Estimating the Health Effect of Cigarette Smoking Duration in South Africa
Abstract
1. Introduction
2. Material and Methods
2.1. Data and Key Variables
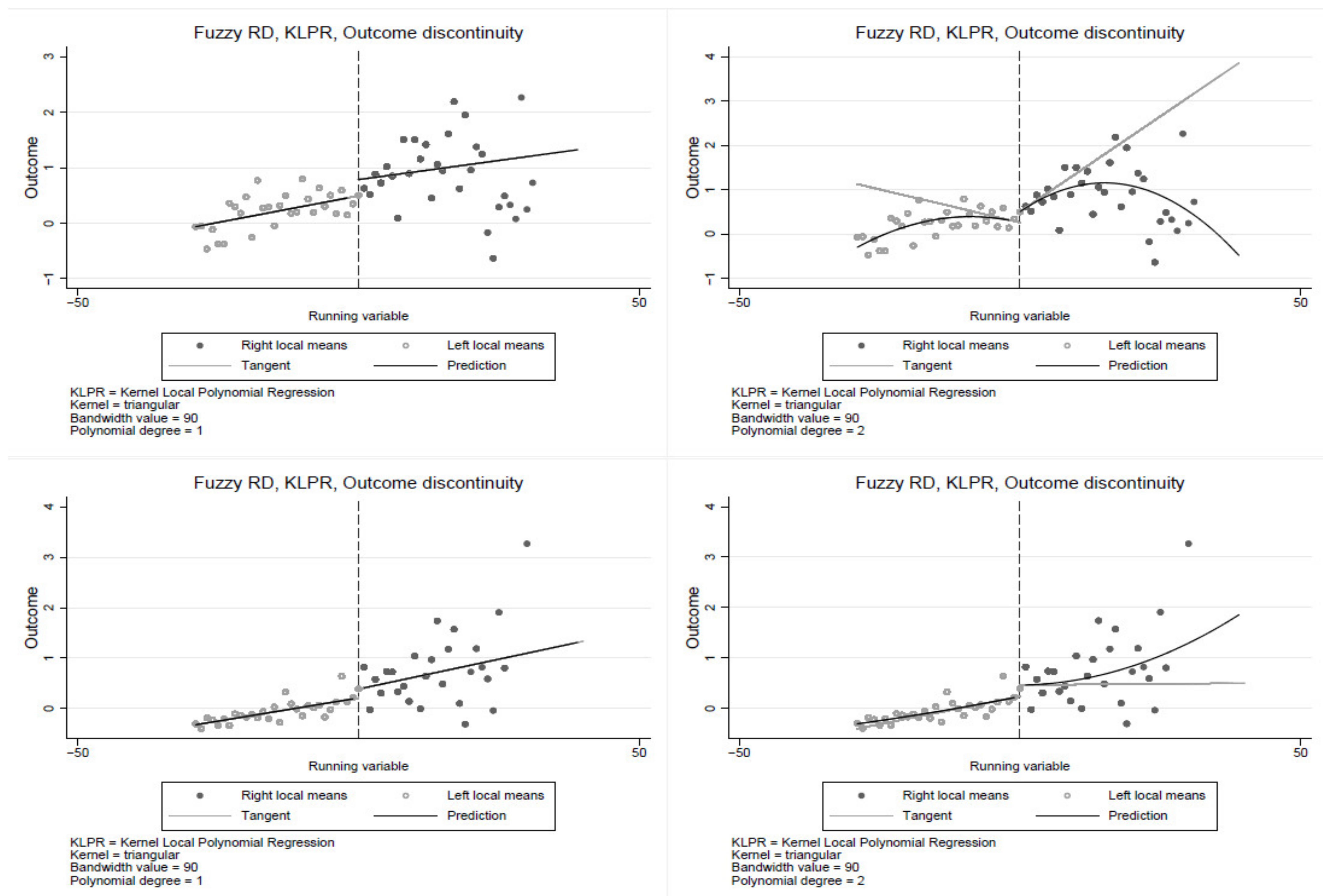
2.2. Empirical Strategy
3. Results
3.1. Descriptive Statistics
3.2. Empirical Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Terzic, A.; Waldman, S. Chronic diseases: The emerging pandemic. Clin. Transl. Sci. 2011, 4, 225–226. [Google Scholar] [CrossRef] [PubMed]
- Alwan, A. Global Status Report on Non-Communicable Diseases 2010; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Trédaniel, J.; Boffetta, P.; Saracci, R.; Hirsch, A. Environmental tobacco smoke and the risk of cancer in adults. Eur. J. Cancer 1993, 29, 2058–2068. [Google Scholar] [CrossRef]
- Law, M.R.; Morris, J.; Wald, N.J. Environmental tobacco smoke exposure and ischaemic heart disease: An evaluation of the evidence. BMJ 1997, 315, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Brennan, P.; Buffler, P.A.; Reynolds, P.; Wu, A.H.; Wichmann, H.E.; Agudo, A.; Pershagen, G.; Jöckel, K.-H.; Benhamou, S.; Greenberg, R.S.; et al. Secondhand smoke exposure in adulthood and risk of lung cancer among never smokers: A pooled analysis of two large studies. Int. J. Cancer 2004, 109, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Costenbader, K.H.; Feskanich, D.; Mandl, L.A.; Karlson, E.W. Smoking intensity, duration, and cessation, and the risk of rheumatoid arthritis in women. Am. J. Med. 2006, 119, 503-e1. [Google Scholar] [CrossRef]
- Ng, M.; Freeman, M.K.; Fleming, T.D.; Robinson, M.; Dwyer-Lindgren, L.; Thomson, B.; Wollum, A.; Sanman, E.; Wulf, S.; Lopez, A.D.; et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. Jama 2014, 311, 183–192. [Google Scholar] [CrossRef]
- Ezzati, M.; Lopez, A.D. Estimates of global mortality attributable to smoking in 2000. Lancet 2003, 362, 847–852. [Google Scholar] [CrossRef]
- Vallejo-Torres, L.; Morris, S. The contribution of smoking and obesity to income-related inequalities in health in England. Soc. Sci. Med. 2010, 71, 1189–1198. [Google Scholar] [CrossRef]
- Mukong, A.K.; Van Walbeek, C.; Ross, H. Lifestyle and Income-related Inequality in Health in South Africa. Int. J. Equity Health 2017, 16, 103. [Google Scholar] [CrossRef]
- Rezayatmand, R.; Groot, W.; Pavlova, M. Smoking behaviour and health care costs coverage: A European cross-country comparison. Int. J. Health Econ. Manag. 2017, 17, 453–471. [Google Scholar] [CrossRef]
- Goodchild, M.; Nargis, N.; D’Espaignet, E.T. Global economic cost of smoking-attributable diseases. Tob. Control 2018, 27, 58–64. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Statistics South Africa. Mortality and Causes of Death in South Africa, 2016: Findings from Death Notification; Statistics South Africa: Pretoria, South Africa, 2018.
- Peto, R. Influence of dose and duration of smoking on lung cancer rates. IARC Sci. Publ. 1986, 74, 23–33. [Google Scholar]
- Jha, P.; Chaloupka, F.J. Tobacco Control in Developing Countries; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Chen, H.; Huang, X.; Guo, X.; Mailman, R.; Park, Y.; Kamel, F.; Umbach, D.; Xu, Q.; Hollenbeck, A.; Schatzkin, A.; et al. Smoking duration, intensity, and risk of Parkinson disease. Neurology 2010, 74, 878–884. [Google Scholar] [CrossRef]
- Knoke, J.D.; Shanks, T.G.; Vaughn, J.W.; Thun, M.J.; Burns, D.M. Lung Cancer Mortality Is Related to Age in Addition to Duration and Intensity of Cigarette Smoking: An Analysis of CPS-I Data. Cancer Epidemiol. Biomark. Prev. 2004, 13, 949–957. [Google Scholar] [CrossRef]
- Flanders, W.D.; Lally, C.A.; Zhu, B.-P.; Henley, S.J.; Thun, M.J. Lung cancer mortality in relation to age, duration of smoking, and daily cigarette consumption: Results from Cancer Prevention Study II. Cancer Res. 2003, 63, 6556–6562. [Google Scholar] [PubMed]
- Jackson, D.J.; Batiste, E.; Rendall-Mkosi, K. Effect of smoking and alcohol use during pregnancy on the occurrence of low birthweight in a farming region in South Africa. Paediatr. Périnat. Epidemiol. 2007, 21, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Chikte, U.; Pontes, C.C.; Karangwa, I.; Kimmie-Dhansay, F.; Erasmus, R.T.; Kengne, A.P.; Matsha, T.E. Periodontal Disease Status among Adults from South Africa—Prevalence and Effect of Smoking. Int. J. Environ. Res. Public Health 2019, 16, 3662. [Google Scholar] [CrossRef]
- Tomita, A.; I Manuel, J. Evidence on the Association Between Cigarette Smoking and Incident Depression from the South African National Income Dynamics Study 2008–2015: Mental Health Implications for a Resource-Limited Setting. Nicotine Tob. Res. 2020, 22, 118–123. [Google Scholar] [CrossRef]
- Mukong, A.; Tingum, E. The demand for cigarettes: New evidence from South Africa. Tob. Induc. Dis. 2019, 16, 1–15. [Google Scholar]
- Cancer Society of South Africa. Fact Sheet on Tobacco Products. Available online: https://www.tandfonline.com/doi/full/10.1080/0376835X.2019.1640108 (accessed on 30 August 2022).
- Stats SA (Statistics South Africa). Mortality and Causes of Death from Death Notification 2015; Stats SA: Pretoria, South Africa, 2017.
- Sitas, F.; Harris-Roxas, B.; Bradshaw, D.; Lopez, A.D. Smoking and epidemics of respiratory infections. Bull. World Health Organ. 2021, 99, 164–165. [Google Scholar] [CrossRef]
- Hurst, R.; Rollema, H.; Bertrand, D. Nicotinic acetylcholine receptors: From basic science to therapeutics. Pharmacol. Ther. 2013, 137, 22–54. [Google Scholar] [CrossRef] [PubMed]
- Harling, G.; Ehrlich, R.; Myer, L. The social epidemiology of tuberculosis in South Africa: A multilevel analysis. Soc. Sci. Med. 2008, 66, 492–505. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.P.; Connett, J.E.; Zapawa, L.M. Does nicotine replacement therapy cause cancer? Evidence from the Lung Health Study. Nicotine Tob. Res. 2009, 11, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Schane, R.E.; Ling, P.M.; Glantz, S.A. Health effects of light and intermittent smoking: A review. Circulation 2010, 121, 1518–1522. [Google Scholar] [CrossRef] [PubMed]
- Wolf, P.A.; Agostino, R.B.D.; Kannel, W.B.; Bonita, R.; Belanger, A.J. Cigarette smoking as a risk factor for stroke: The Framingham Study. Jama 1988, 259, 1025–1029. [Google Scholar] [CrossRef]
- Boden, J.; Fergusson, D.; Horwood, L. Cigarette smoking and depression: Tests of causal linkages using a longitudinal birth cohort. Br. J. Psychiatry 2010, 196, 440–446. [Google Scholar] [CrossRef]
- Kimengsi, J.N.; Mukong, A.K.; Giessen, L.; Pretzsch, J. Institutional dynamics and forest use practices in the Santchou Landscape of Cameroon. Environ. Sci. Policy 2022, 128, 68–80. [Google Scholar] [CrossRef]
- Kimengsi, J.N.; Mukong, A.K. Forest resource endogenous cultural institutions in rural Cameroon: Compliance determinants and policy implications. J. Environ. Plan. Manag. 2022, 1–22. [Google Scholar] [CrossRef]
- Ntuli, H.; Mukong, A.K.; Kimengsi, J.N. Institutions and environmental resource extraction within local communities in Mozambique. For. Policy Econ. 2022, 139, 102724. [Google Scholar] [CrossRef]
- Benjamins, M.R.; A Hummer, R.; Eberstein, I.W.; Nam, C.B. Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Soc. Sci. Med. 2004, 59, 1297–1306. [Google Scholar] [CrossRef]
- Van Doorslaer, E.; Gerdtham, U.-G. Does inequality in self-assessed health predict inequality in survival by income? Evidence from Swedish data. Soc. Sci. Med. 2003, 57, 1621–1629. [Google Scholar] [CrossRef]
- Yörük, B.K.; Yörük, C.E. The impact of minimum legal drinking age laws on alcohol consumption, smoking, and marijuana use: Evidence from a regression discontinuity design using exact date of birth. J. Health Econ. 2011, 30, 740–752. [Google Scholar] [CrossRef]
- Cheng, M.-Y.; Fan, J.; Marron, J.S. On automatic boundary corrections. Ann. Stat. 1997, 25, 1691–1708. [Google Scholar] [CrossRef]
- Imbens, G.; Kalyanaraman, K. Optimal Bandwidth Choice for the Regression Discontinuity Estimator. Rev. Econ. Stud. 2009, 79, 933–959. [Google Scholar] [CrossRef]
- Thacker, E.L.; OReilly, E.J.; Weisskopf, M.G.; Chen, H.; Schwarzschild, M.A.; McCullough, M.L.; Calle, E.E.; Thun, M.J.; Ascherio, A. Temporal relationship between cigarette smoking and risk of Parkinson disease. Neurology 2007, 68, 764–768. [Google Scholar] [CrossRef]
- Ritz, B.; Ascherio, A.; Checkoway, H.; Marder, K.S.; Nelson, L.M.; Rocca, W.A.; Ross, G.W.; Strickland, D.; Eeden, S.K.V.D.; Gorell, J. Pooled Analysis of Tobacco Use and Risk of Parkinson Disease. Arch. Neurol. 2007, 64, 990–997. [Google Scholar] [CrossRef]
- Terzikhan, N.; Verhamme, K.M.C.; Hofman, A.; Stricker, B.H.; Brusselle, G.; Lahousse, L. Prevalence and incidence of COPD in smokers and non-smokers: The Rotterdam Study. Eur. J. Epidemiol. 2016, 31, 785–792. [Google Scholar] [CrossRef]
- Pezzuto, A.; Lionetto, L.; Ricci, A.; Simmaco, M.; Borro, M. Inter-individual variation in CYP2A6 activity and chronic obstructive pulmonary disease in smokers: Perspectives for an early predictive marker. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1867, 165990. [Google Scholar] [CrossRef]
- Pleasants, R.A.; Rivera, M.P.; Tilley, S.L.; Bhatt, S.P. Both Duration and Pack-Years of Tobacco Smoking Should Be Used for Clinical Practice and Research. Ann. Am. Thorac. Soc. 2020, 17, 804–806. [Google Scholar] [CrossRef]



| All Individuals | Smokers Only | |||||
|---|---|---|---|---|---|---|
| Variable | Obs. | Mean | Std. Dev. | Obs. | Mean | Std. Dev. |
| Individual is a current smoker | 22,727 | 0.203 | 0.403 | |||
| Have years of smoking for smokers | 4267 | 17.34 | 0.332 | |||
| Diagnosed of tuberculosis | 21,937 | 0.035 | 0.184 | 4038 | 0.056 | 0.230 |
| Diagnosed of high blood pressure | 20,358 | 0.106 | 0.308 | 3897 | 0.098 | 0.297 |
| Diagnosed of diabetes | 22,034 | 0.036 | 0.187 | 4176 | 0.027 | 0.162 |
| Diagnosed of stroke | 22,575 | 0.009 | 0.096 | 4240 | 0.010 | 0.099 |
| Diagnosed of a heart disease | 22,356 | 0.018 | 0.134 | 4179 | 0.020 | 0.141 |
| Diagnosed of cancer | 22,648 | 0.013 | 0.114 | 4250 | 0.016 | 0.124 |
| Have persistent cough | 22,737 | 0.127 | 0.333 | 4265 | 0.168 | 0.374 |
| Experienced depression | 22,742 | 0.447 | 0.497 | 4263 | 0.505 | 0.500 |
| Experienced chest pain | 22,735 | 0.093 | 0.291 | 4264 | 0.128 | 0.334 |
| Self-reported poor health | 22,744 | 0.108 | 0.311 | 4262 | 0.126 | 0.332 |
| Health index | 19,440 | 0.026 | 1.247 | 3642 | 0.175 | 1.335 |
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Variables | SAH | Index | SAH | Index | SAH | Index | SAH | Index |
| 10 years | 0.025 | 0.101 ** | 0.020 | 0.160 *** | 0.012 | 0.206 *** | 0.012 | 0.128 *** |
| (0.015) | (0.041) | (0.015) | (0.046) | (0.013) | (0.039) | (0.011) | (0.033) | |
| 10–19 years | 0.023 | 0.091 ** | 0.012 | 0.141 *** | 0.029 ** | 0.094 ** | 0.037 *** | 0.150 *** |
| (0.015) | (0.046) | (0.014) | (0.052) | (0.013) | (0.044) | (0.011) | (0.040) | |
| 20–29 years | 0.026 * | 0.250 *** | 0.060 *** | 0.378 *** | 0.053 *** | 0.155 *** | 0.036 *** | 0.116 ** |
| (0.014) | (0.050) | (0.015) | (0.057) | (0.013) | (0.050) | (0.011) | (0.049) | |
| 30+ years | 0.065 *** | 0.365 *** | 0.028 ** | 0.474 *** | 0.059 *** | 0.386 *** | 0.040 *** | 0.313 *** |
| (0.013) | (0.045) | (0.011) | (0.052) | (0.011) | (0.045) | (0.009) | (0.048) | |
| Constant | −0.979 *** | −1.146 *** | −0.732 *** | −0.482 *** | ||||
| (0.099) | (0.096) | (0.091) | (0.075) | |||||
| Observations | 14,912 | 14,847 | 16,321 | 16,048 | 18,322 | 18,188 | 22,241 | 19,037 |
| R-squared | 0.106 | 0.129 | 0.139 | 0.100 | ||||
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Index | SAH | Index | SAH | Index | SAH | Index | SAH | |
| ATET | 0.142 *** | 0.035 *** | 0.139 *** | 0.023 *** | 0.164 *** | 0.042 *** | 0.103 *** | 0.024 *** |
| (0.029) | (0.009) | (0.032) | (0.008) | (0.028) | (0.007) | (0.026) | (0.006) | |
| Observations | 15,241 | 15,307 | 16,432 | 16,717 | 18,516 | 18,651 | 19,367 | 22,657 |
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||
| Female | Male | Female | Male | Female | Male | Female | Male | |
| ATET | 0.133 *** | 0.148 *** | 0.132 ** | 0.150 *** | 0.288 *** | 0.135 *** | 0.168 *** | 0.093 *** |
| (0.049) | (0.037) | (0.067) | (0.039) | (0.057) | (0.033) | (0.058) | (0.030) | |
| Observations | 9131 | 6111 | 9626 | 6806 | 11,031 | 7486 | 10,901 | 8467 |
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black | Coloured | White | Black | Coloured | White | Black | Coloured | White | Black | Coloured | White | |
| ATET | 0.16 *** | 0.13 ** | 0.14 * | 0.19 *** | 0.00 | 0.29 * | 0.17 *** | 0.09 | 0.31 ** | 0.10 *** | 0.10 * | 0.14 |
| (0.04) | (0.06) | (0.07) | (0.03) | (0.07) | (0.16) | (0.03) | (0.06) | (0.13) | (0.03) | (0.06) | (0.12) | |
| Observations | 12,001 | 2143 | 1097 | 13,718 | 2091 | 624 | 15,245 | 2555 | 716 | 16,345 | 2441 | 582 |
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||||||
| Primary | Secondary | Tertiary | Primary | Secondary | Tertiary | Primary | Secondary | Tertiary | Primary | Secondary | Tertiary | |
| ATET | 0.24 *** | 0.05 | 0.20 *** | 0.16 ** | 0.12 *** | 0.02 | 0.20 *** | 0.11 *** | 0.23 *** | 0.15 ** | 0.08 *** | 0.18 *** |
| (0.05) | (0.03) | (0.08) | (0.06) | (0.04) | (0.10) | (0.06) | (0.03) | (0.08) | (0.07) | (0.03) | (0.07) | |
| Observations | 5811 | 8355 | 1076 | 5835 | 9492 | 1105 | 5941 | 10,862 | 1713 | 4526 | 12,585 | 2256 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mukong, A.K. Estimating the Health Effect of Cigarette Smoking Duration in South Africa. Int. J. Environ. Res. Public Health 2022, 19, 13005. https://doi.org/10.3390/ijerph192013005
Mukong AK. Estimating the Health Effect of Cigarette Smoking Duration in South Africa. International Journal of Environmental Research and Public Health. 2022; 19(20):13005. https://doi.org/10.3390/ijerph192013005
Chicago/Turabian StyleMukong, Alfred Kechia. 2022. "Estimating the Health Effect of Cigarette Smoking Duration in South Africa" International Journal of Environmental Research and Public Health 19, no. 20: 13005. https://doi.org/10.3390/ijerph192013005
APA StyleMukong, A. K. (2022). Estimating the Health Effect of Cigarette Smoking Duration in South Africa. International Journal of Environmental Research and Public Health, 19(20), 13005. https://doi.org/10.3390/ijerph192013005






