Abstract
Introduction: Since the advent of 2019 novel coronavirus (COVID-19), the coexistence between social stigma and depression symptoms (depression hereafter) in COVID-19 patients has been mentioned, but the mechanisms involved remains unclear. This study aimed to explore how the stigma affects depression during the mid-pandemic period. Methods: A cross-sectional survey using non-probability sampling was conducted among asymptomatic COVID-19 carriers in Shanghai, China (April 2022). An online questionnaire was used to obtain information on demographic characteristics and psychological traits. Logistic regression and path analysis were performed to analyze the depression risk factors and examine the mediation model, respectively. Results: A total of 1283 participants (59.6% men) were involved in this study, in which 44.7% of carriers reported having depression. Univariate analyses found that education level (OR 0.575; 95% CI 0.448–0.737) and doses of vaccine (OR 1.693; 95% CI 1.042–2.750), were significantly associated with depression among asymptomatic carriers. The association between social stigma and depression was fully mediated by their feelings of entrapment and decadence (indirect effect = 0.204, p < 0.001; direct effect = −0.059, p = 0.058). The mediating role of entrapment between stigma and depression was moderated by age group (estimate = 0.116, p = 0.008). Conclusion: Mental health issues resulting from the COVID-19 pandemic are increasingly apparent in China and require urgent attention and responses. These findings provide new perspectives for the early prevention of depression in asymptomatic carriers.
1. Introduction
The pandemic of 2019 novel coronavirus (COVID-19) has become a major global public health challenge [1,2]. It is self-evident that it not only caused the burden of physical illness but has also triggered a wide range of declines in mental well-being [3,4]. A meta-analysis suggested that the global prevalence of major depressive disorder increased the most among a series of negative psychology issues with the emergence of COVID-19. The prevalence of depression increased by 27.6% (25.1% to 30.3%), with a loss of disability-adjusted life-years of 4.94 million (33.6 to 68.7) [5]. Global levels of depression in the general population, health care providers and patients during the COVID-19 pandemic went up to 24.0% (21.0–27.1%) [6]. A meta-analysis revealed that psychological problems in infected patients were prominent, with a prevalence of 45% depression [7].
Although risk factors for depression in vulnerable groups have been documented [8,9,10], current information regarding how the factors affect depression is lacking. Evidence suggested that COVID-19 survivors experienced higher stigma levels compared with healthy controls [11]. COVID-19-related stigma refers to a disagreeable or negative self-attitude that develops after infection or close contact with COVID-19 patients [12], including the negative deflection of social identity, with self-concept thus leading to a “spoiled identity” [12,13]. Additional evidence suggests a correlation between depression and social stigma. Liu et al. emphasized the importance of stigma in exacerbating the emotional impact of infected patients [9]. A prospective cohort study of COVID-19 survivors found that discrimination may partly account for the high incidence of depression after infection remission [14]. The identity-threat model of stigma raised by Brenda Major et al., which views stigma as a stressor, attempts to explain the effects of stigma on psychological well-being such as depression through coping strategies [15,16].
The economic consequences and psychosocial impacts of the COVID-19 pandemic are pervasive and profound [17,18,19]. Consequently, to avoid long-term mental health issues, there is an urgent need to clarify the mechanisms of the development of depression for COVID-19 patients [20,21]. The Social Rank Theory (SRT) proposes that depression evolves as a natural result of prolonged involuntary subordination [22]. Faced with an unfavorable situation (e.g., unachievable objectives, attempted change or challenge inhibited), individuals involuntarily yield adaptive responses through an automatic shutdown strategy [23]. If the situations persist and cannot be changed or escaped, the adaptive response will progressively change to maladjustment and eventually lead to depression [24,25]. Entrapment and decadence are precisely the key maladaptive defensive responses to this process. Entrapment is described as a common situation when there is a strong motivation to escape from an unsatisfying status, but that expectation cannot be met [22,26]. It could activate the Involuntary Defeat Strategy that, along with the feelings of decadence, forms a “depressogenic feedback loop” and ultimately contributes to the development of depression [27].
To our knowledge, little is known about the exact mechanisms on how stigma affects depression. Aiming to address this gap in understanding, we hypothesized and constructed a mediating model in which entrapment and decadence are mediators between social stigma and depression. The reasons are as follows: First, the identity-threat model of stigma posits that intrusive thinking and rumination about an event or issues occur when stigmatized individuals respond to stigma with involuntary engagement [15,28]. These two responses may have potential connection points with the assumed prerequisites of the SRT, that adverse situations are uncomfortable for individuals but cannot yet be accepted or escaped. That is, the identity-threat model of stigma implies that stigma affects entrapment and decadence. Second, entrapment and decadence are psychological signals prior to the onset of depression based on the SRT. Finally, a stigma-related stressor begins with external stimuli, while entrapment or decadence are inherently intrinsic psychological products, which satisfies the theoretical requirement of chronological order.
The primary objective of this study was to explore potential mediations between social stigma and depression via entrapment or decadence based on quantitative data from asymptomatic COVID-19 carriers in Shanghai, China. These findings may help us further understand the impact of the pandemic on COVID-19 patients’ mental health and inform subsequent intervention strategies and services for depression related to COVID-19.
2. Methods
2.1. Study Design and Participants
This is a cross-sectional study of asymptomatic COVID-19 carriers admitted to the Ruijin Jiahe Fangcang shelter hospital (Shanghai, China) in April 2022. Non-probability sampling was used to recruit participants for this study. Health care providers were responsible for advocacy and inviting asymptomatic patients, aiming to cover over 80% of patients admitted. According to previous studies, the expected prevalence of depression among COVID-19 carriers was 45% [7]. We used α of 0.05 and a permissible error of 0.03. Considering a non-response rate of 10%, the required sample size was 1209.
Inclusion criteria included: (1) older than 18 years. (2) A diagnosis of asymptomatic COVID-19 infection, which was judged by the threshold Cycle (Ct) value obtained from the real-time reverse transcriptase-polymerase chain reaction (RT-PCR) test. The test for SARS-CoV-2 RNA in the nasopharynx is considered positive at a CT value below 35. (3) Able to use WeChat to complete the questionnaire independently. (4) Capable of providing informed consent. The study was approved by the Ethics Committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (protocol code LL202070).
2.2. Data Collection
To comply with social distancing guidelines, an electronic questionnaire was selected for assessment in this study. Health care providers asked participants to answer questions based on their feelings and thoughts in the recent period when the diagnosis of COVID-19 was confirmed and presented QR codes of the questionnaire to the participants. Self-designed questionnaires were administered to collect information about demographic characteristics and psychological traits (social stigma, entrapment, decadence and depression). The information was gathered via the online survey platform “Questionnaire Star”. All survey respondents provided their informed written consent before the survey.
2.3. Measures
2.3.1. Background Characteristics
Information on background characteristics was collected, including age, sex, education level, marriage status, length of time from diagnosis, and doses of COVID-19 vaccines.
2.3.2. Social Stigma
Stigma from COVID-19 was measured via two subscales of the Social Impact Scale (SIS) [29], a generic stigma scale initially applied to patients with cancer or infectious diseases (e.g., human immunodeficiency virus, HIV) (Cronbach’s α = 0.85–0.90). Sixteen items assessed the social stigma related to COVID-19 at the mid-stage of the outbreak. (1) Social rejection measures stigma-related stressors, including traditional infectious disease’s role beliefs (perceiving others to treat them with less respect, no longer consider them competent or avoid them), and experiencing a major life event (being denied employment, education or being otherwise neglected) [16,29]. It gives the individual a sense of being discriminated against at work and in society [29]. (2) Social isolation signifies a sense of anomie in the traditional sociological sense, including feelings of loneliness, inequality with others and uselessness, accompanied by a devalued social identity [16,29]. Compared to HIV stigma, the stigmatization of COVID-19 has less of a moral link and perhaps less self-blame than HIV [30]. In addition, the trajectory of people diagnosed as positive needs to be disclosed in order to reduce public panic. We therefore believe that internalized shame from the SIS is not sufficiently consistent with the content of the social stigma of individuals at the early stage of diagnosis. Thus, only two subscales of the SIS were included. Sample items included “my employer/co-workers have discriminated against me because of my illness”, “some people act as though I am less competent than usual.” The options were rated from 1 (strongly disagree) to 4 (strongly agree). Higher total scores suggested higher levels of COVID-19-related stigma. A score lower than the 75th percentile—a score of 35—was defined as a low level. The Chinese version of the SIS has been found to have good psychological traits [31]. The SIS was applied to measure COVID-19-related stigma in Chinese COVID-19 survivors in 2020 [11]. The Cronbach’s α of the SIS in this study was 0.967, with factor loadings of 0.511–0.745. Psychometrics for the current study sample are enclosed in the Supplementary Materials.
2.3.3. Entrapment and Decadence
Feelings of entrapment was assessed by the Chinese version of Entrapment Scale (ES) [32] (Cronbach’s α = 0.96). The ES is a 16-item self-report scale used to identify the subjective experiences of entrapment [22]., e.g., “I am in a situation I feel trapped in”. Options for each item range from 0 (not at all), 1 (light), 2 (medium), 3 (heavy), and 4 (serious) [33]. The total possible score can be between 0 and 64. A level above the 75th percentile was defined as a high level of sense of entrapment.
Feelings of decadence were quantified with the Chinese version of the subscale of Defeat Scale (DS) (Cronbach’s α = 0.93), which is designed to assess personal perceptions of failed struggles and loss of rank within the last week [22]., e.g., “I feel defeated by life”. The response options are 0 (never), 1 (seldom), 2 (sometimes), 3 (often), and 4 (always). The overall scores for this 13-item scale range from 0 to 52. A total score over the 75th percentile was defined as a high level of decadence. Both scales have demonstrated validity and reliability among Chinese populations [32,34]. In the present study, the internal consistency coefficients of ES and DS were 0.973 and 0.904, respectively, and the factor loadings of each item in confirmatory factor analysis were roughly above 0.7. Details are presented in the Supplementary Materials.
2.3.4. Depression
The Zung Self-Rating Depression Scale (SDS), which consists of 20 self-report items, was used to assess participants’ depression based on their feelings [35]. The SDS scale includes physiological and psychological symptoms which have been identified in factor analysis studies of depression [35]. Ten items reflect the negative aspect., e.g., “I feel down-hearted and blue”. Ten items express positive aspects and are reverse scored., e.g., “morning is when I feel the best”. Each question has four response options, from 1 (none, or a little of the time) to 4 (most, or all of the time). The final raw score is the sum of the 20 items, ranging from 20 to 80. A higher score indicates a higher level of depressive severity. The total raw score ≥ 42 is taken as presenting with depression. Additionally, the cut-off value has also been adopted in other Chinese studies [36,37]. The Chinese version of the SDS has been shown to be a valid tool for screening depression (Cronbach’s α = 0.82) [36,38].
2.4. Statistical Analysis
The normally distributed variable (age) and skewedly distributed variables (stigma, entrapment, decadence, and depression) were described as the mean with standard deviation (SD) and median (interquartile range (IQR)), respectively. Categorical variables (e.g., sex and education level) were expressed as counts and percentages. The univariate logistic regression model was used to identify the characteristics associated with depression.
The Change-in-Estimate procedure was used for confounder identification and selection [39]. All socio-demographic variables and the target variable (stigma) were included in a multivariate logistic regression to build the initial full model. Covariates were selected by backward elimination. In this procedure, the covariate for which removal caused a change of less than 10% in the OR of stigma was removed [39]. The correlation coefficients between variables in final model were based on Spearman correlation analysis. We performed three hierarchical regression analyses to initially test the mediating effect. In step 1, the association of significant sociodemographic characteristics to depression was tested. The stigma factor was added in the step 2. Entrapment; decadence; and entrapment and decadence were added separately in step 3 to test for changes in the effect of stigma on depression.
After adjusting for covariates, path analysis was conducted to examine the relationships among stigma, entrapment, decadence, and depression. Four psychosocial variables are expressed as quantitative data in the mediation model. Two product-of-coefficients strategies (bias-corrected and percentile methods) were performed to examine the mediating role of entrapment and decadence in the association between stigma and depression [40]. In this process, 5000 bootstrap samples were used. The 95% confidence intervals (CI) that do not contain zero indicate the significance of the indirect effects [40,41]. Finally, a bias-corrected bootstrapping procedure based on 5000 resamples was employed to examine the significance of the age-moderated mediation effect. Using the mean value as the cut-off point, age was divided into high and low groups in the moderation analysis. The high age group mentioned in this study is only relative to the low group.
To enhance the credibility of our analysis, a temporal validation was conducted [42]. The data were randomized to the training group and validation group in a 3:1 ratio. Then, the bootstrapping method was used for temporal validation.
Descriptive analyses, logistic regression, correlation analysis and hierarchical regression were conducted using IBM SPSS Statistics 26.0 (IBM Corp., Armonk, NY, USA). Path analysis was conducted using R software (V. 4.2.1; http://www.Rproject.org; URL (accessed on 1 June 2022)). p values < 0.05 were considered as statistically significant.
3. Results
3.1. Participants
Of 1750 individuals referred to hospital, 1425 completed the questionnaire. The response rate was 81.4%. After excluding 142 participants who did not meet the inclusion criteria, a total of 1283 participants were included, as shown in Figure 1.
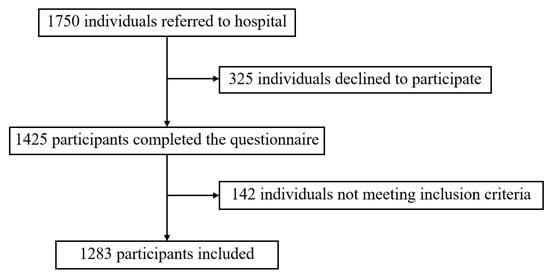
Figure 1.
Participants’ recruitment flow chart.
3.2. Sociodemographic Characteristics
Table 1 shows the demographic and psychosocial characteristics of 1283 asymptomatic COVID-19 carriers during the COVID-19 outbreak in Shanghai. The mean age of participants was 39.6 ± 11.1 years with a range from 18 to 71, and 765 (59.6%) were men. The majority of participants were married (948 (73.9%)) and graduated from senior secondary or below (906 [70.6%]). More than eighty percent of participants (1097) were diagnosed as asymptomatic carriers for greater than or equal to 8 days, among which, 646 (50.4%) tested positive for SARS-CoV-2 RNA within two weeks. Regarding COVID-19 vaccination, a large number of participants received the vaccine, of which, 808 (63.0%) received three doses, 355 (27.7%) received two doses, and less than ten percent of participants (9.4%) did not receive the vaccine or only received a single dose.

Table 1.
Characteristics of asymptomatic COVID-19 carriers and univariate logistic regression analysis of depression (n = 1283).
In the univariate analysis (Table 1), education level (OR 0.575; 95% CI 0.448–0.737) and doses of vaccine (OR 1.693; 95% CI 1.042–2.750) were significantly associated with depression among asymptomatic COVID-19 carriers. Higher educational attainment was a protective factor, whereas three doses of vaccine was a risk factor for depression.
3.3. Covariate Selection and Correlation Analysis
Considering the significant effect of education level and vaccination dose on depression in both univariate and multivariate logistic regressions, these two covariates were included in the subsequent analysis (Supplementary Materials Table S7). The Change-in-Estimate procedure showed that by sequentially removing the socio-demographic variables (the four remaining variables), none of the ORs of the stigma changed by more than 10%; thus, all met the criteria for exclusion (Supplementary Materials Table S8).
As shown in Table 2, the median perceived stigmatization score for all participants was 29.0 (IQR = 18.0), with 305 participants (23.8%) reaching a high level. Participants’ median entrapment and decadence scores were 1.0 (IQR = 10.0) and 2.0 (IQR = 12.0), among which, 318 (24.8%) and 304 (23.7%) reported high levels, respectively. With respect to depression, the median score of the SDS was 40.0 (IQR = 19.0), and nearly half of the participants (574 (44.7%)) reported having depression.

Table 2.
Psychological scores and relationship between variables in model.
Education level was significantly associated with all other variables. Doses of vaccine was significantly associated with stigma. Stigma was positively correlated with depression, entrapment and decadence. Depression was positively correlated with entrapment and decadence, and entrapment was positively correlated with decadence.
3.4. Hierarchical Regression Analysis
Our data met the assumption for mediation. Significant sociodemographic characteristics, including education level and doses of vaccine tested in step 1, explained 2.0% of the variance in depression. Stigma scores, added in step 2, had significant effects on depression (β = 0.148, t = 5.551, p < 0.001). However, the effect was no longer significant after the addition of entrapment and decadence in step 3 (p > 0.05) (Table 3).

Table 3.
Hierarchical regression analysis (n = 1283).
3.5. Path Analysis
Adjusted for covariates (i.e., education level, doses of vaccine), the results of the path analysis are detailed in Table 4. The indirect path from perceived stigma to depression through entrapment (p < 0.001) and decadence (p = 0.001) were significant, while the direct path between them was not significant (p = 0.058). In another word, entrapment and decadence completely mediated the relationship between stigma and depression (estimate = 0.204, Delta z = 10.912, p < 0.001).

Table 4.
Results of path analysis (n = 1283).
As shown in Figure 2, stigma among COVID-19 carriers was positively associated with their feelings of entrapment (estimate = 0.507, p < 0.001), which in turn was positively associated with their risk of depression (estimate = 0.247, p < 0.001). Similarly, the social stigmatization of participants was significantly linked to the sense of decadence (estimate = 0.461, p < 0.001), which in turn was positively related to depressive symptoms (estimate = 0.171, p < 0.001). When comparing indirect effects in the mediator models of entrapment and decadence, the differences were not significant (p = 0.254) (Table 3).
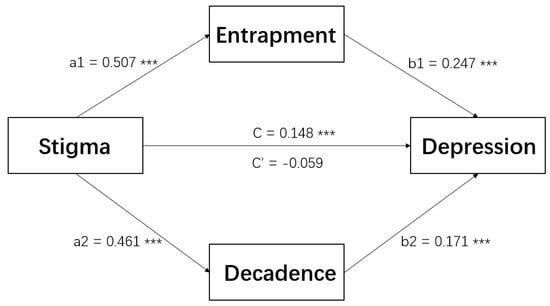
Figure 2.
The mediating role of entrapment and decadence in the relationship between stigma and depression (n = 1283). *** p < 0.001. Note: education level and doses of vaccine significantly associated with depression in logistic regression were controlled as covariates in the path analysis. C’: change in coefficient when mediating variables are incorporated.
The mediating role of entrapment between stigma and depression was moderated by age group (estimate = 0.116, p = 0.008). For participants aged 18–39 years, the indirect effect of entrapment was significant (estimate = 0.182, Delta z = 4.962, p < 0.001). For subjects aged 40–71 years, the mediating role of entrapment was still positively correlated with stigma and depression, but much weaker (estimate = 0.066, Delta z = 2.754, p = 0.006). However, the moderating role of age group in the decadence path was not significant (estimate = −0.114, p = 0.762) (Table 3).
3.6. Temporal Validation
We additionally considered the relationship between one variable and all other variables in the model in the training set; the path plot is shown in Supplementary Materials Figure S1. The results of the validation set showed that entrapment and decadence partially mediated the relationship between stigma and depression (Supplementary Materials Table S9).
4. Discussion
We conducted a quantitative study to explore the potential mechanism of how stigma affects the likelihood of depression in asymptomatic carriers during the mid-stage of the COVID-19 outbreak in Shanghai. In the current study, depression was reported by 44.7% of participants. A high education level was a protective factor for depression. This study characterized the psychological status of COVID-19 asymptomatic carriers, underscoring the importance of psychiatric screening and early interventions in this subgroup. Moreover, we found a mediating role of entrapment and decadence on the relationship between social stigma and depression, which offers a new way to mitigate the high prevalence of depression among asymptomatic carriers in China.
We found that the prevalence of depression reported by asymptomatic carriers was comparable to the rate in COVID-19 patients in previous studies [7,43]. Since physicians prioritize the physical illnesses of hospital patients, it is not surprising that the mental health issues of this subpopulation did not receive attention. Asymptomatic carriers account for a large proportion of COVID-19 patients in China, which highlights the importance of raising awareness of psychiatric screening in infected patients. In addition, the final model showed that a higher education level was a protective factor for depression. Inconsistent findings were reported for the association between education level and psychological symptoms [7,9]. One explanation for our finding is that better-educated individuals tend to acquire the correct information and awareness about COVID-19, therefore being more likely to avoid some adverse psychological health outcomes.
In line with our hypothesis, entrapment and decadence mediate the relationship between stigma and depression in asymptomatic carriers during the epidemic. People who suffered from stigma were more likely to feel trapped and decadent, which, in turn, was associated with an increase depressive symptoms. Two conceptual frameworks described at the beginning of the article guided this mediation assumption complementarily. Moreover, we found that the indirect relationship between stigma and depression through entrapment was moderated by age group. This further supports the finding that stigma can affect depression via entrapment.
Mediation analysis is essentially a correlation analysis [44]. Based on accumulated theory and research, we hypothesized that entrapment mediates the relationship between stigma and depression. However, the existence of a correlation between stigma and depression may also be the result of reverse causality or the presence of confounding factors. We found a significant difference in the correlation coefficients between stigma and depression in the two age groups, which at least suggests that the correlation is not exactly the result of the two possible causes mentioned above (reverse causality and confounding factors) [44,45]. Otherwise, their correlation would not differ. Thus, the mediation effect exists.
Our findings have three implications for the early detection of depression and effective mental health services for asymptomatic carriers. First and foremost, the timely assessment of stigmatizing stressors associated with COVID-19 must be carried out. Prior studies suggest that social stigma is not only a product of structural inequalities caused by bias and discrimination, but also the result of individual failures to cope adaptively with the stressors [15]. Ding K et al. also suggested that personal-level factors are more likely to be related to depression [46,47]. Therefore, the consideration of individuals’ stigmatizing stressors in early depression interventions is clearly warranted. This study focused on stigmatizing stressors related to job refusals and other overlooked situations. In future research, we believe there is a need to help infected individuals identify the well-defined type of stigma-related stress (e.g., being quarantined or treatment factors) they encounter to effectively help them cope with it successfully.
Second, response efforts to alleviate entrapment and decadence can be a crucial early intervention point for depression. Our main results shows that entrapment and decadence fully mediated the association between COVID-19-related stigma and depression. It appears that improving entrapment and decadence may effectively block the effects of stigma on depression. Specifically, an assessment of the psychological status of entrapment and decadence can be included in the early detection of depressive symptoms. Additionally, hospitals can implement remote mental health psychiatric counseling and screening programs through telemedicine or online mental health interventions [48,49]. Preventive strategies and early interventions are needed to adequately address early psychological abnormal states and avoid long-term mental health problems.
Third, this research provides a basis for implementing individualized mental health intervention strategies. Our findings revealed that the indirect link between stigmatization and depression via entrapment is stronger in younger age groups, which implies we could give priority to younger infected individuals with respect to entrapment-reducing interventions. Meanwhile, we also need to find other influential factors of the mental state of entrapment and decadence for relatively high age groups in the future.
The current study involves several limitations. First, participants were recruited by non-probability sampling approaches, which may be subject to sampling bias. The non-response rate in this study was 18.4%, which may underestimate the prevalence of depression. Second, participants were recruited from one location, and we need to be cautious when applying the results to other areas. However, we did use a larger sample in our study, so the results may provide a worthy reference for the exploration of depressive mechanisms. Third, the cross-sectional study design limits our ability to establish causal mediation relationships. The mediating effect was developed and temporally validated based on the observational data. Future studies should trace changes in the psychological status of carriers at 376 later stages to further verify the causal mechanism. Fourth, other stigma-related stressors such as isolation factors or treatment factors were not studied. Future research could consider more stressors into account to understand the mechanism in depth.
5. Conclusions
This is one of the few studies to provide insights into the relationship between social stigma and depression among asymptomatic COVID-19 carriers in the post-epidemic era. Asymptomatic carriers were more likely to exhibit depression in the mid-stage of the pandemic. The current data showed the linkage between social stigma and depression through the mediating effects of entrapment and decadence. The routine assessment of stigma and screening for entrapment and decadence should be incorporated into early intervention strategies for depression among carriers to alleviate the psychological burden of the outbreak on society.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192013006/s1, Table S1. Factor loading of the Chinese version of the two subscale of Social Impact Scale (SIS) (n = 628); Table S2. Confirmatory factor analysis parameter estimation of the two subscale of SIS (n = 655); Table S3. Validity and reliability of the ES; Table S4. Confirmatory factor analysis parameter estimation of entrapment (n = 655); Table S5. Validity and reliability of the DS; Table S6. Confirmatory factor analysis parameter estimation of decadence (n = 655); Table S7. A multivariate logistic regression model of depression; Table S8. Logistic regression of depression with backward elimination/Change-In-Estimate procedure; Table S9. Parameter estimates for Mediation Analysis in the validation group (n = 298); Figure S1. The mediating role of entrapment and decadence in the relationship between stigma and depression in the training group (n = 985).
Author Contributions
Conceptualization, Z.W., Y.C. (Yong Cai) and F.H.; data curation, D.S., J.L. and X.Y.; formal analysis, H.C., Y.C. (Yingjie Chen) and Y.Z.; investigation, J.L. and X.Y.; supervision, D.S. and L.X.; writing—original draft, H.C., Y.C. (Yingjie Chen), Y.Z. and L.X.; writing—review and editing, H.C., Y.C. (Yingjie Chen), Y.Z., Z.W., Y.C. (Yong Cai) and F.H. All authors have read and agreed to the published version of the manuscript.
Funding
This work was support by Science and Technology Commission Shanghai Municipality (No. 20JC1410204) for the Seroepidemiological Study of Novel Coronavirus Pneumonia in Key Populations.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Ruijin Hospital of Shanghai JiaoTong University School of Medicine (protocol code LL202070).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not publicly available due to privacy restrictions.
Acknowledgments
The authors are grateful to the study participants for their contribution. The authors would also like to express deep gratitude to all the members of the Ruijin Jiahe Fangcang Shelter Hospital for providing assistance with recruitment and investigation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Oh, H.; Schiffman, J.; Marsh, J.; Zhou, S.; Koyanagi, A.; DeVylder, J. COVID-19 Infection and Psychotic Experiences: Findings from the Healthy Minds Study 2020. Biol. Psychiatry Glob. Open Sci. 2021, 1, 310–316. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Castaldelli-Maia, J.M.; Marziali, M.E.; Lu, Z.; Martins, S.S. Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 2021, 51, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Huang, E.; Zuo, Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 2021, 1486, 90–111. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Liu, D.; Baumeister, R.F.; Veilleux, J.C.; Chen, C.; Liu, W.; Yue, Y.; Zhang, S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res 2020, 292, 113297. [Google Scholar] [CrossRef]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-Arimi, S. Physical and mental health complications post-COVID-19: Scoping review. J. Psychosom. Res. 2021, 147, 110525. [Google Scholar] [CrossRef]
- Yuan, Y.; Zhao, Y.J.; Zhang, Q.E.; Zhang, L.; Cheung, T.; Jackson, T.; Jiang, G.-Q.; Xiang, Y.-T. COVID-19-related stigma and its sociodemographic correlates: A comparative study. Glob. Health 2021, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic Staff. COVID-19 (Coronavirus) Stigma: What It Is and How to Reduce It. 2020. Available online: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-stigma/art-20484278 (accessed on 18 June 2022).
- Brohan, E.; Slade, M.; Clement, S.; Thornicroft, G. Experiences of mental illness stigma, prejudice and discrimination: A review of measures. BMC Health Serv. Res. 2010, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.T.; Kaiser, C.R. A theoretical perspective on coping with stigma. J. Soc. Issues 2001, 57, 73–92. [Google Scholar] [CrossRef]
- Major, B.; O’Brien, L.T. The social psychology of stigma. Annu. Rev. Psychol. 2005, 56, 393–421. [Google Scholar] [CrossRef]
- Hotopf, M.; Bullmore, E.; O’Connor, R.C.; Holmes, E.A. The scope of mental health research during the COVID-19 pandemic and its aftermath. Br. J. Psychiatry 2020, 217, 540–542. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults before and during the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Xiang, Y.T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Gilbert, P.; Allan, S. The role of defeat and entrapment (arrested flight) in depression: An exploration of an evolutionary view. Psychol. Med. 1998, 28, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Price, J.; Sloman, L.; Gardner, R., Jr.; Gilbert, P.; Rohde, P. The social competition hypothesis of depression. Br. J. Psychiatry 1994, 164, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P. Depression and stress: A biopsychosocial exploration of evolved functions and mechanisms. Stress 2001, 4, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Nesse, R.M. Is depression an adaptation? Arch. Gen. Psychiatry 2000, 57, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Michail, M.; Birchwood, M. Social anxiety disorder and shame cognitions in psychosis. Psychol. Med. 2013, 43, 133–142. [Google Scholar] [CrossRef]
- Taylor, P.J.; Gooding, P.; Wood, A.M.; Tarrier, N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychol. Bull. 2011, 137, 391–420. [Google Scholar] [CrossRef]
- Smart, L.; Wegner, D.M. Covering up what can′t be seen: Concealable stigma and mental control. J. Pers. Soc. Psychol. 1999, 77, 474–486. [Google Scholar] [CrossRef]
- Fife, B.L.; Wright, E.R. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. J. Health Soc. Behav. 2000, 41, 50–67. [Google Scholar] [CrossRef]
- Li, M.; Long, J.; Wang, X.; Liao, Y.; Liu, Y.; Hao, Y.; Wu, Q.; Zhou, Y.; Wang, Y.; Wang, Y.; et al. A Comparison of COVID-19 Stigma and AIDS Stigma During the COVID-19 Pandemic: A Cross-Sectional Study in China. Front. Psychiatry 2021, 12, 782501. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.W.; Chung, L.; Fife, B.L.; Hsiung, P.C. Evaluation of the psychometrics of the Social Impact Scale: A measure of stigmatization. Int. J. Rehabil. Res. 2007, 30, 235–238. [Google Scholar] [CrossRef]
- Gong, R.J.; Wang, Y.; Cai, Y.; Wang, S. Validity and reliability of the Chinese vision of the entrapment scale in medical students. Chin. Ment. Health J 2019, 33, 393–397. [Google Scholar]
- Gilbert, P.; Allan, S.; Brough, S.; Melley, S.; Miles, J.N. Relationship of anhedonia and anxiety to social rank, defeat and entrapment. J. Affect. Disord. 2002, 71, 141–151. [Google Scholar] [CrossRef]
- Tang, H.W.S.; Gong, R.; Wang, Z.; Cai, Y. Reliability and validity of defeat scale on anxiety and depression in medical students. J. Shanghai Jiaotong Univ. Sci. 2019, 39, 84–88. [Google Scholar]
- Zung, W.W. A Self-Rating Depression Scale. Arch. Gen. Psychiatry 1965, 12, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Lei, M.; Li, C.; Xiao, X.; Qiu, J.; Dai, Y.; Zhang, Q. Evaluation of the psychometric properties of the Chinese version of the Resilience Scale in Wenchuan earthquake survivors. Compr. Psychiatry 2012, 53, 616–622. [Google Scholar] [CrossRef]
- Feng, Q.; Zhang, Q.L.; Du, Y.; Ye, Y.L.; He, Q.Q. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS ONE 2014, 9, e100914. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, R.; Li, G.; Mao, S.; Yuan, Y. The reliability and validity of a Chinese-version Short Health Anxiety Inventory: An investigation of university students. Neuropsychiatr. Dis. Treat. 2015, 11, 1739–1747. [Google Scholar] [CrossRef]
- Weng, H.Y.; Hsueh, Y.H.; Messam, L.L.; Hertz, P.I. Methods of covariate selection: Directed acyclic graphs and the change-in-estimate procedure. Am. J. Epidemiol. 2009, 169, 1182–1190. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Wen, Z.; Ye, B. Analyses of mediating effects: The development of methods and models (in Chinese with an English abstract). Adv. Psychol. Sci. 2014, 22, 731–745. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD Statement. BMC Med. 2015, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.F.; Li, W.; Deng, H.B.; Wang, L.; Wang, Y.; Wang, P.-H.; Bo, H.-X.; Cao, J.; Wang, Y.; Zhu, L.-Y.; et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020, 275, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T. Mediating Effects and Moderating Effects in Causal Inference (in Chinese with an English abstract). China Ind. Econ. 2022, 5, 100–120. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Ding, K.; Yang, J.; Chin, M.-K.; Sullivan, L.; Demirhan, G.; Violant-Holz, V.; Uvinha, R.R.; Dai, J.; Xu, X.; Popeska, B.; et al. Mental Health among Adults during the COVID-19 Pandemic Lockdown: A Cross-Sectional Multi-Country Comparison. Int. J. Environ. Res. Public Health 2021, 18, 2686. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. J. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatr. 2020, 33, e100213. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).