Abstract
Background: There is a risk of pelvic floor dysfunction (PFD) from baby delivery. Many clinical guidelines recommend pelvic floor muscle training (PFMT) as the conservative treatment for PFD because pelvic floor muscles (PFMs) play a crucial role in development of PFD. However, there is disagreement about the method and intensity of PFM training and the relevant measurements. To pilot the study in PFM training, we designed a Pelvic Floor Workout (PEFLOW) for women to train their pelvic through entire body exercises, and we planned a trial to evaluate its effectiveness through comparing the outcomes from a group of postpartum women who perform PELFLOW at home under professional guidance online with the control group. Methods/design: The randomized controlled trial was projected to be conducted from November 2021 to March 2023. A total of 260 postpartum women would be recruited from the obstetrics departments of the study hospital and women would be eligible for participation randomized into experimental or control groups (EG/CG) if their PFM strength are scaled by less than Modified Oxford grading Scale (MOS) to be less than grade 3. Women in EG would perform a 12-week PEFLOW online under the supervision and guidance of a physiotherapist, while women in CG would have no interventions. Assessments would be conducted at enrollment, post intervention (for EG) or 18th to 24th week postpartum (for CG), and 1 year postpartum. Assessment would be performed in terms of pelvic floor symptoms, including MOS, cough stress test, urinary leakage symptoms, pelvic organ prolapse quantitation (POP-Q), and vaginal relaxation, clinic examinations including Pelvic floor electrophysiological test, Pelvic floor ultrasound and Spine X-ray, overall body test including trunk endurance test, handgrip test, body composition test, and questionnaires including International Physical Activity Questionnaire Score-Short Form(IPAQ-SF), Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20), Pelvic Floor Impact Questionnaire-7 (PFIQ-7), the 6-item Female Sexual Function Index (FSFI-6), and the Pittsburgh Sleep Quality Index (PSQI). Primary analysis will be performed to test our main hypothesis that PEFLOW is effective with respect to strengthen PFM strength. Discussion: This trial will demonstrate that pelvic floor-care is accessible to most women and clinical practice on PFD may change relevantly should this study find that Online PEFLOW approach is effective to improve PFMs. Trial registration: ClinicalTrials.gov, NCT05218239.
1. Introduction/Background
Pelvic floor dysfunction (PFD) is a series of symptoms of dysfunction caused by injuries on pelvic floor muscle, nerve, ligament, and fascia injury. PFD has a serious negative impact on the common life of woman, who would experience different degrees of urinary incontinence, pelvic organ prolapse, chronic pelvic pain, sexual dysfunction, etc. Although not clinically emergent, PFD brings a heavy economic burden to the women who suffers from this problem. The latest updated data show that the prevalence of urinary incontinence in Chinese women reaches 30.9%, the incidence of symptomatic pelvic organ prolapse is up to 9.6% [1], and the prevalence of sexual dysfunction is about 29.7% [2]. Pelvic floor diseases are more prevalent among women who have multiple births.
Pregnancy and vaginal delivery have independently been proved to be the risk factors for the development of severe urinary incontinent (SUI) as they could obviously weaken the pelvic floor muscle (PFM) strength. However, it was hard to evaluate patients’ muscle strength objectively; therefore, it was hard to validate whether a measure could be effective to have the weakened pelvic floor muscles be recovered before Modified Oxford scale (MOS) for muscle strength was published [3]. MOS provides quantitative scales for muscle strength, and it is simple and easy to apply clinically. It is becoming widely accepted method for pelvic floor muscle strength assessment since it was published. Literately and clinically, MOS 4 and 5 is identified as having “good” or “strong” muscle contraction which represents a normal condition of the pelvic floor muscles; relevantly MOS ≤3 indicates a weak contraction or no contraction being felt [4]. Some studies suggested that pelvic floor muscle strength be correlated with the incidence of pelvic organ prolapse (POP). Thus, Pelvic Organ Prolapse Quantification (POP-Q) was developed for evaluation of the pelvic floor muscle [5]. Borello-France et al. [6] used POP-Q to evaluated women’s pelvic floor muscle in their studies and argued that women with stage II of prolapse were better than those with stage III or IV in elevating their pelvic floor, and also would be easier to get benefit from PFM training than those over stage III. Scientific evidence showed that 10–20% of patients who were not intervened for the clinically confirmed POP got progressed in term of POP-Q scoring in 2-year follow-up [7,8], so early prevention or treatment should have high priority. The incidence rate of POP is higher in middle aged and elderly women. PFM training is recommended to women postpartum for it reduces the incidence of PFD during 6–12 months postpartum [9] and should possibly reducing the incidence of diseases from muscle dysfunction related to the anatomical changes with aging [10]. A program of supervised PFM training was recommended as a first option for women with symptomatic POP-Q stage I or stage II [11]. MOS and POP-Q can be the objective indicators be used to validate the effectiveness of any measure in improving PFM.
PFM training is the most popular conservative intervention for PFD. Its role in PFM improvement is becoming more and more important along with the rapid development of rehabilitation medicine and it is more and more acceptable by women as their requirements for improvement of quality of life are getting stronger. There are many kinds of programs for post-delivery exercises that are commercially available for women. Formulating a rehabilitation program after childbirth is certainly an effective strategy for most women to benefit from the post-delivery recovery. However, PFM rehabilitation relied on the synchronous recovery of both type I and type II muscle fibers, and, as it is difficult to identify type I and type II of the muscle fibers accurately by nonprofessionals during pelvic floor muscle contraction, exercises are usually not properly programmed, and the effectiveness of such programs are not easy to gain. Formulating a science-based rehabilitation program that can trained type I and type II muscle fibers for their synchronous rehabilitation after childbirth is certainly an effective strategy for most women to benefit from the post-delivery recovery.
Many pelvic floor rehabilitation methods were explored in previous studies. In 1948, Kegel training was first proposed and adopted as the gold standard of pelvic floor muscle training (PFMT) [12]. PFMT refers to the conscious exercise via autonomic contraction of the pelvic floor muscles that are dominated by pubococcinate muscles. The American Urogynecologic Society evaluated PFMT as the wisest exercise choice for women and recommended it as the first-line treatment for PFD [13]. Kegel exercise has rarely been used alone until now. The human body is an organic whole, so PFMT should not be limited to the local pelvic floor. In 1980, abdominal hypopressive technique (AHT) [14] was invented. It emphasizes PFMT to be combined with activation of transverse abdominis muscle and diaphragmatic breathing [14]. Some studies found that training of the core muscles, including rectus abdominis, transversus abdominis, internal or external oblique, lumbar multifidus, and erector spinae muscles [15] for their stability, such as Yoga exercises, can strengthen PFM [16,17]. A French therapist, Philippe, proposed a concept of Global Postural Re-education (GPR) [18,19] and demonstrated that GPR was advantageous in improving respiratory muscle strength and reducing urinary incontinence since GPR was projected to correct postural misalignments by stretching the muscle chains [19]. In consideration that the spine is a continuous boney structure that is closely associated with pelvic dynamics [20], some investigators in recent years focused their research on restoring the balance of anatomic mechanical systems through adjustment of the posture. It was found that therapeutic exercise on posture adjustment (diaphragm and lumbar position) for patients with poor respiration and posture can improve the neuromuscular control on muscles of deep abdomen, diaphragm, and pelvic floor, and promote the stability of lumbar and pelvic floor. In addition, a significant correlation between overall posture and PFD was also demonstrated in several studies [20,21].
In 2020, the Canadian Society of Obstetricians and Gynecologists (SOGC) recommended that, to gain effectiveness, PFMT should be performed under supervision for at least 3 months [22]. Some previous studies [23,24,25,26] in alleviation of symptomatic ureter leakage demonstrated that physical exercise with PFMT was effective on the pelvic floor muscle.
In referring to the above published studies and concepts and based on the previous study [27] of our team, our team from Peking University Peoples Hospital (PKUPH) developed a Pelvic Floor Workout (also named as PKUPH-PEFLOW), which focuses on training to improve the strength, endurance, flexibility, stability, and flexibility of core muscles, including diaphragmatic, abdominal, pelvic floor, and lower back muscles. We also designed a randomized controlled clinical trial to demonstrate the effectiveness of PEFLOW. The trial was designed on hypothesis that (1) a 12-week Global Pelvic Floor Workout would improve the pelvic floor muscle strength of postpartum women; (2) the 12-week Global Pelvic Floor Workout would positively impact on the overall function of postpartum women, including pelvic floor function, body posture, pain, etc.; and (3) body posture, physical activity level, trunk muscle endurance and strength would have beneficial effects on maternal overall function.
2. Methods
2.1. Study Design
This is a randomized controlled trial to be conducted from November 2021 to March 2023. Participants are recruited from the obstetrics departments of Peking University People’s Hospital. The study was approved by Peking University Institutional Review Board (number: 2021PHB254-001) and registered in Clinical.Trials.gov (number: NCT05218239).
2.2. Inclusion Criteria
Postpartum women will be eligible for enrollment if they are: (1) in 6th to 12th week postpartum; (2) without history of clinically confirmed systematic diseases, such as neurological conditions and cardiac insufficiency, currently not wearing cardiac pacemaker or receiving hormone therapy, and/or not been treated with radical surgery for pelvis and sling or surgery for prolapse before pregnancy, and with no pregnant complications; (3) willing to participate signing informed consent form; and (4) able to read without cognitive problem from poor education or diagnosed mental problem.
2.3. Exclusion Criteria
Participants will be excluded if they are: (1) confirmed by postpartum pelvic examination to be >grade 3 of pelvic floor muscle strength by Modified Oxford Scale (MOS); (2) ≥stage III for Pelvic Organ Prolapse Quantification (POP-Q); (3) symptomatically confirmed to have severe urinary incontinence (Women with more than one incontinent episode per day AND an important volume of urine loss [28] or urine leakage occurred in a quiet state were classified as having severe urinary incontinence); or (4) any limb dysfunction that unenabled women to take this training. A participant will be recorded as“ drop off from trial” if she becomes pregnant during the follow-ups.
2.4. Site Investigators and Roles
To conduct and evaluate the project, the study should assign the following persons to play roles: (1) a gynecologist (can be the chief investigator) who would conduct baseline examination and evaluation for eligible women, and another two gynecologists who would conduct examinations at the second and third follow-up visits, respectively, who was unaware of the data from the last follow-up. The examinations would include MOS, POP-Q, cough stress test, and vaginal relaxation.
(2) A research coordinator who is responsible for informed consent, study record and data management, contacting with and be accompanied with the participants during the examinations.
(3) A physiotherapist who would apply the designed intervention to participant in experimental group (EG).
(4) A physiotherapist assistant who would be responsible for correcting actions of EG during training and record Borg’s Rating of Perceived Exertion 6-20 (RPE) Scale after each session of training. (5) Clinic examiners who would be responsible for pelvic floor surface electromyography (sEMG), pelvic floor ultrasound examination, and Spine X-ray.
2.5. Randomization and Allocation Concealment
Eligible women would be randomized into two groups, the experimental group (EG) and the control group (CG), at a ratio of 1:1. A randomization list would be created by a statistician from Peking University for each center before the start of the research. Randomization would be performed using SAS 9.4 (SAS Institute, Cary, NC, USA). The randomization lists would be concealed until a woman is confirmed eligible for participation. Then, the research coordinator in the site would assign the eligible participant to EG or CG. With such a randomization, the numbers of participants in EG and CG are expected to be statistically balanced. Participants and the physiotherapists engaging in the intervention are not blind to the randomized assignment because it is not feasible to do. However, to minimize the risk of assessor’s unblinding, participants are blind to other’s assignments and encouraged not to discuss their treatment with the independent assessor in the informed consent procedures and at the time of each assessment.
2.6. Assessment Schedule
Each participant would experience three assessments to go through the whole procedures in this study. The first assessment is for enrollment and would be given when women is confirmed eligible for participation. The second assessment would be conducted after 18th week postpartum but not later than 24th week. The final assessment would be performed in one year after delivery (Figure 1).
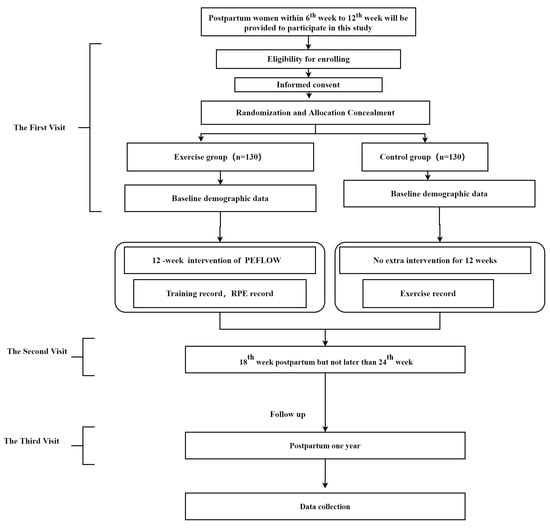
Figure 1.
Flowchart of the trial.
2.7. Interventions
All participants in EG and CG would be undergo postpartum pelvic floor evaluation according to standard comical procedures, which includes instructions for PFM strengthening with Kegel [12] and Knack [29] methods to improve voluntary contraction of the pelvic floor muscles, as well as daily living habits and posture education, such as reducing stool time, avoiding heavy lifting, etc. No extra intervention would be given to the participants in CG.
In addition to the clinical standard pelvic floor evaluation, participants in EG would be provided with a Pelvic Floor Workout (PEFLOW). PEFLOW is a general program for physical training of the pelvic floor via entire body exercise. PEFLOW trains on coordination of breathing and muscle movement, maximum contraction of PFM, quick contraction of the PFM, and enduring contraction of PFM. The frequency of exercise following PEFLOW is 2 sessions a week for 12 weeks. It should be performed under the guidance of the professional physiotherapist for the whole process. It is designed for offline and online exercise. Due to COVID-19 pandemic prevention, PEFLOW in this study would be performed by the participants in EG at home under the online guidance of 2 physiotherapists. In order to keep the training effective, we would conduct the training in grouping [26] with each including less than 10 persons and ensure that no woman is over than 12 weeks postpartum at her first session of PEFLOW.
The Physiotherapist-online-guided PEFLOW (OG-PEFLOW) would be performed by participants in EG twice sessions a week for 12 weeks (Figure3). OG-PEFLOW would be provided via Zoom and in the form of live broadcasting. To monitor the performance of the participants, the participants would be requested to turn on the camera on their playing devices during the whole sessional procedures; however, they would be fully informed that no video or picture would be recorded or shot to protect their privacy. In each session of the OG-PEFLOW, a physiotherapist would perform exercise guidance, while another physiotherapist would monitor the performance of the participants and take notes. Details of the PEFLOW will be published in another manuscript.
During the 12 weeks of intervention, participants in EG group would be requested to record their training load using RPE scale [30] every time after each training session. RPE quantitative evaluation of exercise load is calculated by “RPE score times x Exercise duration”. RPE scale indicates the exercise intensity in a specific time and the participants’ subjective psychological response to the stimulation from the exercise loads. In addition, Both EG and CG needs to record their training or exercise (if any) from the 6th week to 1 year postpartum. All of those records would be used for post-intervention assessment after 12-week intervention of EG.
The PEFLOW (Table 1 and Table 2) is a multimodal exercise program including moderate-intensity, aerobic, resistance, balance, and stretching exercise combined with PFMT, and the duration of each training session is about 60 min. Included in this program are ten sections, one for pelvic floor warm-up, eight for global exercises, and one for cooling down.

Table 1.
The 12-week Pelvic Floor Workout and the sectioning.

Table 2.
Data collection and follow-up instruments.
All participants in EG are informed to claim to the medical providers involved if any experiencing symptoms related to sport injury (e.g., knee pain, elbow pain, etc.). Any patients claiming to have such injury would be referred to the obstetric department or the physio therapist for treatment followed by an assessment for whether they should continue the training or not. An anticipated adverse event log would be prepared and sent to the principal investigator (PI) when such injury happens.
3. Data Collection and Management
Demographic data, including the age, height, weight, body mass index (BMI), prenatal maximum weight, physical activity during pre-pregnancy and pregnancy, and background data including the working position, smoking, alcohol consumption, urine leakage, asthma, constipation, family history of PFD, delivery history of pregnancy, weight gain during pregnancy, and fetal weight, would be collected at the enrollment visit of the study; while the following questionnaires would be filled by all participants at baseline and at all follow-up visits:
- (1)
- The International Physical Activity Questionnaire Score-Short Form (IPAQ-SF), which were recommended as a cost-effective method to assess physical activity by nine questions recording the activity of four levels of intensities in short forms: vigorous-intensity, moderate-intensity, walking, and sitting [31];
- (2)
- The Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20) and Pelvic Floor Impact Questionnaire-7 (PFIQ-7), which were designed to comprehensively evaluate to what extent the lower urinary tract, lower gastrointestinal tract, and pelvic organ prolapse symptoms affect the quality of life of women who suffer from PFD [32];
- (3)
- The Female Sexual Function Index (FSFI-6) [33], a common tool that has been validated for clinical use for evaluating female sexual function in six terms [34,35];
- (4)
- The Pittsburgh Sleep Quality Index (PSQI), which was developed in 1989 and accepted as the most common measure of sleep quality [36].
Baseline demographic data, IPAQ-SF, PFDI-20, PFIQ-7, FSFI-6, and PSQI were integrated into a WeChat mini program and can be filled by the Participants themselves by scanning a QR code on WeChat, a social App that is commonly used by the public in China. The body mass index (BMI) among the demographic data and all the scores or grades for all the questionnaires can be automatically come out by the configured formulas in the WeChat mini program.
Following the questionnaires in each of the visits would be the physical examination including PFM strength evaluation by Modified Oxford Grading (MOS) [3], pelvic organ prolapse quantitation (POP-Q) stage [5], vaginal relaxtity, symptomatic SUI detection and grading, pelvic floor surface electromyography (sEMG) based on Glazer protocol [37], pelvic floor ultrasound examination, quantitative measurement of pelvic sagittal rotation degree by X-ray, and evaluation of the overall body composition and strength.
Pelvic floor surface electromyography (sEMG) would be tested based on Glazer protocol. The participants would be taught to contract the pelvic floor muscle correctly and will have one practice before testing.
SUI is defined by SUI symptoms or a positive result of the cough stress test. Before the cough stress test, participants are suggested to keep fully bladder. Positive result of the test is defined as involuntarily urinary leakage when asked to cough in the lithotomy position.
Pelvic floor ultrasound indicators, which include LAM thickness, diameter of the levator hiatus, and levator hiatus area, were measured using the proprietary software 4D View via transperineal ultrasound(GE Kretz Medizintechnik), a reproducible and reliable measurement of vaginal support [38].
The quantitative measurement of pelvic sagittal rotation degree on Spine X-ray (Definium7000, General Electric Company, Boston, MD, USA) was analyzed which includes the pelvic tilt angle, the sacral slope angle, the difference of sacral slope and pelvic tilt, the ratio of the pelvic tilt angle to the sacral slope angle, the ratio of the pelvic tilt angle to the pelvic incidence angle and sacral-femoral distance.
The change of the overall body composition would be analyzed through body composition analyzers (Inbody 770), and overall strength which would be measured through hand grip strength test and trunk endurance test. Body composition analyzers would analyze data regarding waist hip ratio, basal metabolic rate, body fat rate, etc. Hand grip strength would be measured by JAMAR Plus+ grip gauge. The measurement accuracy is 0.1 kg. The participants should not have visible hand defects. The grip gauge should be adjusted before measurement. When the participants hold the grip gauge, the second knuckle of the index finger should be at 90 degrees. At the same time, mark the best position of each hand on the grip meter. Before measurement, the participants should remove wrist jewelry to avoid injury. The left and right hand are measured alternately three times. Trunk endurance would be tested using the Plank test, Side bend test, and Biering–Sorensen Test [39]. All the participants were encouraged to keep the positions as long as possible. Time as recorded in seconds with a maximal length of 90 s.
4. Outcomes of the Study
The primary outcome will be the comparison of participants’ pelvic floor muscle strengths using MOS scale at the enrollment baseline and post intervention. The secondary outcomes will be: (1) the occurrence of SUI, (2) the change of the Pelvic floor ultrasound indicators, (3) change of the Pelvic Organ Prolapse Quantitation measured by callipers, (4) change of the pelvic sagittal rotation degree, and (5) the change of the overall body composition and strength. The list of data collection instruments and time of data collection is presented in Table 2 and Table 3.

Table 3.
Outline of Soring for general pelvic floor function.
The other secondary outcome measures involved in the Table 2 will be calculated and discussed separately.
4.1. Sample Analysis
Sample size was calculated according to the improvement rate of MOS grade after 12-week training using PASS 2019 software. According to the preliminary experiment, the improvement rate of MOS in the CG was 20% and that of women in EG was 60% at 6 months postpartum. Group sample sizes of 106 in each group achieve 90.248% power to detect a difference between the group proportions of 0.4. The CG proportion is 0.2. The EG proportion is assumed to be 0.4 under the null hypothesis and 0.6 under the alternative hypothesis. The test statistic used is the one-sided Z test (unpooled). However, in considering 20% of the possible dropout, a total of 260 women will be randomized.
4.2. Statistical Analysis
Data will be analyzed using SPSS version 26.0 (SPSS, Inc., Chicago, IL, USA) and the statistically significant difference will be identified if p < 0.05. Descriptive statistics including numbers and proportions, means and standard deviations, or medians (P25, P75) will be used. Group differences in the primary and secondary outcomes will mainly use chi-square and student’s t tests. For primary outcome, we will count the rate of pelvic muscle strength reaching grade 4 at 6 months postpartum between EG and CG by chi-square test or Fisher’s exact test as appropriate. Analysis of the primary and secondary outcomes will be based on an intention-to-treat basis in consideration of the drop-offs from the follow-ups and be conducted by the statistician at Peking University Clinical Research Institute. For comparison between groups of quantitative data, the analysis of variance or Wilcoxon rank sum test will be used according to the data distribution; chi square test or exact probability method is used for counting data (if chi square test is not applicable), Wilcoxon rank sum test or CMH test is used for grade data, and logistic regression analysis is used for correlation analysis. Repeated ANOVA will be used to assess within-patient correlation. and multivariable linear regression models if potential confounders were imbalanced.
5. Discussion
Pelvic floor rehabilitation is becoming more and more important due to the rapid development of rehabilitation medicine and the improvement of the life quality of demanded by women. PFMT is one of the widely adopted exercise therapies in the clinic for female pelvic floor rehabilitation.
Although medical societies realize that rehabilitative exercises to be the currently demonstrated effective way to improve PFM, consensus on the standard for PFMT is still lack. Many issues are remaining; questions, such as “what is the right to exercise correctly?” and “what is the proper frequency and duration for PFM training?”, and reports on the efficacy of PFMT are much confusing. Due to the positional particularity and abstractness of pelvic floor muscles, it is difficult for a non-medical backgrounded woman to exercise pelvic floor muscle fiber I and fiber II directly, accurately, and/or effectively. PFMT has not been skilled for public populization, although many investigators have efforted exploring more convenient and effective pelvic floor rehabilitation methods.
In referring to comprehensive literature related to our previous research [20], we developed 12-week PEFLOW, with emphases on training of the entire muscle system.
PEFLOW is composed of 10 sections as shown in Table 1. The warm-up section was setup to have the participants percept the pelvic floor contractions in different body positions via self-feeling to the pelvic floor movements. In this section, participants are instructed to practice quick contraction (1”) and relaxation (2”) for perception of type II muscle fiber (fast-twist fiber) and hold-on contraction (8-10”) and relaxation (8-10”) for perception of type I muscle fibers (slow-twist fiber). The training of multiple repetitions for fast-twist fibers is also a way of targeting slow-twist fiber [41]. Section 1 was integrated in the program to train the pelvic contractions corelating to the movements of standing, heel lifting, single feet standing, and walking. According to the literature, feet play roles in control and adjustment of postures, and exercises corelated with the movement of feet can improve body balance and simulate feedback perception [42]. Section 2 was setup to improve the flexibility and mobility of the lumbar vertebrae and pelvic, so as to make them adapt the changes in woman’s body postures that is the unavoidable outcome of pregnancy and delivery due to the changes in lumbar vertebrae bulge, pelvic width and tilt, and the relevant muscle tension [43]. With Section 3, we tend to train the movements of PFM with correlating to breaths. It was programed based on a rational from multiple studies that exhaling maximizes PFM tension and strength [14,44]. Sections 4–8 were programed to train joint contractions of the core muscles, surrounding muscles and PFMs as what more and more scientific evidence demonstrated that PFM contraction can be optimized by joint contractions of the core muscles such as abdominal, lumbar dorsal, and diaphragm muscles [40], and surrounding muscles such as hip abductors [45,46].
Optimal and long-term therapeutic effects are anticipated. We made PEFLOW be performed at home due to the meeting restrictions in COVID-19 pandemic. However, we anticipate that home exercise with the facilitation of online guidance and encouragement will increase the participation rate and the concordance of the women in taking correct exercise. The requirement for participants to report the RPE score after each training session is not only an encouragement to the participants, but a guarantee of the appropriate training intensity being kept training effectively and safely [47].
The possible limitation of this trial might be that we lack more precise measurements for physical activity level, such as wrist or waist accelerometers to monitor heart rate during daily physical activities and trainings.
6. Conclusions
In conclusion, this study is expects that the 12-week online PEFLOW is a cost-effective training for the recovery of Pelvic floor muscle function, which is suitable for future clinic trails and also for clinical promotions.
Author Contributions
X.S. and W.J. are responsible for study design, conceptualization, and supervision. H.Z. is responsible for data management, writing articles, PEFLOW designs, and instructions for exercises. H.Z., D.Z., L.G. and B.X., are responsible for writing—review and editing. H.L. is responsible for software and methodology. Y.D. is responsible for data collection and exercises assistant. X.S. is responsible for funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Key Technology R&D Program of China (number: 2018YFC2002204) and the Chinese Association of Plastics and Aesthetics (number: 2020-Z-27).
Institutional Review Board Statement
This study protocol has been approved by the Ethics Committee of Peking University People’s Hospital (number: 2021PHB254-001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We thank all the participants in the study, all investigators in the project, and all clinical examiners from Peking University People’s Hospital for their contributions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhu, L.; Wenjia, L.O.U. Current situation of female pelvic floor rehabilitation in China. Chin. J. Fam. Plan. Gynecotokol. 2020, 12, 3–4, 8. (In Chinese) [Google Scholar]
- Lan, Z.H.U.; Wenjia, L.O.U. Pay attention to female sexual dysfunction diseases. J. Pract. Obstet. Gynecol. 2018, 34, 401–402. (In Chinese) [Google Scholar]
- Ferreira, C.H.J.; Barbosa, P.B.; Souza, F.D.O.; Antônio, F.I.; Franco, M.M.; Bø, K. Inter-rater reliability study of the modified Oxford Grading Scale and the Peritron manometer. Physiotherapy 2011, 97, 132–138. [Google Scholar] [CrossRef] [PubMed]
- El-Haieg, D.O.; Madkour, N.M.; Basha, M.A.A.; Ahmad, R.A.; Sadek, S.M.; Al-Molla, R.M.; Tantwy, E.F.; Almassry, H.N.; Altaher, K.M.; Mahmoud, N.E.M.; et al. Magnetic resonance imaging and 3-dimensional transperineal ultrasound evaluation of pelvic floor dysfunction in symptomatic women: A prospective comparative study. Ultrasonography 2019, 38, 355–364. [Google Scholar] [CrossRef]
- Bump, R.C.; Mattiasson, A.; Bo, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Borello-France, D.F.; Handa, V.L.; Brown, M.B.; Goode, P.; Kreder, K.; Scheufele, L.L.; Weber, A.M.; Pelvic Floor Disorders Network. Pelvic-floor muscle function in women with pelvic organ prolapse. Phys. Ther. 2007, 87, 399–407. [Google Scholar] [CrossRef]
- Gilchrist, A.S.; Campbell, W.; Steele, H.; Brazell, H.; Foote, J.; Swift, S. Outcomes of observation as therapy for pelvic organ prolapse: A study in the natural history of pelvic organ prolapse. Neurourol. Urodyn. 2013, 32, 383–386. [Google Scholar] [CrossRef]
- Miedel, A.; Ek, M.; Tegerstedt, G.; Maehle-Schmidt, M.; Nyren, O.; Hammarstrom, M. Short-term natural history in women with symptoms indicative of pelvic organ prolapse. Int. Urogynecol. J. 2011, 22, 461–468. [Google Scholar] [CrossRef]
- Sigurdardottir, T.; Steingrimsdottir, T.; Geirsson, R.T.; Halldorsson, T.I.; Aspelund, T.; Bo, K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence?: An assessor-blinded randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 222, 247.e1–247.e8. [Google Scholar] [CrossRef]
- Min, L.; Chunxue, Y.; Qiubo, L.; Xudong, D.; Yan, Z.; Guifang, Z.; Kejia, H.; Tianzi, G.; Qing, F. Effectiveness of intravaginal electrical stimulation combined with electromyography biofeedback-mediated pelvic floor muscle training for postpartum symptomatic pelvic organ prolapse: Protocol for the PROSPECT randomized trial. Trials 2022, 23, 131. [Google Scholar] [CrossRef]
- Bo, K.; Angles-Acedo, S.; Batra, A.; Braekken, I.H.; Chan, Y.L.; Jorge, C.H.; Kruger, J.; Yadav, M.; Dumoulin, C. International urogynecology consultation chapter 3 committee 2; conservative treatment of patient with pelvic organ prolapse: Pelvic floor muscle training. Int. Urogynecol. J. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kegel, A.H. Progressive resistance exercise in the functional restoration of the perineal muscles. Am. J. Obstet. Gynecol. 1948, 56, 238–248. [Google Scholar] [CrossRef]
- Iglesia, C.B.; Smithling, K.R. Pelvic Organ Prolapse. Am. Fam. Physician 2017, 96, 179–185. [Google Scholar]
- Zachovajeviene, B.; Siupsinskas, L.; Zachovajevas, P.; Venclovas, Z.; Milonas, D. Effect of diaphragm and abdominal muscle training on pelvic floor strength and endurance: Results of a prospective randomized trial. Sci. Rep. 2019, 9, 19192. [Google Scholar] [CrossRef] [PubMed]
- Oliva-Lozano, J.M.; Muyor, J.M. Core Muscle Activity During Physical Fitness Exercises: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4306. [Google Scholar] [CrossRef] [PubMed]
- Brennen, R.; Lin, K.Y.; Denehy, L.; Frawley, H.C. The Effect of Pelvic Floor Muscle Interventions on Pelvic Floor Dysfunction After Gynecological Cancer Treatment: A Systematic Review. Phys. Ther. 2020, 100, 1357–1371. [Google Scholar] [CrossRef] [PubMed]
- Tenfelde, S.; Logan, R.; Abernethy, M. Yoga from the pelvic floor. Beginnings 2014, 34, 24–26. [Google Scholar]
- Fozzatti, C.; Herrmann, V.; Palma, T.; Riccetto, C.L.; Palma, P.C. Global Postural Re-education: An alternative approach for stress urinary incontinence? Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 152, 218–224. [Google Scholar] [CrossRef]
- Fozzatti, M.C.; Palma, P.; Herrmann, V.; Dambros, M. Impact of global postural reeducation for treatment of female stress urinary incontinence. Rev. Assoc. Med. Bras. 2008, 54, 17–22. [Google Scholar] [CrossRef]
- Liu, T.; Hou, X.; Xie, B.; Wu, J.; Yang, X.; Sun, X.; Wang, J. Pelvic incidence: A study of a spinopelvic parameter in MRI evaluation of pelvic organ prolapse. Eur. J. Radiol. 2020, 132, 109286. [Google Scholar] [CrossRef]
- Teodori, R.M.; Negri, J.R.; Cruz, M.C.; Marques, A.P. Global Postural Re-education: A literature review. Rev. Bras. Fisioter. 2011, 15, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Dufour, S.; Wu, M. No. 397—Conservative Care of Urinary Incontinence in Women. J. Obstet. Gynaecol. Can. 2020, 42, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Talley, K.M.C.; Wyman, J.F.; Bronas, U.; Olson-Kellogg, B.J.; McCarthy, T.C. Defeating Urinary Incontinence with Exercise Training: Results of a Pilot Study in Frail Older Women. J. Am. Geriatr. Soc. 2017, 65, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Virtuoso, J.F.; Menezes, E.C.; Mazo, G.Z. Effect of Weight Training with Pelvic Floor Muscle Training in Elderly Women with Urinary Incontinence. Res. Q. Exerc. Sport 2019, 90, 141–150. [Google Scholar] [CrossRef]
- Bo, K. Physiotherapy management of urinary incontinence in females. J. Physiother. 2020, 66, 147–154. [Google Scholar] [CrossRef]
- Dumoulin, C.; Morin, M.; Danieli, C.; Cacciari, L.; Mayrand, M.H.; Tousignant, M.; Abrahamowicz, M. Group-Based vs Individual Pelvic Floor Muscle Training to Treat Urinary Incontinence in Older Women: A Randomized Clinical Trial. JAMA Intern. Med. 2020, 180, 1284–1293. [Google Scholar] [CrossRef]
- Gao, L.; Zhang, D.; Wang, S.; Jia, Y.; Wang, H.; Sun, X.; Wang, J. Effect of the App-Based Video Guidance on Prenatal Pelvic Floor Muscle Training Combined with Global Postural Re-education for Stress Urinary Incontinence Prevention: A Protocol for a Multicenter, Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12929. [Google Scholar] [CrossRef]
- Gasquet, I.; Tcherny-Lessenot, S.; Gaudebout, P.; Bosio, L.G.B.; Klein, P.; Haab, F. Influence of the severity of stress urinary incontinence on quality of life, health care seeking, and treatment: A national cross-sectional survey. Eur. Urol. 2006, 50, 818–825. [Google Scholar] [CrossRef]
- de Andrade, R.L.; Bo, K.; Antonio, F.I.; Driusso, P.; Mateus-Vasconcelos, E.C.L.; Ramos, S.; Julio, M.P.; Ferreira, C.H.J. An education program about pelvic floor muscles improved women’s knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: A randomised trial. J. Physiother. 2018, 64, 91–96. [Google Scholar] [CrossRef]
- Arney, B.E.; Glover, R.; Fusco, A.; Cortis, C.; de Koning, J.J.; van Erp, T.; Jaime, S.; Mikat, R.P.; Porcari, J.P.; Foster, C. Comparison of RPE (Rating of Perceived Exertion) Scales for Session RPE. Int. J. Sports Physiol. Perform. 2019, 14, 994–996. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Barber, M.D.; Walters, M.D.; Bump, R.C. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am. J. Obstet. Gynecol. 2005, 193, 103–113. [Google Scholar] [CrossRef]
- Isidori, A.M.; Pozza, C.; Esposito, K.; Giugliano, D.; Morano, S.; Vignozzi, L.; Corona, G.; Lenzi, A.; Jannini, E.A. Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J. Sex. Med. 2010, 7, 1139–1146. [Google Scholar] [CrossRef] [PubMed]
- Chedraui, P.; Perez-Lopez, F.R.; Sanchez, H.; Aguirre, W.; Martinez, N.; Miranda, O.; Plaza, M.S.; Schwager, G.; Narvaez, J.; Quintero, J.C.; et al. Assessment of sexual function of mid-aged Ecuadorian women with the 6-item Female Sexual Function Index. Maturitas 2012, 71, 407–412. [Google Scholar] [CrossRef]
- Sonbahar, A.E.; Culha, M.G.; Jannini, E. The validity and reliability of the Turkish version of the 6-item female sexual function index (FSFI-6) and the relationship between climacturia and female sexual dysfunction. Int. J. Impot. Res. 2021, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Oleksy, L.; Wojciechowska, M.; Mika, A.; Antos, E.; Bylina, D.; Kielnar, R.; Pruszczynski, B.; Stolarczyk, A. Normative values for Glazer Protocol in the evaluation of pelvic floor muscle bioelectrical activity. Medicine 2020, 99, e19060. [Google Scholar] [CrossRef]
- Kobak, W.H.; Rosenberger, K.; Walters, M.D. Interobserver variation in the assessment of pelvic organ prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 1996, 7, 121–124. [Google Scholar] [CrossRef]
- Martinez-Romero, M.T.; Ayala, F.; De Ste, C.M.; Vera-Garcia, F.J.; Sainz, D.B.P.; Santonja-Medina, F.; Sanchez-Meca, J. A Meta-Analysis of the Reliability of Four Field-Based Trunk Extension Endurance Tests. Int. J. Environ. Res. Public Health 2020, 17, 3088. [Google Scholar] [CrossRef]
- Blomquist, J.L.; Carroll, M.; Munoz, A.; Handa, V.L. Pelvic floor muscle strength and the incidence of pelvic floor disorders after vaginal and cesarean delivery. Am. J. Obstet. Gynecol. 2020, 222, 62.e1–62.e8. [Google Scholar] [CrossRef]
- Deshmukh, A.S.; Steenberg, D.E.; Hostrup, M.; Birk, J.B.; Larsen, J.K.; Santos, A.; Kjobsted, R.; Hingst, J.R.; Scheele, C.C.; Murgia, M.; et al. Deep muscle-proteomic analysis of freeze-dried human muscle biopsies reveals fiber type-specific adaptations to exercise training. Nat. Commun. 2021, 12, 304. [Google Scholar] [CrossRef] [PubMed]
- Viseux, F.; Lemaire, A.; Barbier, F.; Charpentier, P.; Leteneur, S.; Villeneuve, P. How can the stimulation of plantar cutaneous receptors improve postural control? Review and clinical commentary. Neurophysiol. Clin. 2019, 49, 263–268. [Google Scholar] [CrossRef] [PubMed]
- de Tayrac, R.; Schantz, C. Childbirth pelvic floor trauma: Anatomy, physiology, pathophysiology and special situations—CNGOF perineal prevention and protection in obstetrics guidelines. Gynecol. Obstet. Fertil. Senol. 2018, 46, 900–912. [Google Scholar] [CrossRef] [PubMed]
- Wieland, L.S.; Shrestha, N.; Lassi, Z.S.; Panda, S.; Chiaramonte, D.; Skoetz, N. Yoga for treating urinary incontinence in women. Cochrane Database Syst. Rev. 2019, 2, CD012668. [Google Scholar] [CrossRef]
- Tuttle, L.J.; Autry, T.; Kemp, C.; Lassaga-Bishop, M.; Mettenleiter, M.; Shetter, H.; Zukowski, J. Hip exercises improve intravaginal squeeze pressure in older women. Physiother. Theory Pract. 2020, 36, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.S.; Pedriali, F.R.; Urbano, M.R.; Moreira, E.H.; Averbeck, M.A.; Almeida, S.H.M. The effects of Pilates method on pelvic floor muscle strength in patients with post-prostatectomy urinary incontinence: A randomized clinical trial. Neurourol. Urodyn. 2018, 37, 346–353. [Google Scholar] [CrossRef]
- Nygaard, I.E.; Wolpern, A.; Bardsley, T.; Egger, M.J.; Shaw, J.M. Early postpartum physical activity and pelvic floor support and symptoms 1 year postpartum. Am. J. Obstet. Gynecol. 2021, 224, 193.e1–193.e19. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
