Interstitial Pregnancy Treated with Mifepristone and Methotrexate with High Serum β-hCG Level in a Patient Wishing to Preserve Fertility: Time to Define Standardized Criteria for Medical/Surgical Therapy?
Abstract
:1. Introduction
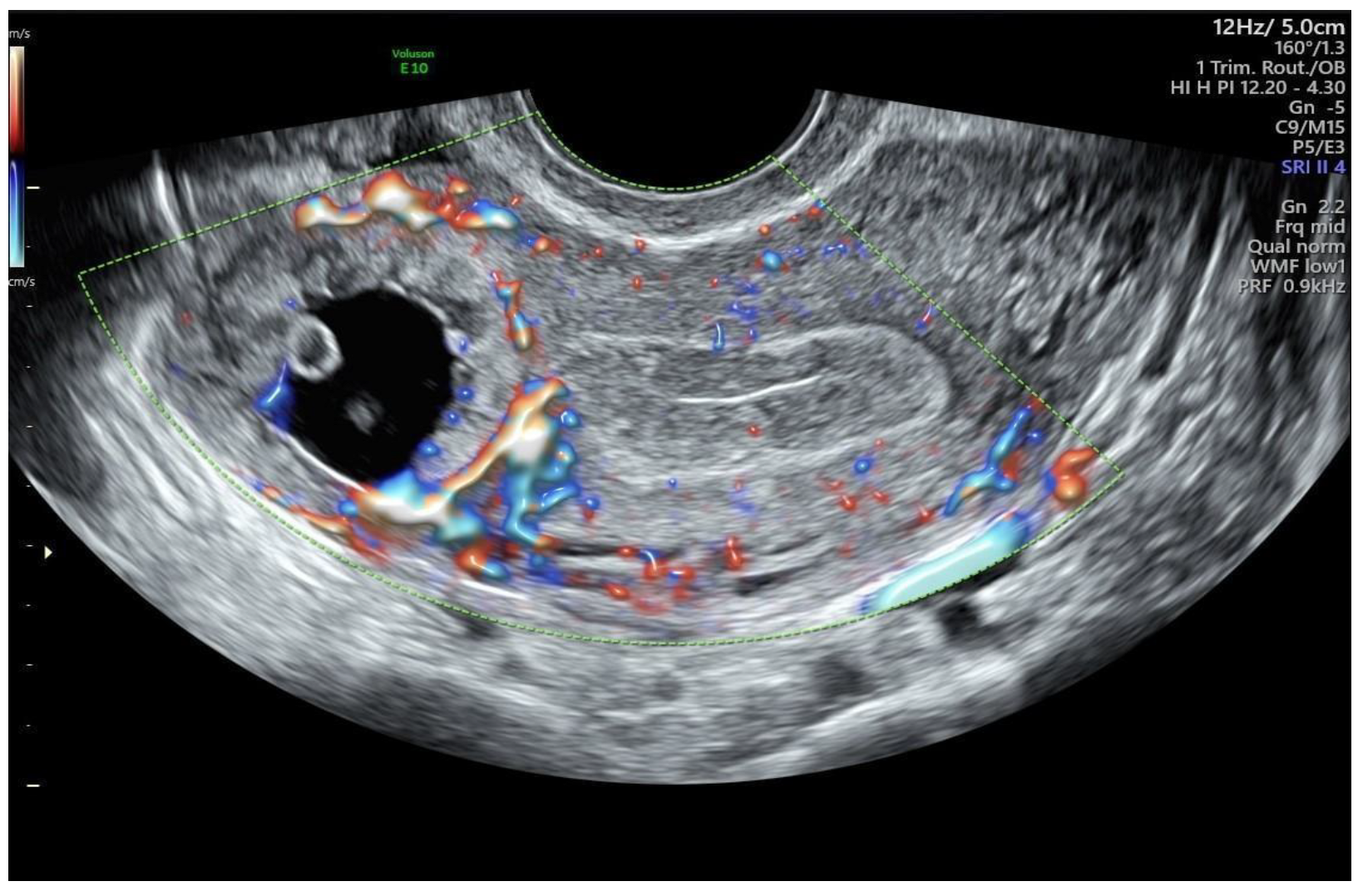
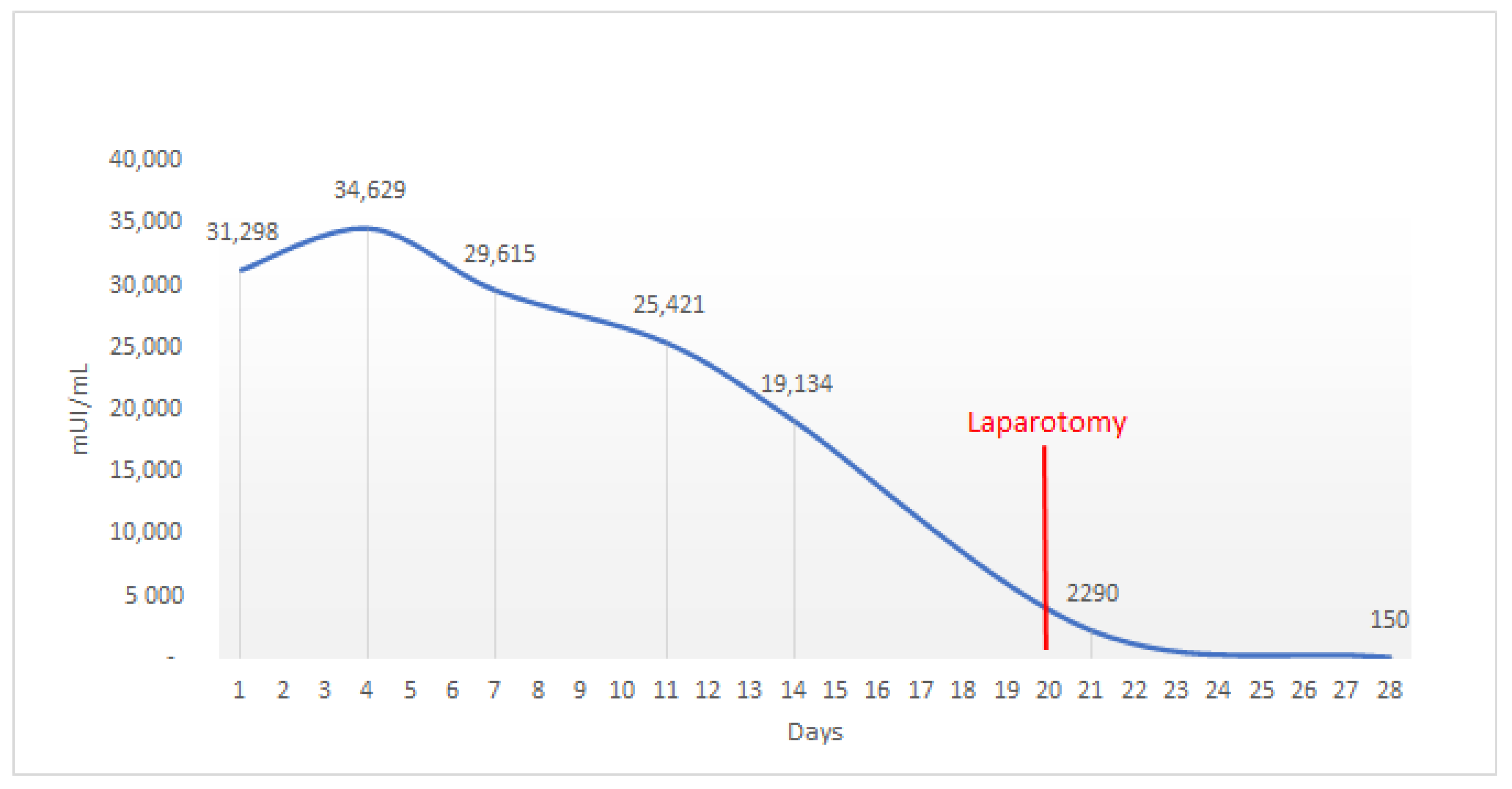
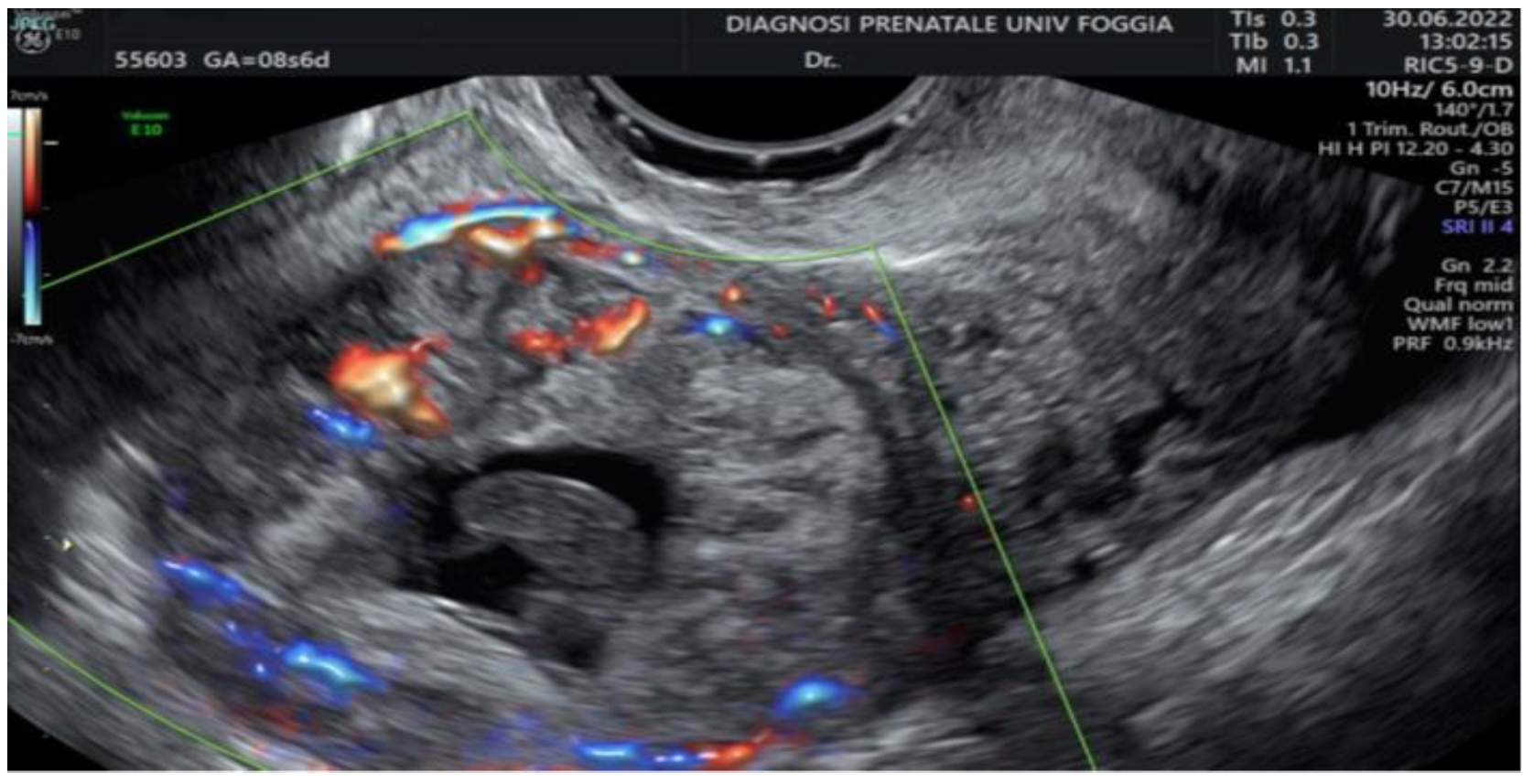
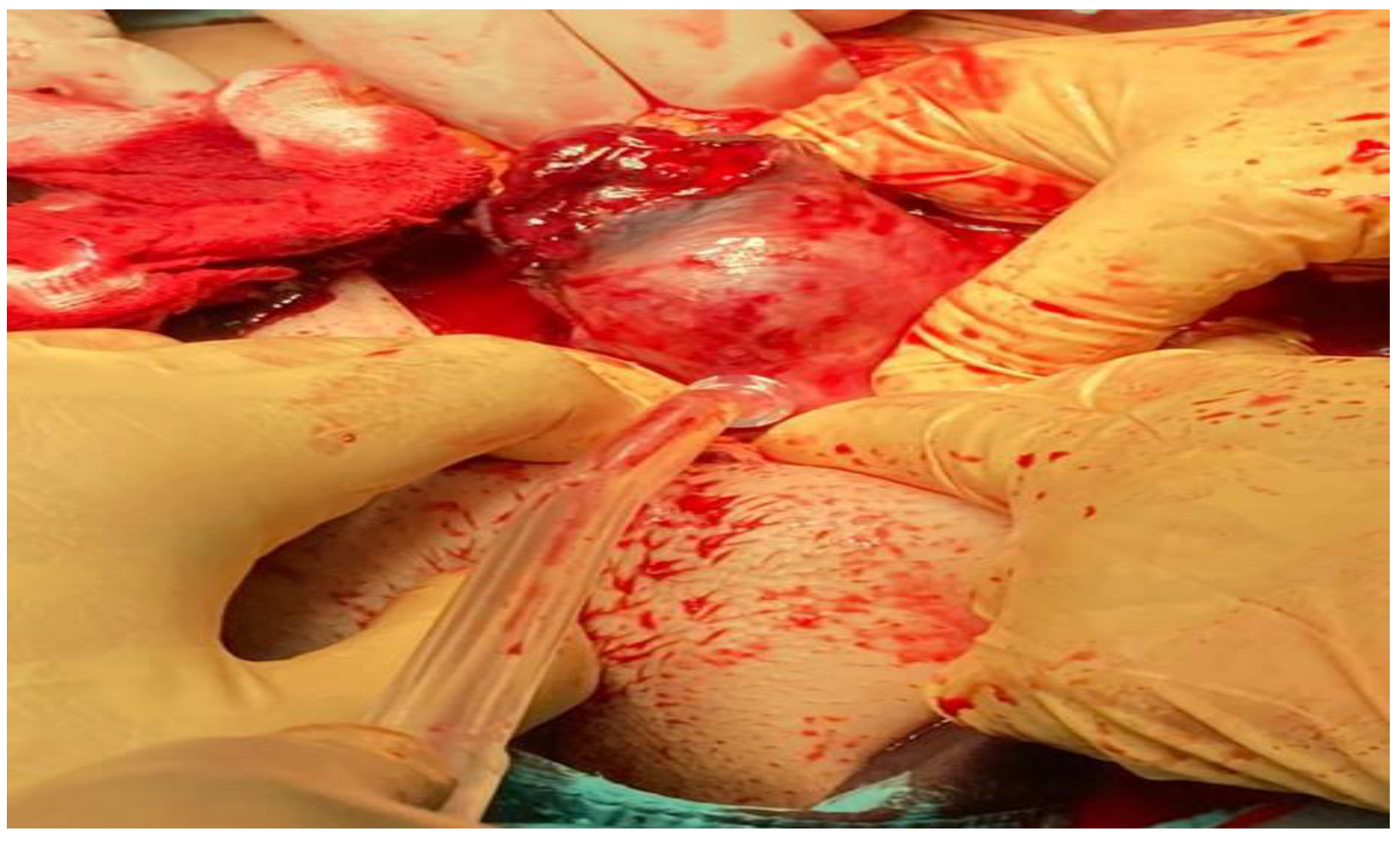
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sorrentino, F.; De Feo, V.; Stabile, G.; Tinelli, R.; D’Alterio, M.N.; Ricci, G.; Angioni, S.; Nappi, L. Cesarean Scar Pregnancy Treated by Artery Embolization Combined with Diode Laser: A Novel Approach for a Rare Disease. Medicina 2021, 57, 411. [Google Scholar] [CrossRef] [PubMed]
- Restaino, S.; De Gennaro, E.; Floris, S.; Stabile, G.; Zinicola, G.; Sorrentino, F.; Vizzielli, G.; Driul, L. Surgical Treatment Following Failed Medical Treatment of an Interstitial Pregnancy. Medicina 2022, 58, 937. [Google Scholar] [CrossRef] [PubMed]
- Dendas, W.; Schobbens, J.C.; Mestdagh, G.; Meylaerts, L.; Verswijvel, G.; Van Holsbeke, C. Management and outcome of heterotopic interstitial pregnancy: Case report and review of literature. Ultrasound 2017, 25, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Tulandi, T.; Al-Jaroudi, D. Interstitial pregnancy: Results generated from the Society of Reproductive Surgeons Registry. Obstet Gynecol. 2004, 103, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Stabile, G.; Romano, F.; Buonomo, F.; Zinicola, G.; Ricci, G. Conservative Treatment of Interstitial Ectopic Pregnancy with the Combination of Mifepristone and Methotrexate: Our Experience and Review of the Literature. BioMed Res. Int. 2020, 2020, 8703496. [Google Scholar] [CrossRef] [PubMed]
- McGrattan, M.; Chan, W.; Murji, A. A Purse-String Approach to Laparoscopic Cornuotomy for Interstitial Ectopic Pregnancy. J. Obstet. Gynaecol. Can. 2022, 44, 75–76.e2. [Google Scholar] [CrossRef]
- Tulandi, T.; Barbieri, R.L.; Falk, S.J. Ectopic Pregnancy: Clinical Manifestations and Diagnosis. UpToDate. 2022. Available online: https://www.uptodate.com/contents/ectopic-pregnancy-clinical-manifestations-and-diagnosis (accessed on 10 July 2022).
- Rizk, B.; Holliday, C.P.; Abuzeid, M. Challenges in the diagnosis and management of interstitial and cornual ectopic pregnancies. Middle East Fertil. Soc. J. 2013, 18, 235–240. [Google Scholar] [CrossRef]
- Wang, J.; Huang, D.; Lin, X.; Saravelos, S.H.; Chen, J.; Zhang, X.; Li, T.; Zhang, S. Incidence of Interstitial Pregnancy After In Vitro Fertilization/Embryo Transfer and the Outcome of a Consecutive Series of 38 Cases Managed by Laparoscopic Cornuostomy or Cornual Repair. J. Minim. Invasive Gynecol. 2016, 23, 739–747. [Google Scholar] [CrossRef]
- SIEOG. Linee Guida per Ecografia Ostetrica e Ginecologica; SIEOG: Roma, Italy, 2021. [Google Scholar]
- Jurkovic, D.; Mavrelos, D. Catch me if you scan: Ultrasound diagnosis of ectopic pregnancy. Ultrasound Obstet. Gynecol. 2007, 30, 1–7. [Google Scholar] [CrossRef]
- Stabile, G.; Romano, F.; Zinicola, G.; Topouzova, G.A.; Di Lorenzo, G.; Mangino, F.P.; Ricci, G. Interstitial Ectopic Pregnancy: The Role of Mifepristone in the Medical Treatment. Int. J. Environ. Res. Public Health 2021, 18, 9781. [Google Scholar] [CrossRef]
- Brincat, M.; Bryant-Smith, A.; Holland, T.K. The diagnosis and management of interstitial ectopic pregnancies: A review. Gynecol. Surg. 2019, 16, 2. [Google Scholar] [CrossRef]
- Stovall, T.G.; Ling, F.W. Single-dose methotrexate: An expanded clinical trial. Am. J. Obstet. Gynecol. 1993, 168, 1759–1762. [Google Scholar] [CrossRef]
- Moawad, N.S.; Mahajan, S.T.; Moniz, M.H.; Taylor, S.E.; Hurd, W.W. Current diagnosis and treatment of interstitial pregnancy. Am. J. Obstet. Gynecol. 2010, 202, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Hayashi, H.; Kutsuzawa, T.; Fujimoto, S.; Ichinoe, K. Treatment of interstitial ectopic pregnancy with methotrexate: Report of a successful case. Fertil Steril. 1982, 37, 851–852. [Google Scholar] [CrossRef]
- Bachman, E.A.; Barnhart, K. Medical management of ectopic pregnancy: A comparison of regimens. Clin. Obstet. Gynecol. 2012, 55, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Gómez García, M.T.; Aguarón Benitez, G.; Barberá Belda, B.; Callejón Rodríguez, C.; González Merlo, G. Medical therapy (methotrexate and mifepristone) alone or in combination with another type of therapy for the management of cervical or interstitial ectopic pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 165, 77–81. [Google Scholar] [CrossRef]
- Stabile, G.; Zinicola, G.; Romano, F.; Buonomo, F.; Mangino, F.P.; Ricci, G. Management of Non-Tubal Ectopic Pregnancies: A Single Center Experience. Diagnostics 2020, 10, 652. [Google Scholar] [CrossRef]
- Casadio, P.; Arena, A.; Verrelli, L.; Ambrosio, M.; Fabbri, M.; Giovannico, K.; Magnarelli, G.; Seracchioli, R. Methotrexate injection for interstitial pregnancy: Hysteroscopic conservative mini-invasive approach. Facts Views Vis. ObGyn 2021, 13, 73–76. [Google Scholar] [CrossRef]
- Ghazali, W.A.H.W.; Abidin, N.H.Z.; Muda, A.M.; Hamid, H.A. Comparative Study on Surgical Outcomes between Laparoscopic and Open Cornuotomy in Urban Tertiary Center of Malaysia. Gynecol. Minim. Invasive Ther. 2018, 7, 22–26. [Google Scholar]
- Lee, M.H.; Im, S.Y.; Kim, M.K.; Shin, S.Y.; Park, W.I. Comparison of Laparoscopic Cornual Resection and Cornuotomy for Interstitial Pregnancy. J. Minim. Invasive Gynecol. 2017, 24, 397–401. [Google Scholar] [CrossRef]
- Lau, S.; Tulandi, T. Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril. 1999, 72, 207–215. [Google Scholar] [CrossRef]
- Yassin, A.S.; Taha, M.S. Interstitial Ectopic Pregnancy, Diagnosis and Management: A Case Report and Literature Review. Ann. Clin. Case Rep. 2017, 2, 1352. [Google Scholar]
- Panelli, D.M.; Phillips, C.H.; Brady, P.C. Incidence, diagnosis and management of tubal and nontubal ectopic pregnancies: A review. Fertil. Res. Pract. 2015, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Surbone, A.; Cottier, O.; Vial, Y.; Francini, K.; Hohlfeld, P.; Achtari, C. Interstitial pregnancies’ diagnosis and management: An eleven cases series. Swiss Med. Wkly. 2013, 143, w13736. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sorrentino, F.; Vasciaveo, L.; De Feo, V.; Zanzarelli, E.; Grandone, E.; Stabile, G.; Nappi, L. Interstitial Pregnancy Treated with Mifepristone and Methotrexate with High Serum β-hCG Level in a Patient Wishing to Preserve Fertility: Time to Define Standardized Criteria for Medical/Surgical Therapy? Int. J. Environ. Res. Public Health 2022, 19, 11464. https://doi.org/10.3390/ijerph191811464
Sorrentino F, Vasciaveo L, De Feo V, Zanzarelli E, Grandone E, Stabile G, Nappi L. Interstitial Pregnancy Treated with Mifepristone and Methotrexate with High Serum β-hCG Level in a Patient Wishing to Preserve Fertility: Time to Define Standardized Criteria for Medical/Surgical Therapy? International Journal of Environmental Research and Public Health. 2022; 19(18):11464. https://doi.org/10.3390/ijerph191811464
Chicago/Turabian StyleSorrentino, Felice, Lorenzo Vasciaveo, Vincenzo De Feo, Erika Zanzarelli, Elvira Grandone, Guglielmo Stabile, and Luigi Nappi. 2022. "Interstitial Pregnancy Treated with Mifepristone and Methotrexate with High Serum β-hCG Level in a Patient Wishing to Preserve Fertility: Time to Define Standardized Criteria for Medical/Surgical Therapy?" International Journal of Environmental Research and Public Health 19, no. 18: 11464. https://doi.org/10.3390/ijerph191811464
APA StyleSorrentino, F., Vasciaveo, L., De Feo, V., Zanzarelli, E., Grandone, E., Stabile, G., & Nappi, L. (2022). Interstitial Pregnancy Treated with Mifepristone and Methotrexate with High Serum β-hCG Level in a Patient Wishing to Preserve Fertility: Time to Define Standardized Criteria for Medical/Surgical Therapy? International Journal of Environmental Research and Public Health, 19(18), 11464. https://doi.org/10.3390/ijerph191811464








