Coronavirus Disease Pandemic Effect on Medical-Seeking Behaviors Even in One Resource-Competent Community: A Case Controlled Study
Abstract
1. Introduction
2. Materials and Methods
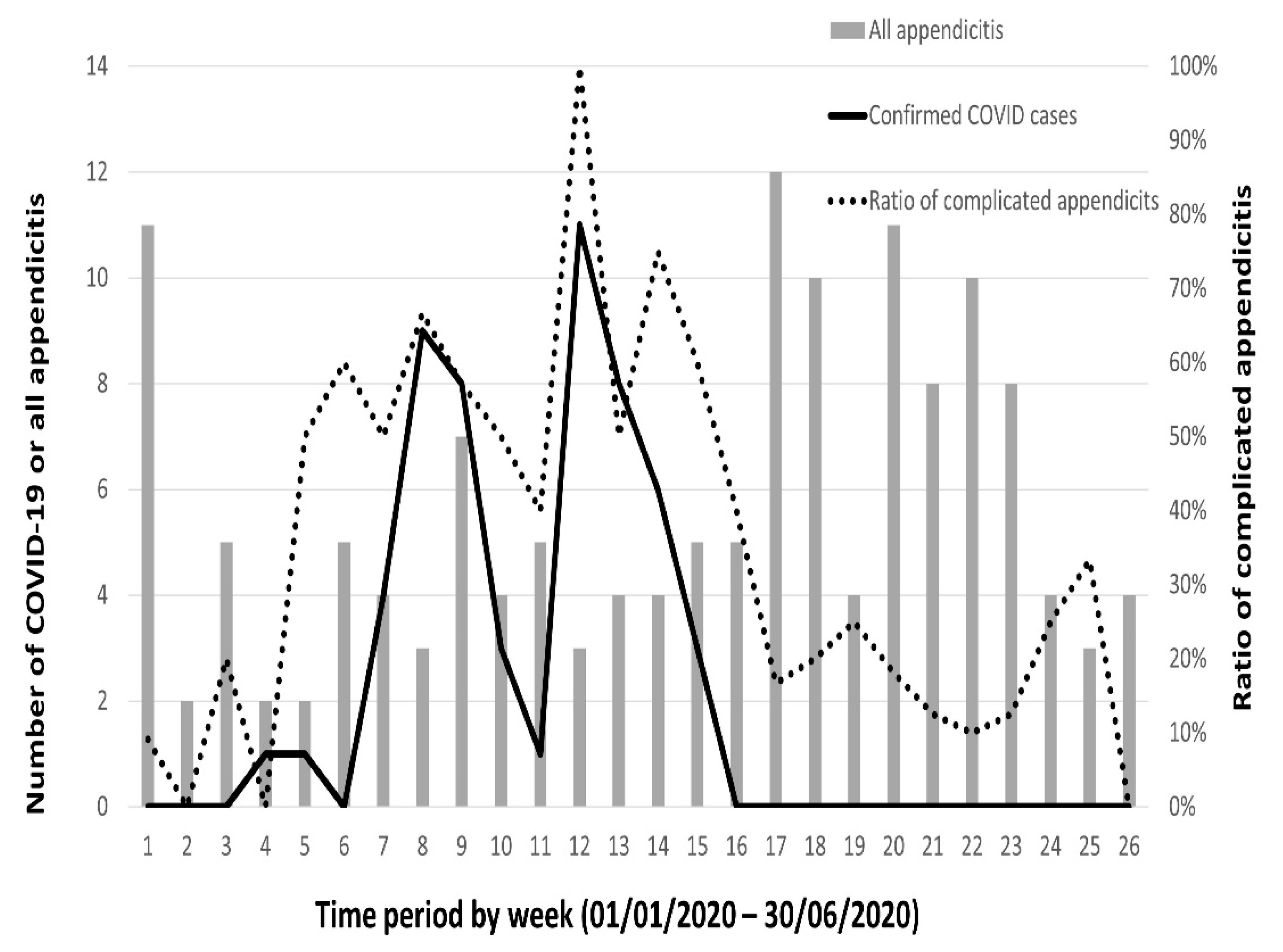
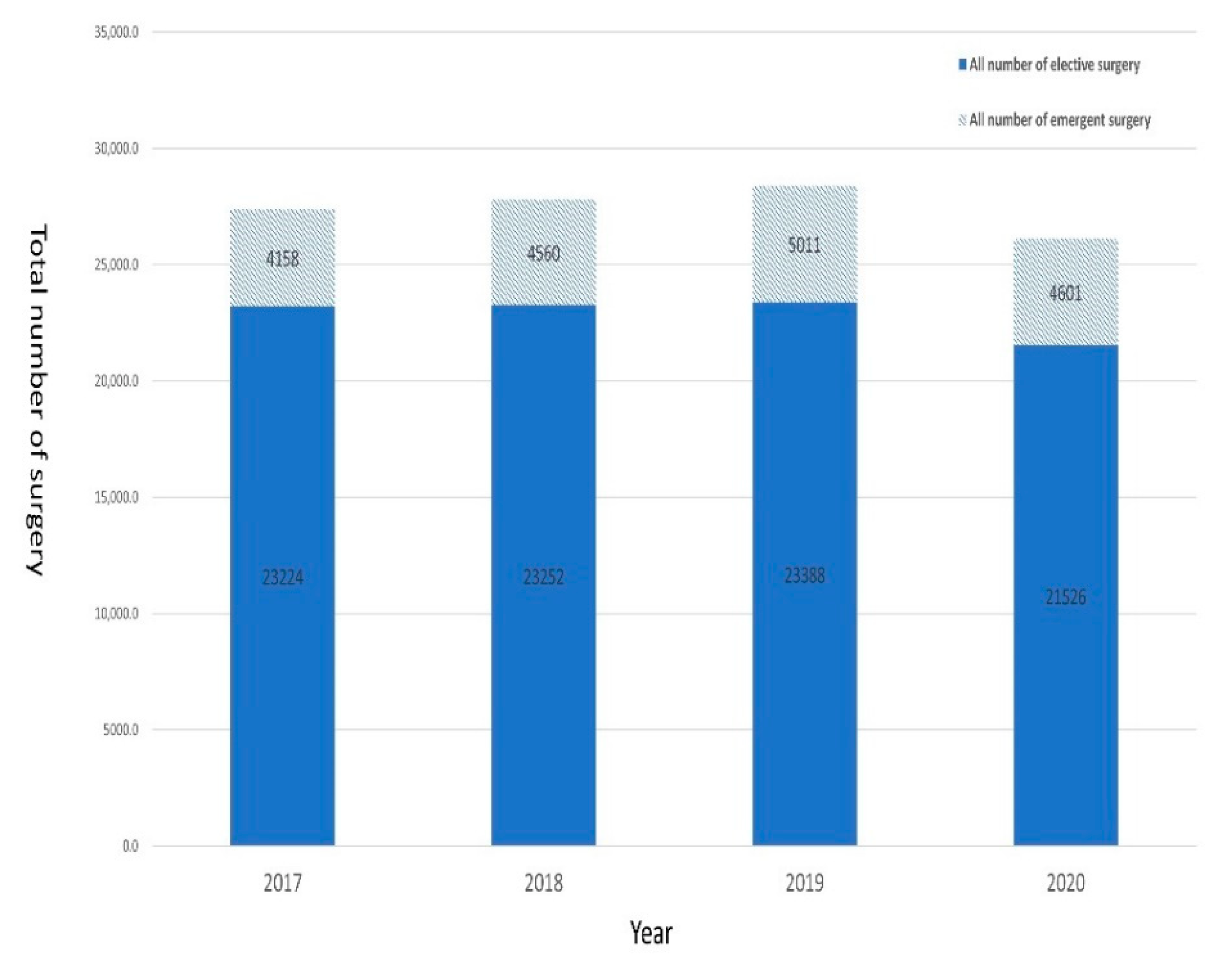
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chrisman, N.J. The health seeking process: An approach to the natural history of illness. Cult. Med. Psychiatry 1977, 1, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Clewley, D.; Rhon, D.; Flynn, T.; Koppenhaver, S.; Cook, C. Health seeking behavior as a predictor of healthcare utilization in a population of patients with spinal pain. PLoS ONE 2018, 13, e0201348. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.M. National health surveys and the behavioral model of health services use. Med. Care 2008, 46, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, D.L.; Martinez, M.E.; Gentleman, J.F.; Sanmartin, C.; Berthelot, J.M. Socioeconomic status and utilization of health care services in Canada and the United States: Findings from a binational health survey. Med. Care 2009, 47, 1136–1146. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Listings of WHO’s Response to COVID-19. Available online: https://www.who.int/news-room/detail/29-06-2020-covidtimeline (accessed on 18 July 2022).
- Boserup, B.; McKenney, M.; Elkbuli, A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020, 38, 1732–1736. [Google Scholar] [CrossRef]
- Addiss, D.G.; Shaffer, N.; Fowler, B.S.; Tauxe, R.V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 1990, 132, 910–925. [Google Scholar] [CrossRef]
- Bhangu, A.; Soreide, K.; Di Saverio, S.; Assarsson, J.H.; Drake, F.T. Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet 2015, 386, 1278–1287. [Google Scholar] [CrossRef]
- Sartelli, M.; Baiocchi, G.L.; Di Saverio, S.; Ferrara, F.; Labricciosa, F.M.; Ansaloni, L.; Coccolini, F.; Vijayan, D.; Abbas, A.; Abongwa, H.K.; et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J. Emerg. Surg. 2018, 13, 19. [Google Scholar] [CrossRef]
- Fisher, J.C.; Tomita, S.S.; Ginsburg, H.B.; Gordon, A.; Walker, D.; Kuenzler, K.A. Increase in Pediatric Perforated Appendicitis in the New York City Metropolitan Region at the Epicenter of the COVID-19 Outbreak. Ann. Surg. 2021, 273, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Burgard, M.; Cherbanyk, F.; Nassiopoulos, K.; Malekzadeh, S.; Pugin, F.; Egger, B. An effect of the COVID-19 pandemic: Significantly more complicated appendicitis due to delayed presentation of patients! PLoS ONE 2021, 16, e0249171. [Google Scholar] [CrossRef]
- Wang, C.J.; Ng, C.Y.; Brook, R.H. Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA 2020, 323, 1341–1342. [Google Scholar] [CrossRef] [PubMed]
- Zangbar, B.; Rhee, P.; Pandit, V.; Hsu, C.H.; Khalil, M.; Okeefe, T.; Neumayer, L.; Joseph, B. Seasonal Variation in Emergency General Surgery. Ann. Surg. 2016, 263, 76–81. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Ho, T.W.; Yen, H.H.; Wu, C.H.; Kuo, T.C.; Yang, C.Y.; Tien, Y.W. Endoscopic Retrograde Biliary Drainage Causes Intra-Abdominal Abscess in Pancreaticoduodenectomy Patients: An Important But Neglected Risk Factor. Ann. Surg. Oncol. 2019, 26, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Summers, J.; Cheng, H.Y.; Lin, H.H.; Barnard, L.T.; Kvalsvig, A.; Wilson, N.; Baker, M.G. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg. Health West Pac. 2020, 4, 100044. [Google Scholar] [CrossRef] [PubMed]
- Tsioplis, C.; Brockschmidt, C.; Sander, S.; Henne-Bruns, D.; Kornmann, M. Factors influencing the course of acute appendicitis in adults and children. Langenbecks Arch. Surg. 2013, 398, 857–867. [Google Scholar] [CrossRef]
- Perez, K.S.; Allen, S.R. Complicated appendicitis and considerations for interval appendectomy. JAAPA 2018, 31, 35–41. [Google Scholar] [CrossRef]
- Schafer, F.M.; Meyer, J.; Kellnar, S.; Warmbrunn, J.; Schuster, T.; Simon, S.; Meyer, T.; Platzer, J.; Hubertus, J.; Seitz, S.T.; et al. Increased Incidence of Perforated Appendicitis in Children During COVID-19 Pandemic in a Bavarian Multi-Center Study. Front. Pediatr. 2021, 9, 683607. [Google Scholar] [CrossRef]
- Orthopoulos, G.; Santone, E.; Izzo, F.; Tirabassi, M.; Perez-Caraballo, A.M.; Corriveau, N.; Jabbour, N. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am. J. Surg. 2021, 221, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
- Saah, F.I.; Amu, H.; Seidu, A.A.; Bain, L.E. Health knowledge and care seeking behaviour in resource-limited settings amidst the COVID-19 pandemic: A qualitative study in Ghana. PLoS ONE 2021, 16, e0250940. [Google Scholar] [CrossRef] [PubMed]
- Boslaugh, S. Encyclopedia of Epidemiology; Sage Publications: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Venegas-Vera, A.V.; Colbert, G.B.; Lerma, E.V. Positive and negative impact of social media in the COVID-19 era. Rev. Cardiovasc. Med. 2020, 21, 561–564. [Google Scholar] [CrossRef] [PubMed]
- Mheidly, N.; Fares, J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J. Public Health Policy 2020, 41, 410–420. [Google Scholar] [CrossRef]
- Kishore, S.P.; Kolappa, K.; Jarvis, J.D.; Park, P.H.; Belt, R.; Balasubramaniam, T.; Kiddell-Monroe, R. Overcoming Obstacles To Enable Access To Medicines For Noncommunicable Diseases In Poor Countries. Health Aff. 2015, 34, 1569–1577. [Google Scholar] [CrossRef][Green Version]
- Wu, J.M.; Ho, T.W.; Tien, Y.W. Correlation Between the Increased Hospital Volume and Decreased Overall Perioperative Mortality in One Universal Health Care System. World J. Surg. 2019, 43, 2194–2202. [Google Scholar] [CrossRef]
- Berlin, N.L.; Dimick, J.B.; Kerr, E.A.; Skolarus, T.A.; Dossett, L.A. Demand for Surgical Procedures Following COVID-19: The Need for Operational Strategies That Optimize Resource Utilization and Value. Ann. Surg. 2020, 272, e272–e274. [Google Scholar] [CrossRef]
- Al-Jabir, A.; Kerwan, A.; Nicola, M.; Alsafi, Z.; Khan, M.; Sohrabi, C.; O’Neill, N.; Iosifidis, C.; Griffin, M.; Mathew, G.; et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice—Part 1. Int. J. Surg. 2020, 79, 168–179. [Google Scholar] [CrossRef]
- Tankel, J.; Keinan, A.; Blich, O.; Koussa, M.; Helou, B.; Shay, S.; Zugayar, D.; Pikarsky, A.; Mazeh, H.; Spira, R.; et al. The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-centre Study. World J. Surg. 2020, 44, 2458–2463. [Google Scholar] [CrossRef]
| Non-Complicated Appendicitis (N = 102) | Complicated Appendicitis (N = 43) | p Value | |
|---|---|---|---|
| Age, year, median (IQR) | 55.5 (36.8, 65.1) | 53.3 (36.4, 65.5) | 0.710 |
| Gender | 0.360 | ||
| Female | 46 (45.1%) | 23 (53.5%) | |
| Male | 56 (54.9%) | 20 (46.5%) | |
| Body mass index, median (IQR) | 23.0 (21.3, 25.2) | 23.5 (21.0, 25.1) | 0.970 |
| Charlson comorbidity index score | 0.140 | ||
| ≤2 | 97 (95.1%) | 38 (88.4%) | |
| >2 | 5 (4.9%) | 5 (11.6%) | |
| Residence in Taipei/New Taipei City | 93 (91.2%) | 38 (88.4%) | 0.690 |
| Duration of symptoms until presentation to ER, n (%) | 0.001 | ||
| ≤48 h | 93 (91.2%) | 33 (79.1%) | |
| >48 h | 9 (8.8%) | 9 (20.9%) | |
| Time from ER visit to surgery (hours), median (IQR) | 11.0 (10.0, 14.0) | 13.0 (11.0, 15.0) | 0.190 |
| Body temperature > 38 degrees Celsius | 27 (26.5%) | 20 (46.5%) | 0.019 |
| White blood count, 109/L, median (IQR) | 11.0 (9.0, 14.8) | 10.2 (7.9, 11.7) | 0.170 |
| Appendectomy performed | 100 (98.0%) | 36 (83.7%) | 0.001 |
| Length of hospital stays (day), median (IQR) | 4.0 (3.0, 7.0) | 5.0 (3.0, 11.0) | 0.080 |
| Control Period (N = 320) | COVID-19 Period (N = 145) | p Value | |
|---|---|---|---|
| Age, year, median (IQR) | 47.9 (33.4, 63.4) | 55.2 (36.8, 65.4) | 0.088 |
| Gender | 0.220 | ||
| Female | 172 (53.8%) | 69 (47.6%) | |
| Male | 148 (46.3%) | 76 (52.4%) | |
| Body mass index, median (IQR) | 23.0 (21.0, 24.7) | 23.1 (21.3, 25.1) | 0.210 |
| Charlson comorbidity index score | 0.690 | ||
| ≤2 | 301 (94.1%) | 135 (93.1%) | |
| >2 | 19 (5.9%) | 10 (6.9%) | |
| Residence in Taipei/New Taipei City | 290 (90.6%) | 131 (90.3%) | 0.920 |
| Duration of symptoms until presentation to ER, n (%) | 0.011 | ||
| ≤48 h | 291 (90.9%) | 120 (82.8%) | |
| >48 h | 29 (9.1%) | 25 (17.2%) | |
| Time from ER visit to surgery (hours), median (IQR) | 10.0 (9.0, 13.0) | 11.0 (10.0, 14.0) | 0.340 |
| Body temperature > 38 degrees Celsius | 129 (40.3%) | 47 (32.4%) | 0.100 |
| White blood count, 109/L, median (IQR) | 9.4 (7.6, 11.6) | 10.8 (8.9, 13.2) | 0.010 |
| Complicated appendicitis | 62 (19.4%) | 43 (29.7%) | 0.014 |
| Length of hospital stays (day), median (IQR) | 4.0 (3.0, 6.0) | 5.0 (3.0, 8.0) | 0.043 |
| Variables | Odds Ratio | 95% CI | p Value |
|---|---|---|---|
| Age (every one-year increment) | 1.01 | 0.99–1.02 | 0.245 |
| Male gender (ref: female) | 0.93 | 0.58–1.50 | 0.793 |
| Body mass index | 0.93 | 0.86–1.01 | 0.132 |
| Charlson comorbidity index score > 2 (ref: ≤2) | 1.38 | 0.58–3.28 | 0.459 |
| Residence in Taipei/New Taipei City | 0.76 | 0.40–1.42 | 0.395 |
| Duration of symptoms until presentation >48 h (ref: ≤48 h) | 1.70 | 1.06–2.36 | 0.044 |
| Body temperature > 38 degrees Celsius | 0.74 | 0.35–1.57 | 0.446 |
| White blood counts | 1.01 | 0.76–2.97 | 0.985 |
| COVID-19 period (ref: control period: 2017–2019) | 1.87 | 1.23–2.52 | 0.008 |
| Variables | Coefficients | 95% Confident Interval | p Value | |
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Age (every one-year increment) | 0.16 | −0.02 | 0.13 | 0.524 |
| Male gender (ref: female) | 0.64 | −1.93 | 3.21 | 0.627 |
| Body mass index | −0.15 | −0.60 | 0.31 | 0.530 |
| Charlson comorbidity index score>2 (ref: ≤2) | 2.51 | 1.25 | 3.16 | <0.001 |
| Residence in Taipei/New Taipei City | −3.05 | −7.4 | 1.29 | 0.168 |
| Complicated appendicitis | 2.10 | 0.92 | 3.31 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, F.; Wu, J.-M.; Lin, Y.-C.; Ho, T.-W.; Lin, H.-L.; Yu, H.-Y.; Lai, I.-R. Coronavirus Disease Pandemic Effect on Medical-Seeking Behaviors Even in One Resource-Competent Community: A Case Controlled Study. Int. J. Environ. Res. Public Health 2022, 19, 10822. https://doi.org/10.3390/ijerph191710822
Wang F, Wu J-M, Lin Y-C, Ho T-W, Lin H-L, Yu H-Y, Lai I-R. Coronavirus Disease Pandemic Effect on Medical-Seeking Behaviors Even in One Resource-Competent Community: A Case Controlled Study. International Journal of Environmental Research and Public Health. 2022; 19(17):10822. https://doi.org/10.3390/ijerph191710822
Chicago/Turabian StyleWang, Fang, Jin-Ming Wu, Yi-Chieh Lin, Te-Wei Ho, Hui-Lin Lin, Hsi-Yu Yu, and I-Rue Lai. 2022. "Coronavirus Disease Pandemic Effect on Medical-Seeking Behaviors Even in One Resource-Competent Community: A Case Controlled Study" International Journal of Environmental Research and Public Health 19, no. 17: 10822. https://doi.org/10.3390/ijerph191710822
APA StyleWang, F., Wu, J.-M., Lin, Y.-C., Ho, T.-W., Lin, H.-L., Yu, H.-Y., & Lai, I.-R. (2022). Coronavirus Disease Pandemic Effect on Medical-Seeking Behaviors Even in One Resource-Competent Community: A Case Controlled Study. International Journal of Environmental Research and Public Health, 19(17), 10822. https://doi.org/10.3390/ijerph191710822







