“We’re Lucky to Have Doctors at All”; A Qualitative Exploration of Australian Farmers’ Barriers and Facilitators to Health-Related Help-Seeking
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
- Over 18 years of age;
- Owned or worked on a farm to produce goods for sale at a commercial level;
- Lived or worked in any of the three target regions of South Australia;
- Did not report any cognitive impairment that might inhibit their ability to answer questions.
2.2. Recruitment
2.3. Analysis
2.4. Reflexivity
3. Results
3.1. Demographic Characteristics
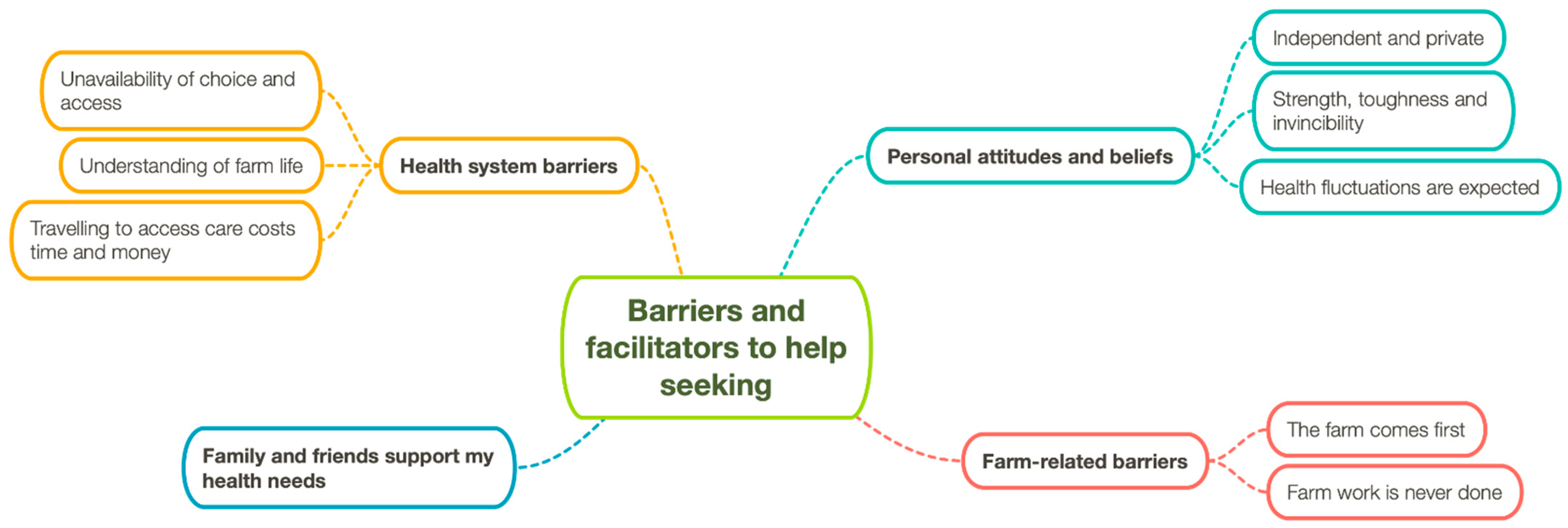
3.2. Thematic Analysis
3.2.1. Theme 1: Personal Attitudes and Beliefs
Subtheme 1: Independent and Private
“I’m just the sorta person that thinks that you’ve gotta, you gotta set to the task and fix the problem... generally the best person to do that’s yourself because mentally there’s a sort of defeat, fronting up to someone.”(Male, mid 40s #1, SE)
“I’m on medication [for depression] but you know it doesn’t worry me; I don’t advertise the fact that I try … and hide it, you know.”(Male, late 60s, EP)
“People say that they’ve gotta go to the chiropractor, but they won’t tell you they’ve gotta go to the counsellor.”(Male, mid 40s #2, SE)
“When I was acutely..., I was probably ashamed of my depression. I tried never to show my true, total emotion in front of my wife. I tried to do that in private.”(Male, mid 50s, MN)
Subtheme 2: Strength, Toughness and Invincibility
“You need a certain amount of resilience and hardiness.”(Male, mid 40s #2, SE)
“I think it’s built into their character, that farmers are pretty capable, tough, don’t need help, can be independent and can work everything out themselves, which is a big barrier to get over.”(Female, mid 60s, EP)
“I felt like it was a little bit of a cop-out that I went and saw him [the GP]. I knew what the problem was, I just had to fix it.”(Male, mid 40s #1, SE)
“We sorta tend to tough it out a bit longer.”(Male, mid 40s, MN)
“Well, I’m still active, I realise I’m not invincible, and I’m starting to look after myself a bit better I think.”(Male, mid 60s, EP)
“They just really think that they can keep fighting on and that nothing can really happen to them.”(Female, mid 30s, EP)
Subtheme 3: Health Fluctuations Are Expected
“Got a crook back that plays up all the time… But that’s just ongoing; it’s not debilitating, but if it goes out, it’s pretty ordinary for a few days, and you get it right.”(Male, early 60s, EP)
“I dislocated a couple of fingers there yesterday, and I don’t view them as injuries. They’re just part of it, it’s just what happens.”(Male, mid 40s #1, SE)
“It’s just one of those things; you live in a constant area of pain.”(Male, late 50s, SE)
“Well, why wouldn’t ya? Nothing to do by sitting around doing nothing. Might as well keep going, yeah.”(Male, late 50s, SE)
“I don’t go unless I’ve got something wrong.”(Male, late 60s, EP)
“I thought it was very suspicious. I got very sweaty and things started to go a bit pear-shaped.”(Male, late 60s, EP)
“You’re getting around that network, and yeah, I won’t sweep it under the carpet I’ll talk about it.”(Male, mid 40s #1, SE)
“I’m going to react when I have a bad flu. I’m going to lay on the couch and try and convince everybody that I’m very close to death and I’m happy to tell anyone that walks past that I’m only a few breaths away.”(Male, mid 40s #1, SE- in jest)
“Unless you’re feeling really, really crook, but even that you always find something to do … don’t go sitting in the house all day long, no.”(Male, mid 50s, SE)
“You know if you’re feeling flat you might do any easier job, but there’s no days off, ‘cos you live and work at home.”(Male, mid 40s #3, SE)
3.2.2. Theme 2: Farm-Related Barriers
Subtheme 1: The Farm Comes First
“I s’pose the other thing we get in a small community is there’s a lot of pressure to I s’pose provide for your community… There’s just a lota community work to do in a small community and I s’pose that’s something at times just increases your workload but someone’s gotta do it.”(Male, mid 40s, MN)
“Our crop must go in on time; everything’s gotta be right because you know two bad years in a row and you can go from being financially okay to being in deep, deep trouble.”(Male, mid 60s, EP)
So, health wise how many farmers will ignore health-warning signals because of other pressures, especially financial pressures? I’d say a huge amount, and I have also been guilty of the same sin.”(Male, mid 50s, MN)
“But to get that organised, to leave a farm and get everything set-up so that everything keeps going while you’re away? I’ve never achieved it. That’s the sort of thing I think we do miss out on because there’s too much ongoing stuff on farms.”(Female, mid 60s, EP)
“I believe most farmers are under manned to what they should be. I think we’re all short staffed and people are always in a hurry and that’s what makes people get tired, overtired and still work and that’s where the danger comes in.”(Male, mid 50s, EP)
“So it might mean that morning I don’t do Pilates but I’ve got it in the back of my mind that I can stop at any time during the day and do it. It doesn’t have to be done in the house, it doesn’t have to be done in the morning.”(Male, mid-60s MN)
Subtheme 2: Farm Work Is Never Done
“Unfortunately, in our game you just get stuck there, and you just do seven days a week and one week goes into another.”(Male, mid 40s #1, SE)
“If there’s work to be done, you tend to … I’ve never come to this situation where we’ve had something important on and I haven’t been able to do it.”(Male, early 60s, EP)
“If we’re busy we just don’t have a choice, you’ve just got to be busy.”(Male, early 40s, MN)
3.2.3. Theme 3: Health System Barriers
Subtheme 2: Understanding of Farm Life
“You know, I’m sure that people, health professionals in the city, think we are mad. They really do.”(Male, mid 40s #1, SE)
“Overseas-trained doctors, well, I was going to say, doctors, medical people. Because sometimes they are difficult to understand and maybe they find me difficult to understand, so communication can be a problem.”(Male, mid 60s, MN)
Subtheme 3: Travelling to Access Care Costs Time and Money
“Then it might also depend on whether I can access somebody to do that work instead of myself.”(Male, mid 60s, MN)
“I’m not going to drive to [regional centre] for one appointment. I like to be a bit more efficient than that. So, there’s probably more efficiency in heading to [major city], but I’ll still want to work it in with a few other jobs.”(Male, mid 40s #2, SE)
“I think most of the services are down here; it’s just the waiting, the cost and the travel.”(Male, mid 40s, SE)
“All the costs, too. Like, having to come over because we haven’t got the facilities over home. So, that’s where the cost factor comes in too. You know, we’re lucky we’ve got somewhere to stay here in Adelaide, but if you haven’t … If you had to pay for accommodation plus treatments and all of that, it soon adds up.”(Female, mid 40s, EP)
3.2.4. Theme 4: Family and Friends Support My Health Needs
“While I’m a firm believer in medical intervention for people that are suffering I also believe that the problems that you resolve yourself are better resolved than the ones that are covered up by medication.”(Male, mid 40s #1, SE)
“Their wife will most likely make the appointment and say I’ve made you a doctor’s appointment for 2 o’clock on Thursday and he says yeah fine. May go, may not go.”(Male, mid 40s #1, SE)
“Well, it’s about them trying to get help for a start or get their partner getting them help.”(Male, early 60s, EP)
“Yeah I’ve got a couple of mates that I’ll ring up. It’s not really to talk about the problems but just to say ‘g’day, see how you’re going.”(Male, mid 60s, MN)
“The men walking around on the golf course, and you know they might have just talked about... You know they could joke about it, moan and groan with each other and I just think a lot of communication and that’s good when everyone’s sort of in that same situation.”(Female, mid 30s, EP)
“I guess if you’re down for any length of time, ‘cos you’d know your wife’d tell you.”(Male, mid 40s #2, SE)
“If you can have open communication with a partner and support each other and recognise and have the awareness to recognise that then you can do something about it; nip it in the bud.”(Male, mid 40s #1, SE)
“There are times when you know very well that they should be at the doctor and they wait until it’s a lot worse before they go and that has consequences.”(Female, mid 60s, EP)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McCurdy, S.A.; Carroll, D.J. Agricultural injury. Am. J. Ind. Med. 2000, 38, 463–480. [Google Scholar] [CrossRef]
- Safe Work Australia. Work Health and Safety in the Agricultural Industry; Safe Work: Canberra, Australia, 2016.
- Sprince, N.; Park, H.; Zwerling, C.; Whitten, P.; Lynch, C.; Burmeister, L.; Thu, K.; Gillette, P.; Alavanja, M. Risk factors for low back injury among farmers in Iowa: A case-control study nested in the agricultural health study. J. Occup. Environ. Hyg. 2007, 4, 10–16. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Labor Safety and Health. Topics- Agricultural Operations. Available online: https://www.osha.gov/dsg/topics/agriculturaloperations/ (accessed on 4 October 2014).
- Fennell, K.M.; Jarrett, C.E.; Kettler, L.J.; Dollman, J.; Turnbull, D.A. “Watching the bank balance build up then blow away and the rain clouds do the same”: A thematic analysis of South Australian farmers’ sources of stress during drought. J. Rural. Stud. 2016, 46, 102–110. [Google Scholar] [CrossRef]
- Kennedy, A.J.; Maple, M.J.; McKay, K.; Brumby, S.A. Suicide and accidental death in Australia’s rural farming communities: A review of the literature. Rural. Remote Health 2014, 14, 2517. [Google Scholar] [CrossRef] [PubMed]
- Page, A.; Fragar, L. Suicide in Australian farming, 1988–1997. Aust. N. Z. J. Psychiatry 2002, 36, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Safe Work Australia Work-Related Injuries and Fatalities on Australian Farms; Safe Work: Canberra, Australia, 2013.
- Brumby, S.; Chandrasekara, A.; McCoombe, S.; Kremer, P.; Lewandowski, P. Farming fit? Dispelling the Australian Agrarian myth. BMC Res. Notes 2011, 4, 89. [Google Scholar] [CrossRef]
- Brumby, S.; Chandrasekara, A.; Kremer, P.; Torres, S.; McCoombe, S.; Lewandowski, P. The effect of physical activity on psychological distress, cortisol and obesity: Results of the farming fit intervention program. BMC Public Health 2013, 13, 1018. [Google Scholar] [CrossRef]
- Fragar, L.; Depczynski, J.; Lower, T. Mortality patterns of Australian male farmers and farm managers. Aust. J. Rural. Health 2011, 19, 179–184. [Google Scholar] [CrossRef]
- Fragar, L.; Eather, J.; Depczynski, J.; Lower, T. Alcohol and Farm Workplace Project; Australian Centre for Agricultural Health and Safety: Moree, Australia, 2010.
- Willder, S.; Brumby, S. Health Status and Behaviours of Australian Farming Men. New Male Stud. Int. J. 2012, 1, 34–48. [Google Scholar]
- Brew, B.; Inder, K.; Allen, J.; Thomas, M.; Kelly, B. The health and wellbeing of Australian farmers: A longitudinal cohort study. BMC Public Health 2016, 16, 988. [Google Scholar] [CrossRef]
- Hull, M.J.; Fennell, K.M.; Vallury, K.; Jones, M.; Dollman, J. A comparison of barriers to mental health support-seeking among farming and non-farming adults in rural South Australia. Aust. J. Rural Health 2017, 25, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Fennell, K.M.; Martin, K.; Wilson, C.J.; Trenerry, C.; Sharplin, G.; Dollman, J. Barriers to seeking help for skin cancer detection in rural Australia. J. Clin. Med. 2017, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare Rural, Regional and Remote Health: Indicators of Health Status and Determinants of Health; AIHW: Canberra, Australia, 2008.
- Australian Institute of Health and Welfare Australia’s Health 2016; AIHW: Canberra, Australia, 2016.
- Rawolle, T.A.; Sadauskas, D.; van Kessel, G.; Dollman, J. Farmers’ perceptions of health in the Riverland region of South Australia: ‘If it’s broke, fix it’. Aust. J. Rural. Health 2016, 24, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Brumby, S.; Chandrasekara, A.; McCoombe, S.; Kremer, P.; Lewandowski, P. Cardiovascular risk factors and psychological distress in Australian farming communities. Aust. J. Rural. Health 2012, 20, 131–137. [Google Scholar] [CrossRef]
- Bryant, L.; Garnham, B. The fallen hero: Masculinity, shame and farmer suicide in Australia. Gend. Place Cult. 2015, 22, 67–82. [Google Scholar] [CrossRef]
- Lovelock, K. The injured and diseased farmer: Occupational health, embodiment and technologies of harm and care. Sociol. Health Illn. 2012, 34, 576–590. [Google Scholar] [CrossRef]
- Seiz, R.C.; Downey, E.P. What farm families tell us that can be useful in educating for health and safety. J. Ext. 2001, 39, 6FEEA5. [Google Scholar]
- Staniford, A.K.; Dollard, M.F.; Guerin, B. Stress and help-seeking for drought-stricken citrus growers in the Riverland of South Australia. Aust. J. Rural. Health 2009, 17, 147–154. [Google Scholar] [CrossRef]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. “Don’t break down on Tuesday because the mental health services are only in town on Thursday”: A qualitative study of service provision related barriers to, and facilitators of farmers’ mental health help-seeking. Adm. Policy Ment. Health Ment. Health Serv. Res. 2020, 48, 514–527. [Google Scholar] [CrossRef]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. ‘Farming is not just an occupation [but] a whole lifestyle’: A qualitative examination of lifestyle and cultural factors affecting mental health help-seeking in Australian Farmers. Sociol. Rural. 2020, 60, 151–173. [Google Scholar] [CrossRef]
- Sandelowski, M. Focus on research methods-whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 2011 Census QuickStats: Mid North. Available online: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/40503?opendocument&navpos=220 (accessed on 20 July 2019).
- Australian Bureau of Statistics. 2011 Census QuickStats: Eyre Peninsula. Available online: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/406011130?opendocument&navpos=220 (accessed on 20 July 2019).
- Australian Bureau of Statistics. 2011 Census QuickStats: South East. Available online: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/407?opendocument&navpos=220 (accessed on 20 July 2019).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Grbich, C. Qualitative Data Analysis: An Introduction; Sage: London, UK, 2012; ISBN 1-4462-0296-8. [Google Scholar]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE Publications: London, UK, 2013. [Google Scholar]
- Attride-Stirling, J. Thematic networks: An analytic tool for qualitative research. Qual. Res. 2001, 1, 385–405. [Google Scholar] [CrossRef]
- Cornally, N.; McCarthy, G. Help-seeking behaviour: A concept analysis. Int. J. Nurs. Pract. 2011, 17, 280–288. [Google Scholar] [CrossRef]
- Ajzen, I. From intentions to actions: A theory of planned behavior. In Action Control; Springer: New York, NY, USA, 1985; pp. 11–39. [Google Scholar]
- Barney, L.J.; Griffiths, K.; Jorm, A.; Christensen, H. Stigma about depression and its impact on help-seeking intentions. Aust. N. Z. J. Psychiatry 2006, 40, 51–54. [Google Scholar] [CrossRef]
- Kutek, S.M.; Turnbull, D.; Fairweather-Schmidt, A.K. Rural men’s subjective well-being and the role of social support and sense of community: Evidence for the potential benefit of enhancing informal networks. Aust. J. Rural. Health 2011, 19, 20–26. [Google Scholar] [CrossRef]
- Stain, H.J.; Kelly, B.; Lewin, T.J.; Higginbotham, N.; Beard, J.R.; Hourihan, F. Social networks and mental health among a farming population. Soc. Psychiatry Psychiatr. Epidemiol. 2008, 43, 843–849. [Google Scholar] [CrossRef]
- Baker, T.; McCoombe, S.; Mercer-Grant, C.; Brumby, S. Chest pain in rural communities; Balancing decisions and distance. Emerg. Med. Australas. 2011, 23, 337–345. [Google Scholar] [CrossRef]
- Fennell, K.; Hull, M.; Jones, M.; Dollman, J. A comparison of barriers to accessing services for mental and physical health conditions in a sample of rural Australian adults. Rural. Remote Health 2018, 18, 4155. [Google Scholar] [CrossRef] [PubMed]
- McColl, L. The influence of bush identity on attitudes to mental health in a Queensland community. Rural. Soc. 2007, 17, 107–124. [Google Scholar] [CrossRef] [Green Version]
- Wrigley, S.; Jackson, H.; Judd, F.; Komiti, A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust. N. Z. J. Psychiatry 2005, 39, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Fraser, C.; Jackson, H.; Judd, F.; Komiti, A.; Robins, G.; Murray, G.; Humphreys, J.; Pattison, P.; Hodgins, G. Changing places: The impact of rural restructuring on mental health in Australia. Health Place 2005, 11, 157–171. [Google Scholar] [CrossRef]
- Judd, F.; Jackson, H.; Komiti, A.; Murray, G.; Fraser, C.; Grieve, A.; Gomez, R. Help-seeking by rural residents for mental health problems: The importance of Agrarian values. Aust. N. Z. J. Psychiatry 2006, 40, 769–776. [Google Scholar] [CrossRef]
- Judd, F.; Komiti, A.; Jackson, H. How does being female assist help-seeking for mental health problems? Aust. N. Z. J. Psychiatry 2008, 42, 24–29. [Google Scholar] [CrossRef]
- Kaukiainen, A.; Kõlves, K. Too tough to ask for help? Stoicism and attitudes to mental health professionals in rural Australia. Rural. Remote Health 2020, 20, 5399. [Google Scholar] [CrossRef]
- Alston, M.; Kent, J. Social Impacts of Drought; Charles Sturt University: Wagga Wagga, Australia, 2004. [Google Scholar]
- Nelson, S. Finding tomorrow’s agricultural workforce. Aust. Farm Bus. Manag. J. 2011, 8, 47–60. [Google Scholar]
- Australian Bureau of Statistics. Australian Social Trends: Australian Farming and Farmers, Catalogue No. 4102.0; Australian Bureau of Statistics: Canberra, Australia, 2012.
- Meadows, G.; Enticott, J.; Inder, B.; Russell, G.; Gurr, R. Better access to mental health care and the failure of the medicare principle of universality. Med. J. Aust. 2015, 202, 190–194. [Google Scholar] [CrossRef]
- Murray, G.; Judd, F.; Jackson, H.; Fraser, C.; Komiti, A.; Hodgins, G.; Pattison, P.; Humphreys, J.; Robins, G. Rurality and mental health: The role of accessibility. Aust. N. Z. J. Psychiatry 2004, 38, 629–634. [Google Scholar] [CrossRef]
- Rankin, S.L.; Hughes-Anderson, W.; House, A.K.; Heath, D.I.; Aitken, R.J.; House, J. Costs of accessing surgical specialists by rural and remote residents. ANZ J. Surg. 2001, 71, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, H.; Travers, C.; Cartwright, C.; Smith, N. Mental health literacy in rural Queensland: Results of a community survey. Aust. N. Z. J. Psychiatry 2006, 40, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Labor Force and Other Characteristics of Farmers; 1301.0—Year Book Australia, 2012; Australian Bureau of Statistics: Canberra, Australia, 2012.
- Patel, M.X.; Doku, V.; Tennakoon, L. Challenges in recruitment of research participants. Adv. Psychiatr. Treat. 2003, 9, 229–238. [Google Scholar] [CrossRef] [Green Version]
| Participant Characteristics | Frequency (n) |
|---|---|
| Total | 15 |
| Men | 12 |
| Age (years) | |
| Mean (±SD) | 51.7 (±12.6) |
| Region | |
| Mid North | 4 |
| South East | 4 |
| Eyre Peninsula | 7 |
| Farming experience (years) | |
| 0–19 | 2 |
| 20–39 | 10 |
| 40+ | 3 |
| Type of farm | |
| Cropping | 6 |
| Sheep, cropping | 6 |
| Sheep, beef | 1 |
| Beef cattle | 1 |
| Dairy | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hull, M.J.; Gunn, K.M.; Smith, A.E.; Jones, M.; Dollman, J. “We’re Lucky to Have Doctors at All”; A Qualitative Exploration of Australian Farmers’ Barriers and Facilitators to Health-Related Help-Seeking. Int. J. Environ. Res. Public Health 2022, 19, 11075. https://doi.org/10.3390/ijerph191711075
Hull MJ, Gunn KM, Smith AE, Jones M, Dollman J. “We’re Lucky to Have Doctors at All”; A Qualitative Exploration of Australian Farmers’ Barriers and Facilitators to Health-Related Help-Seeking. International Journal of Environmental Research and Public Health. 2022; 19(17):11075. https://doi.org/10.3390/ijerph191711075
Chicago/Turabian StyleHull, Melissa J., Kate M. Gunn, Ashleigh E. Smith, Martin Jones, and James Dollman. 2022. "“We’re Lucky to Have Doctors at All”; A Qualitative Exploration of Australian Farmers’ Barriers and Facilitators to Health-Related Help-Seeking" International Journal of Environmental Research and Public Health 19, no. 17: 11075. https://doi.org/10.3390/ijerph191711075
APA StyleHull, M. J., Gunn, K. M., Smith, A. E., Jones, M., & Dollman, J. (2022). “We’re Lucky to Have Doctors at All”; A Qualitative Exploration of Australian Farmers’ Barriers and Facilitators to Health-Related Help-Seeking. International Journal of Environmental Research and Public Health, 19(17), 11075. https://doi.org/10.3390/ijerph191711075







