The Relevance of Internal Working Models of Self and Others for Equine-Assisted Psychodynamic Psychotherapy
Abstract
:1. Introduction
1.1. Animal-Assisted and Equine-Assisted Psychotherapy
1.2. Study Aims
2. Method
2.1. Design
2.2. Participants and Procedure
Inclusion and Exclusion Criteria
2.3. Intervention
2.4. Measurements
2.5. Statistical Analyses
3. Results
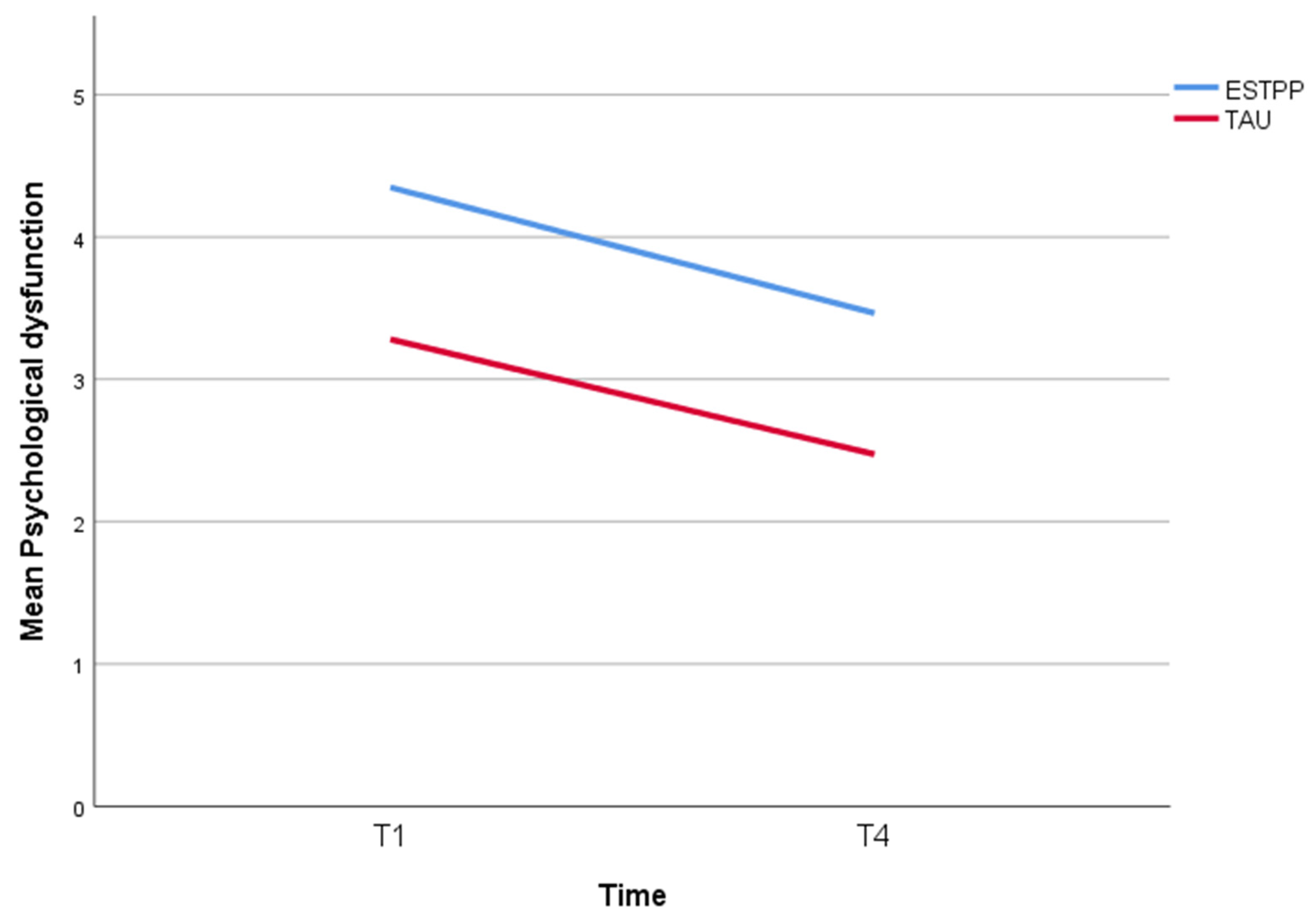
3.1. Difference in Effects of ESTPP and TAU on Psychological Dysfunction
3.2. Estimated Effects over Time for ESTPP
3.3. Estimated Effects over Time of Internal Working Models of Self and Others (MoS, MoO) for ESTPP
4. Discussion
4.1. Internal Working Models Self and Others in ESTPP
4.2. Limitations
4.3. Future Research Aims
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karterud, S.; Pedersen, G.; Bjordal, E.; Brabrand, J.; Friis, S.; Haaseth, Ø.; Haavaldsen, G.; Irion, T.; Leirvåg, H.; Tørum, E.; et al. Day Treatment of Patients with Personality Disorders: Experiences from a Norwegian Treatment Research Network. J. Personal. Disord. 2003, 17, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Leichsenring, F.; Luyten, P.; Hilsenroth, M.J.; Abbass, A.; Barber, J.P.; Keefe, J.R.; Leweke, F.; Rabung, S.; Steinert, C. Psychodynamic Therapy Meets Evidence-Based Medicine: A Systematic Review Using Updated Criteria. Lancet. Psychiatry 2015, 2, 648–660. [Google Scholar] [CrossRef]
- Leichsenring, F.; Leibing, E. Psychodynamic Psychotherapy: A Systematic Review of Techniques, Indications and Empirical Evidence. Psychol. Psychother. Theory Res. Pract. 2007, 80, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Bateman, A. Adversity, Attachment, and Mentalizing. Compr. Psychiatry 2016, 64, 59–66. [Google Scholar] [CrossRef]
- Fonagy, P. The Effectiveness of Psychodynamic Psychotherapies: An Update. World Psychiatry 2015, 14, 137–150. [Google Scholar] [CrossRef]
- Horn, E.K.; Bartak, A.; Meerman, A.M.; Rossum, B.V.; Ziegler, U.M.; Thunnissen, M.; Soons, M.; Andrea, H.; Hamers, E.F.; Emmelkamp, P.M.; et al. Effectiveness of Psychotherapy in Personality Disorders Not Otherwise Specified: A Comparison of Different Treatment Modalities. Clin. Psychol. Psychother. 2015, 22, 426–442. [Google Scholar] [CrossRef]
- Gabbard, G.O.; Westen, D. Rethinking Therapeutic Action. Int. J. Psychoanal. 2003, 84, 823–841. [Google Scholar] [CrossRef]
- Luyten, P.; Fonagy, P. Integrating and Differentiating Personality and Psychopathology: A Psychodynamic Perspective. J. Personal. 2021, 90, 75–88. [Google Scholar] [CrossRef]
- Luyten, P.; Campbell, C.; Fonagy, P. Borderline Personality Disorder, Complex Trauma, and Problems with Self and Identity: A Social-Communicative Approach. J. Personal. 2020, 88, 88–105. [Google Scholar] [CrossRef]
- Van der Kolk, B.A. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma; Penguin Publishing Group, Viking Books: East Rutherford, NJ, USA, 2014. [Google Scholar]
- Wallin, D. Attachment in Psychotherapy; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Perry, B. Examining child maltreatment through a neurodevelopmental lens: Clinical applications of the neurosequential model of therapeutics. J. Loss Trauma 2009, 14, 240–255. [Google Scholar] [CrossRef]
- Siegel, D. The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are, 2nd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Putnam, K.T.; Harris, W.W.; Putnam, F.W. Synergistic Childhood Adversities and Complex Adult Psychopathology. J. Trauma. Stress 2013, 26, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Liotti, G. Attachment Disorganization and the Controlling Strategies: An Illustration of the Contributions of Attachment Theory to Developmental Psychopathology and to Psychotherapy Integration. J. Psychother. Integr. 2011, 21, 232–252. [Google Scholar] [CrossRef]
- Van Dijke, A.; Ford, J.D. Adult Attachment and Emotion Dysregulation in Borderline Personality and Somatoform Disorders. Bord. Personal. Disord. Emot. Dysregul. 2015, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Van Buren, A.; Cooley, E.L. Attachment Styles, View of Self and Negative Affect. N. Am. J. Psychol. 2002, 4, 417–430. [Google Scholar]
- Levy, K.N.; Kivity, Y.; Johnson, B.N.; Gooch, C.V. Adult Attachment as a Predictor and Moderator of Psychotherapy Outcome: A Meta-Analysis. J. Clin. Psychol. 2018, 74, 1996–2013. [Google Scholar] [CrossRef]
- Van Assche, L.; Van de Ven, L.; Vandenbulcke, M.; Luyten, P. Ghosts from the Past? The Association between Childhood Interpersonal Trauma, Attachment and Anxiety and Depression in Late Life. Aging Ment. Health 2019, 24, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Van Dijke, A. Dysfunctional Affect Regulation in Borderline Personality Disorder and in Somatoform Disorder. Eur. J. Psychotraumatol. 2012, 3, 1. [Google Scholar] [CrossRef]
- Karterud, S.; Kongerslev, M.T. Psychotherapy of Personality Disorders Needs an Integrative Theory of Personality. J. Psychother. Integr. 2020, 31, 34. [Google Scholar] [CrossRef]
- Van Dijke, A. The clinical assessment of attachment trauma related self- and affect dysregulation. In Affect Regulation: Conceptual and Clinical Issues; Vingerhoets, A., Nyklicek, I., Denollet, J., Eds.; Springer: New York, NY, USA, 2008; pp. 150–169. [Google Scholar] [CrossRef]
- Ford, J.; Courtois, C. Treatment of Complex Traumatic Stress Disorders in Adults; Guilford: New York, NY, USA, 2020. [Google Scholar]
- Ford, J.D. New findings questioning the construct validity of complex posttraumatic stress disorder (cPTSD): Let’s take a closer look. Eur. J. Psychotraumatol. 2020, 11, 1708145. [Google Scholar] [CrossRef]
- Van Dijke, A.; Hopman, J.A.B.; Ford, J.D. Affect Dysregulation, Adult Attachment Problems, and Dissociation Mediate the Relationship between Childhood Trauma and Borderline Personality Disorder Symptoms in Adulthood. Eur. J. Trauma Dissociation 2018, 2, 91–99. [Google Scholar] [CrossRef]
- Spinazzola, J.; Van der Kolk, B.; Ford, J.D. When Nowhere Is Safe: Interpersonal Trauma and Attachment Adversity as Antecedents of Posttraumatic Stress Disorder and Developmental Trauma Disorder. J. Trauma. Stress 2018, 31, 631–642. [Google Scholar] [CrossRef] [PubMed]
- Van Dijke, A.; Hopman, J.A.B.; Ford, J.D. Affect Dysregulation, Psychoform Dissociation, and Adult Relational Fears Mediate the Relationship between Childhood Trauma and Complex Posttraumatic Stress Disorder Independent of the Symptoms of Borderline Personality Disorder. Eur. J. Psychotraumatol. 2018, 9, 1400878. [Google Scholar] [CrossRef] [PubMed]
- Van Dijke, A.; Ford, J.D.; Frank, L.E.; van der Hart, O. Association of Childhood Complex Trauma and Dissociation with Complex PTSD Symptoms in Adulthood. J. Trauma Dissociation 2015, 16, 428–441. [Google Scholar] [CrossRef] [PubMed]
- Berry, K.; Danquah, A. Attachment-Informed Therapy for Adults: Towards a Unifying Perspective on Practice. Psychol. Psychother. Theory Res. Pract. 2016, 89, 15–32. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R.; Berant, E. An Attachment Perspective on Therapeutic Processes and Outcomes. J. Personal. 2013, 81, 606–616. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R.; Gillath, O.; Nitzberg, R.A. Attachment, Caregiving, and Altruism: Boosting Attachment Security Increases Compassion and Helping. J. Personal. Soc. Psychol. 2005, 89, 817–839. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment Styles Among Young Adults: A Test of a Four-Category Model. J. Personal. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Taylor, P.; Rietzschel, J.; Danquah, A.; Berry, K. Changes in Attachment Representations during Psychological Therapy. Psychother. Res. 2015, 25, 222. [Google Scholar] [CrossRef]
- Zilcha-Mano, S.; Barber, J.P. Learning from Well-Trained and Experienced Dynamic Psychotherapists: Research on the Efficacy of Dynamic Psychotherapy and Its Mechanisms of Change. Contemp. Psychoanal. 2014, 50, 58–88. [Google Scholar] [CrossRef]
- Parish-Plass, N. Animal-Assisted Psychotherapy for Developmental Trauma through the Lens of Interpersonal Neurobiology of Trauma: Creating Connection with Self and Others. J. Psychother. Integr. 2020, 31, 302. [Google Scholar] [CrossRef]
- Percudani, M.; Belloni, G.; Contini, A.; Barbui, C. Monitoring Community Psychiatric Services in Italy: Differences between Patients Who Leave Care and Those Who Stay in Treatment. Br. J. Psychiatry 2002, 180, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Bachi, K.; Terkel, J.; Teichman, M. Equine-Facilitated Psychotherapy for at-Risk Adolescents: The Influence on Self-Image, Self-Control and Trust. Clin. Child Psychol. Psychiatry 2012, 17, 298–312. [Google Scholar] [CrossRef] [PubMed]
- Meyer, L.; Sartori, A. Attachment Theory and Equine-Facilitated Psychotherapy for Vietnam Veterans. Soc. Anim. 2019, 27, 288–306. [Google Scholar] [CrossRef]
- Dietz, T.J.; Davis, D.; Pennings, J. Evaluating Animal-Assisted Therapy in Group Treatment for Child Sexual Abuse. J. Child Sex. Abus. 2012, 21, 665–683. [Google Scholar] [CrossRef] [PubMed]
- Muela, A.; Balluerka, N.; Amiano, N.; Caldentey, M.A.; Aliri, J. Animal-Assisted Psychotherapy for Young People with Behavioural Problems in Residential Care. Clin. Psychol. Psychother. 2017, 24, O1485–O1494. [Google Scholar] [CrossRef] [PubMed]
- Kovács, G.; van Dijke, A.; Noback, I.; Enders-Slegers, M.-J. Integrated Equine-Assisted Short Term Psychodynamic Psychotherapy (EASTPP) equals regular STPP and outperforms in overcoming core problems of patients with personality problems: Interpersonal sensitivity and self esteem. Appl. Neurosci. Ment. Health 2021, 1, 2–20. [Google Scholar] [CrossRef]
- Tedeschi, P. Transforming Trauma: Finding Resiliency and Healing through Animals; Jenkins, M.A., Ed.; Purdue University Press: West Lafayette, IN, USA, 2019. [Google Scholar]
- Trotter, K.S.; Baggerly, J.N. (Eds.) Equine-Assisted Mental Health for Healing Trauma; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Levinson, B. Pet Psychotherapy: Use of Household Pets in the Treatment of Behavior Disorder in Childhood. Psychol. Rep. 1965, 17, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Fine, A.H. Handbook on Animal—Assisted Therapy Theoretical Foundations and Guidelines for Practice, 5th ed.; Academic Press: San Diego, CA, USA, 2019; ISBN 9780123814531. [Google Scholar]
- Balluerka, N.; Muela, A.; Amiano, N.; Caldentey, M.A. Promoting Psychosocial Adaptation of Youths in Residential Care through Animal-Assisted Psychotherapy. Child Abus. Negl. 2015, 50, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Verheggen, T.; Enders-Slegers, M.-J.; Eshuis, J. Enactive Anthrozoology: Toward an Integrative Theoretical Model for Understanding the Therapeutic Relationships between Humans and Animals. Hum. Anim. Interact. Bull. 2017, 5, 13. [Google Scholar]
- International Association of Human Animal Interaction Organizations (IAHAIO). The IAHAIO White Paper: Definitions of Animal Assisted Interventions and Guidelines for Wellness of Animals Involved; IAHAIO: Seattle, WA, USA, 2014. [Google Scholar]
- Schlote, S. Integrating Somatic Experiencing® and Attachment into Equine-Assisted Trauma Recovery. In Equine-Assisted Mental Health for Healing Trauma; Trotter, K., Baggerly, J., Eds.; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Shani, L. Animal-assisted dyadic therapy: A therapy model promoting development of the reflective function in the parent–child bond. Clin. Child Psychol. Psychiatry 2017, 22, 46–58. [Google Scholar] [CrossRef]
- Mormann, F.; Dubois, J.; Kornblith, S.; Milosavljevic, M.; Cerf, M.; Ison, M.; Tsuchiya, N.; Kraskov, A.; Quiroga, R.Q.; Adolphs, R.; et al. A Category-Specific Response to Animals in the Right Human Amygdala. Nat. Neurosci. 2011, 14, 1247–1249. [Google Scholar] [CrossRef] [PubMed]
- Ish-Lev, H.; Amit, R. Elements of Group Psychotherapy Found in Individual Animal assisted Psychotherapy. In Animal-Assisted Psychotherapy: Theory, Issues and Practice; Parish-Plass, N., Ed.; Purdue University Press: West Lafayette, IN, USA, 2013; pp. 145–169. [Google Scholar]
- Siporin, S. Talking Horses: Equine Psychotherapy and Intersubjectivity. Psychodyn. Pract. 2012, 18, 457. [Google Scholar] [CrossRef]
- Lundgren, K.F. What Science Says about Equine-Human Interaction in Equine-Assisted Therapy: An Outline to a Theoretical Framework. In Equine-Assisted Mental Health Interventions: Harnessing Solutions to Common Problems; Routledge: New York, NY, USA, 2019; p. 19. ISBN 9781351673266. [Google Scholar]
- Shultz-Jobe, B.; Choe, K.; Jobe, T. Natural Lifemanship’s Trauma-Focused Equine-Assisted Psychotherapy (EAP). In Equine-Assisted Mental Health for Healing Trauma; Trotter, K., Baggerly, J., Eds.; Routledge: New York, NY, USA, 2018; pp. 154–170. [Google Scholar] [CrossRef]
- Ekholm Fry, N. Equine-Assisted Therapy for Trauma—Accidents. In Equine-Assisted Mental Health for Healing Trauma; Trotter, K., Baggerly, J., Eds.; Routledge: New York, NY, USA, 2018; pp. 125–139. [Google Scholar]
- Kovács, G. Experiential Equine-Assisted Focal Psychodynamic Psychotherapy: Addressing Personality and Attachment in Clients with Chronic Childhood Trauma. In Equine-Assisted Mental Health for Healing Trauma; Trotter, K., Baggerly, J., Eds.; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Williams, P. Equine-Assisted Group Therapy for Adolescent Sexual Trauma Survivors: Development, Implementation, and Outcomes. In Equine-Assisted Mental Health for Healing Trauma; Trotter, K., Baggerly, J., Eds.; Routledge: New York, NY, USA, 2018. [Google Scholar] [CrossRef]
- Gaskill, R.; Perry, B. Child sexual abuse, traumatic experiences, and their impact on the developing brain. In Handbook of Child Sexual Abuse: Identification, Assessment, and Treatment; Goodyear-Brown, P., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2012; pp. 29–47. [Google Scholar] [CrossRef]
- Smith, A.V.; Proops, L.; Grounds, K.; Wathan, J.; McComb, K. Functionally Relevant Responses to Human Facial Expressions of Emotion in the Domestic Horse (Equus caballus). Biol. Lett. 2016, 12. [Google Scholar] [CrossRef]
- Topal, J.; Miklosi, A.; Csanyi, V.; Doka, A. Attachment Behaviour in Dogs (Canis familiaris): A New Application of Ainsworth Strange Situation Test. J. Comp. Psychol. 1998, 112, 219–229. [Google Scholar] [CrossRef] [PubMed]
- VanFleet, R.; Faa-Thompson, T. Animal Assisted Play Therapy; Professional Resources Press: Sarasota, FL, USA, 2017. [Google Scholar]
- Wilson, E. Biophilia; Harvard University Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Panksepp, J. Cross-Species Affective Neuroscience Decoding of the Primal Affective Experiences of Humans and Related Animals. PLoS ONE 2011, 6, e21236. [Google Scholar] [CrossRef]
- Julius, H.; Beetz, A.; Kotrschal, K.; Turner, D.; Uvnas-Moberg, K. Attachment to Pets: An Integrative View of Human-Animal Relationships with Implications for Therapeutic Practice; Hofgreve: Cambridge, MA, USA, 2013; ISBN 9783801724948. [Google Scholar]
- Mikulincer, M.; Shaver, P.R.; Pereg, D. Attachment Theory and Affect Regulation: The Dynamics, Development, and Cognitive Consequences of Attachment-Related Strategies. Motiv. Emot. 2003, 27, 77–102. [Google Scholar] [CrossRef]
- Baljon, M.; Geuzinge, R. Echo’s van Trauma: Slachtoffers Als Daders. Daders Als Slachtoffers [Echoes of Trauma: Victims as Offenders. Offenders as Victims]; Boom Publishers: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Beetz, A.; Uvnäs-Moberg, K.; Julius, H.; Kotrschal, K. Psychosocial and Psychophysiological Effects of Human-Animal Interactions: The Possible Role of Oxytocin. Front. Psychol. 2012, 3, 234. [Google Scholar] [CrossRef] [PubMed]
- Anchin, J.C. Cybernetic Systems, Existential Phenomenology, and Solution-Focused Narrative: Therapeutic Transformation of Negative Affective States through Integratively Oriented Brief Psychotherapy. J. Psychother. Integr. 2003, 13, 334–442. [Google Scholar] [CrossRef]
- Kovács, G.; van Dijke, A.; Enders-Slegers, M.J. Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5661. [Google Scholar] [CrossRef]
- Kazdin, A.E.; Blase, S.L. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspect. Psychol. Sci. 2011, 6, 21–37. [Google Scholar] [CrossRef]
- Zilcha-Mano, S. Major Developments in Methods Addressing for Whom Psychotherapy May Work and Why. Psychother. Res. 2018, 29, 693. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.N.; Ellison, W.D.; Scott, L.N.; Bernecker, S.L. Attachment Style. J. Clin. Psychol. 2011, 67, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Bernheim, D.; Gander, M.; Keller, F.; Becker, M.; Lischke, A.; Mentel, R.; Freyberger, H.J.; Buchheim, A. The role of attachment characteristics in dialectical behavior therapy for patients with borderline personality disorder. Clin. Psychol. Psychother. 2019, 26, 339–349. [Google Scholar] [CrossRef]
- Altmann, U.; Nodop, S.; Dinger, U.; Ehrenthal, J.C.; Schauenburg, H.; Dymel, W.; Willutzki, U.; Strauss, B.M. Differential effects of adult attachment in cognitive-behavioural and psychodynamic therapy in social anxiety disorder: A comparison between a self-rating and an observer rating. Clin. Psychol. Psychother. 2020, 28, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Hards, E.; Ellis, J.; Fisk, J.; Reynolds, S. Negative View of the Self and Symptoms of Depression in Adolescents. J. Affect. Disord. 2020, 262, 143–148. [Google Scholar] [CrossRef]
- Wang, X.; Li, P.; Zheng, L.; Liu, Z.; Cui, G.; Li, L.; Zhang, L.; Hu, Q.; Guo, Y.; Wan, L.; et al. The Passive Recipient: Neural Correlates of Negative Self-View in Depression. Brain Behav. 2022, 12, e2477. [Google Scholar] [CrossRef]
- Vissers, W.; Hutschemaekers, G.; Keijsers, G.; Van der Veld, W.; Hendriks, G.J. Utility of measuring remoralization in addition to symptoms in efficacy research: A preliminary study. Psychother. Res. 2010, 20, 611–618. [Google Scholar] [CrossRef] [PubMed]
- APA. Handboek Voor de Classificatie van Psychische Stoornissen (DSM-5). Dutch Translation of Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2014. [Google Scholar]
- Bartak, A.; Soeteman, D.I.; Verheul, R.; Busschbach, J.J.V. Strengthening the Status of Psychotherapy for Personality Disorders: An Integrated Perspective on Effects and Costs. Can. J. Psychiatry 2007, 52, 803. [Google Scholar] [CrossRef] [Green Version]
- Bartak, A.; Andrea, H.; Spreeuwenberg, M.D.; Ziegler, U.M.; Dekker, J.; Rossum, B.V.; Hamers, E.F.M.; Scholte, W.; Aerts, J.; Busschbach, J.J.V.; et al. Effectiveness of Outpatient, Day Hospital, and Inpatient Psychotherapeutic Treatment for Patients with Cluster B Personality Disorders. Psychother. Psychosom. 2010, 80, 28–38. [Google Scholar] [CrossRef]
- De Beurs, E.; Zitman, F.G. The Brief Symptom Inventory (BSI): Reliability and Validity of a Practical Alternative to SCL-90. Maandbl. Geest. Volksgezond. 2006, 61, 120–141. [Google Scholar]
- De Beurs, E.; den Hollander-Gijsman, M.E.; Helmich, S.; Zitman, F.G. The Tripartite Model for Assessing Symptoms of Anxiety and Depression: Psychometrics of the Dutch Version of the Mood and Anxiety Symptoms Questionnaire. Behav. Res. Ther. 2007, 45, 1609–1617. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R.; Melisaratos, N. The Brief Symptom Inventory: An Introductory Report. Psychol. Med. 1983, 13, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Arrindell, W.; Ettema, J. SCL-90. Manual for a Multidimensional Indicator of Psychopathology; Swets & Zeitlinger: Lisse, The Netherlands, 2003. [Google Scholar]
- Evers, A.; Van Vliet-Mulders, J.; Groot, C. COTAN; Boom Publishers: Amsterdam, The Netherlands, 2005. [Google Scholar]
- van Oudenhoven, J.P.; Hofstra, J. De Hechtingsstijllijst (HSL): Handleiding; University of Groningen: Groningen, The Netherlands, 2005. [Google Scholar]
- Van Oudenhoven, J.P.; Hofstra, J.; Bakker, W. Ontwikkeling En Evaluatie van de Hechtingsstijl Vragenlijst (HSL). Ned. Tijdschr. Psychol. 2003, 58, 95–102. [Google Scholar]
- Mosterman, R.M.; Hofstra, J. Clinical Validation of the Restructured Attachment Styles Questionnaire; University of Groningen: Groningen, The Netherlands, 2015. [Google Scholar]
- Griffin, D.W.; Bartholomew, K. Models of the Self and Other: Fundamental Dimensions Underlying Measures of Adult Attachment. J. Personal. Soc. Psychol. 1994, 67, 430–445. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Luborsky, L.; Rosenthal, R.; Diguer, L.; Andrusyna, T.P.; Berman, J.S.; Levitt, J.T.; Seligman, D.A.; Krause, E.D. The Dodo bird verdict is alive and well—Mostly. Clin. Psychol. 2002, 9, 2–12. [Google Scholar] [CrossRef]
- Wampold, B.E.; Imel, Z.E.; Laska, K.M.; Benish, S.; Miller, S.D.; Fluckiger, C.; del Re, A.C.; Baardseth, T.P.; Budge, S. Determining What Works in the Treatment of PTSD. Clin. Psychol. Rev. 2010, 30, 923–933. [Google Scholar] [CrossRef]
- Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H. The first 10,000 Adult Attachment Interviews: Distributions of adult attachment representations in clinical and non-clinical groups. Attach. Hum. Dev. 2009, 11, 223–263. [Google Scholar] [CrossRef]
- Anestis, M.D.; Anestis, J.C.; Zawilinski, L.L.; Hopkins, T.A.; Lilienfeld, S.O. Equine-Related Treatments for Mental Disorders Lack Empirical Support: A Systematic Review of Empirical Investigations. J. Clin. Psychol. 2014, 70, 1115–1132. [Google Scholar] [CrossRef]
- Luyten, P.; Lowyck, B.; Blatt, S.J. Mechanisms of Change Through the Lens of Two-Polarities Models of Personality Development: State of the Art and New Directions. Psychoanal. Inq. 2017, 37, 179–190. [Google Scholar] [CrossRef]
- Toska, G.A.; Neimeyer, G.J.; Taylor, J.M.; Kavas, B.; Rice, K.G. European Journal of Psychotherapy and Counselling Epistemology and Allegiance: Exploring the Role of Therapists’ Epistemic Commitments on Psychotherapy Outcomes. Eur. J. Psychother. Couns. 2010, 12, 65–75. [Google Scholar] [CrossRef]
- Meyer, B.; Pilkonis, P.; Proietti, J.; Heape, C.; Egan, M. Attachment Styles and Personality Disorders as Predictors of Symptom Course. J. Personal. Disord. 2005, 15, 5. [Google Scholar] [CrossRef]
- Strauss, B.; Kirchmann, H.; Eckert, J.; Lobo-Drost, A.; Marquet, A.; Papenhausen, R.; Mosheim, R.; Biebl, W.; Liebler, A.; Seidler, K.-P.; et al. Attachment characteristics and treatment outcome following inpatient psychotherapy: Results of a multisite study. Psychother. Res. 2007, 16, 579–594. [Google Scholar] [CrossRef]
- Bernecker, S.L.; Constantino, M.J.; Atkinson, L.R.; Bagby, R.M.; Ravitz, P.; McBride, C. Attachment Style as a Moderating Influence on the Efficacy of Cognitive-Behavioral and Interpersonal Psychotherapy for Depression: A Failure to Replicate. Psychotherapy 2016, 53, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Voorendonk, E.M.; De Jongh, A.; Rozendaal, L.; Van Minnen, A. Trauma-focused psychotherapy outcome for complex PTSD patients: Results of an intensive psychotherapy program. Eur. J. Psychotraumatol. 2020, 11. [Google Scholar] [CrossRef]
- Dozier, M. Attachment Organization and Treatment Use for Adults with Serious Psychopathological Disorders. Dev. Psychopathol. 1990, 2, 47–60. [Google Scholar] [CrossRef]
- Vogel, D.L.; Wei, M. Adult Attachment and Help-Seeking Intent: The Mediating Roles of Psychological Distress and Perceived Social Support. J. Couns. Psychol. 2005, 52, 347–357. [Google Scholar] [CrossRef]
- Byrd, K.R.; Patterson, C.L.; Turchik, J.A. Working Alliance as a Mediator of Client Attachment Dimensions and Psychotherapy Outcome. Psychotherapy 2010, 47, 631–636. [Google Scholar] [CrossRef]
- Horowitz, L.M.; Rosenberg, S.E.; Bartholomew, K. Interpersonal Problems, Attachment Styles, and Outcome in Brief Dynamic Psychotherapy. J. Consult. Clin. Psychol. 1993, 61, 549–560. [Google Scholar] [CrossRef]
- Newman, M.G.; Castonguay, L.G.; Jacobson, N.C.; Moore, G.A. Adult Attachment as a Moderator of Treatment Outcome for Generalized Anxiety Disorder: Comparison between Cognitive-Behavioral Therapy (CBT) plus Supportive Listening and CBT plus Interpersonal and Emotional Processing Therapy. J. Consult. Clin. Psychol. 2015, 83, 915–925. [Google Scholar] [CrossRef]
- Griffioen, R.E.; Van der Steen, S.; Verheggen, T.; Enders-Slegers, M.J.; Cox, R. Changes in Behavioural Synchrony during Dog-Assisted Therapy for Children with Autism Spectrum Disorder and Children with Down Syndrome. J. Appl. Res. Intellect. Disabil. 2020, 33, 398–408. [Google Scholar] [CrossRef]
- Zilcha-Mano, S.; Mikulincer, M.; Shaver, P.R. Pets as Safe Havens and Secure Bases: The Moderating Role of Pet Attachment Orientations. J. Res. Personal. 2012, 46, 571–580. [Google Scholar] [CrossRef]
- Dinger, U.; Ehrenthal, J.C.; Nikendei, C.; Schauenburg, H. Change in Self-Esteem Predicts Depressive Symptoms at Follow-up after Intensive Multimodal Psychotherapy for Major Depression. Clin. Psychol. Psychother. 2017, 24, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- Mallinckrodt, B.; Anderson, M.Z.; Choi, G.; Levy, K.N.; Petrowski, K.; Sauer, E.M.; Tishby, O.; Wiseman, H. Pseudosecure vs. individuated-secure client attachment to therapist: Implications for therapy process and outcome. Psychother. Res. 2016, 27, 677–691. [Google Scholar] [CrossRef] [PubMed]
- Payne, P.; Levine, P.A.; Crane-Godreau, M.A. Somatic Experiencing: Using Interoception and Proprioception as Core Elements of Trauma Therapy. Front. Psychol. 2015, 6, 93. [Google Scholar] [CrossRef]
- Fotopoulou, A.; Tsakiris, M. Mentalizing homeostasis: The social origins of interoceptive inference—Replies to Commentaries. Neuropsychoanalysis 2017, 19, 71–76. [Google Scholar] [CrossRef]
| T0 (2 Months before T1, Waiting List ESTPP) | T1 (Start Therapy) | T2 (after 1 Week Intensive Module ESTPP) | T3 (6 Months after Start ESTPP) | T4 (12 Months after Start) | |
|---|---|---|---|---|---|
| ESTPP | BSI, RQ, BDI, ASQ | BSI, RQ, BDI | BSI, RQ, BDI | BSI, RQ, BDI | BSI, RQ, BDI |
| TAU | BSI | (BSI) |
| MoS | MoO | |
|---|---|---|
| Secure | 1 | 1 |
| Fearful | 0 | 0 |
| Dismissive | 1 | 0 |
| Preoccupied | 0 | 1 |
| ESTPP | TAU | |||
|---|---|---|---|---|
| M (SD) | N | M (SD) | N | |
| Age | 37.6 (12.5) | 193 | 30.5 (10.9) | 107 |
| Male | 32 (16.6%) | 29 (27.1%) | ||
| Psychological dysfunction | 4.7 (1.5) | 186 | 3.3 (1.2) | 107 |
| Remoralization | 2.1 (.6) | 180 | ||
| Depression | 24.7 (11.1) | 153 | ||
| Attachment Style ESTPP | ||||
| Secure | 40 (20.2%) | |||
| Preoccupied | 82 (41.4%) | |||
| Dismissive | 37 (18.7%) | |||
| Fearful | 34 (17.2%) |
| ESTPP | TAU | |||||||
|---|---|---|---|---|---|---|---|---|
| M (SD) | N | p | d | M (SD) | N | p | d | |
| Measurement | ||||||||
| T1 | 4.3 (1.4) | 119 | 3.3 (1.2) | 107 | ||||
| T4 | 3.5 (1.6) | 56 | 2.5 (1.2) | 106 | ||||
| ∆, difference in scores, EE (95%CI) | ||||||||
| T4 vs. T1 | −1.3 (−1.6 to −0.1) | <0.001 | 0.9 | −0.8 (−1.1 to −0.5) | <0.001 | 0.7 | ||
| ESTPP vs. TAU | −1.2 (−0.7 to 0.3) | 0.45 | 0.8 | |||||
| Psychological Dysfunction | Remoralization | Depression | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | N | p | M (SD) | N | p | M (SD) | N | p | |
| Measurement | |||||||||
| T0 | 4.7 (1.5) | 186 | 2.1 (0.6) | 180 | 24.7 (11.1) | 153 | |||
| T1 | 4.3 (1.4) | 119 | 2.3 (0.6) | 115 | 22.2 (11.8) | 86 | |||
| T2 | 3.3 (1.4) | 103 | 2.7 (0.7) | 104 | 15.3 (12.0) | 74 | |||
| T3 | 3.2 (1.6) | 115 | 2.6 (0.7) | 113 | 15.5 (11.9) | 91 | |||
| T4 | 3.5 (1.6) | 56 | 2.6 (0.7) | 56 | 16.3 (12.8) | 48 | |||
| ∆, scores compared to T0, EE (95%CI) | |||||||||
| T1 | −0.2 (−0.5 to −0.001) | 0.04 | 0.1(0.1 to 0.2) | 0.003 | −1.6 (−3.6 to 0.5) | 0.14 | |||
| T2 | −1.4 (−1.6 to −1.1) | <0.001 | 0.6 (0.5 to 0.7) | <0.001 | −10.5 (−12.7 to −8.2) | <0.001 | |||
| T3 | −1.5 (−1.8 to −1.3) | <0.001 | 0.5 (0.4 to 0.6) | <0.001 | −10.3 (−12.4 to −8.2) | <0.001 | |||
| T4 | −1.3 (−1.6 to −1.0) | <0.001 | 0.5 (0.4 to 0.6) | <0.001 | −9.3 (−12.1 to −6.6) | <0.001 |
| Psychological Dysfunction | Re-Moralization | Depression | |||||||
|---|---|---|---|---|---|---|---|---|---|
| EE (95%CI) | p | d | EE (95%CI) | p | d | EE (95%CI) | p | d | |
| ∆ for pre-occupied | |||||||||
| T1 | −0.4 (−1 to 0.2) | 0.24 | 0.2 | 0.2 (−0.1 to 0.5) | 0.12 | 0.3 | −1.5 (−6.9 to 3.9) | 0.98 | 0.1 |
| T2 | −1.1 (−1.7 to −0.4) | 0.001 | 0.7 | 0.4 (0.2 to 0.7) | 0.002 | 0.7 | −4.3 (−6.4 to 7.6) | 0.15 | 0.4 |
| T3 | −0.7 (−1.3 to 0) | 0.04 | 0.5 | 0.1 (−0.1 to 0.4) | 0.30 | 0.2 | 0.2 (−5.7 to 6.2) | 0.94 | 0.02 |
| T4 | −0.7 (−1.5 to 0.1) | 0.08 | 0.5 | 0.1 (−0.3 to 0.4) | 0.74 | 0.01 | −2.5 (−9.6 to 4.5) | 0.48 | 0.2 |
| ∆ for fearful | |||||||||
| T1 | −0.3 (−1 to 0.5) | 0.48 | 0.2 | 0.1 (−0.2 to 0.4) | 0.38 | 0.01 | 0 (−6.9 to 6.9) | 0.10 | 0.002 |
| T2 | −0.6 (−1.3 to 0.2) | 0.13 | 0.4 | 0 (−0.3 to 0.3) | 0.10 | 0.002 | −4.8 (−12.2 to 2.6) | 0.21 | 0.4 |
| T3 | −0.6 (−1.3 to 0.1) | 0.09 | 0.4 | 0 (−0.3 to 0.3) | 0.84 | 0.1 | −0.9 (−7.9 to 6.2) | 0.81 | 0.1 |
| T4 | −1 (−1.9 to −0.1) | 0.04 | 0.7 | 0.2 (−0.2 to 0.6) | 0.43 | 0.3 | 0.6 (−7.9 to 9) | 0.90 | 0.1 |
| ∆ for dismissive | |||||||||
| T1 | 0 (−0.7 to 0.7) | 0.98 | 0.01 | 0.1 (−2.4 to 0.4) | 0.70 | 0.2 | 0.1 (−6.4 to 6.6) | 0.99 | 0.01 |
| T2 | −0.7 (−1.4 to 0.1) | 0.07 | 0.5 | 0 (−0.3 to 0.3) | 0.84 | 0.1 | 0.6 (−6.4 to 7.6) | 0.86 | 0.1 |
| T3 | −0.7 (−1.5 to 0) | 0.07 | 0.5 | 0.1 (−0.3 to 0.4) | 0.74 | 0.1 | 0.1 (−7.2 to 7.3) | 0.99 | 0.01 |
| T4 | −1 (−1.9 to −0.1) | 0.04 | 0.7 | −0.1 (−0.4 to 0.3) | 0.74 | 0.2 | −5.2 (−14.3 to 4) | 0.27 | 0.5 |
| ∆ for MoS | |||||||||
| T1 | −0.3 (−0.8 to 0.2) | 0.20 | 0.2 | 0.2 (0 to 0.3) | 0.12 | 0.3 | −0.1 (−5.2 to 3.2) | 0.64 | 0.1 |
| T2 | −0.6 (−1 to −0.8) | 0.02 | 0.4 | 0.2 (0 to 0.4) | 0.02 | 0.02 | −4.6 (−9.1 to −0.1) | 0.04 | 0.4 |
| T3 | −0.3 (−0.8 to 0.2) | 0.19 | 0.2 | 0.2 (0 to 0.4) | 0.06 | 0.3 | 0.1 (−4.3 to 4.5) | 0.96 | 0.01 |
| T4 | −0.4 (−1 to 0.2) | 0.23 | 0.3 | 0.2 (0 to 0.5) | 0.10 | 0.4 | 0.6 (−5 to 6.1) | 0.85 | 0.1 |
| ∆ for MoO | |||||||||
| T1 | 0.2 (−0.3 to 0.6) | 0.45 | 0.1 | −0.1 (−0.2 to 0.2) | 0.63 | 0.1 | 1.2 (−3.2 to 5.7) | 0.59 | 0.1 |
| T2 | 0.1 (−0.4 to 0.6) | 0.65 | 0.1 | −0.3 (−0.5 to −0.1) | 0.008 | 0.5 | 1 (−3.6 to 5.8) | 0.64 | 0.1 |
| T3 | −0.13 (−0.6 to 0.2) | 0.59 | 0.1 | −0.1 (−0.3 to 0.1) | 0.16 | 0.2 | 0 (−4.5 to 4.5) | 10.0 | 0 |
| T4 | −0.47 (−1.1 to 0.2) | 0.15 | 0.3 | 0 (−0.3 to 0.2) | 0.91 | 0.02 | 0.5 (−5.4 to 6.3) | 0.88 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovács, G.; van Dijke, A.; Leontjevas, R.; Enders-Slegers, M.-J. The Relevance of Internal Working Models of Self and Others for Equine-Assisted Psychodynamic Psychotherapy. Int. J. Environ. Res. Public Health 2022, 19, 10803. https://doi.org/10.3390/ijerph191710803
Kovács G, van Dijke A, Leontjevas R, Enders-Slegers M-J. The Relevance of Internal Working Models of Self and Others for Equine-Assisted Psychodynamic Psychotherapy. International Journal of Environmental Research and Public Health. 2022; 19(17):10803. https://doi.org/10.3390/ijerph191710803
Chicago/Turabian StyleKovács, Géza, Annemiek van Dijke, Roeslan Leontjevas, and Marie-José Enders-Slegers. 2022. "The Relevance of Internal Working Models of Self and Others for Equine-Assisted Psychodynamic Psychotherapy" International Journal of Environmental Research and Public Health 19, no. 17: 10803. https://doi.org/10.3390/ijerph191710803
APA StyleKovács, G., van Dijke, A., Leontjevas, R., & Enders-Slegers, M.-J. (2022). The Relevance of Internal Working Models of Self and Others for Equine-Assisted Psychodynamic Psychotherapy. International Journal of Environmental Research and Public Health, 19(17), 10803. https://doi.org/10.3390/ijerph191710803








