The Hong Kong Grocery Shopping Dialog Task (HK-GSDT): A Quick Screening Test for Neurocognitive Disorders
Abstract
1. Introduction
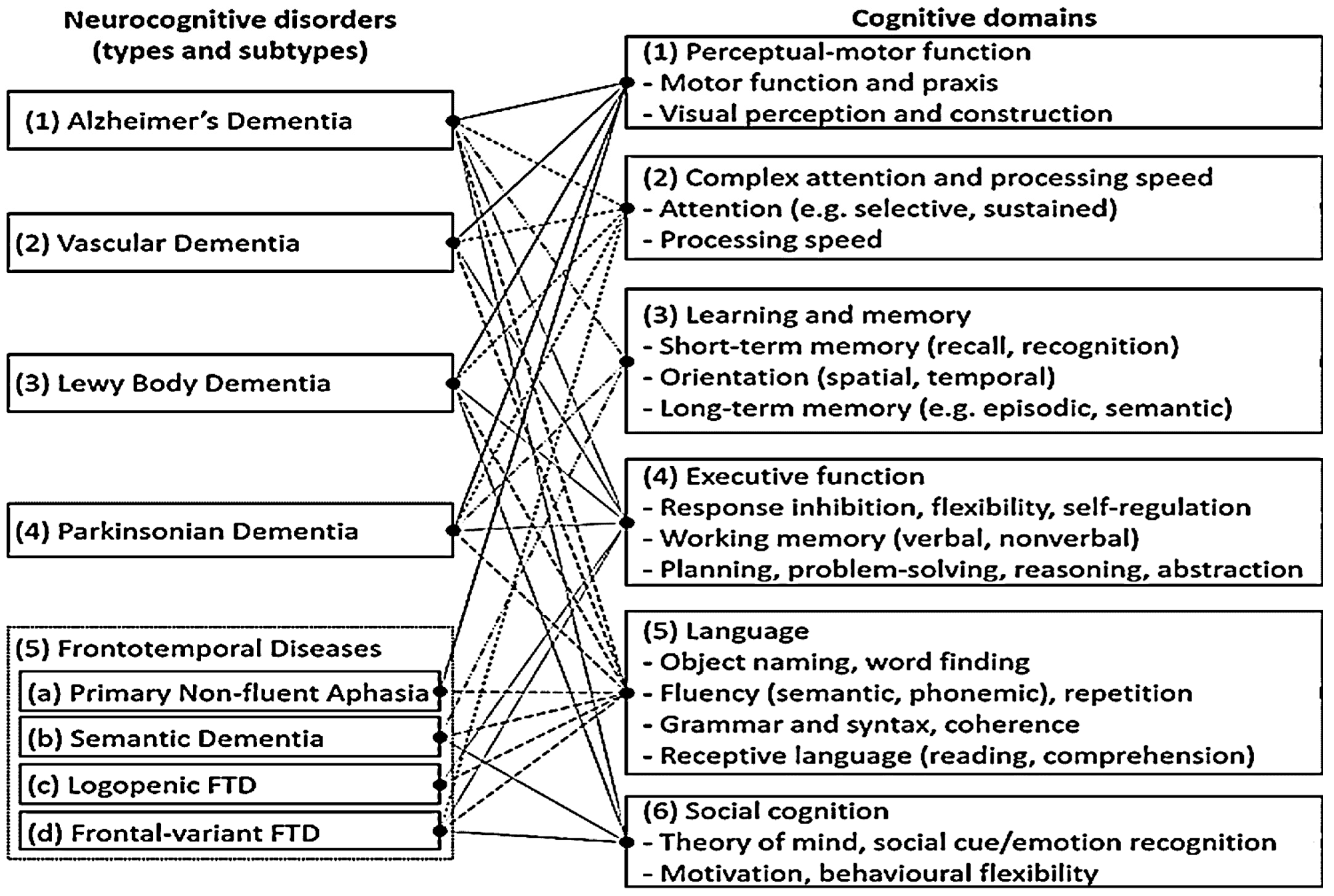
1.1. Cognitive Deficits Associated with Different Types of NCDs
1.2. Neurocognitive Tests for Screening NCDs
1.3. The HK-GSDT
- Dialog example 1—
- Tester:
- Which ingredients do you see in this soup photo?
- Participant:
- I see tofu, pork, egg, and tomato.
- Dialog example 2—
- Tester:
- In case you want to cook the soup, what ingredient you would buy first from the store?
- Participant:
- I would buy pork first.
- Tester:
- How would you walk from the entrance to the shelf to get pork?
- Participant:
- I would go straight to the end of the aisle, turn left, and then turn right to get pork from the “Meat” shelf.
1.4. Strength of the HK-GSDT
1.4.1. Brevity and Ease of Administration
1.4.2. Promisingly Low Test Bias
1.4.3. Wide Coverage of Key Cognitive Functions
1.4.4. Coverage of Cognitive Functions Neglected in the Other Screening Tests
1.5. Current Study
2. Materials and Methods
2.1. Sample
2.2. Measures
2.3. Analytical Strategies
3. Results
3.1. Reliability and Structural Validity
3.2. Divergent and Convergent Validity
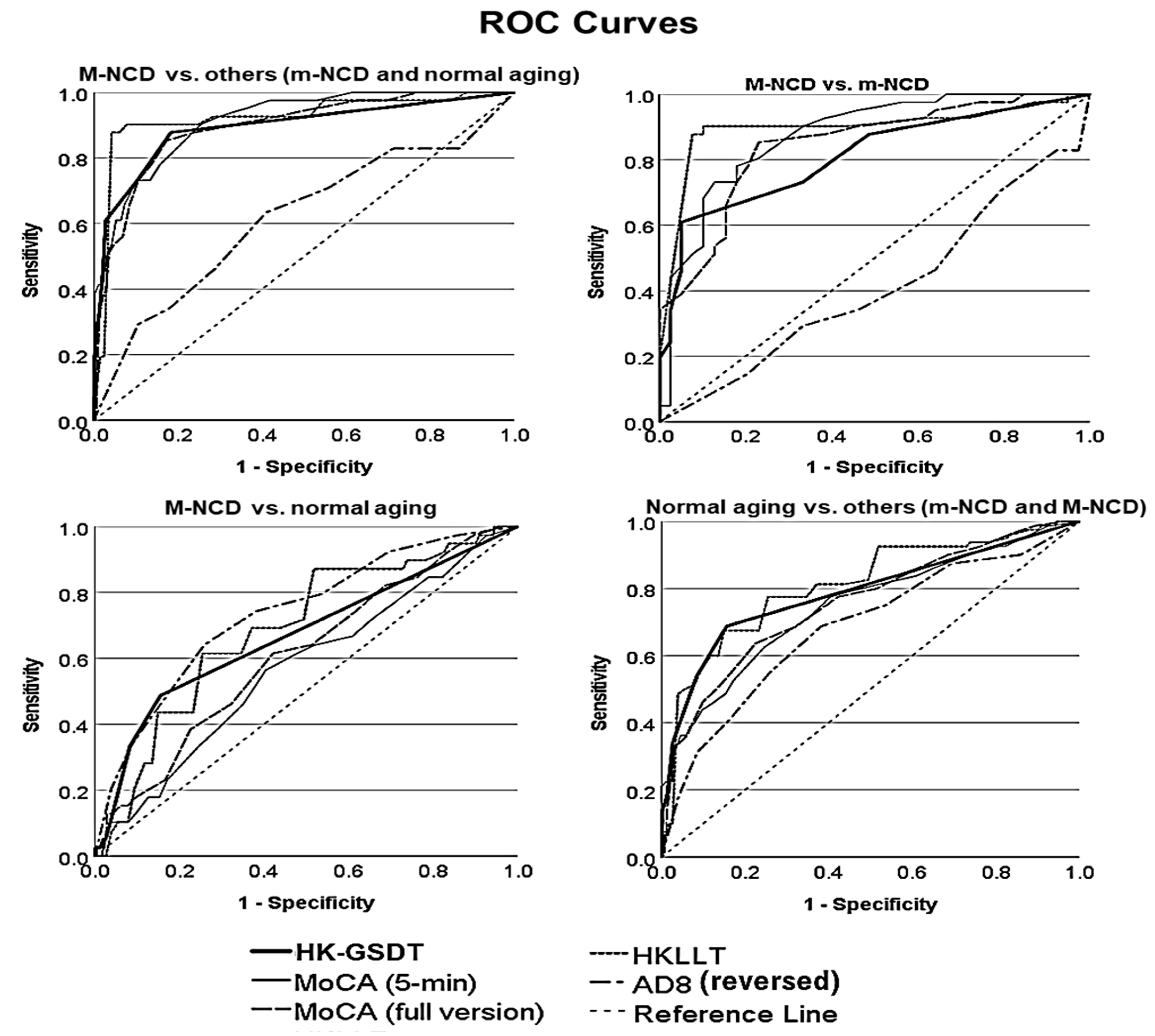
3.3. Criterion Validity: Effectiveness of the HK-GSDT in NCD Screening as a Standalone Test
3.4. Criterion Validity: Effectiveness of the HK-GSDT in NCD Screening in Combination with Other Tests
3.5. Test Bias Related to Demographics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 30 December 2021).
- Lay, J.C.; Wong, P.C.M.; Fung, H.H.; Mok, V.C.T.; Wong, A.; Kwok, T.C.Y.; Woo, J.; Meng, H. Overview of the Spoken Language Correlates of Neurocognitive Disorders. 2022; under review. [Google Scholar]
- Emre, M.; Aarsland, D.; Brown, R.; Burn, D.J.; Duyckaerts, C.; Mizuno, Y.; Broe, G.A.; Cummings, J.; Dickson, D.W.; Gauthier, S. Clinical Diagnostic Criteria for Dementia Associated with Parkinson’s Disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2007, 22, 1689–1707. [Google Scholar] [CrossRef]
- Yutsis, M.; Rosen, A.C.; Deutsch, G.K. Neurocognitive Disorders. In APA Handbook of Psychopathology: Understanding, Assessing, and Treating Adult Mental Disorders; American Psychological Association: Washington, DC, USA, 2018; pp. 321–342. [Google Scholar]
- Sachs-Ericsson, N.; Blazer, D.G. The New DSM-5 Diagnosis of Mild Neurocognitive Disorder and Its Relation to Research in Mild Cognitive Impairment. Aging Ment. Health 2015, 19, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.; Rodriguez, A.D.; Lamy, M.; Neils-Strunjas, J. Cognition, Language, and Clinical Pathological Features of Non-Alzheimer’s Dementias: An Overview. J. Commun. Disord. 2010, 43, 438–452. [Google Scholar] [CrossRef] [PubMed]
- McKeith, I.G.; Dickson, D.W.; Lowe, J.; Emre, M.; O’brien, J.T.; Feldman, H.; Cummings, J.; Duda, J.E.; Lippa, C.; Perry, E.K. Diagnosis and Management of Dementia with Lewy Bodies: Third Report of the DLB Consortium. Neurology 2005, 65, 1863–1872. [Google Scholar] [CrossRef] [PubMed]
- Aarsland, D.; Zaccai, J.; Brayne, C. A Systematic Review of Prevalence Studies of Dementia in Parkinson’s Disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2005, 20, 1255–1263. [Google Scholar] [CrossRef]
- Gorno-Tempini, M.L.; Hillis, A.E.; Weintraub, S.; Kertesz, A.; Mendez, M.; Cappa, S.F.; Ogar, J.M.; Rohrer, J.D.; Black, S.; Boeve, B.F. Classification of Primary Progressive Aphasia and Its Variants. Neurology 2011, 76, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Jarrold, W.; Peintner, B.; Wilkins, D.; Vergryi, D.; Richey, C.; Gorno-Tempini, M.L.; Ogar, J. Aided Diagnosis of Dementia Type through Computer-Based Analysis of Spontaneous Speech. In Proceedings of the Workshop on Computational Linguistics and Clinical Psychology: From Linguistic Signal to Clinical Reality, Baltimore, MD, USA, 27 June 2014; pp. 27–37. [Google Scholar]
- Cullen, B.; O’Neill, B.; Evans, J.J.; Coen, R.F.; Lawlor, B.A. A Review of Screening Tests for Cognitive Impairment. J. Neurol. Neurosurg. Psychiatry 2007, 78, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Lorentz, W.J.; Scanlan, J.M.; Borson, S. Brief Screening Tests for Dementia. Can. J. Psychiatry 2002, 47, 723–733. [Google Scholar] [CrossRef]
- Lonie, J.A.; Tierney, K.M.; Ebmeier, K.P. Screening for Mild Cognitive Impairment: A Systematic Review. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 2009, 24, 902–915. [Google Scholar] [CrossRef]
- Aslam, R.W.; Bates, V.; Dundar, Y.; Hounsome, J.; Richardson, M.; Krishan, A.; Dickson, R.; Boland, A.; Fisher, J.; Robinson, L. A Systematic Review of the Diagnostic Accuracy of Automated Tests for Cognitive Impairment. Int. J. Geriatr. Psychiatry 2018, 33, 561–575. [Google Scholar] [CrossRef]
- Gifford, D.R.; Cummings, J.L. Evaluating Dementia Screening Tests: Methodologic Standards to Rate Their Performance. Neurology 1999, 52, 224. [Google Scholar] [CrossRef] [PubMed]
- Mioshi, E.; Dawson, K.; Mitchell, J.; Arnold, R.; Hodges, J.R. The Addenbrooke’s Cognitive Examination Revised (ACE-R): A Brief Cognitive Test Battery for Dementia Screening. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 2006, 21, 1078–1085. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Kokmen, E.; Smith, G.E.; Petersen, R.C.; Tangalos, E.; Ivnik, R.C. The Short Test of Mental Status: Correlations with Standardized Psychometric Testing. Arch. Neurol. 1991, 48, 725–728. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Dong, B. Screening for Cognitive Impairment in Geriatrics. Clin. Geriatr. Med. 2018, 34, 515–536. [Google Scholar] [CrossRef]
- Wood, R.; Dixon, E.; Elsayed-Ali, S.; Shokeen, E.; Lazar, A.; Lazar, J. Investigating Best Practices for Remote Summative Usability Testing with People with Mild to Moderate Dementia. ACM Trans. Access. Comput. 2021, 14, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Law, L.L.F.; Barnett, F.; Yau, M.K.; Gray, M.A. Measures of Everyday Competence in Older Adults with Cognitive Impairment: A Systematic Review. Age Ageing 2012, 41, 9–16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bielak, A.A.M.; Hatt, C.R.; Diehl, M. Cognitive Performance in Adults’ Daily Lives: Is There a Lab-Life Gap? Res. Hum. Dev. 2017, 14, 219–233. [Google Scholar] [CrossRef]
- Holland, A.L.; Fromm, D.; Wozniak, L. Communication Activities of Daily Living―Third Edition (CADL-3); Pro-Ed: Austin, TX, USA, 2018. [Google Scholar]
- Giles, E.; Patterson, K.; Hodges, J.R. Performance on the Boston Cookie Theft Picture Description Task in Patients with Early Dementia of the Alzheimer’s Type: Missing Information. Aphasiology 1996, 10, 395–408. [Google Scholar] [CrossRef]
- Boschi, V.; Catricala, E.; Consonni, M.; Chesi, C.; Moro, A.; Cappa, S.F. Connected Speech in Neurodegenerative Language Disorders: A Review. Front. Psychol. 2017, 8, 269. [Google Scholar] [CrossRef]
- Fraser, K.C.; Meltzer, J.A.; Rudzicz, F. Linguistic Features Identify Alzheimer’s Disease in Narrative Speech. J. Alzheimer’s Dis. 2016, 49, 407–422. [Google Scholar] [CrossRef] [PubMed]
- Kemper, S.; Altmann, L.J.P. Dementia and Language. In Handbook of the Neuroscience of Aging; Hof, P.R., Mobbs, C.V., Eds.; Academic Press: London, UK, 2009; pp. 293–299. [Google Scholar]
- de la Fuente Garcia, S.; Ritchie, C.W.; Luz, S. Protocol for a Conversation-Based Analysis Study: Prevent-ED Investigates Dialogue Features That May Help Predict Dementia Onset in Later Life. BMJ Open 2019, 9, e026254. [Google Scholar] [CrossRef] [PubMed]
- Rektorova, I.; Mekyska, J.; Janousova, E.; Kostalova, M.; Eliasova, I.; Mrackova, M.; Berankova, D.; Necasova, T.; Smekal, Z.; Marecek, R. Speech Prosody Impairment Predicts Cognitive Decline in Parkinson’s Disease. Parkinsonism Relat. Disord. 2016, 29, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Peach, R.; Wong, P. Integrating the Message Level into Treatment for Agrammatism Using Story Retelling. Aphasiology 2004, 18, 429–441. [Google Scholar] [CrossRef]
- Aggio, N.M.; Ducatti, M.; de Rose, J.C. Cognition and Language in Dementia Patients: Contributions from Behavior Analysis. Behav. Interv. 2018, 33, 322–335. [Google Scholar] [CrossRef]
- Kempler, D.; Goral, M. Language and Dementia: Neuropsychological Aspects. Annu. Rev. Appl. Linguist. 2008, 28, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.C. The Mental Status Examination. In Clinical Methods: The History, Physical and Laboratory Examinations, 3rd ed.; Butterworth-Heinemann Ltd.: Oxford, UK, 1990. [Google Scholar]
- Sachdev, P.S.; Blacker, D.; Blazer, D.G.; Ganguli, M.; Jeste, D.V.; Paulsen, J.S.; Petersen, R.C. Classifying Neurocognitive Disorders: The DSM-5 Approach. Nat. Rev. Neurol. 2014, 10, 634–642. [Google Scholar] [CrossRef]
- Kemper, S.; Sumner, A. The Structure of Verbal Abilities in Young and Older Adults. Psychol. Aging 2001, 16, 312–322. [Google Scholar] [CrossRef]
- Hornberger, M.; Piguet, O. Episodic Memory in Frontotemporal Dementia: A Critical Review. Brain 2012, 135, 678–692. [Google Scholar] [CrossRef]
- Clague, F.; Dudas, R.B.; Thompson, S.A.; Graham, K.S.; Hodges, J.R. Multidimensional Measures of Person Knowledge and Spatial Associative Learning: Can These Be Applied to the Differentiation of Alzheimer’s Disease from Frontotemporal and Vascular Dementia? Neuropsychologia 2005, 43, 1338–1350. [Google Scholar] [CrossRef]
- Ramanan, S.; Flanagan, E.; Leyton, C.E.; Villemagne, V.L.; Rowe, C.C.; Hodges, J.R.; Hornberger, M. Non-Verbal Episodic Memory Deficits in Primary Progressive Aphasias Are Highly Predictive of Underlying Amyloid Pathology. J. Alzheimer’s Dis. 2016, 51, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Pengas, G.; Patterson, K.; Arnold, R.J.; Bird, C.M.; Burgess, N.; Nestor, P.J. Lost and Found: Bespoke Memory Testing for Alzheimer’s Disease and Semantic Dementia. J. Alzheimer’s Dis. 2010, 21, 1347–1365. [Google Scholar] [CrossRef] [PubMed]
- Swainson, R.; Hodges, J.R.; Galton, C.J.; Semple, J.; Michael, A.; Dunn, B.D.; Iddon, J.L.; Robbins, T.W.; Sahakian, B.J. Early Detection and Differential Diagnosis of Alzheimer’s Disease and Depression with Neuropsychological Tasks. Dement. Geriatr. Cogn. Disord. 2001, 12, 265–280. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, A.D.; Sahakian, B.J.; Vesey, R.; Semple, J.M.; Robbins, T.W.; Hodges, J.R. Detecting Dementia: Novel Neuropsychological Markers of Preclinical Alzheimer’s Disease. Dement. Geriatr. Cogn. Disord. 2004, 17, 42–48. [Google Scholar] [CrossRef]
- Taler, V.; Phillips, N.A. Language Performance in Alzheimer’s Disease and Mild Cognitive Impairment: A Comparative Review. J. Clin. Exp. Neuropsychol. 2008, 30, 501–556. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Xiong, Y.Y.; Kwan, P.W.L.; Chan, A.Y.Y.; Lam, W.W.M.; Wang, K.; Chu, W.C.W.; Nyenhuis, D.L.; Nasreddine, Z.; Wong, L.K.S. The Validity, Reliability and Clinical Utility of the Hong Kong Montreal Cognitive Assessment (HK-MoCA) in Patients with Cerebral Small Vessel Disease. Dement. Geriatr. Cogn. Disord. 2009, 28, 81–87. [Google Scholar] [CrossRef]
- Chan, A.S.; Kwok, I. Hong Kong List Learning Test (HKLLT): Manual and Preliminary Norms; Department of Psychology, The Chinese University of Hong Kong: Hong Kong, China, 1999. [Google Scholar]
- Wechsler, D. The Measurement and Appraisal of Adult Intelligence; Williams & Wilkins Co.: Baltimore, MD, USA, 1958. [Google Scholar]
- Kaplan, E.; Goodglass, H.; Weintraub, S. Boston Naming Test; Lea and Febiger: Philadelphia, PA, USA, 1983. [Google Scholar]
- Mack, W.J.; Freed, D.M.; Williams, B.W.; Henderson, V.W. Boston Naming Test: Shortened Versions for Use in Alzheimer’s Disease. J. Gerontol. 1992, 47, 154–158. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”: A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Galvin, J.E.; Roe, C.M.; Powlishta, K.K.; Coats, M.A.; Muich, S.J.; Grant, E.; Miller, J.P.; Storandt, M.; Morris, J.C. The AD8: A Brief Informant Interview to Detect Dementia. Neurology 2005, 65, 559–564. [Google Scholar] [CrossRef]
- Maj, M.; D’Elia, L.; Satz, P.; Janssen, R.; Zaudig, M.; Uchiyama, C.; Starace, F.; Galderisi, S.; Chervinsky, A. Evaluation of Two New Neuropsychological Tests Designed to Minimize Cultural Bias in the Assessment of HIV-1 Seropositive Persons: A WHO Study. Arch. Clin. Neuropsychol. 1993, 8, 123–135. [Google Scholar] [CrossRef]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L.Z. Development and Testing of a Five-item Version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, G.S.; Hagemann, P.D.M.; Coelho, D.D.S.; Santos, F.H.D.; Bertolucci, P.H. Can MoCA and MMSE Be Interchangeable Cognitive Screening Tools? A Systematic Review. Gerontologist 2019, 59, e743–e763. [Google Scholar] [CrossRef] [PubMed]
- Soederberg Miller, L.M. The Effects of Age and Domain Knowledge on Text Processing. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2003, 58, 217–223. [Google Scholar] [CrossRef]
- Wong, P.C.M.; Ou, J.; Pang, C.W.Y.; Zhang, L.; Tse, C.S.; Lam, L.C.W.; Antoniou, M. Language Training Leads to Global Cognitive Improvement in Older Adults: A Preliminary Study. J. Speech Lang. Hear. Res. 2019, 62, 2411–2424. [Google Scholar] [CrossRef]
- Bak, T.H.; Long, M.R.; Vega-Mendoza, M.; Sorace, A. Novelty, Challenge, and Practice: The Impact of Intensive Language Learning on Attentional Functions. PLoS ONE 2016, 11, e0153485. [Google Scholar] [CrossRef] [PubMed]
- Ingvalson, E.M.; Dhar, S.; Wong, P.C.M.; Liu, H. Working Memory Training to Improve Speech Perception in Noise across Languages. J. Acoust. Soc. Am. 2015, 137, 3477–3486. [Google Scholar] [CrossRef] [PubMed]
- Dresler, M.; Shirer, W.R.; Konrad, B.N.; Müller, N.C.J.; Wagner, I.C.; Fernández, G.; Czisch, M.; Greicius, M.D. Mnemonic Training Reshapes Brain Networks to Support Superior Memory. Neuron 2017, 93, 1227–1235. [Google Scholar] [CrossRef]
- Deng, Z.; Chandrasekaran, B.; Wang, S.; Wong, P.C.M. Resting-State Low-Frequency Fluctuations Reflect Individual Differences in Spoken Language Learning. Cortex 2016, 76, 63–78. [Google Scholar] [CrossRef]
- Greicius, M.D.; Srivastava, G.; Reiss, A.L.; Menon, V. Default-Mode Network Activity Distinguishes Alzheimer’s Disease from Healthy Aging: Evidence from Functional MRI. Proc. Natl. Acad. Sci. USA 2004, 101, 4637–4642. [Google Scholar] [CrossRef]
- Wenger, E.; Schaefer, S.; Noack, H.; Kühn, S.; Mårtensson, J.; Heinze, H.-J.; Düzel, E.; Bäckman, L.; Lindenberger, U.; Lövdén, M. Cortical Thickness Changes Following Spatial Navigation Training in Adulthood and Aging. Neuroimage 2012, 59, 3389–3397. [Google Scholar] [CrossRef]
| Cognitive Domains | Specific Cognitive Functions |
|---|---|
| Perceptual-motor function | -Perceptual function: e.g., recognition of dish ingredients, perception of the store’s spatial layout. -Motor function: e.g., articulation of speech, speaking. |
| Attention and Processing speed | -Sustained attention: e.g., continual attention to the interconnected shopping task. -Selective attention: e.g., selective focus on the goal of purchasing the needed ingredients. -Processing speed: e.g., completing each section of the task within a certain timeframe. |
| Learning and Memory | -Semantic memory/knowledge: e.g., knowing the names of ingredients, knowing the membership relationships between ingredients and product categories (e.g., tomato belongs to vegetable). -Verbal episodic memory: e.g., the memory of (names of) ingredients and products. -Non-verbal episodic memory: e.g., the memory of visuospatial details, context, and locations. -Orientation: e.g., locating oneself in the grocery store. |
| Executive function | -Planning, focusing, monitoring, and directing behavior for the goal of getting needed ingredients. -Inhibition: e.g., inhibition of irrelevant information and products in the grocery store. -Switch: e.g., switching goal from purchasing one ingredient to purchasing another ingredient. -Working memory: e.g., holding the task goal in mind throughout the task. |
| Language | -Language comprehension: understanding what the tester says. -Language production: naming ingredients, naming actions, describing shopping steps. -Dialog speech between the tester and the participant. |
| Social cognition | [Social cognition is not highly involved in the test] |
| M-NCD (Dementia) | m-NCD (Mild Cognitive Impairment) | Normal Aging | Total | |
|---|---|---|---|---|
| Sample size (N) | 42 | 39 | 464 | 545 |
| Gender (% female) | 56.1% | 38.5% | 60.8% | 58.8% |
| Age (M ± SD) | 81.8 ± 6.07 | 82.9 ± 4.37 | 71.8 ± 7.78 | 73.4 ± 8.37 |
| Education (M ± SD) | 6.1 ± 5.43 | 6.8 ± 5.09 | 8.4 ± 7.73 | 8.1 ± 7.44 |
| Marital status (%) | ||||
| single/married/divorced/widow | 0/61.9%/4.8%/33.3% | 0/69.2%/10.3%/20.5% | 7.3%/66.4%/6.5%/19.4% | 6.2%/66.1%/6.6%/20.7% |
| Neurocognitive tests | usually AD8 ≥ 2 and HKLLT < −1.5 SD and MoCA ≤ 16th percentile | AD8 ≥ 2 &(HKLLT < −1 SD ORMoCA ≤ 16th percentile) | Scores out of the criteria for M- and m-NCD | |
| Clinical diagnosis | two clinicians | two clinicians | two clinicians |
| M | SD | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. HK-GSDT | 9.38 | 1.49 | −0.42 | −0.003 | 0.12 | −0.16 | 0.15 | −0.16 | 0.42 | 0.29 | 0.35 | 0.35 | 0.56 | 0.58 | 0.60 |
| 2. Age | 73.37 | 8.37 | 0.08 | −0.11 | 0.18 | −0.07 | 0.23 | −0.42 | −0.28 | −0.41 | −0.28 | −0.45 | −0.43 | −0.40 | |
| 3. Gender | [58.8% female] | 0.12 | 0.04 | 0.01 | 0.06 | −0.09 | 0.01 | 0.04 | −0.14 | 0.07 | −0.01 | −0.001 | |||
| 4. Education | 8.14 | 7.44 | −0.08 | −0.002 | −0.07 | 0.10 | 0.07 | 0.12 | 0.11 | 0.12 | 0.19 | 0.13 | |||
| 5. GDS | 0.670 | 1.07 | −0.04 | 0.36 | −0.20 | −0.16 | −0.20 | −0.14 | −0.22 | −0.20 | −0.22 | ||||
| 6. CCT | 1.06 | 0.57 | −0.03 | 0.04 | 0.01 | 0.01 | 0.02 | 0.05 | 0.05 | 0.01 | |||||
| 7. AD8 | 3.26 | 2.36 | −0.20 | −0.19 | −0.18 | −0.25 | −0.30 | −0.25 | −0.25 | ||||||
| 8. Logical memory | 20.52 | 4.51 | 0.32 | 0.42 | 0.47 | 0.50 | 0.52 | 0.51 | |||||||
| 9. Digit span forward | 8.12 | 1.34 | 0.45 | 0.17 | 0.42 | 0.38 | 0.36 | ||||||||
| 10. Digit span backward | 4.82 | 1.50 | 0.33 | 0.49 | 0.52 | 0.44 | |||||||||
| 11. HKLLT | −0.45 | 0.90 | 0.42 | 0.54 | 0.51 | ||||||||||
| 12. mBNT | 20.80 | 4.96 | 0.72 | 0.59 | |||||||||||
| 13. MoCA (full) | 21.16 | 5.32 | 0.74 | ||||||||||||
| 14. MoCA (5-min) | 20.18 | 3.94 | |||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, X.; Wong, P.C.M.; Fung, H.H.; Mok, V.C.T.; Kwok, T.C.Y.; Woo, J.; Wong, K.H.; Meng, H. The Hong Kong Grocery Shopping Dialog Task (HK-GSDT): A Quick Screening Test for Neurocognitive Disorders. Int. J. Environ. Res. Public Health 2022, 19, 13302. https://doi.org/10.3390/ijerph192013302
Gong X, Wong PCM, Fung HH, Mok VCT, Kwok TCY, Woo J, Wong KH, Meng H. The Hong Kong Grocery Shopping Dialog Task (HK-GSDT): A Quick Screening Test for Neurocognitive Disorders. International Journal of Environmental Research and Public Health. 2022; 19(20):13302. https://doi.org/10.3390/ijerph192013302
Chicago/Turabian StyleGong, Xianmin, Patrick C. M. Wong, Helene H. Fung, Vincent C. T. Mok, Timothy C. Y. Kwok, Jean Woo, Ka Ho Wong, and Helen Meng. 2022. "The Hong Kong Grocery Shopping Dialog Task (HK-GSDT): A Quick Screening Test for Neurocognitive Disorders" International Journal of Environmental Research and Public Health 19, no. 20: 13302. https://doi.org/10.3390/ijerph192013302
APA StyleGong, X., Wong, P. C. M., Fung, H. H., Mok, V. C. T., Kwok, T. C. Y., Woo, J., Wong, K. H., & Meng, H. (2022). The Hong Kong Grocery Shopping Dialog Task (HK-GSDT): A Quick Screening Test for Neurocognitive Disorders. International Journal of Environmental Research and Public Health, 19(20), 13302. https://doi.org/10.3390/ijerph192013302







