hospitalization(d) | 1 | Parameter estimation |
| θ | An effective protection rate of masks | 0.50 (0.50~0.85) | Reference [14] |
| a: Vaccination rate = Planned daily vaccinations/Total population | |||
| Meaning | Large City | Medium City | Small City |
|---|---|---|---|
| Total number of the model (N) | 10,000,000 | 5,000,000 | 500,000 |
| Initial susceptible population (S0) | 1,999,630 | 999,730 | 99,830 |
| Number of initial vaccinations (V0) | 8,000,000 | 4,000,000 | 400,000 |
| Number of initial exposure (E0) | 360 | 260 | 160 |
| The initial number of asymptomatic infections (A0) | 7 | 7 | 7 |
| The initial number of mild confirmed cases (I1) | 2 | 2 | 2 |
| The initial number of severe/critical confirmed cases (I2) | 1 | 1 | 1 |
| Category | Scenario1 (Large City) | Scenario2 (Large City) | Scenario3 (Large City) | Scenario4 (Large City) | Scenario1 (Medium City) | Scenario2 (Medium City) | Scenario3 (Medium City) | Scenario4 (Medium City) | Scenario1 (Small City) | Scenario2 (Small City) | Scenario3 (Small City) | Scenario4 (Small City) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maximum daily demand of staff | ||||||||||||
| Nucleic acid sampling person | 3247 | 27,778 | 27,740 | 2778 | 1627 | 13,889 | 13,852 | 1389 | 164 | 1389 | 1353 | 139 |
| sampling service auxiliary personnel | 9742 | 83,333 | 83,219 | 8333 | 4881 | 41,667 | 41,555 | 4167 | 493 | 4167 | 4058 | 417 |
| Laboratory testing personnel | 2805 | 15,253 | 2397 | 271 | 1406 | 7649 | 1197 | 150 | 142 | 792 | 117 | 41 |
| Laboratory-related auxiliary personnel | 1754 | 9533 | 1498 | 170 | 879 | 4780 | 748 | 94 | 89 | 495 | 73 | 25 |
| Maximum daily demand for laboratory testing resources | ||||||||||||
| Nucleic acid extraction instrument (96 wells) | 468 | 2542 | 399 | 45 | 234 | 1275 | 199 | 25 | 24 | 132 | 19 | 7 |
| Fluorescent PCR amplification instrument (96 wells) | 1169 | 6355 | 999 | 113 | 586 | 3187 | 499 | 62 | 59 | 330 | 49 | 17 |
| A2 type double biological safety cabinet | 351 | 1907 | 300 | 34 | 176 | 956 | 150 | 19 | 18 | 99 | 15 | 5 |
| Micro-adjustable sampler (single channel) | 468 | 2542 | 399 | 45 | 234 | 1275 | 199 | 25 | 28 | 132 | 19 | 7 |
| Micro-adjustable sampler (8 channels) | 351 | 1907 | 300 | 34 | 176 | 956 | 150 | 19 | 18 | 99 | 15 | 5 |
| Single-tube palm centrifuge | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| Eight joint pipe | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| 96-well plate centrifuge | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| Small vortex mixer | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| Multi-tube vortex mixer | 117 | 636 | 100 | 11 | 59 | 319 | 50 | 6 | 6 | 33 | 5 | 2 |
| Eight channel pipette | 117 | 636 | 100 | 11 | 59 | 319 | 50 | 6 | 6 | 33 | 5 | 2 |
| Sample feeder rack | 585 | 3178 | 499 | 57 | 293 | 1593 | 249 | 31 | 30 | 165 | 24 | 8 |
| Temperature box for inactivation | 351 | 1907 | 300 | 34 | 176 | 956 | 150 | 19 | 18 | 99 | 15 | 5 |
| Super clean workbench | 117 | 636 | 100 | 11 | 59 | 319 | 50 | 6 | 6 | 33 | 5 | 2 |
| −20 °C freezer | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| Movable UV lamp | 935 | 5084 | 799 | 90 | 469 | 2550 | 399 | 50 | 47 | 264 | 39 | 14 |
| Inner row autoclave | 234 | 1271 | 200 | 23 | 117 | 637 | 100 | 12 | 12 | 66 | 10 | 3 |
| Air disinfector | 351 | 1907 | 300 | 34 | 176 | 956 | 150 | 19 | 18 | 99 | 15 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, Q.; Shang, W.-P.; Jing, M.-X. Effect of Nucleic Acid Screening Measures on COVID-19 Transmission in Cities of Different Scales and Assessment of Related Testing Resource Demands—Evidence from China. Int. J. Environ. Res. Public Health 2022, 19, 13343. https://doi.org/10.3390/ijerph192013343
Gao Q, Shang W-P, Jing M-X. Effect of Nucleic Acid Screening Measures on COVID-19 Transmission in Cities of Different Scales and Assessment of Related Testing Resource Demands—Evidence from China. International Journal of Environmental Research and Public Health. 2022; 19(20):13343. https://doi.org/10.3390/ijerph192013343
Chicago/Turabian StyleGao, Qian, Wen-Peng Shang, and Ming-Xia Jing. 2022. "Effect of Nucleic Acid Screening Measures on COVID-19 Transmission in Cities of Different Scales and Assessment of Related Testing Resource Demands—Evidence from China" International Journal of Environmental Research and Public Health 19, no. 20: 13343. https://doi.org/10.3390/ijerph192013343
APA StyleGao, Q., Shang, W.-P., & Jing, M.-X. (2022). Effect of Nucleic Acid Screening Measures on COVID-19 Transmission in Cities of Different Scales and Assessment of Related Testing Resource Demands—Evidence from China. International Journal of Environmental Research and Public Health, 19(20), 13343. https://doi.org/10.3390/ijerph192013343







