Long-Term Impact of COVID-19 on Hospital Visits of Rural Residents in Guangdong, China: A Controlled Interrupted Time Series Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
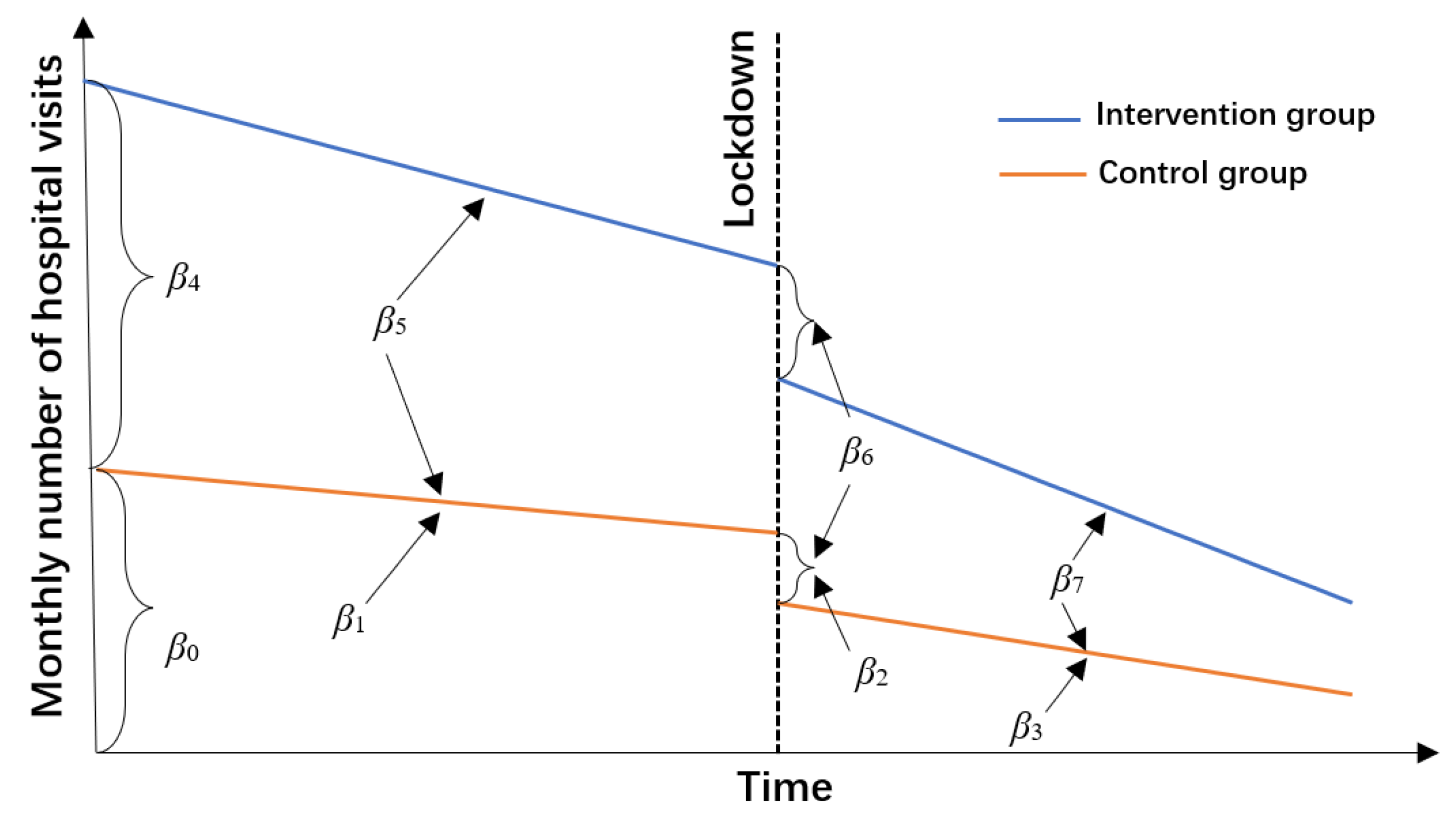
2.2. CITS Design
2.3. Measurement
2.4. Statistical Analysis
β6 Group × Phase + β7 Group × Post + Month + et
3. Results
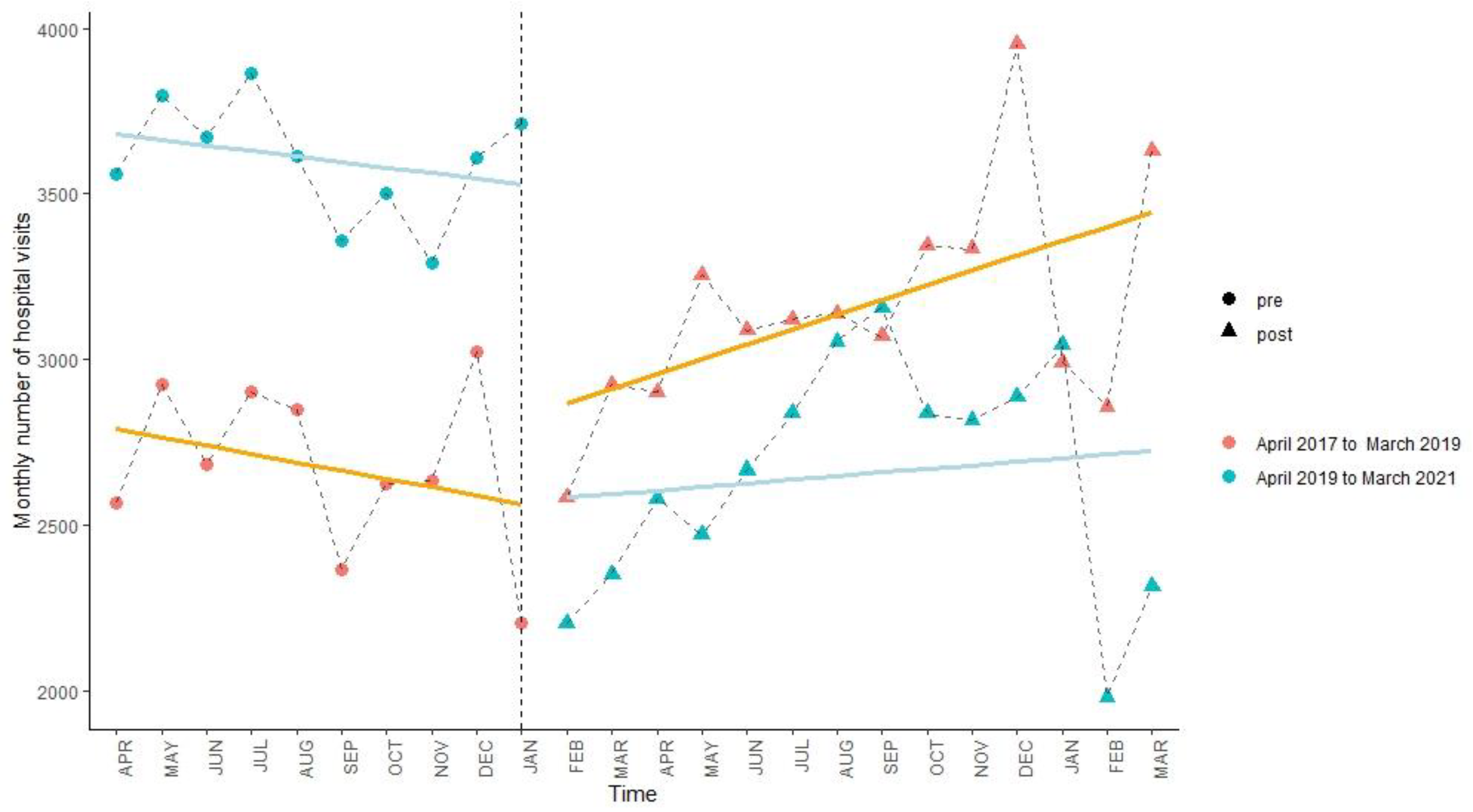
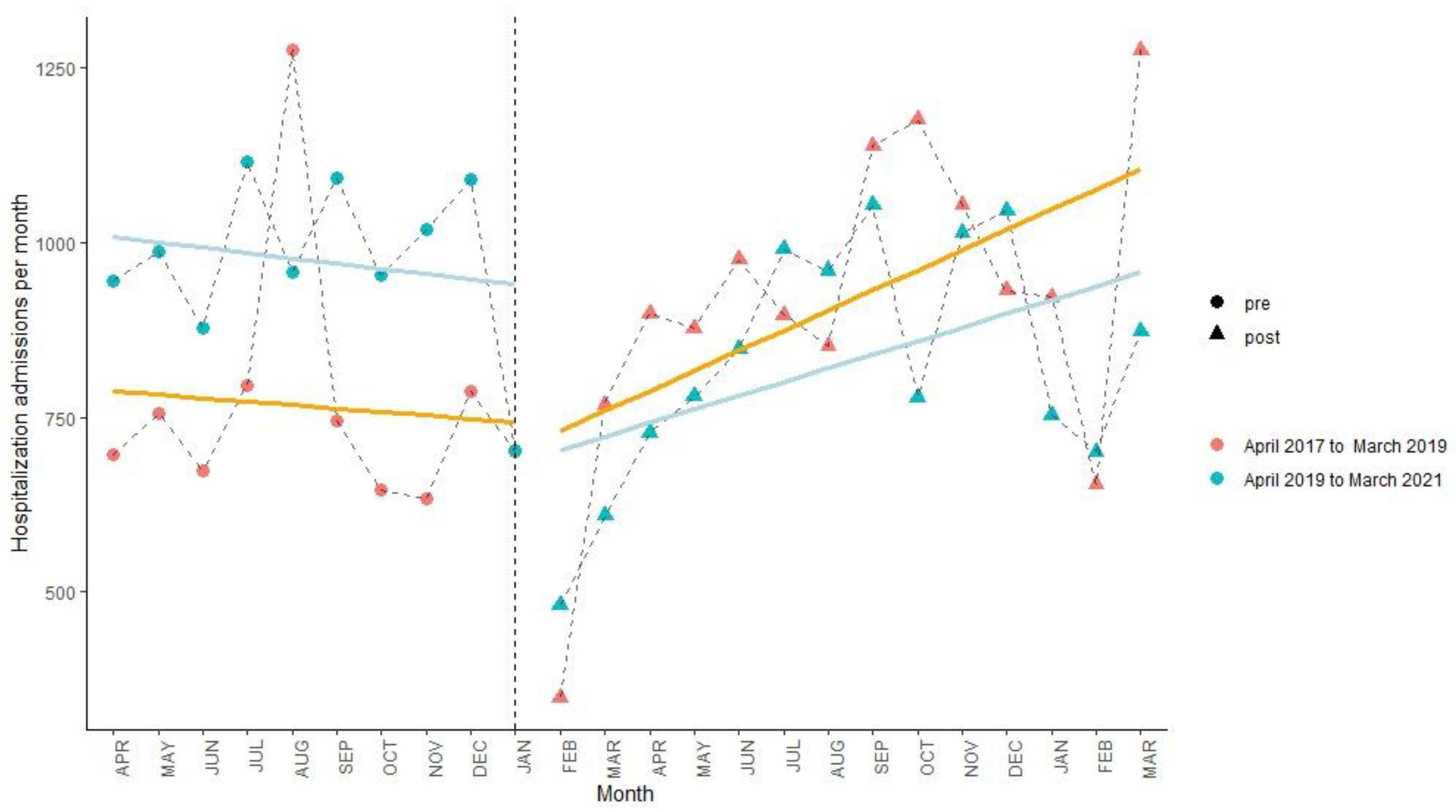
3.1. Changes in the Monthly Number of Hospital Visits in Three Hospitalization Areas
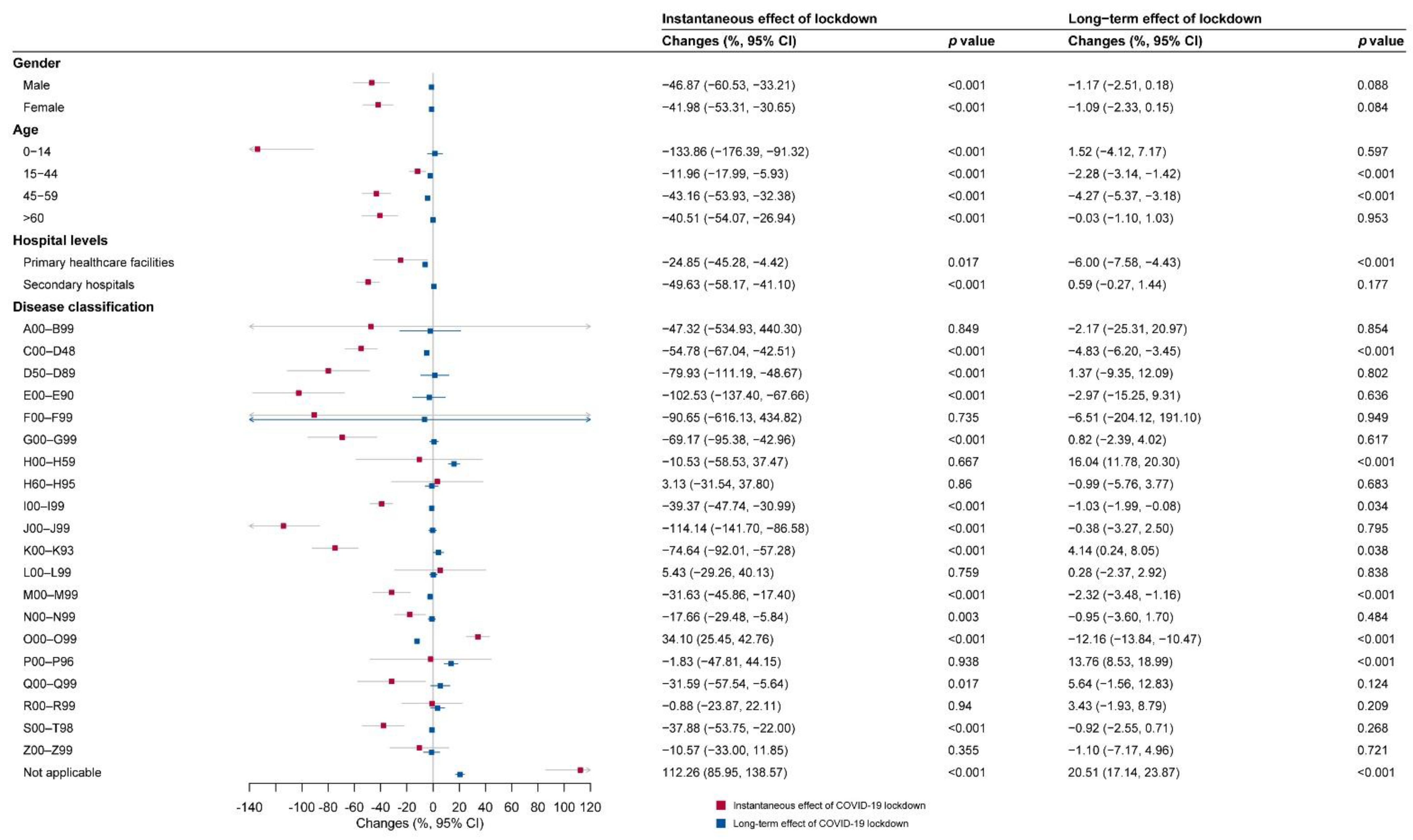
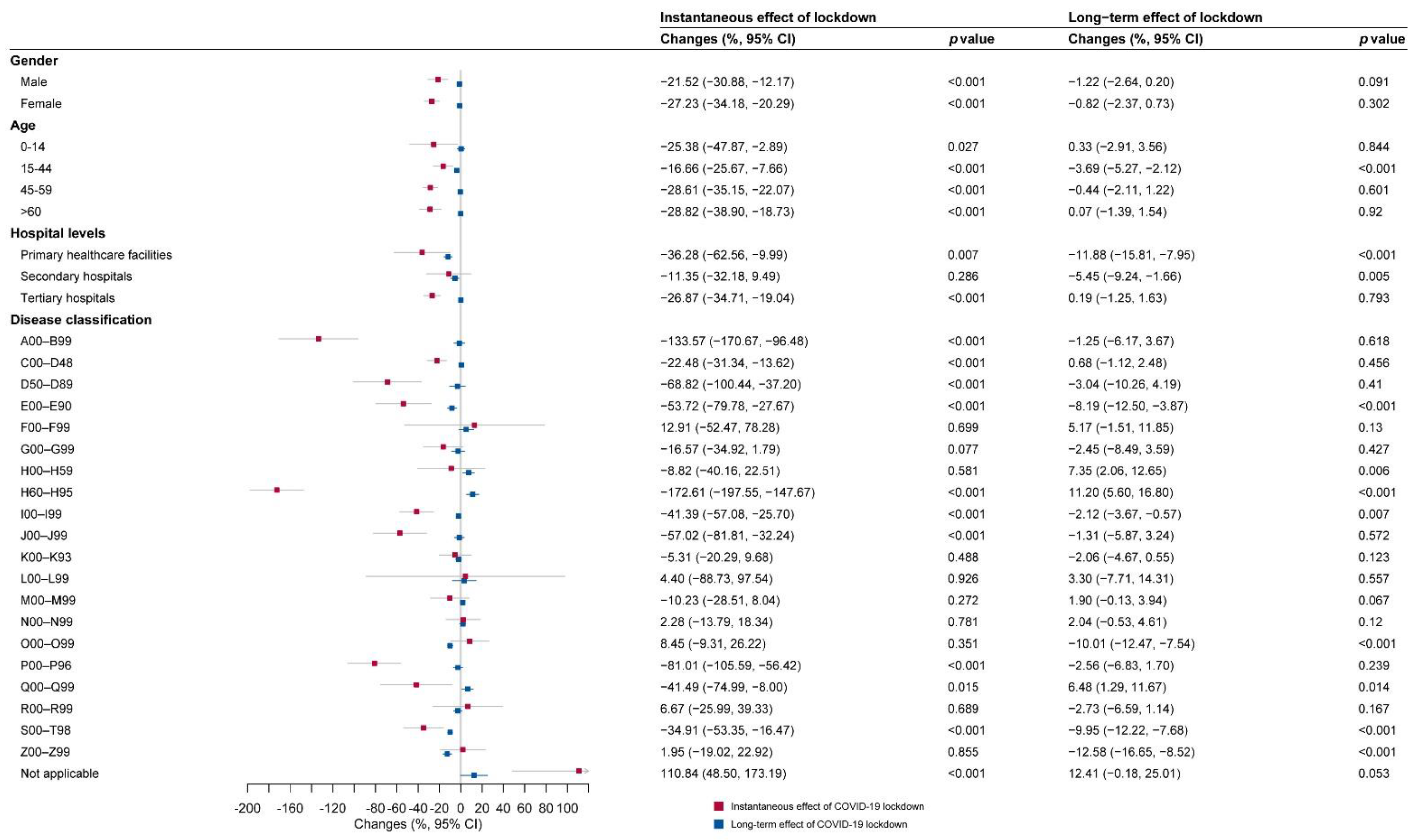
3.2. Instantaneous Effect of COVID-19 According to Subgroup Analyses
3.3. Long-Term Impacts of COVID-19 According to Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saah, F.I.; Amu, H.; Seidu, A.A.; Bain, L.E. Health knowledge and care seeking behaviour in resource-limited settings amidst the COVID-19 pandemic: A qualitative study in Ghana. PLoS ONE 2021, 16, e0250940. [Google Scholar] [CrossRef] [PubMed]
- Westgard, B.C.; Morgan, M.W.; Vazquez-Benitez, G.; Erickson, L.O.; Zwank, M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann. Emerg. Med. 2020, 76, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, R.H.; Wood, R.; Stagg, H.R.; Fischbacher, C.; Villacampa, J.; Simpson, C.R.; Vasileiou, E.; McCowan, C.; Stock, S.J.; Docherty, A.B.; et al. Impact of COVID-19 on accident and emergency attendances and emergency and planned hospital admissions in Scotland: An interrupted time-series analysis. J. R. Soc. Med. 2020, 113, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Hategeka, C.; Carter, S.E.; Chenge, F.M.; Katanga, E.N.; Lurton, G.; Mayaka, S.M.; Mwamba, D.K.; van Kleef, E.; Vanlerberghe, V.; Grepin, K.A. Impact of the COVID-19 pandemic and response on the utilisation of health services in public facilities during the first wave in Kinshasa, the Democratic Republic of the Congo. BMJ Glob. Health 2021, 6, e005955. [Google Scholar] [CrossRef] [PubMed]
- Center for Health Statistics and Information of China. National Medical Care Utilization from January to March; Center for Health Statistics and Information of China: Beijing, China, 2020; Volume 2021. (In Chinese)
- Mahajan, V.; Singh, T.; Azad, C. Using telemedicine during the COVID-19 pandemic. Indian Pediatr. 2020, 57, 652–657. [Google Scholar] [CrossRef]
- Yao, S.; Lin, B.; Liu, Y.; Luo, Y.; Xu, Q.; Huang, J.; Yan, Z.; Liu, X. Impact of COVID-19 on the behavior of community residents with suspected transient ischemic attack. Front. Neurol. 2020, 11, 590406. [Google Scholar] [CrossRef] [PubMed]
- People’s Daily Online. Summary of National Emergency Response Level: 8 Provinces in Level 2 and 21 Provinces in Level 3; People’s Daily Online: Beijing, China, 2020. (In Chinese) [Google Scholar]
- Haider, N.; Osman, A.Y.; Gadzekpo, A.; Akipede, G.O.; Asogun, D.; Ansumana, R.; Lessells, R.J.; Khan, P.; Hamid, M.M.A.; Yeboah-Manu, D.; et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob. Health 2020, 5, e003319. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. India under COVID-19 lockdown. Lancet 2020, 395, 1315. [Google Scholar] [CrossRef]
- Atherly, A.; Van den Broek-Altenburg, E.; Hart, V.; Gleason, K.; Carney, J. Consumer reported care deferrals due to the COVID-19 pandemic, and the role and potential of telemedicine: Cross-sectional analysis. Jmir Public Health Surveill. 2020, 6, 388–397. [Google Scholar] [CrossRef]
- Brown, N.J.; Wilson, B.; Szabadi, S.; Quon, C.; Ong, V.; Himstead, A.; Shlobin, N.A.; Yang, C.Y.; Lien, B.V.; Shahrestani, S.; et al. Ethical considerations and patient safety concerns for cancelling non-urgent surgeries during the COVID-19 pandemic: A review. Patient Saf. Surg. 2021, 15, 19. [Google Scholar] [CrossRef]
- Grubic, A.D.; Ayazi, S.; Zebarjadi, J.; Tahmasbi, H.; Ayazi, K.; Jobe, B.A. COVID-19 outbreak and surgical practice: The rationale for suspending non-urgent surgeries and role of testing modalities. World J. Gastrointest Surg. 2020, 12, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, K.; Chessman, J.; Zhao, J.; Sara, G.; Shetty, A.; Smith, S.; Went, A.; Dyson, S.; Levesque, J.F. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res. Pract. 2020, 30, 3042030. [Google Scholar] [CrossRef] [PubMed]
- Masroor, S. Collateral damage of COVID-19 pandemic: Delayed medical care. J. Card Surg. 2020, 35, 1345–1347. [Google Scholar] [CrossRef]
- Feral-Pierssens, A.L.; Claret, P.G.; Chouihed, T. Collateral damage of the COVID-19 outbreak: Expression of concern. Eur. J. Emerg. Med. 2020, 27, 233–234. [Google Scholar] [CrossRef]
- Rosenbaum, L. The untold toll–the pandemic’s effects on patients without COVID-19. N. Engl. J. Med. 2020, 382, 2368–2371. [Google Scholar] [CrossRef] [PubMed]
- Sud, A.; Torr, B.; Jones, M.E.; Broggio, J.; Scott, S.; Loveday, C.; Garrett, A.; Gronthoud, F.; Nicol, D.L.; Jhanji, S.; et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: A modelling study. Lancet Oncol. 2020, 21, 1035–1044. [Google Scholar] [CrossRef]
- Zhang, Y.; Wen, J.; Alamgir, M.; Xie, J.; Jing, H.; Fang, M.; Wang, J.; Zhang, M.; Meng, Z.; Yang, L.; et al. Impact of the COVID-19 pandemic on inpatient dermatology: A multicentre study from Hubei, China. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e179–e181. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chen, F.; Wang, Z.; Feng, W.; Liu, Y.; Wang, Y.; Song, H. Reductions in hospital admissions and delays in acute stroke care during the pandemic of COVID-19. Front. Neurol. 2020, 11, 584734. [Google Scholar] [CrossRef]
- Luo, Z.J.; Li, S.L.; Li, N.; Li, Y.C.; Zhang, Y.; Cao, Z.X.; Ma, Y.M. Assessment of pediatric outpatient visits for notifiable infectious diseases in a university hospital in Beijing during COVID-19. JAMA Netw. Open 2020, 3, e2019224. [Google Scholar] [CrossRef]
- Xiang, D.; Xiang, X.; Zhang, W.; Yi, S.; Zhang, J.; Gu, X.; Xu, Y.; Huang, K.; Su, X.; Yu, B.; et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J. Am. Coll. Cardiol. 2020, 76, 1318–1324. [Google Scholar] [CrossRef]
- National Bureau of Statistics of China. Main Data of the Seventh National Population Census; National Bureau of Statistics of China: Beijing, China, 2021; (In Chinese). Available online: http://www.stats.gov.cn/xxgk/jd/sjjd2020/202105/t20210511_1817280.html (accessed on 2 March 2022).
- Center for Health Statistics and Information of China. An Analysis Report of National Health Services Survey in China, 2018; Peking Union Medical College Press: Peking, China, 2021. (In Chinese)
- Wang, H.; Zhang, M.; Li, R.; Zhong, O.; Johnstone, H.; Zhou, H.; Xue, H.; Sylvia, S.; Boswell, M.; Loyalka, P.; et al. Tracking the effects of COVID-19 in rural China over time. Int. J. Equity Health 2021, 20, 35. [Google Scholar] [CrossRef] [PubMed]
- Bliznashka, L.; Ahun, M.N.; Velthausz, D.; Donco, R.; Karuskina-Drivdale, S.; Pinto, J.; Yousafzai, A.K.; Jeong, J. Effects of COVID-19 on child health services utilisation and delivery in rural Mozambique: A qualitative study. Health Policy Plan 2022, 37, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.R.; Sunuwar, D.R.; Shah, S.K.; Karki, K.; Sah, L.K.; Adhikari, B.; Sah, R.K. Impact of COVID-19 on health services utilization in Province-2 of Nepal: A qualitative study among community members and stakeholders. BMC Health Serv. Res. 2021, 21, 174. [Google Scholar] [CrossRef] [PubMed]
- Glenister, K.M.; Ervin, K.; Podubinski, T. Detrimental health behaviour changes among females living in rural areas during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 722. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of China. China Health Statistical Yearbook 2020; Peking Union Medical College Press: Beijing, China, 2020. (In Chinese)
- Mao, W.H.; Chen, W. Improving Health System Efficiency: China: The Zero Mark-Up for Essential Medicines at Primary Level Facilities; World Health Organization: Geneva, Switzerland, 2015.
- Lu, W.R.; Wang, W.J.; Li, C.; Xiong, H.G.; Ma, Y.L.; Luo, M.; Peng, H.Y.; Mao, Z.F.; Yin, P. Identification of factors influencing out-of-county hospitalizations in the New Cooperative Medical Scheme. Curr. Med. Sci. 2019, 39, 843–851. [Google Scholar] [CrossRef]
- Jiang, X.; Wei, W.; Wang, S.; Zhang, T.; Lu, C. Effects of COVID-19 on urban population flow in China. Int. J. Environ. Res. Public Health 2021, 18, 1617. [Google Scholar] [CrossRef]
- Ministry of Civil Affairs of China. Administrative Divisions of China; Ministry of Civil Affairs of China: Beijing, China, 2020. (In Chinese)
- Jandoc, R.; Burden, A.M.; Mamdani, M.; Lévesque, L.E.; Cadarette, S.M. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J. Clin. Epidemiol. 2015, 68, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.T.; Stanley, J.C. Experimental and Quasiexperimental Designs for Research; Houghton Mifflin: Boston, MA, USA, 1963. [Google Scholar]
- Lopez, B.J.; Cummins, S.; Gasparrini, A. The use of controls in interrupted time series studies of public health interventions. Int. J. Epidemiol. 2018, 47, 2082–2093. [Google Scholar] [CrossRef]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision; World Health Organization: Geneva, Switzerland, 2021.
- Yang, Z.; Hardin, J.W.; Addy, C.L.; Vuong, Q.H. Testing approaches for overdispersion in poisson regression versus the generalized poisson model. Biom. J. Biom. Z. 2007, 49, 565–584. [Google Scholar] [CrossRef]
- Newey, W.K.; West, K.D.; Кеннет, Д.В. A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Appl. Econom. 2014, 55, 124–132. [Google Scholar] [CrossRef]
- Li, X.; Krumholz, H.M.; Yip, W.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Li, C.; Lu, J.; Su, M.; et al. Quality of primary health care in China: Challenges and recommendations. Lancet 2020, 395, 1802–1812. [Google Scholar] [CrossRef]
- Du, Z.; You, H.; Zhou, H.; Wang, X.; Xu, J.; Li, Y.; Li, S.; Ma, L.; Gu, J.; Hao, Y. Difficulties encountered by public health workers in COVID-19 outbreak: A cross-sectional study based on five provinces. BMC Health Serv. Res. 2021, 21, 656. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yin, Z.; Xie, Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int. J. Equity Health 2014, 13, 34. [Google Scholar] [CrossRef] [PubMed]
- Musselwhite, C.; Avineri, E.; Susilo, Y. Editorial JTH 16 -The Coronavirus Disease COVID-19 and implications for transport and health. J. Transp. Health 2020, 16, 100853. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.U.G.; Yang, C.H.; Gutierrez, B.; Wu, C.H.; Klein, B.; Pigott, D.M.; du Plessis, L.; Faria, N.R.; Li, R.; Hanage, W.P.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Chen, Y.; Yu, M.; Zhong, J.; Hu, R.; Chen, X.; Wang, C.; Xie, K.; Eggleston, K. The effects of chronic disease management in primary health care: Evidence from rural China. J. Health Econ. 2021, 80, 102539. [Google Scholar] [CrossRef] [PubMed]
- Jiaqi, X.; Shuxian, W.; Linlin, Y.; Li, L.; Wen, C. Does China’s universal two-child policy affect contraceptive use among internal migrant women in China? Evidence based on panel data. Contraception 2022, 105, 7–13. [Google Scholar] [CrossRef]
- National Bureau of Statistics of China. Press Conference for Main Data of the Seventh National Population Census; National Bureau of Statistics of China: Beijing, China, 2021; (In Chinese). Available online: http://www.stats.gov.cn/ztjc/zdtjgz/zgrkpc/dqcrkpc/ggl/202105/t20210519_1817693.html (accessed on 16 March 2022).
- National Bureau of Statistics of China. The National Economy Will Continue to Recover in 2021 and the Expected Development Goals Will Be Well Accomplished; National Bureau of Statistics of China: Beijing, China, 2022. (In Chinese)
- Abdel-Moneim, A. COVID-19 pandemic and male fertility: Clinical manifestations and pathogenic mechanisms. Biochemistry 2021, 86, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Lu, H.; Zhang, Q.; Li, X.; Wang, T.; Liu, Q.; Yang, Q.; Qiang, L. Impact of COVID-19 on female fertility: A systematic review and meta-analysis protocol. BMJ Open 2021, 11, e045524. [Google Scholar] [CrossRef]
- Hossain, M.M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Res 2020, 9, 636. [Google Scholar] [CrossRef] [PubMed]
- Kola, L.; Kohrt, B.A.; Hanlon, C.; Naslund, J.A.; Sikander, S.; Balaji, M.; Benjet, C.; Cheung, E.Y.L.; Eaton, J.; Gonsalves, P.; et al. COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. Lancet Psychiatry 2021, 8, 535–550. [Google Scholar] [CrossRef]
- Tuna, O.; Enez, D.A.; Tarakcioglu, M.C.; Aksoy, U.M. COVID-19 positive psychiatry inpatient unit: A unique experience. Asia Pac. Psychiatry 2020, 12, e12410. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, F. South Africa’s Mental Health Care Falls by Wayside during Pandemic; The Voice of America: Washington, DC, USA, 2020. [Google Scholar]
- Xiong, J.Q.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Carek, P.J.; Laibstain, S.E.; Carek, S.M. Exercise for the Treatment of Depression and Anxiety. Int. J. Psychiatry Med. 2011, 41, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sanchez-Villegas, A.; Kivimaki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Ortuno Sanchez-Pedreno, F.; Van der Does, W.; Angel Martinez-Gonzalez, M. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health Action Plan 2013–2020; WHO Press: Geneva, Switzerland, 2013.
- World Health Organization. Maintaining Essential Health Services: Operational Guidance for the COVID-19 Context: Interim Guidance, 1 June 2020; World Health Organization: Geneva, Switzerland, 2020.
- Carswell, K.; Harper-Shehadeh, M.; Watts, S.; Van’T, H.E.; Abi, R.J.; Heim, E.; Wenger, A.; van Ommeren, M. Step-by-Step: A new WHO digital mental health intervention for depression. Mhealth 2018, 4, 34. [Google Scholar] [CrossRef]
- Sachs, J.D.; Schmidt-Traub, G.; Mazzucato, M.; Messner, D.; Nakicenovic, N.; Rockstrom, J. Six transformations to achieve the Sustainable Development Goals. Nat. Sustain. 2019, 2, 805–814. [Google Scholar] [CrossRef]
- Gurzawska-Comis, K.; Becker, K.; Brunello, G.; Gurzawska, A.; Schwarz, F. Recommendations for dental care during COVID-19 pandemic. J. Clin. Med. 2020, 9, 1833. [Google Scholar] [CrossRef] [PubMed]
- Safadi, K.; Kruger, J.M.; Chowers, I.; Solomon, A.; Amer, R.; Aweidah, H.; Frenkel, S.; Mechoulam, H.; Anteby, I.; Ben, E.H.; et al. Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol. 2020, 5, e000487. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Viana, A., Jr.; Wang, Y.; Wei, H.Q.; Yan, A.H.; Capasso, R. Otolaryngology during COVID-19: Preventive care and precautionary measures. Am. J. Otolaryngol. 2020, 41, 102508. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.M.; Wu, M.Y.; Lu, J.M.; Li, T.Z.; Shen, P.; Tang, M.L.; Jin, M.J.; Lin, H.B.; Shui, L.M.; Chen, K.; et al. Effect of COVID-19 on hospital visits in Ningbo, China: An interrupted time-series analysis. Int. J. Qual. Health Care 2021, 33, mzab078. [Google Scholar] [CrossRef] [PubMed]
- Napoli, P.E.; Nioi, M.; D’Aloja, E.; Fossarello, M. Safety recommendations and medical liability in ocular surgery during the COVID-19 pandemic: An unsolved dilemma. J. Clin. Med. 2020, 9, 1403. [Google Scholar] [CrossRef] [PubMed]
- Rajendrababu, S.; Durai, I.; Mani, I.; Ramasamy, K.S.; Shukla, A.G.; Robin, A.L. Urgent and emergent glaucoma care during the COVID-19 pandemic: An analysis at a tertiary care hospital in South India. Indian J. Ophthalmol. 2021, 69, 2215–2221. [Google Scholar] [CrossRef] [PubMed]
- Naderi, K.; Maubon, L.; Jameel, A.; Patel, D.S.; Gormley, J.; Shah, V.; Lai, L.; Low, S.; Verma, S.; Robbie, S.; et al. Attitudes to cataract surgery during the COVID-19 pandemic: A patient survey. Eye 2020, 34, 2161–2162. [Google Scholar] [CrossRef]


| Implementation Period | Control Period | |||||
|---|---|---|---|---|---|---|
| Pre-COVID (a) | COVID-Impacted (b) | Change 1 (%): (b − a)/a | Equivalent Pre-COVID (c) | Equivalent COVID-Impacted (d) | Change 2 (%): (d − c)/c | |
| Overall | 3599 (171) | 2657 (339) | −26.18 | 2677 (245) | 3156 (328) | 17.89 |
| Gender | ||||||
| Female | 1767 (125) | 1363 (201) | −22.90 | 1164 (131) | 1474 (167) | 26.64 |
| Male | 1832 (60) | 1294 (147) | −29.35 | 1514 (134) | 1682 (170) | 11.16 |
| Age (years) | ||||||
| 0–14 | 471 (67) | 222 (69) | −52.82 | 368 (81) | 421 (84) | 14.62 |
| 15–44 | 816 (57) | 629 (67) | −22.92 | 805 (84) | 812 (83) | 0.84 |
| 45–59 | 565 (30) | 402 (55) | −28.75 | 345 (46) | 449 (66) | 30.40 |
| ≥60 | 1747 (109) | 1403 (212) | −19.70 | 1160 (142) | 1474 (184) | 27.04 |
| Hospital levels | ||||||
| Primary healthcare facilities | 1035 (90) | 778 (224) | −24.88 | 844 (115) | 1030 (137) | 22.00 |
| Secondary hospitals | 2564 (136) | 1879 (269) | −26.71 | 1833 (159) | 2127 (223) | 16.00 |
| Tertiary hospitals | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| Disease classification (ICD–10 code) | ||||||
| A00–B99 | 114 (30) | 67 (24) | −41.14 | 81 (24) | 92 (26) | 14.16 |
| C00–D48 | 169 (17) | 147 (23) | −13.01 | 94 (15) | 120 (19) | 27.78 |
| D50–D89 | 53 (8) | 45 (9) | −15.77 | 17 (4) | 48 (9) | 177.87 |
| E00–E90 | 104 (16) | 88 (25) | −15.36 | 30 (7) | 77 (19) | 160.22 |
| F00–F99 | 11 (2) | 8 (3) | −33.63 | 4 (2) | 7 (3) | 73.21 |
| G00–G99 | 151 (21) | 115 (24) | −23.95 | 37 (9) | 98 (21) | 165.86 |
| H00–H59 | 75 (10) | 62 (21) | −17.08 | 76 (27) | 70 (27) | −7.28 |
| H60–H95 | 15 (5) | 9 (3) | −40.72 | 16 (6) | 16 (4) | 0.53 |
| I00–I99 | 776 (53) | 606 (76) | −21.96 | 514 (65) | 683 (104) | 32.81 |
| J00–J99 | 698 (114) | 341 (102) | −51.20 | 500 (114) | 587 (115) | 17.46 |
| K00–K93 | 359 (44) | 199 (25) | −44.65 | 230 (43) | 352 (35) | 53.12 |
| L00–L99 | 43 (10) | 39 (13) | −10.14 | 25 (9) | 31 (8) | 24.14 |
| M00–M99 | 226 (27) | 153 (32) | −32.09 | 173 (27) | 192 (30) | 11.22 |
| N00–N99 | 209 (20) | 165 (22) | −21.34 | 103 (16) | 161 (39) | 56.32 |
| O00–O99 | 287 (32) | 243 (76) | −15.39 | 465 (77) | 322 (33) | −30.80 |
| P00–P96 | 50 (10) | 135 (73) | 171.26 | 53 (13) | 51 (9) | −4.14 |
| Q00–Q99 | 11 (2) | 11 (4) | 1.08 | 4 (2) | 8 (2) | 120.08 |
| R00–R99 | 46 (11) | 37 (7) | −21.18 | 100 (28) | 56 (12) | −43.97 |
| S00–T98 | 154 (13) | 137 (21) | −11.34 | 94 (18) | 126 (17) | 34.68 |
| Z00–Z99 | 39 (7) | 41 (7) | 5.96 | 33 (7) | 47 (15) | 40.49 |
| Not applicable | 9 (4) | 12 (6) | 32.31 | 31 (11) | 13 (7) | −56.21 |
| Implementation Period | Control Period | |||||
|---|---|---|---|---|---|---|
| Pre-COVID (a) | COVID-Impacted (b) | Change 1 (%): (b − a)/a | Equivalent Pre-COVID (c) | Equivalent COVID-Impacted (d) | Change 2 (%): (d − c)/c | |
| Overall | 1698 (112) | 1372 (210) | −19.18 | 1643 (186) | 1734 (243) | 5.53 |
| Gender | ||||||
| Female | 781 (59) | 645 (115) | −17.39 | 775 (89) | 797 (125) | 2.90 |
| Male | 917 (60) | 727 (98) | −20.70 | 868 (109) | 936 (125) | 7.87 |
| Age (years) | ||||||
| 0–14 | 183 (63) | 124 (77) | −32.20 | 187 (33) | 211 (32) | 13.04 |
| 15–44 | 458 (94) | 433 (208) | −5.37 | 487 (60) | 487 (57) | 0.09 |
| 45–59 | 369 (46) | 355 (139) | −3.87 | 328 (40) | 355 (55) | 8.44 |
| ≥60 | 688 (133) | 460 (165) | −33.10 | 642 (91) | 680 (130) | 5.99 |
| Hospital levels | ||||||
| Primary healthcare facilities | 111 (94) | 30 (56) | −73.13 | 110 (19) | 78 (36) | −28.77 |
| Secondary hospitals | 515 (191) | 279 (413) | −45.87 | 207 (48) | 472 (131) | 127.84 |
| Tertiary hospitals | 1019 (379) | 1047 (514) | −2.80 | 1204 (144) | 1118 (124) | −7.17 |
| Disease classification (ICD–10 codes) | ||||||
| A00–B99 | 38 (8) | 19 (5) | −48.76 | 42 (10) | 41 (10) | −4.03 |
| C00–D48 | 201 (17) | 185 (32) | −7.89 | 170 (27) | 161 (31) | −5.32 |
| D50–D89 | 23 (5) | 18 (3) | −20.57 | 31 (7) | 23 (5) | −26.74 |
| E00–E90 | 47 (7) | 37 (9) | −21.58 | 40 (4) | 44 (11) | 9.81 |
| F00–F99 | 74 (25) | 127 (27) | 72.65 | 42 (12) | 55 (12) | 29.18 |
| G00–G99 | 68 (16) | 64 (11) | −6.20 | 33 (11) | 42 (10) | 26.13 |
| H00–H59 | 84 (31) | 56 (21) | −33.85 | 96 (45) | 66 (24) | −30.89 |
| H60–H95 | 12 (6) | 8 (3) | −33.88 | 13 (4) | 18 (6) | 36.21 |
| I00–I99 | 200 (24) | 158 (23) | −20.83 | 249 (35) | 255 (44) | 2.34 |
| J00–J99 | 211 (38) | 104 (28) | −50.85 | 196 (35) | 214 (38) | 9.53 |
| K00–K93 | 176 (16) | 137 (23) | −21.99 | 178 (25) | 180 (24) | 0.90 |
| L00–L99 | 17 (3) | 14 (4) | −14.54 | 13 (3) | 15 (4) | 19.60 |
| M00–M99 | 131 (30) | 89 (21) | −32.22 | 142 (25) | 205 (91) | 44.21 |
| N00–N99 | 154 (17) | 112 (26) | −27.22 | 142 (22) | 152 (25) | 7.07 |
| O00–O99 | 81 (10) | 74 (10) | −9.26 | 101 (13) | 94 (10) | −6.28 |
| P00–P96 | 41 (7) | 33 (6) | −18.94 | 32 (7) | 37 (8) | 15.57 |
| Q00–Q99 | 14 (6) | 11 (7) | −21.58 | 11 (7) | 11 (5) | −1.63 |
| R00–R99 | 16 (3) | 14 (5) | −14.82 | 20 (8) | 15 (4) | −24.91 |
| S00–T98 | 57 (7) | 48 (11) | −15.07 | 48 (10) | 55 (10) | 14.02 |
| Z00–Z99 | 51 (12) | 59 (12) | 16.16 | 37 (5) | 46 (23) | 25.54 |
| Not applicable | 3 (3) | 5 (2) | 65.90 | 6 (4) | 4 (3) | −26.15 |
| Implementation Period | Control Period | |||||
|---|---|---|---|---|---|---|
| Pre-COVID (a) | COVID-Impacted (b) | Change 1 (%): (b − a)/a | Equivalent Pre-COVID (c) | Equivalent COVID-Impacted (d) | Change 2 (%): (d − c)/c | |
| Overall | 974 (116) | 829 (166) | −14.89 | 771 (176) | 912 (221) | 18.26 |
| Gender | ||||||
| Female | 476 (46) | 417 (74) | −12.33 | 371 (88) | 434 (104) | 17.04 |
| Male | 498 (72) | 412 (94) | −17.33 | 400 (90) | 478 (119) | 19.39 |
| Age (years) | ||||||
| 0–14 | 102 (14) | 82 (16) | −18.87 | 72 (27) | 88 (31) | 22.98 |
| 15–44 | 252 (34) | 200 (40) | −20.42 | 243 (52) | 259 (61) | 6.63 |
| 45–59 | 327 (42) | 286 (59) | −12.60 | 248 (64) | 307 (76) | 23.48 |
| ≥60 | 294 (33) | 260 (57) | −11.33 | 209 (40) | 258 (62) | 23.95 |
| Hospital levels | ||||||
| Primary healthcare facilities | 17 (3) | 14 (4) | −16.04 | 10 (4) | 13 (5) | 35.64 |
| Secondary hospitals | 175 (28) | 155 (35) | −11.26 | 130 (47) | 159 (57) | 22.72 |
| Tertiary hospitals | 775 (91) | 655 (134) | −15.43 | 625 (131) | 733 (166) | 17.25 |
| Disease classification (ICD-10 codes) | ||||||
| A00–B99 | 18 (5) | 10 (4) | −44.84 | 19 (10) | 19 (6) | 1.66 |
| C00–D48 | 271 (21) | 247 (45) | −8.83 | 214 (24) | 261 (47) | 21.98 |
| D50–D89 | 13 (3) | 8 (3) | −35.43 | 7 (5) | 9 (4) | 25.00 |
| E00–E90 | 22 (4) | 17 (5) | −23.42 | 16 (6) | 20 (9) | 28.30 |
| F00–F99 | 12 (5) | 9 (4) | −22.41 | 13 (6) | 14 (5) | 6.32 |
| G00–G99 | 23 (6) | 20 (5) | −13.04 | 22 (10) | 21 (8) | −2.90 |
| H00–H59 | 19 (6) | 16 (6) | −19.73 | 14 (6) | 16 (6) | 9.62 |
| H60–H95 | 9 (3) | 6 (2) | −34.32 | 4 (2) | 7 (4) | 64.97 |
| I00–I99 | 134 (26) | 123 (33) | −7.87 | 97 (21) | 121 (37) | 25.39 |
| J00–J99 | 80 (13) | 47 (11) | −41.22 | 51 (19) | 72 (23) | 41.31 |
| K00–K93 | 75 (12) | 65 (17) | −13.09 | 64 (17) | 77 (25) | 19.90 |
| L00–L99 | 8 (2) | 6 (3) | −25.75 | 6 (3) | 5 (4) | −7.27 |
| M00–M99 | 48 (9) | 35 (8) | −27.52 | 41 (8) | 41 (12) | 0.52 |
| N00–N99 | 79 (19) | 54 (19) | −31.37 | 68 (21) | 79 (21) | 16.90 |
| O00–O99 | 33 (6) | 28 (5) | −14.51 | 41 (11) | 40 (13) | −0.91 |
| P00–P96 | 11 (4) | 11 (4) | −2.36 | 10 (5) | 12 (4) | 22.24 |
| Q00–Q99 | 15 (4) | 13 (6) | −9.36 | 14 (5) | 12 (5) | −14.81 |
| R00–R99 | 21 (4) | 17 (5) | −17.13 | 19 (6) | 17 (6) | −10.43 |
| S00–T98 | 23 (6) | 19 (5) | −17.58 | 22 (6) | 25 (10) | 14.88 |
| Z00–Z99 | 61 (8) | 75 (16) | 24.26 | 29 (12) | 37 (16) | 27.45 |
| Not applicable | 2 (2) | 3 (2) | 104.76 | 2 (2) | 6 (4) | 214.29 |
| Variable | Coefficient | Within-County Area | Out-Of-County but Within-City Area | Out-of-City Area | |||
|---|---|---|---|---|---|---|---|
| Changes (%, 95% CI) | p | Changes (%, 95% CI) | p | Changes (%, 95% CI) | p | ||
| Time | β1 | −2.10 (−3.61, −0.57) | 0.007 | 0.05 (−1.17, 1.27) | 0.939 | 0.07 (−2.52, 2.65) | 0.961 |
| Phase | β2 | 24.22 (12.09, 36.34) | <0.001 | 10.03 (−0.76, 20.83) | 0.069 | −1.02 (−19.66, 17.62) | 0.914 |
| Post | β3 | 3.17 (1.63, 4.66) | <0.001 | 0.00 (−1.04, 1.04) | 0.997 | 3.73 (1.26, 6.21) | 0.003 |
| Group | β4 | 27.79 (24.92, 30.64) | <0.001 | 5.77 (3.03, 8.52) | <0.001 | 24.52 (19.37, 29.67) | <0.001 |
| Group × Time | β5 | 0.47 (−0.21, 1.06) | 0.192 | −0.55 (−1.27, 0.16) | 0.129 | −0.10 (−0.97, 0.77) | 0.817 |
| Group × Phase | β6 | −43.77 (−57.78, −29.72) | <0.001 | −38.28 (−46.38, −30.17) | <0.001 | −24.28 (−32.17, −16.38) | <0.001 |
| Group × Post | β7 | −1.11 (−2.47, 0.27) | 0.114 | 2.81 (1.96, 3.66) | <0.001 | −1.04 (−2.52, 0.44) | 0.167 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhong, W.; Yin, R.; Pan, Y.; Zhang, X.; Renzaho, A.M.N.; Ling, L.; Li, X.; Chen, W. Long-Term Impact of COVID-19 on Hospital Visits of Rural Residents in Guangdong, China: A Controlled Interrupted Time Series Study. Int. J. Environ. Res. Public Health 2022, 19, 13259. https://doi.org/10.3390/ijerph192013259
Zhong W, Yin R, Pan Y, Zhang X, Renzaho AMN, Ling L, Li X, Chen W. Long-Term Impact of COVID-19 on Hospital Visits of Rural Residents in Guangdong, China: A Controlled Interrupted Time Series Study. International Journal of Environmental Research and Public Health. 2022; 19(20):13259. https://doi.org/10.3390/ijerph192013259
Chicago/Turabian StyleZhong, Wenfang, Rong Yin, Yan Pan, Xiangliang Zhang, Andre M. N. Renzaho, Li Ling, Xingge Li, and Wen Chen. 2022. "Long-Term Impact of COVID-19 on Hospital Visits of Rural Residents in Guangdong, China: A Controlled Interrupted Time Series Study" International Journal of Environmental Research and Public Health 19, no. 20: 13259. https://doi.org/10.3390/ijerph192013259
APA StyleZhong, W., Yin, R., Pan, Y., Zhang, X., Renzaho, A. M. N., Ling, L., Li, X., & Chen, W. (2022). Long-Term Impact of COVID-19 on Hospital Visits of Rural Residents in Guangdong, China: A Controlled Interrupted Time Series Study. International Journal of Environmental Research and Public Health, 19(20), 13259. https://doi.org/10.3390/ijerph192013259






