Indirect Effects of Ebola Virus Disease Epidemics on Health Systems in the Democratic Republic of the Congo, Guinea, Sierra Leone and Liberia: A Scoping Review Supplemented with Expert Interviews
Abstract
1. Introduction
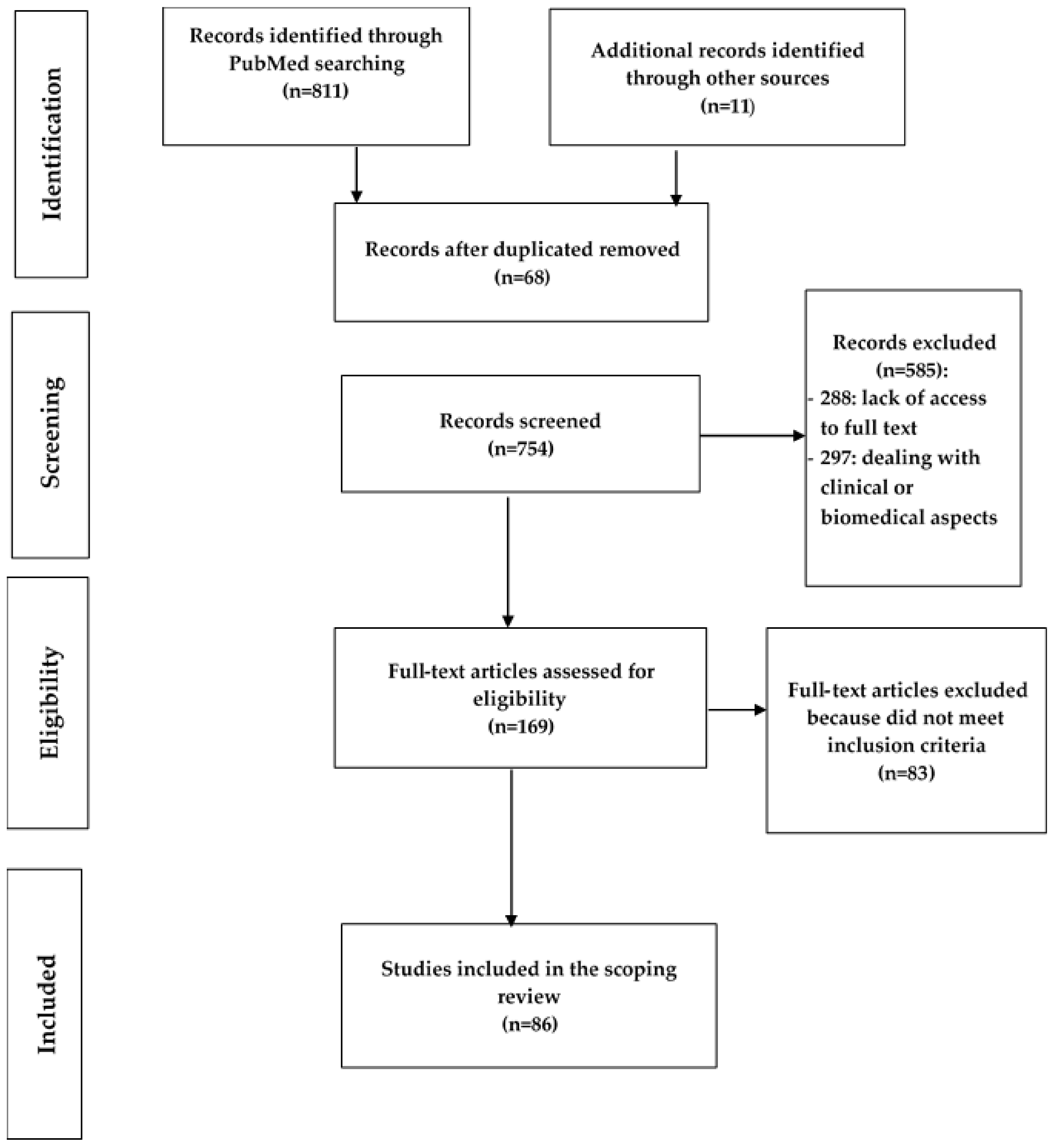
2. Materials and Methods
- Ebola virus disease
- Health service delivery in Africa
- Health workforce in Africa
- Health information systems in Africa
- Health care financing in Africa
- Essential medicines in Africa
- Leadership or governance in Africa
- [(1) and (2)] or [(1) and (3)] or [(1) and (4)] or [(1) and (5)] or [(1) and (6)] or [(1) and (7)]
3. Results
3.1. Delivery of (Essential) Health Services
3.2. Health Workers
3.3. Health Information System (HIS)
3.4. Financing
3.5. Essential Medicines, Medical Products and Equipment
3.6. Leadership and Governance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacob, S.T.; Crozier, I.; Fischer, W.A.; Hewlett, A.; Kraft, C.S.; Vega, M.A.D.L.; Soka, M.J.; Wahl, V.; Griffiths, A.; Bollinger, L.; et al. Ebola virus disease. Nat. Rev. Dis. Primers 2020, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Fontela, C.; McElroy, A.K. Ebola Virus Disease in Humans: Pathophysiology and Immunity. In Marburg-and Ebolaviruses; Springer: Cham, Switzerland, 2017; Volume 411, pp. 141–169. [Google Scholar] [CrossRef]
- Ki, M. What do we really fear? The epidemiological characteristics of Ebola and our preparedness. Epidemiol. Health 2014, 36, e2014014. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Malvy, D.; McElroy, A.K.; de Clerck, H.; Günther, S.; van Griensven, J. Ebola virus disease. Lancet 2019, 393, 936–948. [Google Scholar] [CrossRef]
- Beeching, N.J.; Fenech, M.; Houlihan, C.F. Ebola virus disease. BMJ 2014, 349, g7348. [Google Scholar] [CrossRef]
- Iversen, P.L.; Kane, C.D.; Zeng, X.; Panchal, R.G.; Warren, T.K.; Radoshitzky, S.R.; Kuhn, J.H.; Mudhasani, R.R.; Cooper, C.L.; Shurtleff, A.C.; et al. Recent successes in therapeutics for Ebola virus disease: No time for complacency. Lancet Infect. Dis. 2020, 20, e231–e237. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ebola Virus Disease. Available online: https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease (accessed on 28 December 2020).
- Chowell, G.; Tariq, A.; Kiskowski, M. Vaccination strategies to control Ebola epidemics in the context of variable household inaccessibility levels. PLOS Negl. Trop. Dis. 2019, 13, e0007814. [Google Scholar] [CrossRef]
- Shoman, H.; Karafillakis, E.; Rawaf, S. The link between the West African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: A systematic review. Glob. Health 2017, 13, 1–22. [Google Scholar] [CrossRef]
- Bolkan, H.A.; Bash-Taqi, D.A.; Samai, M.; Gerdin, M.; von Schreeb, J. Ebola and Indirect Effects on Health Service Function in Sierra Leone. PLoS Curr. 2014, 6. [Google Scholar] [CrossRef]
- Genevie, F. Repenser les Systèmes de Santé; Finances et Développement: Edinburgh, UK, 2020. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- WHO. Managing Epidemics. 2021. Available online: https://www.who.int/emergencies/diseases/managing-epidemics/en/ (accessed on 9 August 2021).
- WHO. Everybody’s Business—Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Sakyi, K.S.; Saalim, K.; Morrison, E.; Zohra, F.T.; Owusu, P.G.; Zora, J.; Thieda, P.; Dalglish, S.; Kanyangarara, M. Reported health system solutions implemented to contain COVID-19 in six West African countries: A media content analysis. J. Glob. Health Rep. 2022, 6, e2022008. [Google Scholar] [CrossRef]
- Mikkelsen-Lopez, I.; Wyss, K.; de Savigny, D. An approach to addressing governance from a health system framework perspective. BMC Int. Health Hum. Rights 2011, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Smith, V.; DeVane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res. Methodol. 2011, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Ansumana, R.; Keitell, S.; Roberts, G.M.; Ntoumi, F.; Petersen, E.; Ippolito, G.; Zumla, A. Impact of infectious disease epidemics on tuberculosis diagnostic, management, and prevention services: Experiences and lessons from the 2014–2015 Ebola virus disease outbreak in West Africa. Int. J. Infect. Dis. 2017, 56, 101–104. [Google Scholar] [CrossRef]
- Bolkan, H.A.; van Duinen, A.; Samai, M.; Bash-Taqi, D.A.; Gassama, I.; Waalewijn, B.; Wibe, A.; Von Schreeb, J. Admissions and surgery as indicators of hospital functions in Sierra Leone during the west-African Ebola outbreak. BMC Health Serv. Res. 2018, 18, 846. [Google Scholar] [CrossRef]
- Ribacke, K.J.B.; Saulnier, D.; Eriksson, A.; Von Schreeb, J. Effects of the West Africa Ebola Virus Disease on Health-Care Utilization—A Systematic Review. Front. Public Health 2016, 4, 222. [Google Scholar] [CrossRef]
- Kolie, D.; Camara, B.S.; Delamou, A.; Béavogui, A.H.; Hermans, V.; Edwards, J.K.; Benedetti, G.; Muller, C.P.; van Griensven, J.; Zachariah, R. The Ebola-effect in Guinea 2014-15: Tangled trends of malaria care in children under-five. PLoS ONE 2018, 13, e0192798. [Google Scholar] [CrossRef]
- Lapão, L.V.; Silva, A.; Pereira, N.; Vasconcelos, P.; Conceição, C. Ebola impact on African health systems entails a quest for more international and local resilience: The case of African Portuguese speaking countries. Pan. Afr. Med. J. 2015, 22 (Suppl. 1), 15. [Google Scholar] [CrossRef]
- Ly, J.; Sathananthan, V.; Griffiths, T.; Kanjee, Z.; Kenny, A.; Gordon, N.; Basu, G.; Battistoli, D.; Dorr, L.; Lorenzen, B.; et al. Facility-Based Delivery during the Ebola Virus Disease Epidemic in Rural Liberia: Analysis from a Cross-Sectional, Population-Based Household Survey. PLOS Med. 2016, 13, e1002096. [Google Scholar] [CrossRef]
- Magassouba, A.S.; Diallo, B.D.; Camara, L.M.; Sow, K.; Camara, S.; Bah, B.; Barry, A.O.; Diallo, T.H.; Camara, A.; Bangoura, A.M.; et al. Impact of the Ebola virus disease outbreak (2014–2016) on tuberculosis surveillance activities by Guinea’s National Tuberculosis Control Program: A time series analysis. BMC Public Health 2020, 20, 1200. [Google Scholar] [CrossRef] [PubMed]
- Masresha, B.G.; Luce, R.; Weldegebriel, G.; Katsande, R.; Gasasira, A.; Mihigo, R. The impact of a prolonged ebola outbreak on measles elimination activities in Guinea, Liberia and Sierra Leone, 2014–2015. Pan Afr. Med. J. 2020, 35, 8. [Google Scholar] [CrossRef] [PubMed]
- McQuilkin, P.A.; Udhayashankar, K.; Niescierenko, M.; Maranda, L. Health-Care Access during the Ebola Virus Epidemic in Liberia. Am. J. Trop. Med. Hyg. 2017, 97, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Plucinski, M.M.; Guilavogui, T.; Sidikiba, S.; Diakité, N.; Diakité, S.; Dioubaté, M.; Bah, I.; Hennessee, I.; Butts, J.K.; Halsey, E.S.; et al. Effect of the Ebola-virus-disease epidemic on malaria case management in Guinea, 2014: A cross-sectional survey of health facilities. Lancet Infect. Dis. 2015, 15, 1017–1023. [Google Scholar] [CrossRef][Green Version]
- Quaglio, G.; Tognon, F.; Finos, L.; Bome, D.; Sesay, S.; Kebbie, A.; Di Gennaro, F.; Camara, B.S.; Marotta, C.; Pisani, V.; et al. Impact of Ebola outbreak on reproductive health services in a rural district of Sierra Leone: A prospective observational study. BMJ Open 2019, 9, e029093. [Google Scholar] [CrossRef] [PubMed]
- Ribacke, K.J.B.; van Duinen, A.; Nordenstedt, H.; Höijer, J.; Molnes, R.; Froseth, T.W.; Koroma, A.P.; Darj, E.; Bolkan, H.A.; Ekström, A. The Impact of the West Africa Ebola Outbreak on Obstetric Health Care in Sierra Leone. PLoS ONE 2016, 11, e0150080. [Google Scholar] [CrossRef]
- Siekmans, K.; Sohani, S.; Boima, T.; Koffa, F.; Basil, L.; Laaziz, S. Community-based health care is an essential component of a resilient health system: Evidence from Ebola outbreak in Liberia. BMC Public Health 2017, 17, 84. [Google Scholar] [CrossRef] [PubMed]
- Theuring, S.; Koroma, A.P.; Harms, G. In the hospital, there will be nobody to pamper me: A qualitative assessment on barriers to facility-based delivery in post-Ebola Sierra Leone. Reprod. Health 2018, 15, 155. [Google Scholar] [CrossRef]
- Wilhelm, J.A.; Helleringer, S. Utilization of non-Ebola health care services during Ebola outbreaks: A systematic review and meta-analysis. J. Glob. Health 2019, 9, 010406. [Google Scholar] [CrossRef]
- Yerger, P.; Jalloh, M.; Coltart, C.E.M.; King, C. Barriers to maternal health services during the Ebola outbreak in three West African countries: A literature review. BMJ Glob. Health 2020, 5, e002974. [Google Scholar] [CrossRef]
- Camara, B.S.; Delamou, A.; Diro, E.; Béavogui, A.H.; El Ayadi, A.M.; Sidibé, S.; Grovogui, F.M.; Takarinda, K.C.; Bouedouno, P.; Sandouno, S.D.; et al. Effect of the 2014/2015 Ebola outbreak on reproductive health services in a rural district of Guinea: An ecological study. Trans. R. Soc. Trop. Med. Hyg. 2017, 111, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Lori, J.R.; Rominski, S.D.; Perosky, J.E.; Munro, M.L.; Williams, G.; Bell, S.A.; Nyanplu, A.B.; Amarah, P.N.; Boyd, C.J. A case series study on the effect of Ebola on facility-based deliveries in rural Liberia. BMC Pregnancy Childbirth 2015, 15, 254. [Google Scholar] [CrossRef] [PubMed]
- Wagenaar, B.H.; Augusto, O.; Beste, J.; Toomay, S.J.; Wickett, E.; Dunbar, N.; Bawo, L.; Wesseh, C.S. The 2014–2015 Ebola Virus Disease Outbreak and Primary Healthcare Delivery in Liberia: Time-Series Analyses for 2010–2016. PLoS Med. 2018, 15, e1002508. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; White, S.; Ormrod, J.; Sam, B.; Bull, F.; Pieh, S.; Gopalakrishnan, S.; Broek, N.V.D. Work-based risk factors and quality of life in health care workers providing maternal and newborn care during the Sierra Leone Ebola epidemic: Findings using the WHOQOL-BREF and HSE Management Standards Tool. BMJ Open 2020, 10, e032929. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.; Blidi, N.; Yokie, J.; Momolu, M.; Agbo, C.; Tuopileyi, R.; Rude, J.M.; Seid, M.; Dereje, Y.; Wambai, Z.; et al. Strengthening immunization service delivery post Ebola virus disease (EVD) outbreak in Liberia 2015–2017. Pan Afr. Med. J. 2019, 33, 5. [Google Scholar] [CrossRef] [PubMed]
- Cancedda, C.; Davis, S.; Dierberg, K.; Lascher, J.; Kelly, D.; Bailor Barrie, M.; Koroma, A.; George, P.; Kamara, A.A.; Marsh, R. Strengthening Health Systems While Responding to a Health Crisis: Lessons Learned by a Nongovern-mental Organization During the Ebola Virus Disease Epidemic in Sierra Leone. J. Infect. Dis. 2016, 214 (Suppl. 3), S153–S163. [Google Scholar] [CrossRef]
- Decroo, T.; Delamou, A.; Reeder, J.C. Operational research: Did health systems in Sierra Leone recover after the 2014–2015 Ebola outbreak? F1000Res 2019, 8, 792. [Google Scholar] [CrossRef]
- Li, W.; Jalloh, M.F.; Bunnell, R.; Aki-Sawyerr, Y.; Conteh, L.; Sengeh, P.; Redd, J.T.; Hersey, S.; Morgan, O.; Jalloh, M.B.; et al. Public Confidence in the Health Care System 1 Year After the Start of the Ebola Virus Disease Outbreak—Sierra Leone, July 2015. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 538–542. [Google Scholar] [CrossRef]
- Sochas, L.; Channon, A.; Nam, S. Counting indirect crisis-related deaths in the context of a low-resilience health system: The case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017, 32, iii32–iii39. [Google Scholar] [CrossRef]
- Kodish, S.R.; Simen-Kapeu, A.; Beauliere, J.-M.; Ngnie-Teta, I.; Jalloh, M.B.; Pyne-Bailey, S.; Schwartz, H.; Wirth, J.P. Consensus building around nutrition lessons from the 2014–16 Ebola virus disease outbreak in Guinea and Sierra Leone. Health Policy Plan. 2019, 34, 83–91. [Google Scholar] [CrossRef]
- Bemah, P.; Baller, A.; Cooper, C.; Massaquoi, M.; Skrip, L.; Rude, J.M.; Twyman, A.; Moses, P.; Seifeldin, R.; Udhayashankar, K.; et al. Strengthening healthcare workforce capacity during and post Ebola outbreaks in Liberia: An innovative and effective approach to epidemic preparedness and response. Pan. Afr. Med. J. 2019, 33, 9. [Google Scholar] [CrossRef] [PubMed]
- Elston, J.W.T.; Danis, K.; Gray, N.; West, K.; Lokuge, K.; Black, B.; Stringer, B.; Jimmisa, A.S.; Biankoe, A.; O Sanko, M.; et al. Maternal health after Ebola: Unmet needs and barriers to healthcare in rural Sierra Leone. Health Policy Plan. 2019, 35, 78–90. [Google Scholar] [CrossRef] [PubMed]
- Forrester, J.D.; Pillai, S.K.; Beer, K.D.; Bjork, A.; Neatherlin, J.; Massaquoi, M.; Nyenswah, T.G.; Montgomery, J.M.; De Cock, K. Assessment of Ebola Virus Disease, Health Care Infrastructure, and Preparedness—Four Counties, Southeastern Liberia, August 2014. MMWR. Morb. Mortal. Wkly. Rep. 2014, 63, 891–893. [Google Scholar] [PubMed]
- Raven, J.; Wurie, H.; Witter, S. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: A qualitative study. BMC Health Serv. Res. 2018, 18, 251. [Google Scholar] [CrossRef] [PubMed]
- Tiffany, A.; Haile, M.; Grais, R.F.; Serafini, M.; Traoré, A.; Genton, B.; Guilavogui, T.; Sterk, E.; Moundekeno, F.P. Community-Based Surveillance to Monitor Mortality in a Malaria-Endemic and Ebola-Epidemic Setting in Rural Guinea. Am. J. Trop. Med. Hyg. 2016, 95, 1389–1397. [Google Scholar] [CrossRef]
- Shumbullo, E. Ebola outbreak 2014–2016: Effects on other health services. In CMI BRIEF; Chr. Michelsen Institute: Bergen, Norway, 2020. [Google Scholar]
- Barry, A.; O’Fallon, J.B.; Hazerjian, J.; Brodish, P. Une Évaluation Rapide des Effets de la Flambée d’Ebola. Measure Evaluation. 2015. Available online: https://www.measureevaluation.org/resources/publications/sr-15-121-fr.html (accessed on 30 August 2022).
- ACAPS. Impact de la Maladie à Virus Ebola Sur Les Systèmes de Santé. ACAPS. 2015. Available online: https://reliefweb.int/report/guinea/document-dinformation-acaps-la-maladie-virus-ebola-en-afrique-de-louest-impact-sur-les (accessed on 30 August 2022).
- Elston, J.; Moosa, A.; Moses, F.; Walker, G.; Dotta, N.; Waldman, R.; Wright, J. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J. Public Health 2015, 38, 673–678. [Google Scholar] [CrossRef]
- Elston, J.; Cartwright, C.; Ndumbi, P.; Wright, J. The health impact of the 2014–15 Ebola outbreak. Public Health 2016, 143, 60–70. [Google Scholar] [CrossRef]
- Reardon, S. Ebola’s mental-health wounds linger in Africa. Nature 2015, 519, 13–15. [Google Scholar] [CrossRef]
- Bebell, L.M.; Oduyebo, T.; Riley, L.E. Ebola virus disease and pregnancy: A review of the current knowledge of Ebola virus path-ogenesis, maternal, and neonatal outcomes. Birth Defects Res. 2017, 109, 353–362. [Google Scholar] [CrossRef]
- Bitanihirwe, B.K.Y. Monitoring and managing mental health in the wake of Ebola. Commentary. Comment. Ann. Ist. Super Sanita 2016, 52, 320–322. [Google Scholar] [CrossRef]
- Logan, G.; Vora, N.M.; Nyensuah, T.G.; Gasasira, A.; Mott, J.; Walke, H.; Mahoney, F.; Luce, R.; Flannery, B. Establishment of a community care center for isolation and management of Ebola patients—Bomi County, Liberia, October 2014. Morb. Mortal. Wkly. Rep. 2014, 63, 1010–1012. [Google Scholar]
- Walker, P.G.T.; White, M.T.; Griffin, J.T.; Reynolds, A.; Ferguson, N.M.; Ghani, A.C. Malaria morbidity and mortality in Ebola-affected countries caused by decreased health-care capacity, and the potential effect of mitigation strategies: A modelling analysis. Lancet Infect. Dis. 2015, 15, 825–832. [Google Scholar] [CrossRef]
- Hanefeld, J.; Mayhew, S.; Legido-Quigley, H.; Martineau, F.; Karanikolos, M.; Blanchet, K.; Liverani, M.; Yei Mokuwa, E.; McKay, G.; Balabanova, D. Towards an understanding of resilience: Responding to health systems shocks. Health Policy Plan. 2018, 33, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Njuguna, C.; Jambai, A.; Chimbaru, A.; Nordstrom, A.; Conteh, R.; Latt, A.; O-Tipo, S.; Musoke, R.; Githuku, J.; Yoti, Z.; et al. Revitalization of integrated disease surveillance and response in Sierra Leone post Ebola virus disease outbreak. BMC Public Health 2019, 19, 364. [Google Scholar] [CrossRef] [PubMed]
- Thiam, S.; Delamou, A.; Camara, S.; Carter, J.; Lama, E.K.; Ndiaye, B.; Nyagero, J.; Nduba, J.; Ngom, M. Challenges in controlling the Ebola outbreak in two prefectures in Guinea: Why did communities continue to resist? Pan. Afr. Med. J. 2015, 22 (Suppl. 1), 22. [Google Scholar] [CrossRef] [PubMed]
- Delamou, A.; El Ayadi, A.M.; Sidibe, S.; Delvaux, T.; Camara, B.S.; Sandouno, S.D.; Beavogui, A.H.; Rutherford, G.W.; Okumura, J.; Zhang, W.-H.; et al. Effect of Ebola virus disease on maternal and child health services in Guinea: A retrospective observational cohort study. Lancet Glob. Health 2017, 5, e448–e457. [Google Scholar] [CrossRef]
- Perosky, J.E.; McLean, K.Z.; Kofa, A.; Nyanplu, A.; Munro-Kramer, M.; Lori, J.R. Utilization of maternity waiting homes: Before, during, and after the Ebola virus disease outbreak in Bong County, Liberia. Int. Health 2019, 12, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Sam, B.; Bull, F.; Pieh, S.B.; Lambert, J.; Mgawadere, F.; Gopalakrishnan, S.; Ameh, C.A.; FWACS; FRCOG; et al. ‘Even when you are afraid, you stay’: Provision of maternity care during the Ebola virus epidemic: A qualitative study. Midwifery 2017, 52, 19–26. [Google Scholar] [CrossRef] [PubMed]
- OXFAM. Plus Jamais Ça! Mettre en Place des Systèmes de Santé Résilients et Tirer les Enseignements de la Crise Liée à Ebola. OXFAM. 2015. Available online: https://reliefweb.int/report/world/plus-jamais-mettre-en-place-des-syst-mes-de-sant-r-silients-et-tirer-les-enseignements (accessed on 30 August 2022).
- Paquet, C.; Vergne, C. Repenser l’aide au Développement Pour Faire Face Aux Conséquences d’Ebola; Le Média du Développement Durable: Paris, France, 2014. [Google Scholar]
- Tambo, E.; Yah, C.S.; E Ugwu, C.; A Olalubi, O.; Wurie, I.; Jonhson, J.K.; Ngogang, J.Y. Fostering prevention and care delivery services capability on HIV pandemic and Ebola outbreak symbiosis in Africa. J. Infect. Dev. Ctries. 2016, 10, 1–12. [Google Scholar] [CrossRef][Green Version]
- Salim, L. Quels Sont les Effets de la Maladie à Virus Ebola sur le Système de Santé Ainsi qu’en Matière de Coopération dans le Secteur en République de Guinée? Master’s Thesis, Faculté des Sciences Sociales, Ulg, Belgium, 2017. Available online: https://matheo.uliege.be/bitstream/2268.2/3631/4/Ly%20m%C3%A9moire.pdf (accessed on 30 August 2022).
- GEC. Ebola en RDC: Système de Santé Parallèle, Effet Pervers de la Réponse, in Groupe d’études sur le Congo. Report, Université de New York. 2020. Available online: https://lesjours.fr/ressources/document/rapport-ebola/rapport-ebola-rdc-systeme-sante-parallele-effet-pervers-reponse.pdf (accessed on 30 August 2022).
- Oleribe, O.O.; Crossey, M.M.; Taylor-Robinson, S.D. Nigerian response to the 2014 Ebola viral disease outbreak: Lessons and cautions. Pan. Afr. Med. J. 2015, 22 (Suppl. 1), 13. [Google Scholar] [CrossRef]
- Ngatu, N.R.; Kayembe, N.J.-M.; Phillips, E.K.; Okech-Ojony, J.; Patou-Musumari, M.; Gaspard-Kibukusa, M.; Madone-Mandina, N.; Godefroid-Mayala, M.; Mutaawe, L.; Manzengo, C.; et al. Epidemiology of ebolavirus disease (EVD) and occupational EVD in health care workers in Sub-Saharan Africa: Need for strengthened public health preparedness. J. Epidemiol. 2017, 27, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Onyeonoro, U.U.; Ekpemiro, U.C.; Abali, C.; Nwokeukwu, H.I. Ebola epidemic—The Nigerian experience. Pan. Afr. Med. J. 2015, 22 (Suppl. 1), 17. [Google Scholar] [CrossRef] [PubMed]
- Moll, R.; Reece, S.; Cosford, P.; Kessel, A. The Ebola epidemic and public health response. Br. Med. Bull. 2016, 117, 15–23. [Google Scholar] [CrossRef][Green Version]
- Ministère de la Santé. Brève Situation de la Riposte à L’épidémie de la Maladie à Virus Ebola (MVE) dans la Province de l’Equateur, République Démocratique du Congo au 30e jour, Report. 2018. Available online: https://www.afro.who.int/publications/breve-situation-de-la-riposte-lepidemie-de-la-maladie-virus-ebola-mve-dans-la-province (accessed on 30 August 2022).
- Kamara, S.; Walder, A.; Duncan, J.; Kabbedijk, A.; Hughes, P.; Muana, A. Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bull. World Health Organ. 2017, 95, 842–847. [Google Scholar] [CrossRef] [PubMed]
- McPake, B.; Dayal, P.; Herbst, C.H. Never again? Challenges in transforming the health workforce landscape in post-Ebola West Africa. Hum. Resour. Health 2019, 17, 19. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Friedman, E.A. A retrospective and prospective analysis of the west African Ebola virus disease epidemic: Robust national health systems at the foundation and an empowered WHO at the apex. Lancet 2015, 385, 1902–1909. [Google Scholar] [CrossRef]
- Nyarko, Y.; Goldfrank, L.; Ogedegbe, G.; Soghoian, S.; Aikins, A.D.-G. Nyu-Ug-KBTH Ghana Ebola Working Group Preparing for Ebola Virus Disease in West African countries not yet affected: Perspectives from Ghanaian health professionals. Glob. Health 2015, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Okware, S.I.; Omaswa, F.; Talisuna, A.; Amandua, J.; Amone, J.; Onek, P.; Opio, A.; Wamala, J.; Lubwama, J.; Luswa, L.; et al. Managing Ebola from rural to urban slum settings: Experiences from Uganda. Afr. Health Sci. 2015, 15, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Ameme, D.K.; Nyarko, K.M.; Afari, E.A.; Antara, S.; Sackey, S.O.; Wurapa, F. Training Ghanaian frontline healthcare workers in public health surveillance and disease outbreak inves-tigation and response. Pan. Afr. Med. J. 2016, 25 (Suppl. 1), 2. [Google Scholar] [CrossRef]
- Marston, B.J.; Dokubo, E.K.; van Steelandt, A.; Martel, L.; Williams, D.; Hersey, S.; Jambai, A.; Keita, S.; Nyenswah, T.G.; Redd, J.T. Ebola Response Impact on Public Health Programs, West Africa, 2014–2017. Emerg. Infect. Dis. 2017, 23, S25–S32. [Google Scholar] [CrossRef]
- Barker, K.M.; Ling, E.J.; Fallah, M.; VandeBogert, B.; Kodl, Y.; Macauley, R.J.; Viswanath, K.; Kruk, E.M. Community engagement for health system resilience: Evidence from Liberia’s Ebola epidemic. Health Policy Plan. 2020, 35, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Standley, C.J.; Muhayangabo, R.; Bah, M.S.; Barry, A.M.; Bile, E.; Fischer, J.E.; Heegaard, W.; Koivogui, L.; Lakiss, S.K.; Sorrell, E.M.; et al. Creating a National Specimen Referral System in Guinea: Lessons from Initial Development and Imple-mentation. Front. Public Health 2019, 16, 83. [Google Scholar] [CrossRef]
- Kanu, H.; Wilson, K.; Sesay-Kamara, N.; Bennett, S.; Mehtar, S.; Storr, J.; Allegranzi, B.; Benya, H.; Park, B.; Kolwaite, A. Creation of a national infection prevention and control programme in Sierra Leone, 2015. BMJ Glob. Health 2019, 4, e001504. [Google Scholar] [CrossRef] [PubMed]
- Van de Pas, R.; Kolie, D.; Delamou, A.; van Damme, W. Health workforce development and retention in Guinea: A policy analysis post-Ebola. Hum. Resour. Health 2019, 17, 63. [Google Scholar] [CrossRef] [PubMed]
- Belfroid, E.; Mollers, M.; Smit, P.W.; Hulscher, M.; Koopmans, M.; Reusken, C.; Timen, A. Positive experiences of volunteers working in deployable laboratories in West Africa during the Ebola out-break. PLoS ONE 2018, 13, e0196320. [Google Scholar] [CrossRef]
- Standley, C.J.; MacDonald, P.D.M.; Attal-Juncqua, A.; Barry, A.M.; Bile, E.C.; Collins, D.L.; Corvil, S.; Ibrahima, D.B.; Hemingway-Foday, J.J.; Katz, R.; et al. Leveraging Partnerships to Maximize Global Health Security Improvements in Guinea, 2015–2019. Health Secur. 2020, 18, S34. [Google Scholar] [CrossRef] [PubMed]
- Médecins Sans Frontières. Poussés au-delà de nos Limites: Une Année de Lutte Contre la Plus Vaste Epidémie d’Ebola de l’Histoire. Médecins Sans Frontières, Report. 2015. Available online: https://www.msf.fr/sites/default/files/2018-03/msf_ebolareport_fr-def.pdf (accessed on 30 August 2022).
- Furuse, Y.; Fallah, M.; Oshitani, H.; Kituyi, L.; Mahmoud, N.; Musa, E.; Gasasira, A.; Nyenswah, T.; Dahn, B.; Bawo, L. Analysis of patient data from laboratories during the Ebola virus disease outbreak in Liberia, April 2014 to March 2015. PLOS Negl. Trop. Dis. 2017, 11, e0005804. [Google Scholar] [CrossRef]
- Joseph Wu, T.S.; Kagoli, M.; Kaasbøll, J.J.; Bjune, G.A. Integrated Disease Surveillance and Response (IDSR) in Malawi: Implementation gaps and challenges for timely alert. PLoS ONE 2018, 13, e0200858. [Google Scholar] [CrossRef] [PubMed]
- Oza, S.; Wing, K.; Sesay, A.A.; Boufkhed, S.; Houlihan, C.; Vandi, L.; Sebba, S.C.; McGowan, C.R.; Cummings, R.; Checchi, F. Improving health information systems during an emergency: Lessons and recommendations from an Ebola treatment centre in Sierra Leone. BMC Med. Inform. Decis. Mak. 2019, 19, 100. [Google Scholar] [CrossRef]
- Durski, K.N.; Singaravelu, S.; Naidoo, D.; Djingarey, M.H.; Fall, I.S.; Yahaya, A.A.; Aylward, B.; Osterholm, M.; Formenty, P. Design thinking during a health emergency: Building a national data collection and reporting system. BMC Public Health 2020, 20, 1896. [Google Scholar] [CrossRef]
- Fähnrich, C.; Denecke, K.; O Adeoye, O.; Benzler, J.; Claus, H.; Kirchner, G.; Mall, S.; Richter, R.; Schapranow, M.P.; Schwarz, N.; et al. Surveillance and Outbreak Response Management System (SORMAS) to support the control of the Ebola virus disease outbreak in West Africa. Eurosurveillance 2015, 20, 21071. [Google Scholar] [CrossRef] [PubMed]
- Oza, S.; Jazayeri, D.; Teich, J.M.; Ball, E.; Nankubuge, P.A.; Rwebembera, J.; Wing, K.; Sesay, A.A.; Kanter, A.S.; Ramos, G.D.; et al. Development and Deployment of the OpenMRS-Ebola Electronic Health Record System for an Ebola Treatment Center in Sierra Leone. J. Med. Internet Res. 2017, 19, e294. [Google Scholar] [CrossRef] [PubMed]
- Pore, M.; Sengeh, D.M.; Mugambi, P.; Purswani, N.V.; Sesay, T.; Arnold, A.L.; Tran, A.-M.; Myers, R. Design and evaluation of a web-based decision support tool for district-level disease surveillance in a low-resource setting. AMIA Annu. Symp. Proc. AMIA Symp. 2018, 2017, 1401–1410. [Google Scholar] [PubMed]
- Heymann, D.L.; Barakamfitiye, D.; Szczeniowski, M.; Muyembe-Tamfum, J.-J.; Bele, O.; Rodier, G. Ebola Hemorrhagic Fever: Lessons from Kikwit, Democratic Republic of the Congo. J. Infect. Dis. 1999, 179, S283–S286. [Google Scholar] [CrossRef]
- Naimoli, J.F.; Saxena, S.; E Hatt, L.; Yarrow, K.M.; White, T.M.; Ifafore-Calfee, T. Health system strengthening: Prospects and threats for its sustainability on the global health policy agenda. Health Policy Plan. 2017, 33, 85–98. [Google Scholar] [CrossRef]
- Dhillon, R.S.; Yates, R. Building back better: Priorities for Ebola-affected countries. Lancet Glob. Health 2015, 3, e435–e436. [Google Scholar] [CrossRef][Green Version]
- McMahon, S.A.; Ho, L.S.; Scott, K.; Brown, H.; Miller, L.; Ratnayake, R.; Ansumana, R. “We and the nurses are now working with one voice”: How community leaders and health committee members describe their role in Sierra Leone’s Ebola response. BMC Health Serv. Res. 2017, 17, 495. [Google Scholar] [CrossRef]
- Kirsch, T.D.; Moseson, H.; Massaquoi, M.; Nyenswah, T.G.; Goodermote, R.; Rodriguez-Barraquer, I.; Lessler, J.; Cumings, D.A.T.; Peters, D.H. Impact of interventions and the incidence of ebola virus disease in Liberia—Implications for future epidemics. Health Policy Plan. 2016, 32, 205–214. [Google Scholar] [CrossRef]
- Li, Z.-J.; Tu, W.-X.; Wang, X.-C.; Shi, G.-Q.; Yin, Z.-D.; Su, H.-J.; Shen, T.; Zhang, D.-P.; Li, J.-D.; Lv, S.; et al. A practical community-based response strategy to interrupt Ebola transmission in sierra Leone, 2014–2015. Infect. Dis. Poverty 2016, 5, 1–10. [Google Scholar] [CrossRef]
- Nsubuga, P.; Masiira, B.; Kihembo, C.; Byakika-Tusiime, J.; Ryan, C.; Nanyunja, M.; Kamadjeu, R.; Talisuna, A. Evaluation of the Ebola Virus Disease (EVD) preparedness and readiness program in Uganda: 2018 to 2019. Pan. Afr. Med. J. 2021, 38, 130. [Google Scholar] [CrossRef]
- Chang, H.-J.; Huang, N.; Lee, C.-H.; Hsu, Y.-J.; Hsieh, C.-J.; Chou, Y.-J. The Impact of the SARS Epidemic on the Utilization of Medical Services: SARS and the Fear of SARS. Am. J. Public Health 2004, 94, 562–564. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.; Moore, J.; Fraher, E.P.; Frogner, B.K.; Pittman, P.; Spetz, J. COVID-19 and the Health Workforce. Med Care Res. Rev. 2020, 78, 4S–6S. [Google Scholar] [CrossRef] [PubMed]
- Hategeka, C.; Carter, S.E.; Chenge, F.M.; Katanga, E.N.; Lurton, G.; Mayaka, S.M.N.; Mwamba, D.K.; van Kleef, E.; Vanlerberghe, V.; Grépin, K.A. Impact of the COVID-19 pandemic and response on the utilisation of health services during the first wave in Kinshasa, the Democratic Republic of the Congo. BMJ Glob. Health 2021, 6, e005955. [Google Scholar] [CrossRef] [PubMed]
- Hayden, E. Ebola Obstructs Malaria Control-Outbreak is Shutting Down Prevention and Treatment Programmes in West Africa. Nature 2014, 514, 15. [Google Scholar] [CrossRef]
- Nagesh, S.; Chakraborty, S. Saving the frontline health workforce amidst the COVID-19 crisis: Challenges and recom-mendations. J. Glob. Health 2020, 10, 010345. [Google Scholar] [CrossRef]
- Tambo, E.; Ugwu, E.C.; Ngogang, J.Y. Need of surveillance response systems to combat Ebola outbreaks and other emerging infectious diseases in African countries. Infect. Dis. Poverty 2014, 3, 29. [Google Scholar] [CrossRef]
- WHO. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and their Measurement Strategies; WHO Library: Geneva, Switzerland, 2010. [Google Scholar]
- Murewanhema, G.; Makurumidze, R. Essential health services delivery in Zimbabwe during the COVID-19 pandemic: Per-spectives and recommendations. Pan. Afr. Med. J. 2020, 35 (Suppl. 2), 143. [Google Scholar] [CrossRef]
| Expert Codes | Expert Affiliations | Expert Duty Country |
|---|---|---|
| INT 01 | MoH | RD. Congo |
| INT 02 | WHO/AFRO | RD. Congo and West Africa |
| INT 03 | MoH | RD. Congo |
| INT 04 | Africa CDC | RD. Congo and West Africa |
| INT 05 | MoH | RD. Congo |
| INT 06 | MoH | RD. Congo |
| INT 07 | CDC | RD. Congo |
| INT 08 | WHO/AFRO | RD. Congo and West Africa |
| INT 09 | University | RD. Congo |
| INT 10 | MSF | RD. Congo |
| INT 11 | WHO/AFRO | RD. Congo |
| Health System Building Blocks | N | % |
|---|---|---|
| Service Delivery | 59/86 | 68.6 |
| Workforce | 40/86 | 46.5 |
| Health Information System | 18/86 | 20.9 |
| Financing | 7/86 | 8.1 |
| Medicines | 9/86 | 10.4 |
| Leadership and Governance | 20/86 | 23.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mulenga-Cilundika, P.; Ekofo, J.; Kabanga, C.; Criel, B.; Van Damme, W.; Chenge, F. Indirect Effects of Ebola Virus Disease Epidemics on Health Systems in the Democratic Republic of the Congo, Guinea, Sierra Leone and Liberia: A Scoping Review Supplemented with Expert Interviews. Int. J. Environ. Res. Public Health 2022, 19, 13113. https://doi.org/10.3390/ijerph192013113
Mulenga-Cilundika P, Ekofo J, Kabanga C, Criel B, Van Damme W, Chenge F. Indirect Effects of Ebola Virus Disease Epidemics on Health Systems in the Democratic Republic of the Congo, Guinea, Sierra Leone and Liberia: A Scoping Review Supplemented with Expert Interviews. International Journal of Environmental Research and Public Health. 2022; 19(20):13113. https://doi.org/10.3390/ijerph192013113
Chicago/Turabian StyleMulenga-Cilundika, Philippe, Joel Ekofo, Chrispin Kabanga, Bart Criel, Wim Van Damme, and Faustin Chenge. 2022. "Indirect Effects of Ebola Virus Disease Epidemics on Health Systems in the Democratic Republic of the Congo, Guinea, Sierra Leone and Liberia: A Scoping Review Supplemented with Expert Interviews" International Journal of Environmental Research and Public Health 19, no. 20: 13113. https://doi.org/10.3390/ijerph192013113
APA StyleMulenga-Cilundika, P., Ekofo, J., Kabanga, C., Criel, B., Van Damme, W., & Chenge, F. (2022). Indirect Effects of Ebola Virus Disease Epidemics on Health Systems in the Democratic Republic of the Congo, Guinea, Sierra Leone and Liberia: A Scoping Review Supplemented with Expert Interviews. International Journal of Environmental Research and Public Health, 19(20), 13113. https://doi.org/10.3390/ijerph192013113






