Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. General Setting
2.3. Specific Setting
2.4. Participants
2.5. Variables
2.6. Data Collection
2.7. Statistical Analysis
3. Results
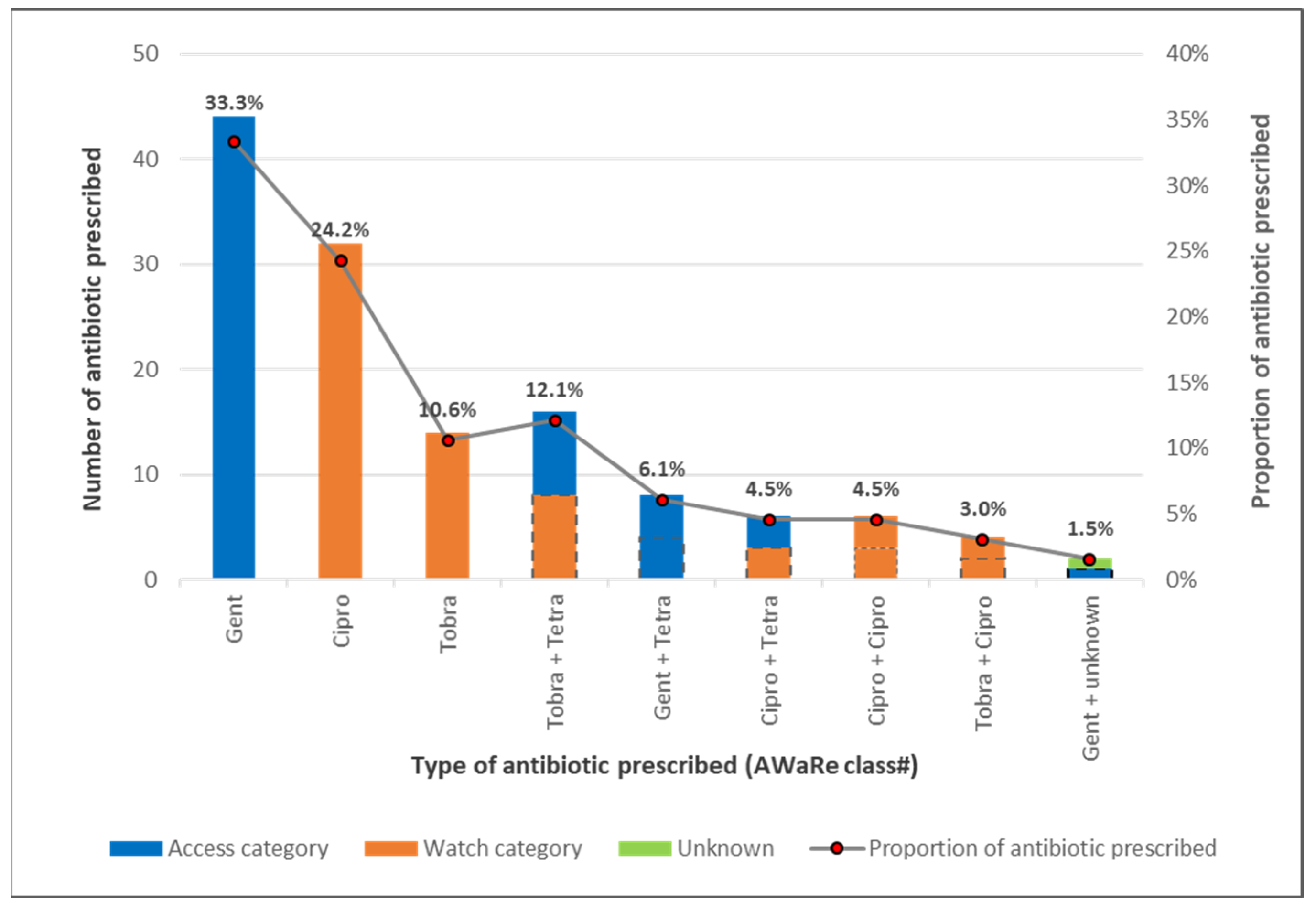
- Proportions for each of the AwaRe class calculated on total number of antibiotic prescribed as the denominator.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leibowitz, H.M. The Red Eye. N. Engl. J. Med. 2000, 343, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Tarabishy, A.B.; Jeng, B.H. Bacteria Conjunctivitis: A Review for Internists. Cleve. Clin. J. Med. 2008, 75, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Friedlaender, M.H. A Review of the Causes and Treatment of Bacterial and Allergic Conjunctivitis. Clin. Ther. 1995, 17, 800–810. [Google Scholar] [CrossRef]
- Azari, A.A.; Barney, N.P. Conjunctivitis: A Systematic Review of Diagnosis and Treatment. JAMA-J. Am. Med. Assoc. 2013, 310, 1721–1729. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, S.A.; Fawley, J.D.; Lu, X.A. Conjunctivitis. Prim. Care-Clin. Off. Pract. 2015, 42, 325–345. [Google Scholar] [CrossRef]
- Opoku-Yamoah, V.; Afrifa-Yamoah, E. Ocular Morbidity Pattern among Patients Attending Red Cross Eye Unit in Sunyani. Int. J. Health Allied Sci. 2021, 10, 197–201. [Google Scholar]
- Rose, P. Management Strategies for Acute Infective Conjunctivitis in Primary Care: A Systematic Review. Expert Opin. Pharmacother. 2007, 8, 1903–1921. [Google Scholar] [CrossRef]
- Jefferis, J.; Perera, R.; Everitt, H.; Van Weert, H.; Rietveld, R.; Glasziou, P.; Rose, P. Acute Infective Conjunctivitis in Primary Care: Who Needs Antibiotics? An Individual Patient Data Meta-Analysis. Br. J. Gen. Pract. 2011, 61, 542–548. [Google Scholar] [CrossRef]
- Spellberg, B.; Blaser, M.; Guidos, R.J.; Boucher, H.W.; Bradley, J.S.; Eisenstein, B.I.; Gerding, D.; Lynfield, R.; Reller, L.B.; Rex, J.; et al. Combating Antimicrobial Resistance: Policy Recommendations to Save Lives. Clin. Infect. Dis. 2011, 52, 397–428. [Google Scholar] [CrossRef]
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance; World Health Organization, 2014. Available online: https://apps.who.int/iris/handle/10665/112642 (accessed on 15 September 2022).
- Steyn, L. Allergy or Infection? A Red-Eye Review. SA Pharm. J. 2021, 88, 10–15. [Google Scholar]
- Bernabé, K.; Langendorf, C.; Ford, N.; Ronat, J.; Murphy, R. Antimicrobial Resistance in West Africa: A Systematic Review and Meta-Analysis. Int. J. Antimicrob. Agents. 2017, 50, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Newman, M.J.; Frimpong, E.; Donkor, E.S.; Opintan, J.A.; Asamoah-Adu, A. Resistance to Antimicrobial Drugs in Ghana. Biol. Trace Elem. Res. 2011, 4, 215–220. [Google Scholar] [CrossRef]
- Opintan, J.; Newman, M.; Arhin, R.; Donkor, E.; Gyansa-Lutterodt, M.; Mills-Pappoe, W. Laboratory-Based Nationwide Surveillance of Antimicrobial Resistance in Ghana. Infect. Drug Resist. 2015, 8, 379–389. [Google Scholar] [CrossRef]
- World Health Organization; Heymann, D.L.; Prentice, T.; Reinders, L.T. The World Health Report 2007: A Safer Future: Global Public Health Security in the 21st Century; World Health Organization: Geneva, Switzerland, 2007.
- Xavier, S.P.; Victor, A.; Cumaquela, G.; Vasco, M.D.; Rodrigues, O.A.S. Inappropriate Use of Antibiotics and Its Predictors in Pediatric Patients Admitted at the Central Hospital of Nampula, Mozambique. Antimicrob. Resist. Infect. Control 2022, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U. Antibiotic Use among Hospitalized Patients in Northern Nigeria: A Multicenter Point-Prevalence Survey. BMC Infect. Dis. 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Ministry of Health Republic of Ghana. Policy on Antimicrobial Use and Resistance, 1st ed.; 2017. Available online: https://www.moh.gov.gh/wp-content/uploads/2018/04/AMR-POLICY-A5_09.03.2018-Signed.pdf (accessed on 15 September 2022)ISBN 9789988266547.
- World Health Organization. The 2019 WHO AWaRe Classification of Antibiotics for Evaluation and Monitoring of Use; World Health Organization, 2019. Available online: https://apps.who.int/iris/handle/10665/327957 (accessed on 15 September 2022).
- World Health Organization. Antimicrobial Stewardship Programmes in Health-Care Facilities in Low- and Middle-Income Countries: A WHO Practical Toolkit. Available online: https://apps.who.int/iris/handle/10665/329404 (accessed on 9 August 2022).
- Rietveld, R.P.; Van Weert, H.C.P.M.; Ter Riet, G.; Bindels, P.J.E. Diagnostic Impact of Signs and Symptoms in Acute Infectious Conjunctivitis: Systematic Literature Search. Br. Med. J. 2003, 327, 789. [Google Scholar] [CrossRef]
- Ouedraogo, A.; Jean Pierre, H.; Bañuls, A.; Ouédraogo, R.; Godreuil, S. Emergence and Spread of Antibiotic Resistance in West Africa: Contributing Factors and Threat Assessment. Med. Sante Trop. 2017, 1, 147–154. [Google Scholar] [CrossRef]
- Ministry of Health; (GNDP). Standard Treatment Guidelines; World Health Organization, 2009; ISBN 9789988257873. Available online: https://www.moh.gov.gh/wp-content/uploads/2020/07/GHANA-STG-2017-1.pdf (accessed on 15 September 2022).
- World Health Organization. The AWaRe Classification of Antibiotics Database; World Health Organization, 2019. Available online: https://www.who.int/publications-detail-redirect/WHOEMPIAU2019.11 (accessed on 15 September 2022).
- WHO Methodology for Point Prevalence Survey on Antibiotic Use in Hospitals. Available online: https://www.who.int/publications/i/item/WHO-EMP-IAU-2018.01 (accessed on 10 August 2022).
- Agyemang-Mireku, F. Pattern of Ocular Conditions among Patients Attending an Eye Clinic in Ghana. Optom. Open Access. 2017, 2, 122. [Google Scholar]
- Abera, B.; Kibret, M. Azithromycin, Fluoroquinolone and Chloramphenicol Resistance of Non-Chlamydia Conjunctival Bacteria in Rural Community of Ethiopia. Indian J. Ophthalmol. 2014, 62, 236–239. [Google Scholar] [CrossRef]
- Sheikh, A. Acute Bacterial Conjunctivitis; John Wiley & Sons, Ltd.: London, UK, 2005. [Google Scholar]
- Høvding, G. Acute Bacterial Conjunctivitis. Acta Ophthalmol. 2008, 86, 5–17. [Google Scholar] [CrossRef]
- Yeu, E.; Hauswirth, S. A Review of the Differential Diagnosis of Acute Infectious Conjunctivitis: Implications for Treatment and Management. Clin. Ophthalmol. 2020, 14, 805. [Google Scholar] [CrossRef] [PubMed]
- Rietveld, R.P.; ter Riet, G.; Bindels, P.J.; Sloos, J.H.; van Weert, H.C. Predicting Bacterial Cause in Infectious Conjunctivitis: Cohort Study on Informativeness of Combinations of Signs and Symptoms. BMJ 2004, 329, 206–210. [Google Scholar] [CrossRef] [PubMed]
- van Weert, H.C.; Tellegen, E.; Ter Riet, G. A New Diagnostic Index for Bacterial Conjunctivitis in Primary Care. A Re-Derivation Study. Eur. J. Gen. Pract. 2014, 20, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Kopke, A. Treating Bacterial Conjunctivitis—A Bird’s Eye View. S. Afr. Gen. Pract. 2021, 2, 128–130. [Google Scholar]
- Charles, R.C.; Lim, H.K.; Charles, W.N. Clarity and Confidence in Managing Infective Conjunctivitis. J. Prim. Health Care 2021, 13, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Amponsah, O.K.O.; Buabeng, K.O.; Owusu-Ofori, A.; Ayisi-Boateng, N.K.; Hämeen-Anttila, K.; Enlund, H. Point Prevalence Survey of Antibiotic Consumption across Three Hospitals in Ghana. JAC-Antimicrob. Resist. 2021, 3, 1–7. [Google Scholar] [CrossRef]
- Shekhawat, N.; Shtein, R.; Blachley, T.; Stein, J. Antibiotic Prescription Fills for Acute Conjunctivitis among Enrollees in a Large United States Managed Care Network. Ophthalmology 2017, 124, 1099–1107. [Google Scholar] [CrossRef]
- Epling, J. Bacterial Conjunctivitis. BMJ Clin. Evid 2012, 2, 1–21. [Google Scholar]

| Variable | Patients with Acute Conjunctivitis n (%) |
|---|---|
| Age (Years) (n = 201) | |
| <5 years | 78 (39) |
| 5–17 years | 43 (21) |
| ≥18 years | 80 (40) |
| Sex (n = 201) | |
| Male | 89 (44) |
| Female |
| Variable | Number of Patients n (%) |
|---|---|
| Antibiotic prescribed (n = 201) | |
| Yes | 111 (55.2) |
| No | 90 (44.8) |
| Attending Cadre (n = 201) | |
| Ophthalmologist | 2 (1.0) |
| Optometrist | 107 (53.2) |
| Ophthalmic nurse | 92 (45.8) |
| Appropriate antibiotic prescription (n = 111) | |
| Yes | 79 (71.2) |
| No | 32 (28.8) |
| Variable | Acute Conjunctivitis Cases | Antibiotics Prescription | p-Value | ||
|---|---|---|---|---|---|
| N | Yes (n = 111) | No (n = 90) | Total (n = 201) | ||
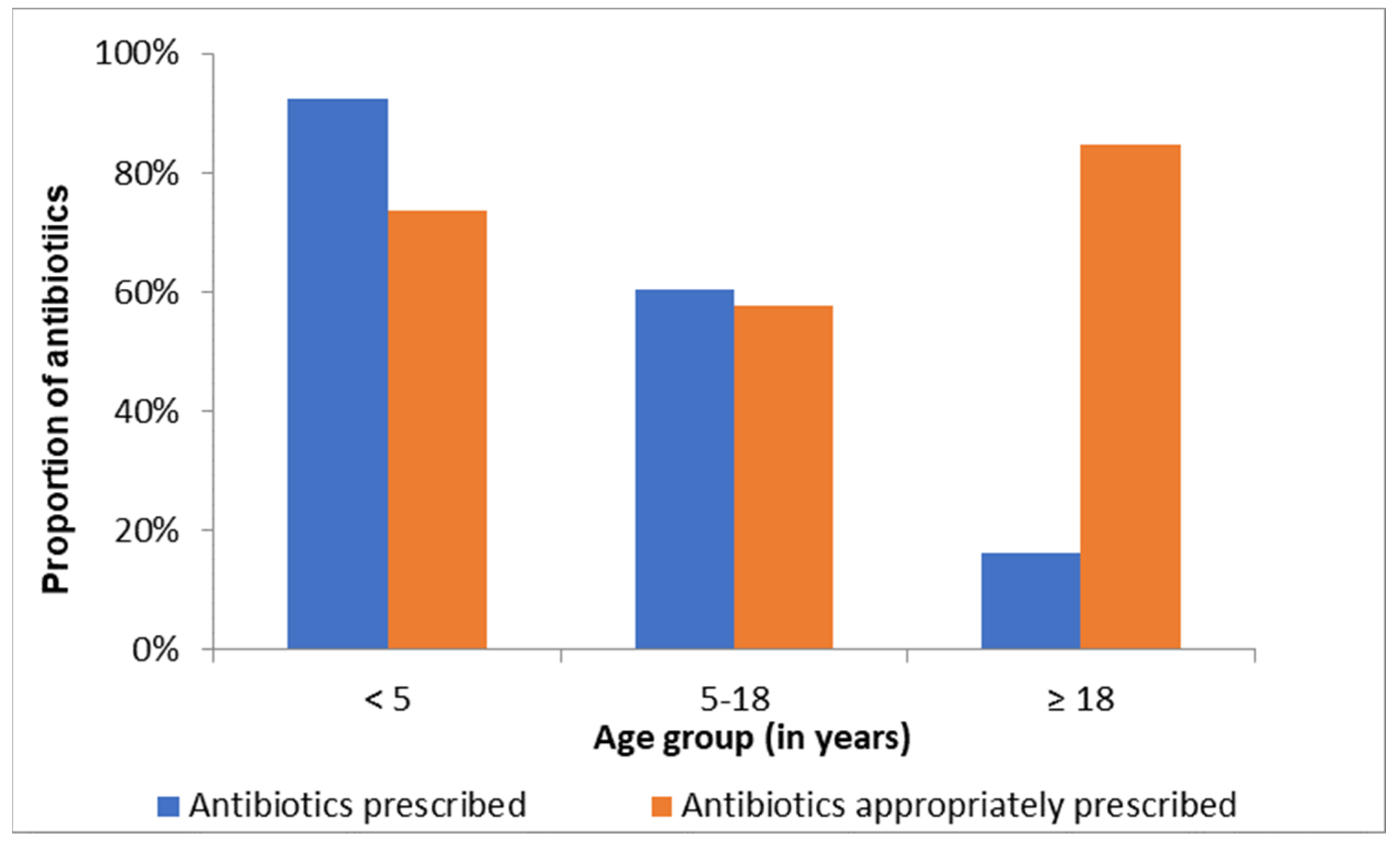
| Age groups (in years) | 201 | <0.0001 c | |||
| <5 years | 72 (92.3%) | 6 (7.7%) | 78 (100%) | ||
| 5–17 years | 26 (60.5%) | 17 (39.5%) | 43 (100%) | ||
| ≥18 years | 13 (16.2%) | 67 (83.8%) | 80 (100%) | ||
| Sex | 201 | 0.214 c | |||
| Male | 54 (60.7%) | 35 (39.3%) | 89 (100%) | ||
| Female | 57 (50.9%) | 55 (49.1%) | 112 (100%) | ||
| Cadre | 201 | 0.843 | |||
| Ophthalmologist|Optometrist | 59 (54.1%) | 50 (45.9%) | 109 (100%) | ||
| Ophthalmic nurse | 52 (56.5%) | 40 (43.5%) | 92 (100%) | ||
| Variable | Prescribed Antibiotics Cases | Appropriate Prescription | p-Value | ||
|---|---|---|---|---|---|
| N | Yes (n = 79) | No (n = 32) | Total (n = 111) | ||
| Age groups (in years) | 111 | 0.164 f | |||
| <5 years | 53 (73.6%) | 19 (26.4%) | 72 (100%) | ||
| 5–18 years | 15 (57.7%) | 11 (42.3%) | 26 (100%) | ||
| ≥18 years | 11 (84.6%) | 2 (15.4%) | 13 (100%) | ||
| Sex | 111 | 0.696 c | |||
| Male | 37 (68.5%) | 17 (31.5%) | 54 (100%) | ||
| Female | 42 (73.7%) | 15 (26.3%) | 57 (100%) | ||
| Attending Cadre | 111 | 0.526 f | |||
| Ophthalmologist/Optometrist | 44 (74.6%) | 15 (25.4%) | 59 (100%) | ||
| Ophthalmic nurse | 35 (67.3%) | 17 (32.7%) | 52 (100%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hope, P.K.F.; Lynen, L.; Mensah, B.; Appiah, F.; Kamau, E.M.; Ashubwe-Jalemba, J.; Peprah Boaitey, K.; Adomako, L.A.B.; Alaverdyan, S.; Appiah-Thompson, B.L.; et al. Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021. Int. J. Environ. Res. Public Health 2022, 19, 11723. https://doi.org/10.3390/ijerph191811723
Hope PKF, Lynen L, Mensah B, Appiah F, Kamau EM, Ashubwe-Jalemba J, Peprah Boaitey K, Adomako LAB, Alaverdyan S, Appiah-Thompson BL, et al. Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021. International Journal of Environmental Research and Public Health. 2022; 19(18):11723. https://doi.org/10.3390/ijerph191811723
Chicago/Turabian StyleHope, Paa Kwesi Fynn, Lutgarde Lynen, Baaba Mensah, Faustina Appiah, Edward Mberu Kamau, Jacklyne Ashubwe-Jalemba, Kwame Peprah Boaitey, Lady Asantewah Boamah Adomako, Sevak Alaverdyan, Benedicta L. Appiah-Thompson, and et al. 2022. "Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021" International Journal of Environmental Research and Public Health 19, no. 18: 11723. https://doi.org/10.3390/ijerph191811723
APA StyleHope, P. K. F., Lynen, L., Mensah, B., Appiah, F., Kamau, E. M., Ashubwe-Jalemba, J., Peprah Boaitey, K., Adomako, L. A. B., Alaverdyan, S., Appiah-Thompson, B. L., Kwarteng Amaning, E., & Baanam, M. Y. (2022). Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021. International Journal of Environmental Research and Public Health, 19(18), 11723. https://doi.org/10.3390/ijerph191811723









