When Lights Can Breathe: Investigating the Influences of Breathing Lights on Users’ Emotion
Abstract
1. Introduction
1.1. Light Environment
1.2. Breathing
1.3. Research Question
2. Material and Methods
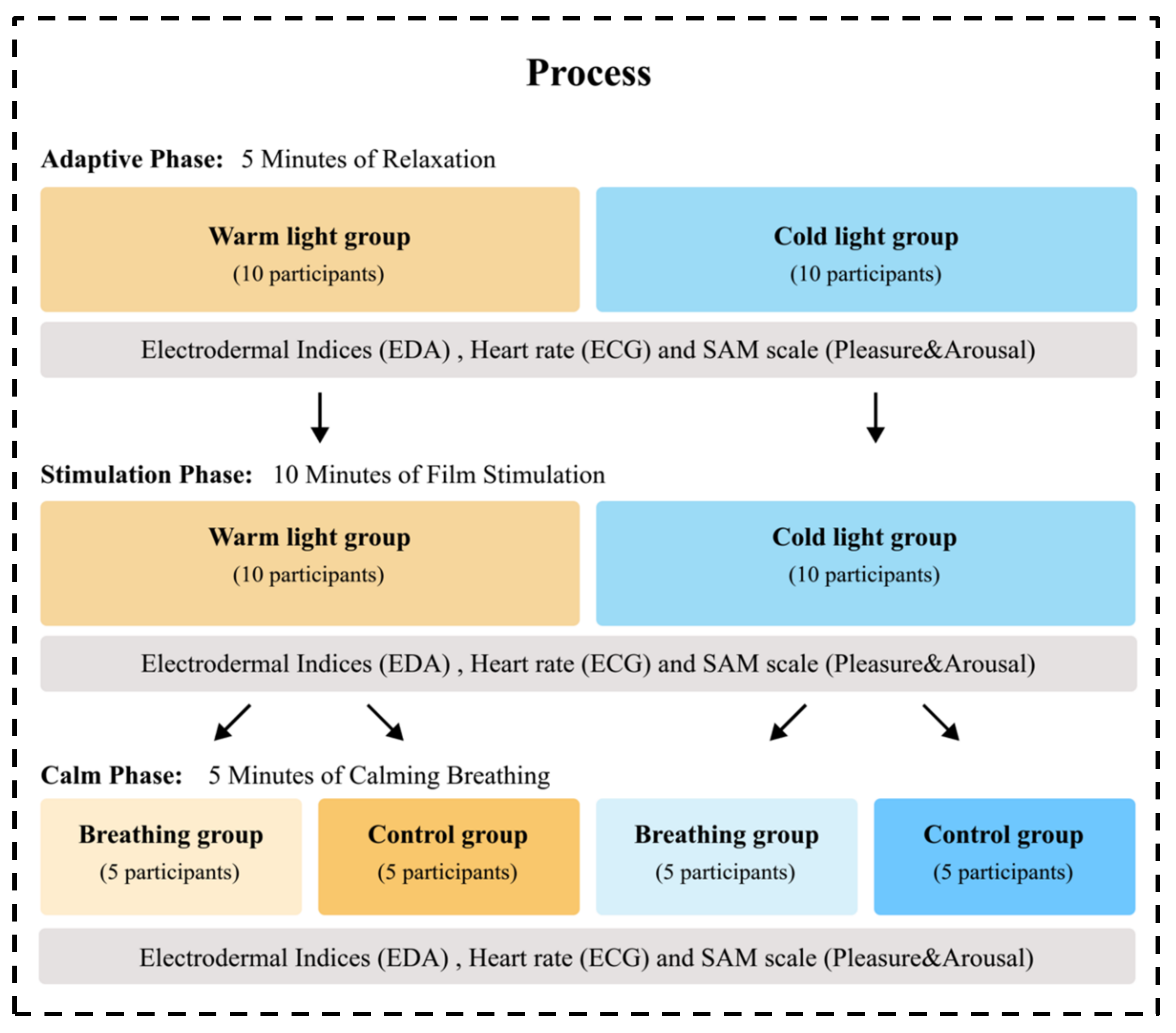
2.1. Participants and Design
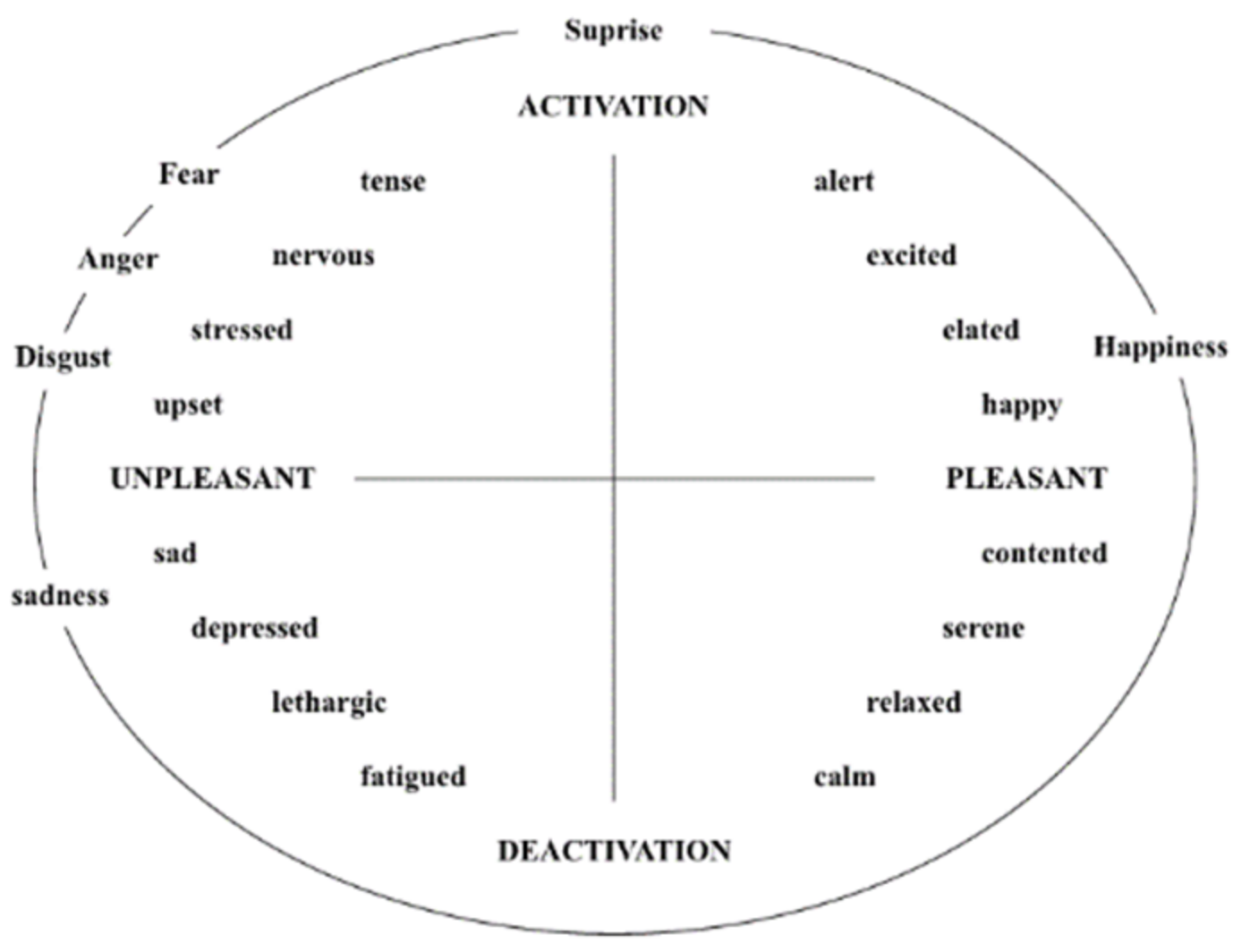
2.2. Measurements
2.2.1. Physiological Monitors
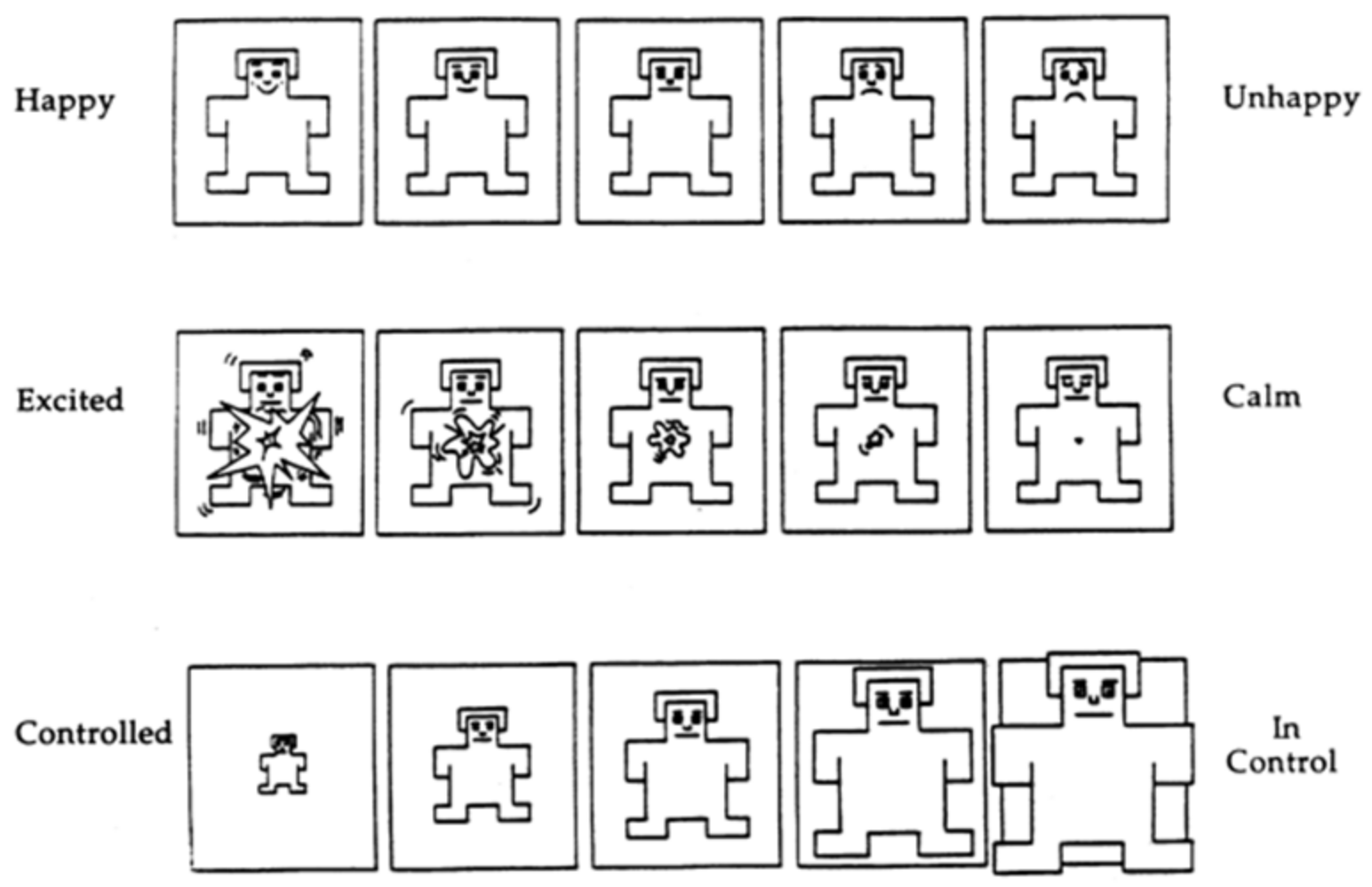
2.2.2. Subjective Mood Scale
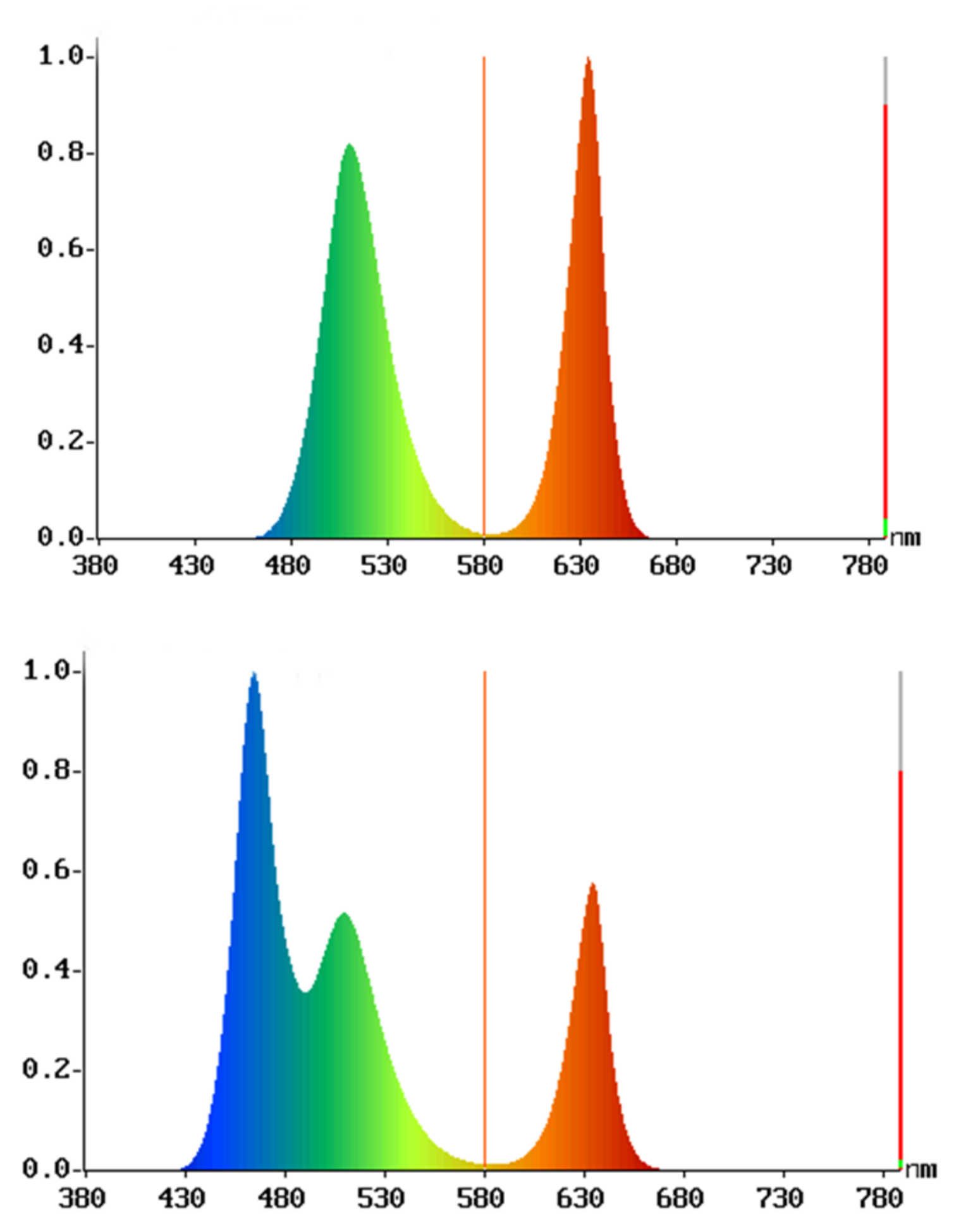
2.3. Emotion Arousal Stimuli Creation
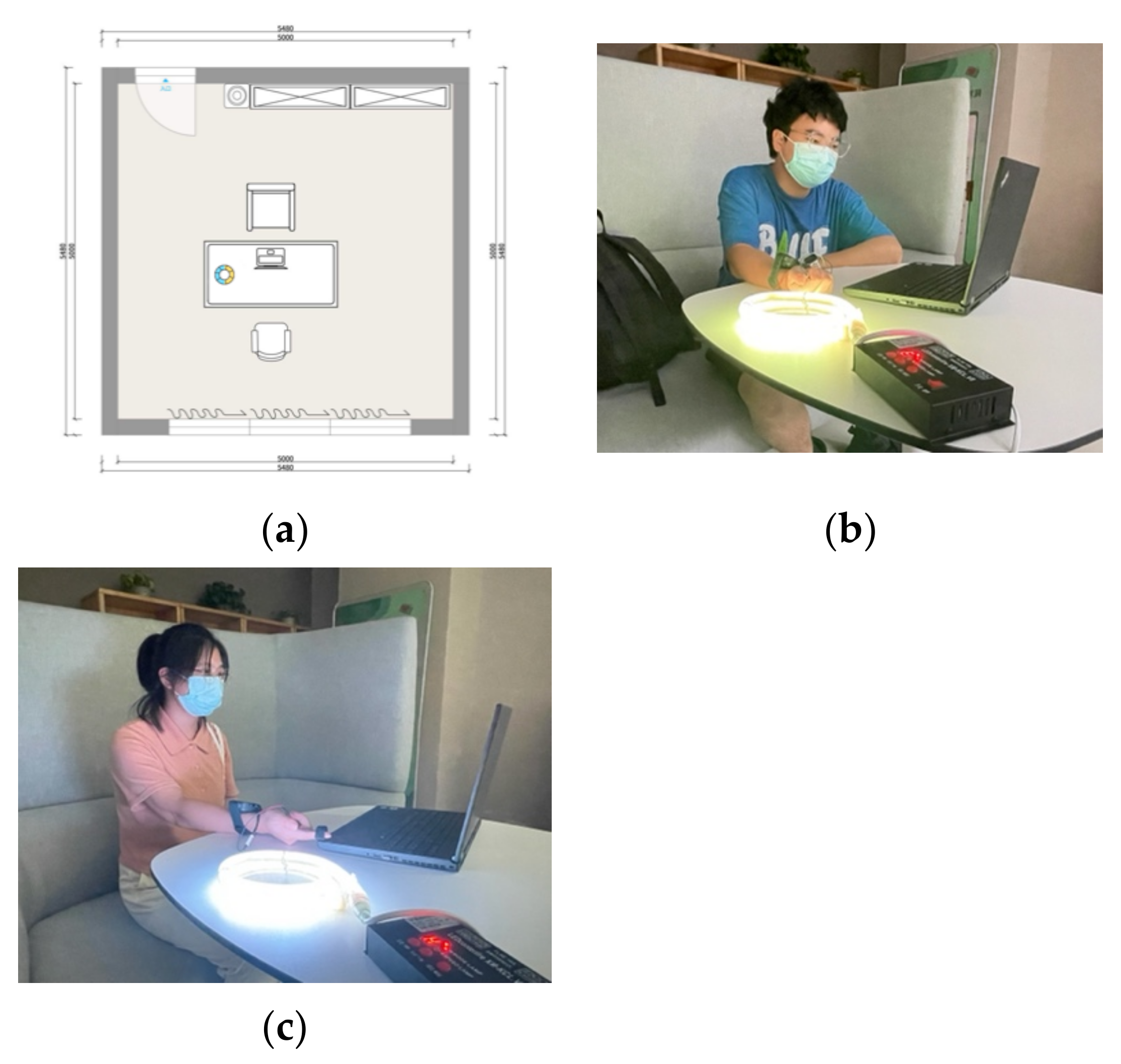
2.4. Experimental Setting
2.5. Procedure
2.6. Data Analysis
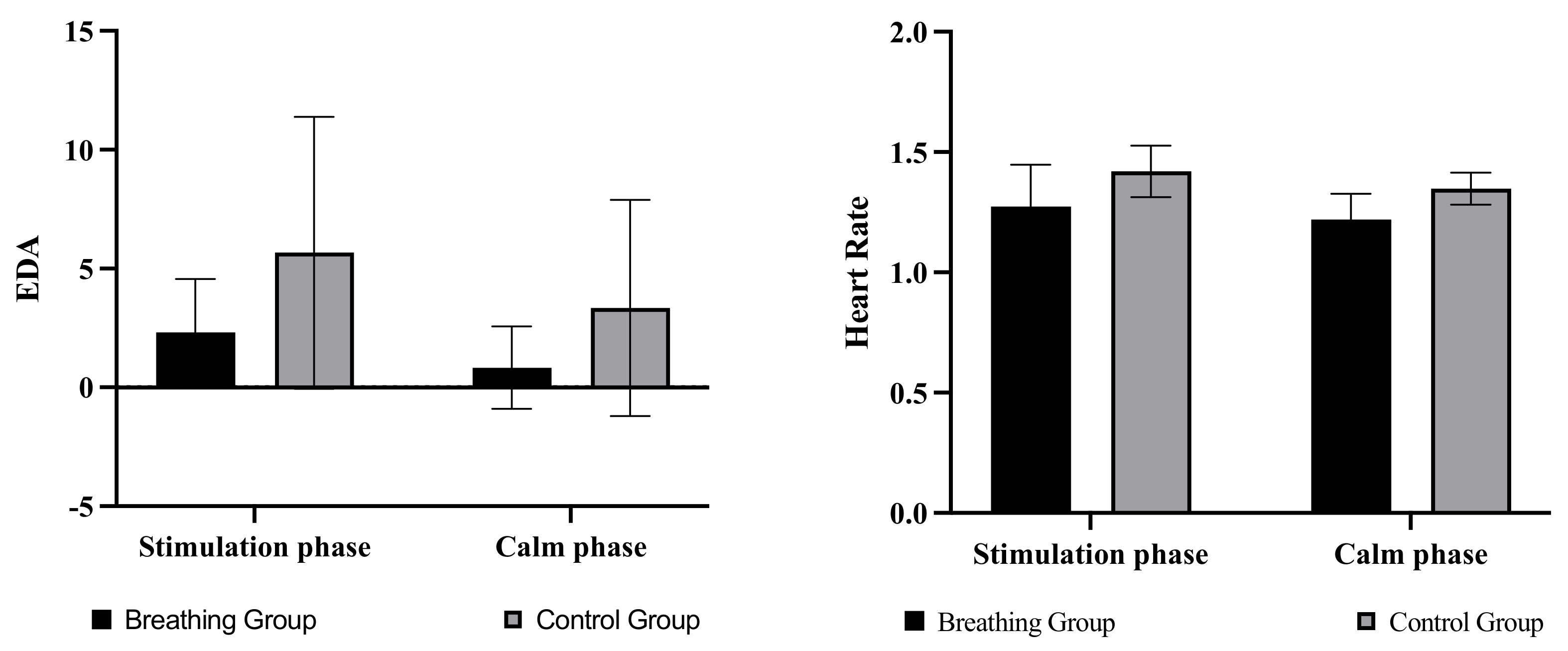
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brainard, G.C.; Hanifin, J.P.; Greeson, J.M.; Byrne, B.; Glickman, G.; Gerner, E.; Rollag, M.D. Action Spectrum for Melatonin Regulation in Humans: Evidence for a Novel Circadian Photoreceptor. J. Neurosci. 2001, 21, 6405–6412. [Google Scholar] [CrossRef] [PubMed]
- Sahin, L.; Figueiro, M.G. Alerting effects of short-wavelength (blue) and long-wavelength (red) lights in the afternoon. Physiol. Behav. 2013, 116–117, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Badia, P.; Myers, B.; Boecker, M.; Culpepper, J.; Harsh, J.R. Bright light effects on body temperature, alertness, EEG and behavior. Physiol. Behav. 1991, 50, 583–588. [Google Scholar] [CrossRef]
- Kim, D.H.; Mansfield, K. Creating positive atmosphere and emotion in an office-like environment: A methodology for the lit environment. Build. Environ. 2021, 194, 107686. [Google Scholar] [CrossRef]
- Chao, W.-C.; Hong, L.-Y.; Hsieh, M.-C.; Wang, E.M.-Y.; Yang, C.-C.; Su, L.-C. Effect of correlated colour temperature and illuminance levels on user’s visual perception under LED lighting in Taiwan. Ergonomics 2020, 63, 175–190. [Google Scholar] [CrossRef] [PubMed]
- Schielke, T. Influence of Lighting Design on Marketing Communication. Leukos 2015, 11, 109–124. [Google Scholar] [CrossRef]
- Su, B.; Hu, J.; Zeng, J.; Wang, R. Traffic Safety Improvement via Optimizing Light Environment in Highway Tunnels. Int. J. Environ. Res. Public Health 2022, 19, 8517. [Google Scholar] [CrossRef] [PubMed]
- Arouca, A.M.; Aleixo, V.E.D.; Vieira, M.L.; Talhavini, M.; Weber, I.T. White Light-Photolysis for the Removal of Polycyclic Aromatic Hydrocarbons from Proximity Firefighting Protective Clothing. Int. J. Environ. Res. Public Health 2022, 19, 10054. [Google Scholar] [CrossRef]
- Wen, P.; Tan, F.; Wu, M.; Cai, Q.; Xu, R.; Zhang, X.; Wang, Y.; Khan, M.S.A.; Chen, W.; Hu, X. The effects of different bedroom light environments in the evening on adolescents. Build. Environ. 2021, 206, 108321. [Google Scholar] [CrossRef]
- Van Bommel, W.J.M.; van den Beld, G.J. Lighting for work: A review of visual and biological effects. Light. Res. Technol. 2004, 36, 255–266. [Google Scholar] [CrossRef]
- van Bommel, W.J.M. Non-visual biological effect of lighting and the practical meaning for lighting for work. Appl. Ergon. 2006, 37, 461–466. [Google Scholar] [CrossRef]
- van Bommel, W. Visual, Biological and Emotional Aspects of Lighting: Recent New Findings and their Meaning for Lighting Practice. Leukos 2005, 2, 7–11. [Google Scholar] [CrossRef]
- Vigh, B.; Manzano, M.J.; Zádori, A.; Frank, C.L.; Lukáts, A.; Röhlich, P.; Szél, A.; Dávid, C. Nonvisual photoreceptors of the deep brain, pineal organs and retina. Histol. Histopathol. 2002, 17, 555–590. [Google Scholar] [CrossRef]
- Ferlazzo, F.; Piccardi, L.; Burattini, C.; Barbalace, M.; Giannini, A.M.; Bisegna, F. Effects of new light sources on task switching and mental rotation performance. J. Environ. Psychol. 2014, 39, 92–100. [Google Scholar] [CrossRef]
- Sahin, L.; Wood, B.M.; Plitnick, B.; Figueiro, M.G. Daytime light exposure: Effects on biomarkers, measures of alertness, and performance. Behav. Brain Res. 2014, 274, 176–185. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Sahin, L.; Roohan, C.; Kalsher, M.; Plitnick, B.; Rea, M.S. Effects of red light on sleep inertia. Nat. Sci. Sleep 2019, 11, 45–57. [Google Scholar] [CrossRef]
- Li, Y.; Ru, T.; Chen, Q.; Qian, L.; Luo, X.; Zhou, G. Effects of illuminance and correlated color temperature of indoor light on emotion perception. Sci. Rep. 2021, 11, 14351. [Google Scholar] [CrossRef]
- Czeisler, C.A.; Kronauer, R.E.; Allan, J.S.; Duffy, J.F.; Jewett, M.E.; Brown, E.N.; Ronda, J.M. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science 1989, 244, 1328–1333. [Google Scholar] [CrossRef]
- Lewy, A.J.; Sack, R.L. The Dim Light Melatonin Onset as a Marker for Orcadian Phase Position. Chronobiol. Int. 1989, 6, 93–102. [Google Scholar] [CrossRef]
- Aoki, H.; Yamada, N.; Ozeki, Y.; Yamane, H.; Kato, N. Minimum light intensity required to suppress nocturnal melatonin concentration in human saliva. Neurosci. Lett. 1998, 252, 91–94. [Google Scholar] [CrossRef]
- Mclntyre, I.M.; Norman, T.R.; Burrows, G.D.; Armstrong, S.M. Human Melatonin Suppression by Light is Intensity Dependent. J. Pineal Res. 1989, 6, 149–156. [Google Scholar] [CrossRef]
- Dijk, D.J.; Beersma, D.G.; Daan, S.; Lewy, A.J. Bright morning light advances the human circadian system without affecting NREM sleep homeostasis. Am. J. Physiol. Integr. Comp. Physiol. 1989, 256, R106–R111. [Google Scholar] [CrossRef]
- Dijk, D.-J.; Cajochen, C.; Borbély, A.A. Effect of a single 3-hour exposure to bright light on core body temperature and sleep in humans. Neurosci. Lett. 1991, 121, 59–62. [Google Scholar] [CrossRef]
- Drennan, M.; Kripke, D.F.; Gillin, J.C. Bright light can delay human temperature rhythm independent of sleep. Am. J. Physiol. Integr. Comp. Physiol. 1989, 257, R136–R141. [Google Scholar] [CrossRef]
- Leccese, F.; Salvadori, G.; Maccheroni, D.; Feltrin, F. Lighting and visual experience of artworks: Results of a study campaign at the National Museum of San Matteo in Pisa, Italy. J. Cult. Herit. 2020, 45, 254–264. [Google Scholar] [CrossRef]
- Shirani, A.; Louis, E.S. Illuminating Rationale and Uses for Light Therapy. J. Clin. Sleep Med. 2009, 5, 155–163. [Google Scholar] [CrossRef]
- Lewy, A.J.; Sack, R.L.; Miller, L.S.; Hoban, T.M. Antidepressant and Circadian Phase-Shifting Effects of Light. Science 1987, 235, 352–354. [Google Scholar] [CrossRef]
- Epperson, C.N.; Terman, M.; Terman, J.S.; Hanusa, B.H.; Oren, D.A.; Peindl, K.S.; Wisner, K.L. Ran-domized Clinical Trial of Bright Light Therapy for Antepartum Depression: Preliminary Findings. J. Clin. Psychiatry 2004, 65, 16604. [Google Scholar] [CrossRef]
- Lewy, A.J.; Sack, R.L. Light Therapy and Psychiatry. Proc. Soc. Exp. Biol. Med. 1986, 183, 11–18. [Google Scholar] [CrossRef]
- Onega, L.L.; Pierce, T.W.; Epperly, L. Bright Light Therapy to Treat Depression in Individuals with Mild/Moderate or Severe Dementia. Issues Ment. Health Nurs. 2018, 39, 370–373. [Google Scholar] [CrossRef]
- Avery, D.H.; Eder, D.N.; Bolte, M.A.; Hellekson, C.J.; Dunner, D.L.; Vitiello, M.V.; Prinz, P.N. Dawn simulation and bright light in the treatment of SAD: A controlled study. Biol. Psychiatry 2001, 50, 205–216. [Google Scholar] [CrossRef]
- Grahn, J.A. See what I hear? Beat perception in auditory and visual rhythms. Exp. Brain Res. 2012, 220, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, H.J.; Osborne, T.; Rea, M.; Peng, A.; Mareschal, D.; Kirkham, N.Z. Incidental category learning and cognitive load in a multisensory environment across childhood. Dev. Psychol. 2018, 54, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Yang, Y.; Cheng, P. The Investigation of Adoption of Voice-User Interface (VUI) in Smart Home Systems among Chinese Older Adults. Sensors 2022, 22, 1614. [Google Scholar] [CrossRef] [PubMed]
- Colavita, F.B. Human sensory dominance. Percept. Psychophys. 1974, 16, 409–412. [Google Scholar] [CrossRef]
- Repp, B.H.; Penel, A. Rhythmic movement is attracted more strongly to auditory than to visual rhythms. Psychol. Res. 2004, 68, 252–270. [Google Scholar] [CrossRef]
- Agarwal, A.; Yadav, G.; Gupta, D.; Tandon, M.; Singh, P.K.; Singh, U. The Role of a Flash of Light for Attenuation of Venous Cannulation Pain: A Prospective, Randomized, Placebo-Controlled Study. Anesth. Analg. 2008, 106, 814–816. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, M.; Makarem, J.; Rooyan, P. Effects of a flash of light in different colors on venous cannulation pain: A randomized, controlled trial. J. Clin. Anesth. 2013, 25, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Ståhl, A.; Jonsson, M.; Mercurio, J.; Karlsson, A.; Höök, K.; Banka Johnson, E.C. The Soma Mat and Breathing Light. In Proceedings of the 2016 CHI Con-Ference Extended Abstracts on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; pp. 305–308. [Google Scholar]
- Yamauchi, M.; Jacono, F.J.; Fujita, Y.; Kumamoto, M.; Yoshikawa, M.; Campanaro, C.K.; Loparo, K.A.; Strohl, K.P.; Kimura, H. Effects of environment light during sleep on autonomic functions of heart rate and breathing. Sleep Breath. 2014, 18, 829–835. [Google Scholar] [CrossRef]
- Bernardi, L.; Porta, C.; Gabutti, A.; Spicuzza, L.; Sleight, P. Modulatory effects of respiration. Auton. Neurosci. 2001, 90, 47–56. [Google Scholar] [CrossRef]
- Umezawa, A. Facilitation and Inhibition of Breathing during Changes in Emotion. In Respiration and Emotion; Haruki, Y., Homma, I., Umezawa, A., Masaoka, Y., Eds.; Springer: Tokyo, Japan, 2001. [Google Scholar] [CrossRef]
- Grossman, P. Respiration, Stress, and Cardiovascular Function. Psychophysiology 1983, 20, 284–300. [Google Scholar] [CrossRef]
- Cohen, H.D.; Goodenough, D.R.; Witkin, H.A.; Oltman, P.; Gould, H.; Shulman, E. The Effects of Stress on Components of the Respiration Cycle. Psychophysiology 1975, 12, 377–380. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, X.; Zhan, Q.; Yang, T.; Xia, S. Respiration-based emotion recognition with deep learning. Comput. Ind. 2017, 92–93, 84–90. [Google Scholar] [CrossRef]
- Levy, M.N.; DeGeest, H.; Zieske, H.; Levy, D. Effects of Respiratory Center Activity on the Heart. Circ. Res. 1966, 18, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Sroufe, L.A. Effects of depth and rate of breathing on heart rate and heart rate variability. Psychophysiology 1971, 8, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Harris, V.A.; Katkin, E.S.; Lick, J.R.; Habberfield, T. Paced Respiration as a Technique for the Modification of Autonomic Response to Stress. Psychophysiology 1976, 13, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.P.; Gerbarg, P.L.; Muench, F. Breathing Practices for Treatment of Psychiatric and Stress-Related Medical Conditions. Psychiatr. Clin. N. Am. 2013, 36, 121–140. [Google Scholar] [CrossRef]
- Brown, R.P.; Gerbarg, P.L. Yoga Breathing, Meditation, and Longevity. Ann. N. Y. Acad. Sci. USA 2009, 1172, 54–62. [Google Scholar] [CrossRef]
- Brown, R.P.; Gerbarg, P.L. Sudarshan Kriya Yogic Breathing in the Treatment of Stress, Anxiety, and Depression: Part I—Neurophysiologic Model. J. Altern. Complement. Med. 2005, 11, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Jerath, R.; Barnes, V.A.; Crawford, M.W. Mind-body response and neurophysiological changes during stress and meditation: Central role of homeostasis. J. Biol. Regul. Homeost. Agents 2014, 28, 545–554. [Google Scholar]
- Harinath, K.; Malhotra, A.S.; Pal, K.; Prasad, R.; Kumar, R.; Kain, T.C.; Rai, L.; Sawhney, R.C. Effects of Hatha Yoga and Omkar Meditation on Cardiorespiratory Performance, Psychologic Profile, and Melatonin Secretion. J. Altern. Complement. Med. 2004, 10, 261–268. [Google Scholar] [CrossRef]
- Ban, Y.; Karasawa, H.; Fukui, R.; Warisawa, S. Relaxushion: Controlling the Rhythm of Breathing for Relaxation by Overwriting Somatic Sensation. In Proceedings of the SIGGRAPH Asia 2018 Emerging Technologies, Tokyo, Japan, 4–7 December 2018; ACM: Tokyo, Japan, 2018; pp. 1–2. [Google Scholar]
- Fonkoue, I.T.; Marvar, P.J.; Norrholm, S.D.; Kankam, M.L.; Li, Y.; DaCosta, D.; Rothbaum, B.O.; Park, J. Acute effects of device-guided slow breathing on sympathetic nerve activity and baroreflex sensitivity in posttraumatic stress disorder. Am. J. Physiol.-Heart Circ. Physiol. 2018, 315, H141–H149. [Google Scholar] [CrossRef] [PubMed]
- Cherniack, N.S.; Chonan, T.; Altose, M.D. Respiratory Sensations and the Voluntary Control of Breathing. In Respiratory Psychophysiology; Wenner-Gren Center International Symposium Series; von Euler, C., Katz-Salamon, M., Eds.; Palgrave: London, UK, 1988. [Google Scholar] [CrossRef]
- Masaoka, Y.; Homma, I. Anxiety and respiratory patterns: Their relationship during mental stress and physical load. Int. J. Psychophysiol. 1997, 27, 153–159. [Google Scholar] [CrossRef]
- Croft, R.J.; Gonsalvez, C.J.; Gander, J.; Lechem, L.; Barry, R.J. Differential relations between heart rate and skin conductance, and public speaking anxiety. J. Behav. Ther. Exp. Psychiatry 2004, 35, 259–271. [Google Scholar] [CrossRef]
- Mundy-Castle, A.C.; McKiever, B.L. The psychophysiological significance of the galvanic skin response. J. Exp. Psychol. 1953, 46, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.T.; Berntson, G.G.; Poehlmann, K.M.; Ito, T.A.; Cacioppo, J.T. The psycho-physiology of emotion. In Handbook of Emotions; Lewis, M., Haviland-Jones, J.M., Barrett, L.F., Eds.; The Guilford Press: New York, NY, USA, 2008; pp. 180–195. [Google Scholar]
- Stern, R.M.; Ray, W.J.; Quigley, K.S. Psychophysiological Recording; Oxford University Press: New York, NY, USA, 2001; ISBN 978-0-19-511359-4. [Google Scholar]
- Caruelle, D.; Gustafsson, A.; Shams, P.; Lervik-Olsen, L. The use of electrodermal activity (EDA) measurement to understand consumer emotions—A literature review and a call for action. J. Bus. Res. 2019, 104, 146–160. [Google Scholar] [CrossRef]
- Winkielman, P.; Berridge, K.C. Unconscious Emotion. Curr. Dir. Psychol. Sci. 2004, 13, 120–123. [Google Scholar] [CrossRef]
- Bradley, M.M.; Lang, P.J. Measuring emotion: The self-assessment manikin and the semantic differential. J. Behav. Ther. Exp. Psychiatry 1994, 25, 49–59. [Google Scholar] [CrossRef]
- Lang, P.J. Studies of motivation and attention. Am. Psychol. 1995, 50, 372. [Google Scholar] [CrossRef]
- Westermann, R.; Spies, K.; Stahl, G.; Hesse, F.W. Relative Effectiveness and Validity of Mood Induction Procedures: A Meta-Analysis. Eur. J. Soc. Psychol. 1996, 26, 557–580. [Google Scholar] [CrossRef]
- Gross, J.J.; Levenson, R.W. Emotion elicitation using films. Cogn. Emot. 1995, 9, 87–108. [Google Scholar] [CrossRef]
- So, S.; Jain, D.; Kanayama, N. Piezoelectric Sensor-Based Continuous Monitoring of Respiratory Rate During Sleep. J. Med Biol. Eng. 2021, 41, 241–250. [Google Scholar] [CrossRef]
- Lewis, M.; Haviland-Jones, J.M.; Barrett, L.F. (Eds.) Handbook of Emotions, 3rd ed.; Guilford Press: New York, NY, USA, 2008; ISBN 978-1-59385-650-2. [Google Scholar]
- Homma, I.; Masaoka, Y. Breathing rhythms and emotions. Exp. Physiol. 2008, 93, 1011–1021. [Google Scholar] [CrossRef]
- Jerath, R.; Crawford, M.W.; Barnes, V.A.; Harden, K. Self-Regulation of Breathing as a Primary Treatment for Anxiety. Appl. Psychophysiol. Biofeedback 2015, 40, 107–115. [Google Scholar] [CrossRef]
- Noble, D.J.; Goolsby, W.N.; Garraway, S.M.; Martin, K.K.; Hochman, S. Slow Breathing Can Be Operantly Conditioned in the Rat and May Reduce Sensitivity to Experimental Stressors. Front. Physiol. 2017, 8, 854. [Google Scholar] [CrossRef]
- Boray, P.F.; Gifford, R.; Rosenblood, L. Effects of warm white, cool white and full-spectrum fluorescent lighting on simple cognitive performance, mood and ratings of others. J. Environ. Psychol. 1989, 9, 297–307. [Google Scholar] [CrossRef]
- Cheng, P.; Mugge, R.; de Bont, C. “Smart Home System is Like a Mother”: The Potential and Risks of Using Product Metaphors to Influence Consumers’ Comprehension of Really New Products. Int. J. Des. 2019, 13, 1–19. [Google Scholar]
- Critchley, H.D. Review: Electrodermal Responses: What Happens in the Brain. J. Neurosci. 2002, 8, 132–142. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, X.; Xie, D. Effects of mental tasks on the cardiorespiratory synchronization. Respir. Physiol. Neurobiol. 2010, 170, 91–95. [Google Scholar] [CrossRef]
- Jerath, R.; Harden, K.; Crawford, M.; Barnes, V.A.; Jensen, M. Role of cardiorespiratory synchronization and sleep physiology: Effects on membrane potential in the restorative functions of sleep. Sleep Med. 2014, 15, 279–288. [Google Scholar] [CrossRef]
- Bahirat, P.; Sun, Q.; Knijnenburg, B.P. Scenario Context v/s Framing and Defaults in Managing Privacy in Household IoT. In Proceedings of the 23rd International Conference on Intelligent User Interfaces Companion, Tokyo Japan, 7–11 March 2018; ACM: Tokyo, Japan, 2018; pp. 1–2. [Google Scholar]
| Colour Temperature | Breathing Group | No-Breathing Group |
|---|---|---|
| Cold light | 5 | 5 |
| Warm light | 5 | 5 |
| Breathing Condition | Light Condition | Statistics | EDA | Heart Rate | Pleasure | Arousal |
|---|---|---|---|---|---|---|
| Breathing group | Warm light | Mean | 2.73/0.45 | 1.28/1.21 | 4.60/5.20 | 6.20/4.40 |
| SD | 1.98/2.03 | 0.18/0.11 | 2.61/1.10 | 1.10/0.89 | ||
| Cold light | Mean | 1.91/1.22 | 1.22/1.19 | 4.00/5.80 | 5.80/2.80 | |
| SD | 2.63/1.49 | 0.21/0.14 | 1.00/2.17 | 1.64/1.10 | ||
| Control group | Warm light | Mean | 9.44/6.13 | 1.47/1.34 | 4.20/4.80 | 5.40/2.60 |
| SD | 5.63/4.95 | 0.11/0.08 | 1.79/0.45 | 1.67/0.89 | ||
| Cold light | Mean | 1.89/0.55 | 1.30/1.31 | 4.60/5.40 | 6.20/4.20 | |
| SD | 2.53/1.64 | 0.08/0.10 | 4.60/1.14 | 1.10/1.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Lu, J.; Xu, Z.; Wang, X. When Lights Can Breathe: Investigating the Influences of Breathing Lights on Users’ Emotion. Int. J. Environ. Res. Public Health 2022, 19, 13205. https://doi.org/10.3390/ijerph192013205
Wang J, Lu J, Xu Z, Wang X. When Lights Can Breathe: Investigating the Influences of Breathing Lights on Users’ Emotion. International Journal of Environmental Research and Public Health. 2022; 19(20):13205. https://doi.org/10.3390/ijerph192013205
Chicago/Turabian StyleWang, Junfeng, Jingjing Lu, Zhiyu Xu, and Xi Wang. 2022. "When Lights Can Breathe: Investigating the Influences of Breathing Lights on Users’ Emotion" International Journal of Environmental Research and Public Health 19, no. 20: 13205. https://doi.org/10.3390/ijerph192013205
APA StyleWang, J., Lu, J., Xu, Z., & Wang, X. (2022). When Lights Can Breathe: Investigating the Influences of Breathing Lights on Users’ Emotion. International Journal of Environmental Research and Public Health, 19(20), 13205. https://doi.org/10.3390/ijerph192013205





