The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
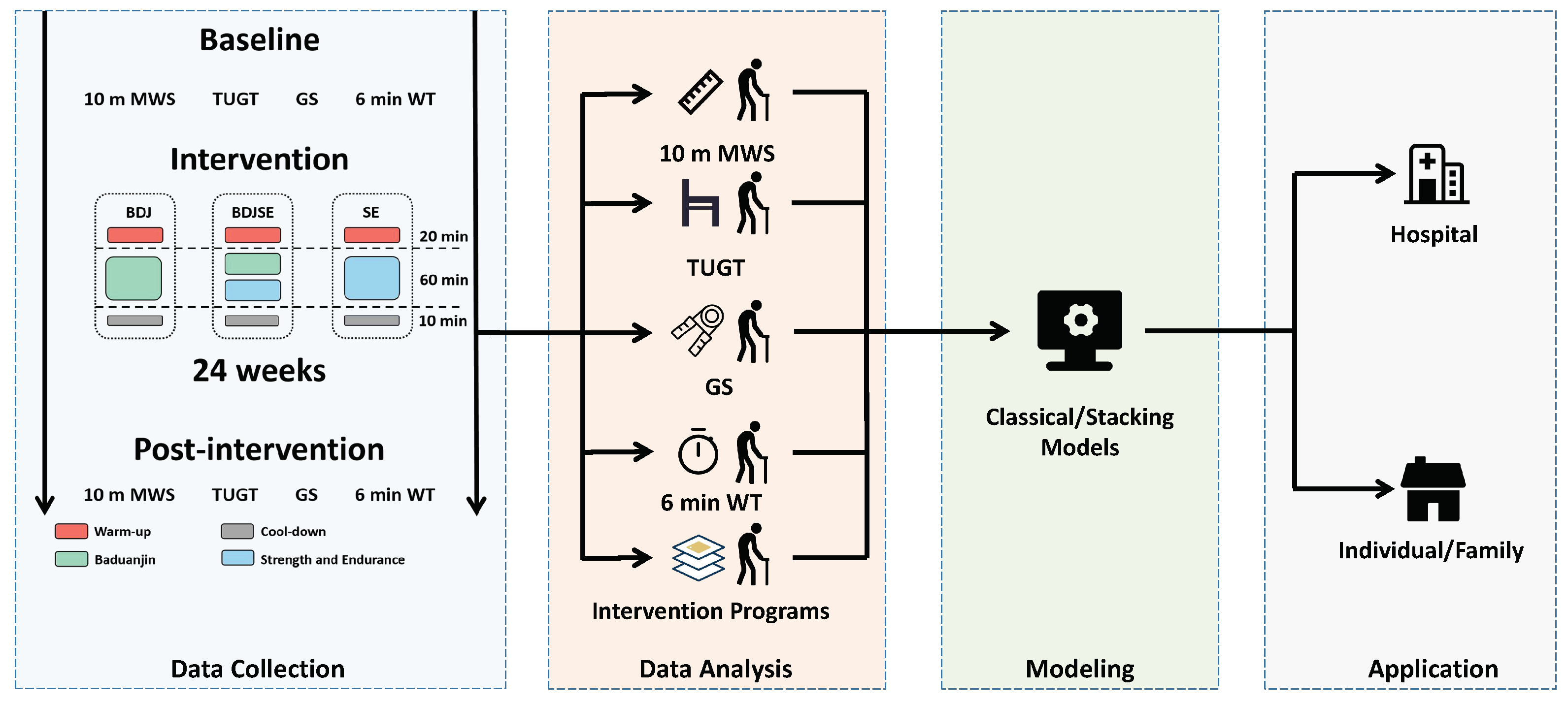
2.2. Study Design
2.2.1. Experimental Arrangement
2.2.2. Intervention
- (1)
- Baduanjin: The exercise regimen of Baduanjin was divided into two phases: the first phase continued for 8 weeks, while the second phase continued for 16 weeks. During the first phase of the project, one group was assigned to perform the intervention three times, while another group, the BDJSE group, was assigned to perform the exercise only once. In the next stage, the number of replicates was three and two for the BDJ and BDJSE groups, respectively.
- (2)
- Strength Training: This consisted of three training phases and included five exercises to improve cardiorespiratory fitness and muscle strength [47]. The five movements included three upper-body movements and two lower-body movements. The three upper-body movements were seated rowing, reverse grip curls, and bicep curls, and the two lower-body movements were calf lifts when seated and hip adduction exercises. Elastic bands were utilized in each and every one of the strength workouts. The intensity of the exercise could be determined by the elastic band color. The training consisted of three distinct phases that were repeated every 8 weeks. Phase I aimed to better acclimate subjects to the high-intensity exercise in Phases II and III by using light loads (40–60% of 1RM) and high repeats (12–20), while simultaneously increasing muscle power and muscle endurance by accomplishing 2–4 rounds of training workouts. The second phase of the program was designed to induce muscle growth and improve the muscle mass to fat mass ratio by continuously raising the load to ultimate capacity (60.0–80.0% of 1RM) with 5–12 repeats and 2–4 rounds. The training protocols were intended to achieve these goals. The third phase was intended to optimize the development of strength and also encourage the growth of muscular tissue by utilizing a greater load (70–85% of 1RM) for 5–8 repeats over 2–4 rounds. The SE group would finish four rounds, while the BDJSE group would finish two rounds, with a break of between 2 and 3 min after each round.
- (3)
- Endurance Training: We monitored the subjects’ heart rates during the exercise period using a heart rate monitor (MYZONE MZ-3, China). The exercise was conducted via continuous walking on an artificial track. In this investigation, the target heart rate was adapted separately for each subject based on the baseline measure. Exercise level was progressively elevated from 50% of baseline heart rate capacity (first 12 weeks) to 80% (the following 12 weeks) [48]. The SE group undertook 30 min of endurance walking exercise, while the BDJSE group accomplished 15 min. In all exercises, at least two medical staff accompanied the training, and the training was promptly terminated if the subjects became uncomfortable.
2.3. Assessment of Frailty
- (1)
- Unconscious weight loss: Participants were asked whether their weight had decreased by more than 4.5 kg (or 5% of body weight) without intention in the past year.
- (2)
- Self-reported fatigue: Participants were asked how often they were too exhausted to participate in any activity that required their full engagement for more than 2 days in a week.
- (3)
- Grip strength: Subjects’ grip strengths were determined by utilizing a calibrated Jamar Hydraulic Hand Dynamometer (model SH5001, Saehan Corp, Masan, Korea, 2017). Every person was given three chances to be evaluated, and their highest score was counted. The grasp was examined to determine if males weighed less than 26 kg and females weighed less than 18 kg.
- (4)
- The walking speed: The 10 meter walk speed of the subjects was recorded. Older people were judged frail if their walking speed was lower than or equal to 1 m/s.
- (5)
- Low level of physical activity: The level of physical activity of individuals was determined by the Physical Activity Scale for the Elderly in the Chinese population (PASE-C) [50]. Low physical activity was defined in men as a cut-off value of less than 383 calories per week and in women of less than 270 calories per week, respectively.
2.4. Assessment of Physical Fitness
- (1)
- 10 m MWS: Subjects performed two 50-m walking exercises as quickly as possible in a calm testing setting, and the time to cover 2.5 to 12.5 m was calculated to ensure the steady status of data. The highest value was utilized in the study.
- (2)
- TUGT: Subjects were seated in a conventional chair 45 cm in height and, when prompted by the research assistant, stood up and performed a 3 meter circumference walk around the room as quickly as possible before returning to their seat.
- (3)
- Grip strength: Grip strength was measured utilizing a calibrated Jamar Hydraulic Hand Dynamometer (model SH5001, Saehan Corp, Masan, Korea, 2017). In a standing position, subjects conducted three grip strength assessments, and the best score was considered the test result.
- (4)
- 6 min WT: The 6 min WT was utilized to evaluate the endurance of the subjects. The test was conducted on a 30-m, enclosed, level promenade. Along the promenade, signs were set every 3 meters, and turn signals were established at each end. Individuals were urged to cover the greatest distance possible along the promenade.
2.5. Data Analyses
2.6. Statistical Analyses
3. Results
3.1. Participants
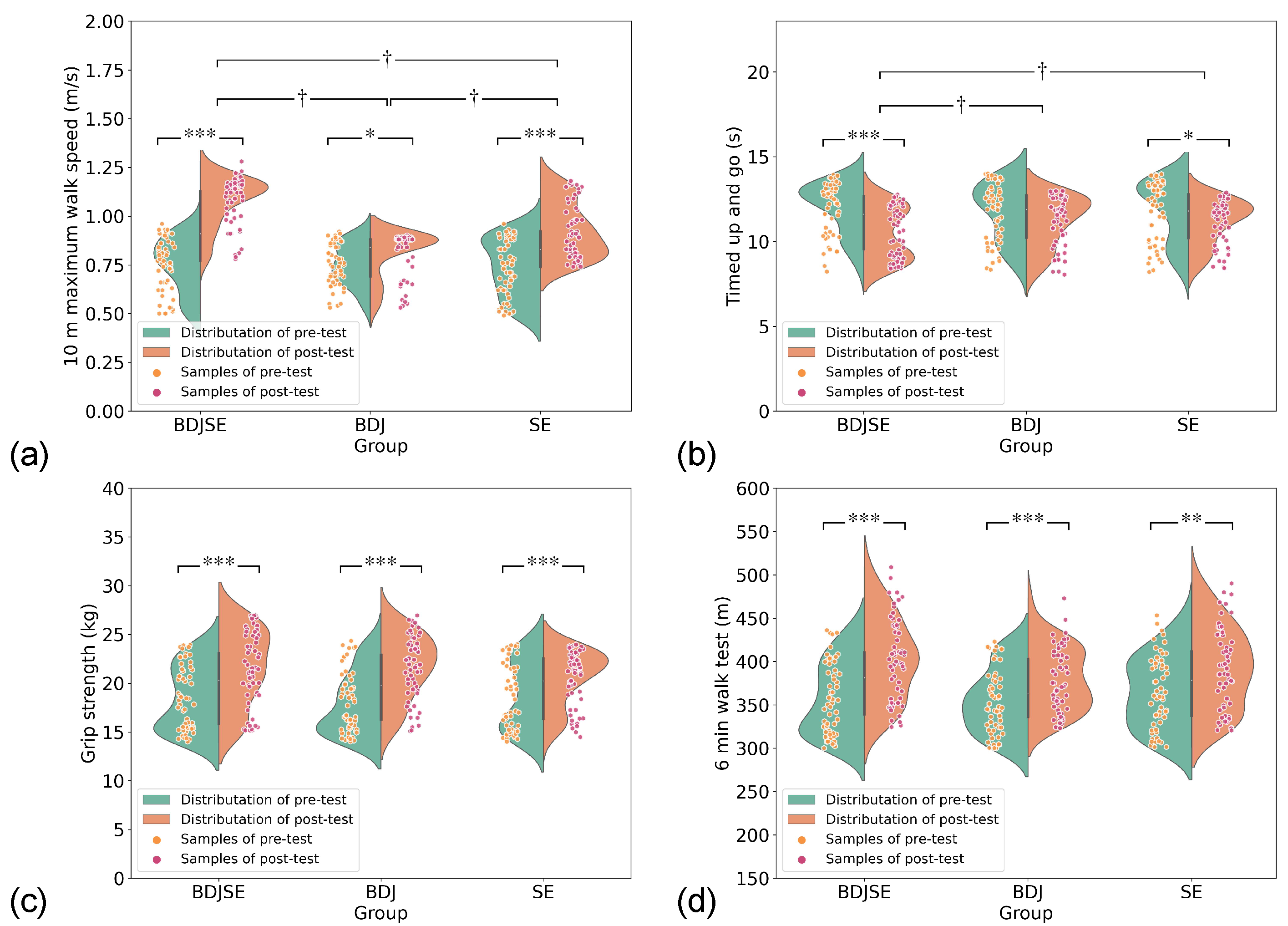
3.2. Two-Way Repeated-Measures ANOVA Results for Physical Fitness
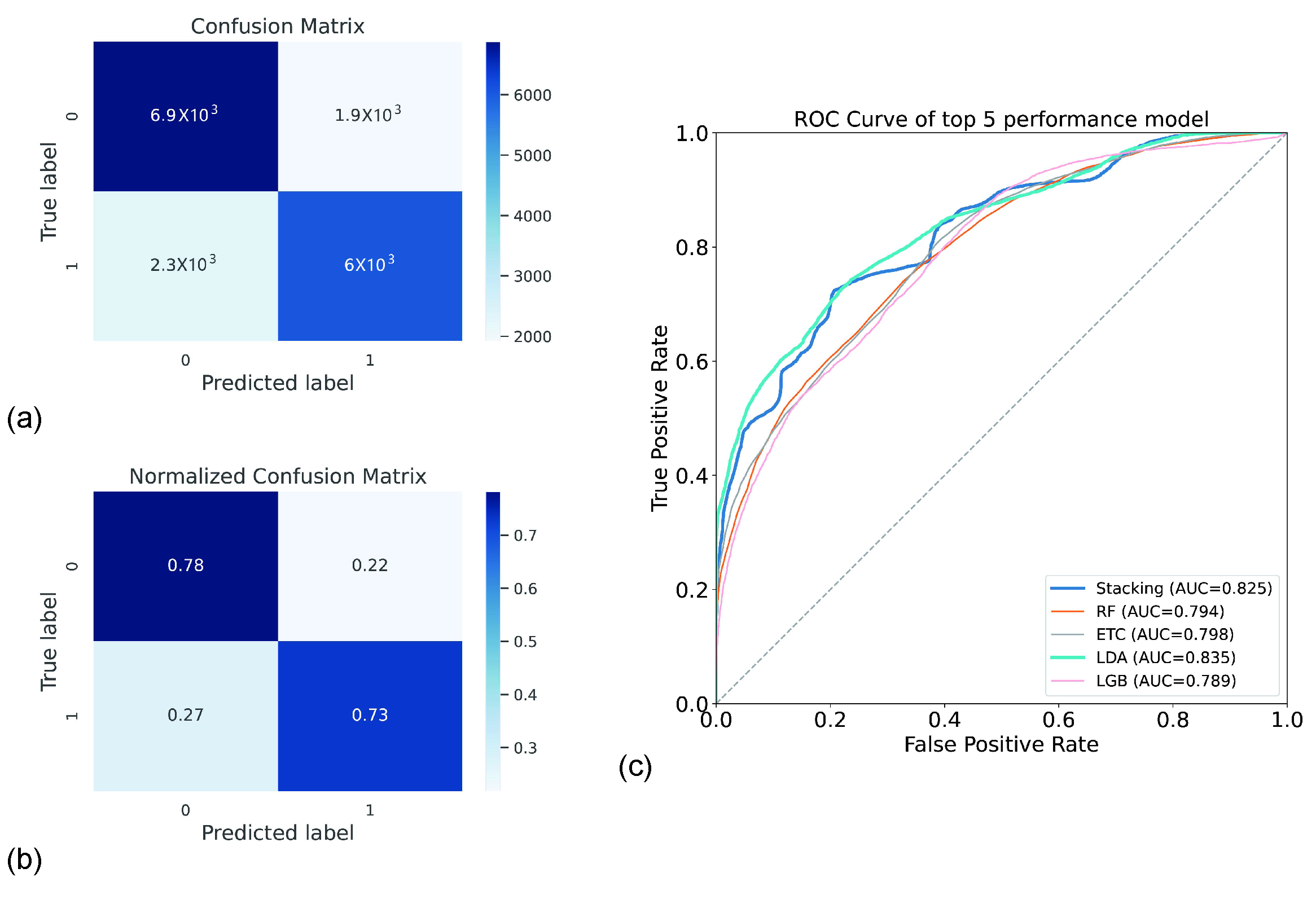
3.3. Results of Machine Learning Model Classification
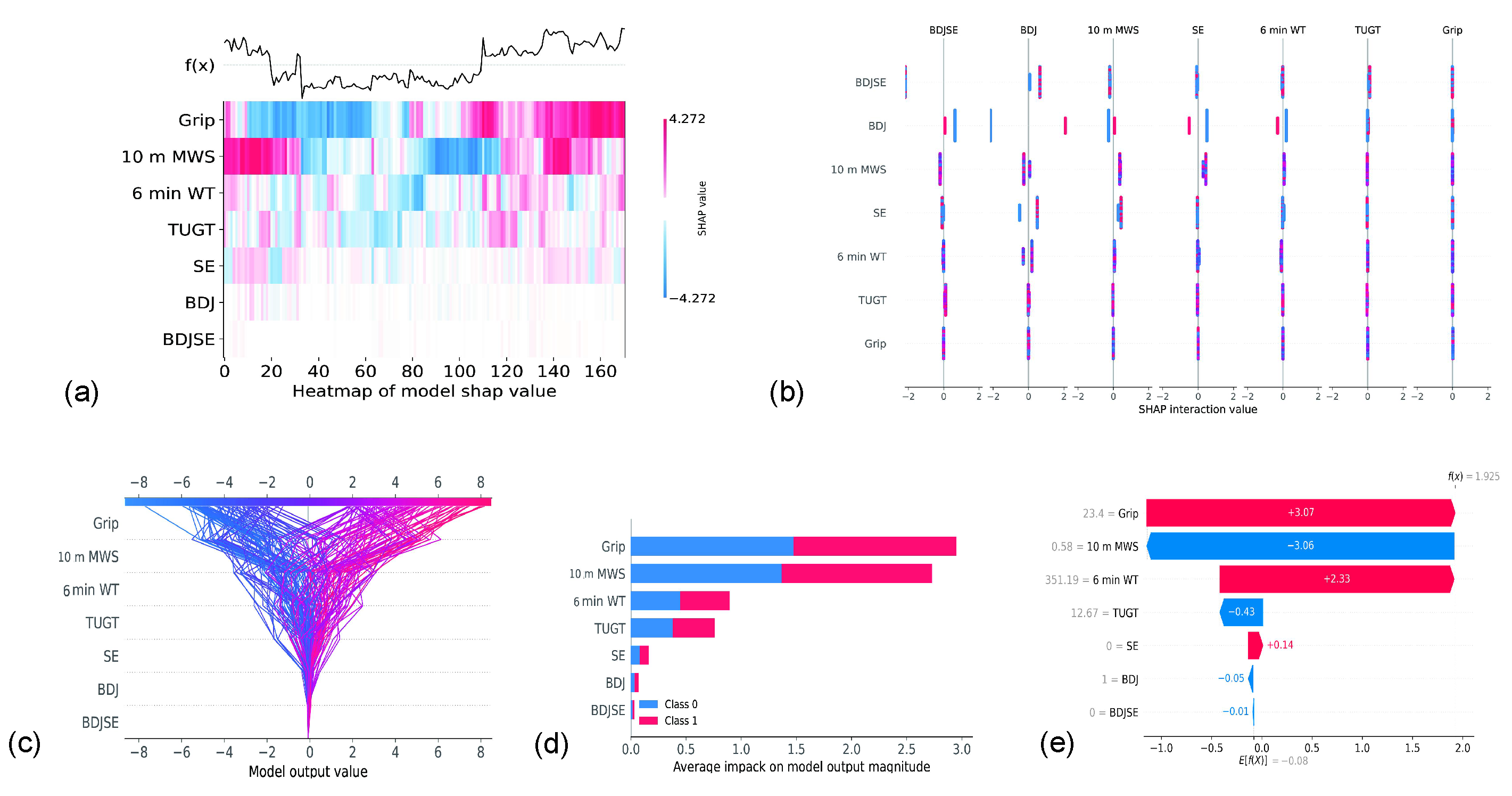
3.4. Contribution of Each Feature
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- To, T.L.; Doan, T.N.; Ho, W.C.; Liao, W.C. Prevalence of Frailty among Community-Dwelling Older Adults in Asian Countries: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 895. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and risk factors for frailty among community-dwelling older people in China: A systematic review and meta-analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.Y.; Sun, Z.; Tan, C.C.; Tan, L.; Xu, W. Multi-Concept Frailty Predicts the Late-Life Occurrence of Cognitive Decline or Dementia: An Updated Systematic Review and Meta-Analysis of Longitudinal Studies. Front. Aging Neurosci. 2022, 14, 855553. [Google Scholar] [CrossRef]
- Cesari, M.; Calvani, R.; Marzetti, E. Frailty in Older Persons. Clin. Geriatr. Med. 2017, 33, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.; Tangen, C.; Walston, J.; Newman, A.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.; Burke, G.; et al. Frailty in Older Adults Evidence for a Phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Kim, S.w.; Han, H.S.; Jung, H.w.; Kim, K.i.; Hwang, D.W.; Kang, S.B.; Kim, C.H. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg. 2014, 149, 633–640. [Google Scholar] [CrossRef]
- McIsaac, D.I.; Bryson, G.L.; van Walraven, C. Association of frailty and 1-year postoperative mortality following major elective noncardiac surgery: A population-based cohort study. JAMA Surg. 2016, 151, 538–545. [Google Scholar] [CrossRef]
- McIsaac, D.I.; Taljaard, M.; Bryson, G.L.; Beaulé, P.E.; Gagné, S.; Hamilton, G.; Hladkowicz, E.; Huang, A.; Joanisse, J.A.; Lavallée, L.T.; et al. Frailty as a predictor of death or new disability after surgery: A prospective cohort study. Ann. Surg. 2020, 271, 283–289. [Google Scholar] [CrossRef]
- Shah, R.; Attwood, K.; Arya, S.; Hall, D.E.; Johanning, J.M.; Gabriel, E.; Visioni, A.; Nurkin, S.; Kukar, M.; Hochwald, S.; et al. Association of frailty with failure to rescue after low-risk and high-risk inpatient surgery. JAMA Surg. 2018, 153, e180214. [Google Scholar] [CrossRef]
- Joseph, B.; Phelan, H.; Hassan, A.; Jokar, T.O.; O’Keeffe, T.; Azim, A.; Gries, L.; Kulvatunyou, N.; Latifi, R.; Rhee, P. The impact of frailty on failure-to-rescue in geriatric trauma patients: A prospective study. J. Trauma Acute Care Surg. 2016, 81, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Arya, S.; Kim, S.I.; Duwayri, Y.; Brewster, L.P.; Veeraswamy, R.; Salam, A.; Dodson, T.F. Frailty increases the risk of 30-day mortality, morbidity, and failure to rescue after elective abdominal aortic aneurysm repair independent of age and comorbidities. J. Vasc. Surg. 2015, 61, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Saxton, A.; Velanovich, V. Preoperative frailty and quality of life as predictors of postoperative complications. Ann. Surg. 2011, 253, 1223–1229. [Google Scholar] [CrossRef] [PubMed]
- Augustin, T.; Burstein, M.D.; Schneider, E.B.; Morris-Stiff, G.; Wey, J.; Chalikonda, S.; Walsh, R.M. Frailty predicts risk of life-threatening complications and mortality after pancreatic resections. Surgery 2016, 160, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Farhat, J.S.; Falvo, A.J.; Horst, M.H.; Swartz, A.; Velanovich, V.; Patton, J.H.; Rubinfeld, I.S. Are the frail destined to fail? Frailty index as a predictor of surgical morbidity and mortality in the elderly. J. Trauma Acute Care Surg. 2011, 213, S65. [Google Scholar] [CrossRef]
- Suskind, A.M.; Walter, L.C.; Jin, C.; Boscardin, J.; Sen, S.; Cooperberg, M.R.; Finlayson, E. Impact of frailty on complications in patients undergoing common urological procedures: A study from the American College of Surgeons National Surgical Quality Improvement database. BJU Int. 2016, 117, 836–842. [Google Scholar] [CrossRef]
- Adams, P.; Ghanem, T.; Stachler, R.; Hall, F.; Velanovich, V.; Rubinfeld, I. Frailty as a predictor of morbidity and mortality in inpatient head and neck surgery. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 783–789. [Google Scholar] [CrossRef]
- George, E.M.; Burke, W.M.; Hou, J.Y.; Tergas, A.I.; Chen, L.; Neugut, A.I.; Ananth, C.V.; Hershman, D.L.; Wright, J.D. Measurement and validation of frailty as a predictor of outcomes in women undergoing major gynaecological surgery. BJOG 2016, 123, 455–461. [Google Scholar] [CrossRef]
- Figueroa, J.F.; Joynt Maddox, K.E.; Beaulieu, N.; Wild, R.C.; Jha, A.K. Concentration of potentially preventable spending among high-cost Medicare subpopulations: An observational study. Ann. Intern. Med. 2017, 167, 706–713. [Google Scholar] [CrossRef]
- Martínez-Reig, M.; Aranda-Reneo, I.; Peña-Longobardo, L.M.; Oliva-Moreno, J.; Barcons-Vilardell, N.; Hoogendijk, E.O.; Abizanda, P. Use of health resources and healthcare costs associated with nutritional risk: The FRADEA study. Clin. Nutr. 2018, 37, 1299–1305. [Google Scholar] [CrossRef]
- Robinson, T.N.; Wu, D.S.; Stiegmann, G.V.; Moss, M. Frailty predicts increased hospital and six-month healthcare cost following colorectal surgery in older adults. Am. J. Surg. 2011, 202, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Goldfarb, M.; Bendayan, M.; Rudski, L.G.; Morin, J.F.; Langlois, Y.; Ma, F.; Lachapelle, K.; Cecere, R.; DeVarennes, B.; Tchervenkov, C.I.; et al. Cost of Cardiac Surgery in Frail Compared With Nonfrail Older Adults. Can. J. Cardiol. 2017, 33, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.; Gahbauer, E.; Allore, H.; Han, L. Transitions Between Frailty States Among Community-Living Older Persons. Arch. Intern. Med. 2006, 166, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liu, Z.; Liu, Y.; Ye, L. Exercise interventions for older people at risk for frailty: A protocol for systematic review and meta-analysis. Medicine 2021, 100. [Google Scholar] [CrossRef] [PubMed]
- Chittrakul, J.; Siviroj, P.; Sungkarat, S.; Sapbamrer, R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 3102. [Google Scholar] [CrossRef]
- Kasim, N.F.; Veldhuijzen van Zanten, J.; Aldred, S. Tai Chi is an effective form of exercise to reduce markers of frailty in older age. Exp. Gerontol. 2020, 135, 110925. [Google Scholar] [CrossRef]
- Cadore, E.L.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Idoate, F.; Millor, N.; Gómez, M.; Rodriguez-Mañas, L.; Izquierdo, M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age 2013, 36, 773–785. [Google Scholar] [CrossRef]
- Bray, N.W.; Smart, R.R.; Jakobi, J.M.; Jones, G.R. Exercise prescription to reverse frailty. Appl. Physiol. Nutr. Metab. 2016, 41, 1112–1116. [Google Scholar] [CrossRef]
- Cadore, E.; Pinto, R.; Bottaro, M.; Izquierdo, M. Strength and Endurance Training Prescription in Healthy and Frail Elderly. Aging Dis. 2014, 5, 183. [Google Scholar] [CrossRef]
- Liao, Y.; Lin, Y.; Zhang, C.; Xue, X.L.; Mao, Q.X.; Zhang, Y.; Dai, J.g.; Wang, T.F. Intervention Effect of Baduanjin Exercise on the Fatigue State in People with Fatigue-Predominant Subhealth: A Cohort Study. J. Altern. Complement. Med. 2015, 21, 554–562. [Google Scholar] [CrossRef]
- Zou, L.; Sasaki, J.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M. A Systematic Review and Meta-Analysis of Baduanjin Qigong for Health Benefits: Randomized Controlled Trials. Evid. Based Complement. Alternat. Med. 2017, 2017, 4548706. [Google Scholar] [CrossRef] [PubMed]
- Devereux-Fitzgerald, A.; Powell, R.; Dewhurst, A.; French, D.P. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc. Sci. Med. 2016, 158, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.Y.; Chen, W.; Wang, R.Y. Effects of Kinect-based exergaming on frailty status and physical performance in the prefrail and frail elderly: A randomized controlled trial. Sci. Rep. 2019, 9, 9353. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Suzuki, T.; Kim, M.; Kojima, N.; Ota, N.; Shimotoyodome, A.; Hase, T.; Hosoi, E.; Yoshida, H. Effects of Exercise and Milk Fat Globule Membrane (MFGM) Supplementation on Body Composition, Physical Function, and Hematological Parameters in Community-Dwelling Frail Japanese Women: A Randomized Double Blind, Placebo-Controlled, Follow-Up Trial. PLoS ONE 2015, 10, e0116256. [Google Scholar] [CrossRef]
- Sadjapong, U.; Yodkeeree, S.; Sungkarat, S.; Siviroj, P. Multicomponent exercise program reduces frailty and inflammatory biomarkers and improves physical performance in community-dwelling older adults: A randomized controlled trial. Int. J. Environ. Res. Public Health 2020, 17, 3760. [Google Scholar] [CrossRef]
- Tarazona-Santabalbina, F.J.; Gómez-Cabrera, M.C.; Pérez-Ros, P.; Martínez-Arnau, F.M.; Cabo, H.; Tsaparas, K.; Salvador-Pascual, A.; Rodriguez-Mañas, L.; Viña, J. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: A randomized clinical trial. J. Am. Med. Dir. Assoc. 2016, 17, 426–433. [Google Scholar] [CrossRef]
- Fernández-García, Á.I.; Gómez-Cabello, A.; Gómez-Bruton, A.; Moradell, A.; Navarrete-Villanueva, D.; Pérez-Gómez, J.; González-Gross, M.; Ara, I.; Casajús, J.A.; Vicente-Rodríguez, G. Effects of multicomponent training and detraining on fitness of older adults with or at risk of frailty: Results of a 10-month quasi-experimental study. Eur. J. Sport Sci. 2022, 1–29. [Google Scholar] [CrossRef]
- Cadore, E.L.; de Asteasu, M.L.S.; Izquierdo, M. Multicomponent exercise and the hallmarks of frailty: Considerations on cognitive impairment and acute hospitalization. Exp. Gerontol. 2019, 122, 10–14. [Google Scholar] [CrossRef]
- Dun, Y.; Hu, P.; Ripley-Gonzalez, J.W.; Zhou, N.; Li, H.; Zhang, W.; Chen, M.; Zheng, Q.; Cui, N.; Wu, S.; et al. Effectiveness of a multicomponent exercise program to reverse pre-frailty in community-dwelling Chinese older adults: A randomised controlled trial. Age Ageing 2022, 51, afac026. [Google Scholar] [CrossRef]
- Meng, D.; Guo, H.; Liang, S.; Tian, Z.; Wang, R.; Yang, G.; Wang, Z. Effectiveness of a Hybrid Exercise Program on the Physical Abilities of Frail Elderly and Explainable Artificial-Intelligence-Based Clinical Assistance. Int. J. Environ. Res. Public Health 2022, 19, 6988. [Google Scholar] [CrossRef]
- Shirwaikar, R.D.; Acharya U, D.; Makkithaya, K.; M, S.; Srivastava, S.; Lewis U, L.E.S. Optimizing neural networks for medical data sets: A case study on neonatal apnea prediction. Artif. Intell. Med. 2019, 98, 59–76. [Google Scholar] [CrossRef] [PubMed]
- Vellido, A. The importance of interpretability and visualization in machine learning for applications in medicine and health care. Neural Comput. Appl. 2020, 32, 18069–18083. [Google Scholar] [CrossRef]
- Hassan, A.; Hassan, M.; Hassan, M.; Ellahham, S. The Role of Artificial Intelligence in Revolutionizing Frailty Diagnosis and Patient Care. Gerontol. Geriatr. Res. 2021, 7, 1055. [Google Scholar]
- Kouroubali, A.; Kondylakis, H.; Logothetidis, F.; Katehakis, D.G. Developing an AI-Enabled Integrated Care Platform for Frailty. Healthcare 2022, 10, 443. [Google Scholar] [CrossRef]
- Oliosi, E.; Guede-Fernández, F.; Londral, A. Machine Learning Approaches for the Frailty Screening: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 8825. [Google Scholar] [CrossRef]
- Mohanty, S.D.; Lekan, D.; McCoy, T.P.; Jenkins, M.; Manda, P. Machine learning for predicting readmission risk among the frail: Explainable AI for healthcare. Patterns 2022, 3, 100395. [Google Scholar] [CrossRef] [PubMed]
- Karavirta, L.; Häkkinen, A.; Sillanpää, E.; García-López, D.; Kauhanen, A.; Haapasaari, A.; Alen, M.; Pakarinen, A.; Kraemer, W.J.; Izquierdo, M.; et al. Effects of combined endurance and strength training on muscle strength, power and hypertrophy in 40–67-year-old men. Scand. J. Med. Sci. Sport. 2011, 21, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Kallinen, M.; Sipilä, S.; Alen, M.; Suominen, H. Improving cardiovascular fitness by strength or endurance training in women aged 76–78 years. A population-based, randomized controlled trial. Age Ageing 2002, 31, 247–254. [Google Scholar] [CrossRef]
- HAN, J.; WANG, J.; XIE, B.; WANG, Y. Comparison of consistency and validity of Fried frailty phenotype, Frail scale and Edmonton frailty scale for frailty screening among community-dwelling older adults. Chin. Gen. Pract. 2021, 24, 2669. [Google Scholar]
- Ngai, S.; Cheung, R.; Lam, P.; Chiu, J.; Fung, E. Validation and reliability of the Physical Activity Scale for the Elderly in Chinese population. J. Rehabil. Med. 2012, 44, 462–465. [Google Scholar] [CrossRef]
- Rothman, M.; Leo-Summers, L.; Gill, T. Prognostic Significance of Potential Frailty Criteria Comment. J. Am. Geriatr. Soc. 2009, 56, 2211–2216. [Google Scholar] [CrossRef] [PubMed]
- Wickstrom, R.J.; Wang, Y.C.; Wickstrom, N.E.; Smith, R.L.; Dunning, K.K. A new two square agility test for workplace health—reliability, validity and minimal detectable change. J. Phys. Ther. Sci. 2019, 31, 823–830. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Syddall, H.; Westbury, L.; Dodds, R.; Dennison, E.; Cooper, C.; Aihie Sayer, A. Mortality in the Hertfordshire Ageing Study: Association with level and loss of hand grip strength in later life. Age Ageing 2016, 46, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Kuh, D.; Cooper, C.; Sayer, A.A. Global variation in grip strength: A systematic review and meta-analysis of normative data. Age Ageing 2016, 45, 209–216. [Google Scholar] [CrossRef]
- Syddall, H.; Cooper, C.; Martin, F.; Briggs, R.; Aihie Sayer, A. Is grip strength a useful single marker of frailty? Age Ageing 2003, 32, 650–656. [Google Scholar] [CrossRef]
- Jones, S.; Tillin, T.; Williams, S.; Coady, E.; Chaturvedi, N.; Hughes, A. Assessment of Exercise Capacity and Oxygen Consumption Using a 6 min Stepper Test in Older Adults. Front. Physiol. 2017, 8, 408. [Google Scholar] [CrossRef]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.Y. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In Proceedings of the NeurIPS Proceedings, Montreal, QC, Canada, 3–8 December 2018. [Google Scholar]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Chen, T.Q.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Abhishek, L. Optical Character Recognition using Ensemble of SVM, MLP and Extra Trees Classifier. In Proceedings of the 2020 International Conference for Emerging Technology (INCET), Belgaum, India, 5–7 June 2020; pp. 1–4. [Google Scholar]
- Li, L.; Zhang, X. Study of data mining algorithm based on decision tree. In Proceedings of the 2010 International Conference On Computer Design and Applications, Qinhuangdao, China, 25–27 June 2010; Volume 1, pp. V1-155–V1-158. [Google Scholar]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Szostak, D.; Walkowiak, K.; Włodarczyk, A. Short-Term Traffic Forecasting in Optical Network using Linear Discriminant Analysis Machine Learning Classifier. In Proceedings of the 2020 22nd International Conference on Transparent Optical Networks (ICTON), Bari, Italy, 19–23 July 2020; pp. 1–4. [Google Scholar]
- Kumar, R.; Naik, S.M.; Naik, V.D.; Shiralli, S.; V.G, S.; Husain, M. Predicting clicks: CTR estimation of advertisements using Logistic Regression classifier. In Proceedings of the 2015 IEEE International Advance Computing Conference (IACC), Banglore, India, 12–13 June 2015; pp. 1134–1138. [Google Scholar]
- Lundberg, S.; Lee, S.I. A Unified Approach to Interpreting Model Predictions. In Proceedings of the 31st International Conference on Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017; pp. 4768–4777. [Google Scholar]
- Zou, L.; Wang, C.; Chen, X.; Wang, H. Baduanjin Exercise for Stroke Rehabilitation: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2018, 15, 600. [Google Scholar] [CrossRef]
- Binder, E.F.; Schechtman, K.B.; Ehsani, A.A.; Steger-May, K.; Brown, M.; Sinacore, D.R.; Yarasheski, K.E.; Holloszy, J.O. Effects of Exercise Training on Frailty in Community-Dwelling Older Adults: Results of a Randomized, Controlled Trial. J. Am. Geriatr. Soc. 2002, 50, 1921–1928. [Google Scholar] [CrossRef]
| Items | BDJ 1 (n = 57) | BDJSE 2 (n = 57) | SE 3 (n = 57) | p Value |
|---|---|---|---|---|
| Sex (male/female) | 28/29 | 27/30 | 25/32 | 0.736 |
| Age (years) | 71.84 ± 3.77 | 70.65 ± 3.73 | 70.74 ± 3.52 | 0.163 |
| Stature (cm) | 165.83 ± 6.77 | 163.41 ± 7.58 | 165.54 ± 8.22 | 0.182 |
| Body mass (kg) | 64.53 ± 5.59 | 62.97 ± 7.11 | 63.05 ± 6.88 | 0.378 |
| Parameters | BDJ 1 (n = 57) | BDJSE 2 (n = 57) | SE 3 (n = 57) | Group × Time # | |||
|---|---|---|---|---|---|---|---|
| Baseline | 24 Weeks | Baseline | 24 Weeks | Baseline | 24 Weeks | p-Value | |
| 10 m MWS (m/s) | 0.75 ± 0.11 | 0.82 ± 0.12 †,* | 0.75 ± 0.14 | 1.08 ± 0.12 †,*** | 0.73 ± 0.13 | 0.93 ± 0.14 †,*** | 0.000 |
| TUGT (s) | 11.76 ± 1.67 | 11.21 ± 1.48 † | 12.01 ± 1.50 | 10.47 ± 1.51 †,*** | 11.90 ± 1.65 | 11.19 ± 1.29 †,* | 0.041 |
| grip strength (kg) | 18.69 ± 3.50 | 20.60 ± 2.77 *** | 18.44 ± 3.28 | 21.58 ± 3.82 *** | 17.93 ± 3.14 | 21.63 ± 3.26 *** | 0.080 |
| 6 min WT (m) | 355.25 ± 37.02 | 380.06 ± 36.55 *** | 357.75 ± 42.01 | 403.21 ± 47.61 *** | 365.07 ± 42.11 | 392.45 ± 47.49 ** | 0.154 |
| Models | Accuracy | Precision | Recall | F1 |
|---|---|---|---|---|
| Decision Tree (%) | 66.3 ± 11.2 | 65.4 ± 12.8 | 65.3 ± 16.2 | 65.1 ± 12.1 |
| GDB Classifier 1 (%) | 66.7 ± 10.6 | 66.7 ± 13.2 | 65.5 ± 16.3 | 64.5 ± 12.5 |
| XGB Classifier 2 (%) | 68.8 ± 10.9 | 70.5 ± 13.2 | 65.1 ± 15.4 | 66.7 ± 12.2 |
| LGBM Classifier 3 (%) | 69.2 ± 10.6 | 70.4 ± 13.2 | 68.0 ± 15.6 | 68.0 ± 11.9 |
| Extra Tree Classifier (%) | 69.7 ± 10.2 | 70.5 ± 12.7 | 68.1 ± 15.6 | 68.0 ± 12.0 |
| RF Classifier 4 (%) | 70.3 ± 10.5 | 71.5 ± 13.4 | 66.7 ± 16.3 | 67.4 ± 12.2 |
| Logistic Regression (%) | 73.7 ± 10.3 | 74.9 ± 12.5 | 71.3 ± 16.0 | 72.1 ± 11.1 |
| LDA Classifier 5 (%) | 75.3 ± 10.3 | 76.2 ± 12.3 | 73.7 ± 15.1 | 74.0 ± 11.6 |
| Stacking (%) | 75.5 ± 10.0 | 77.1 ± 12.2 | 72.8 ± 15.0 | 73.9 ± 11.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Meng, D.; He, S.; Guo, H.; Tian, Z.; Wei, M.; Yang, G.; Wang, Z. The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly. Int. J. Environ. Res. Public Health 2022, 19, 11063. https://doi.org/10.3390/ijerph191711063
Wang Z, Meng D, He S, Guo H, Tian Z, Wei M, Yang G, Wang Z. The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly. International Journal of Environmental Research and Public Health. 2022; 19(17):11063. https://doi.org/10.3390/ijerph191711063
Chicago/Turabian StyleWang, Ziyi, Deyu Meng, Shichun He, Hongzhi Guo, Zhibo Tian, Meiqi Wei, Guang Yang, and Ziheng Wang. 2022. "The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly" International Journal of Environmental Research and Public Health 19, no. 17: 11063. https://doi.org/10.3390/ijerph191711063
APA StyleWang, Z., Meng, D., He, S., Guo, H., Tian, Z., Wei, M., Yang, G., & Wang, Z. (2022). The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly. International Journal of Environmental Research and Public Health, 19(17), 11063. https://doi.org/10.3390/ijerph191711063







