Efficacy and Safety of COVID-19 Treatment Using Convalescent Plasma Transfusion: Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Study Selection and Data Extraction
2.3. Meta-Analysis
2.4. Quality Assessment of Included Studies
3. Results and Discussion
3.1. Characteristics of Included Studies
Description of Included Studies
3.2. Bias Risk
3.3. Effective and Safety of COVID-19 Treatment Using CP Transfusion
3.3.1. Reducing All-Cause Mortality on Day 28
3.3.2. Reducing Time to Hospital Discharge
3.3.3. Adverse Events
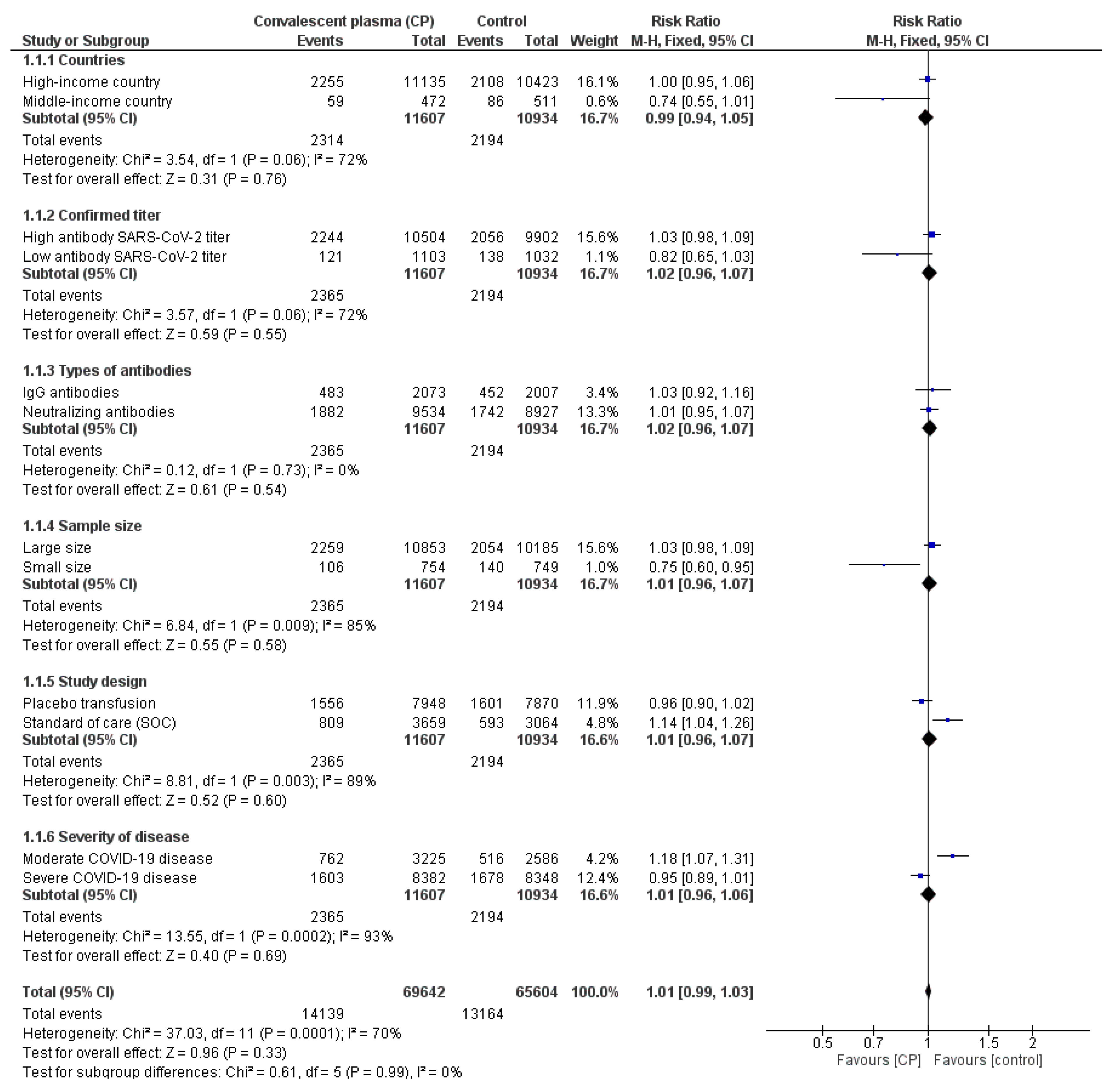
3.3.4. Subgroup Analysis
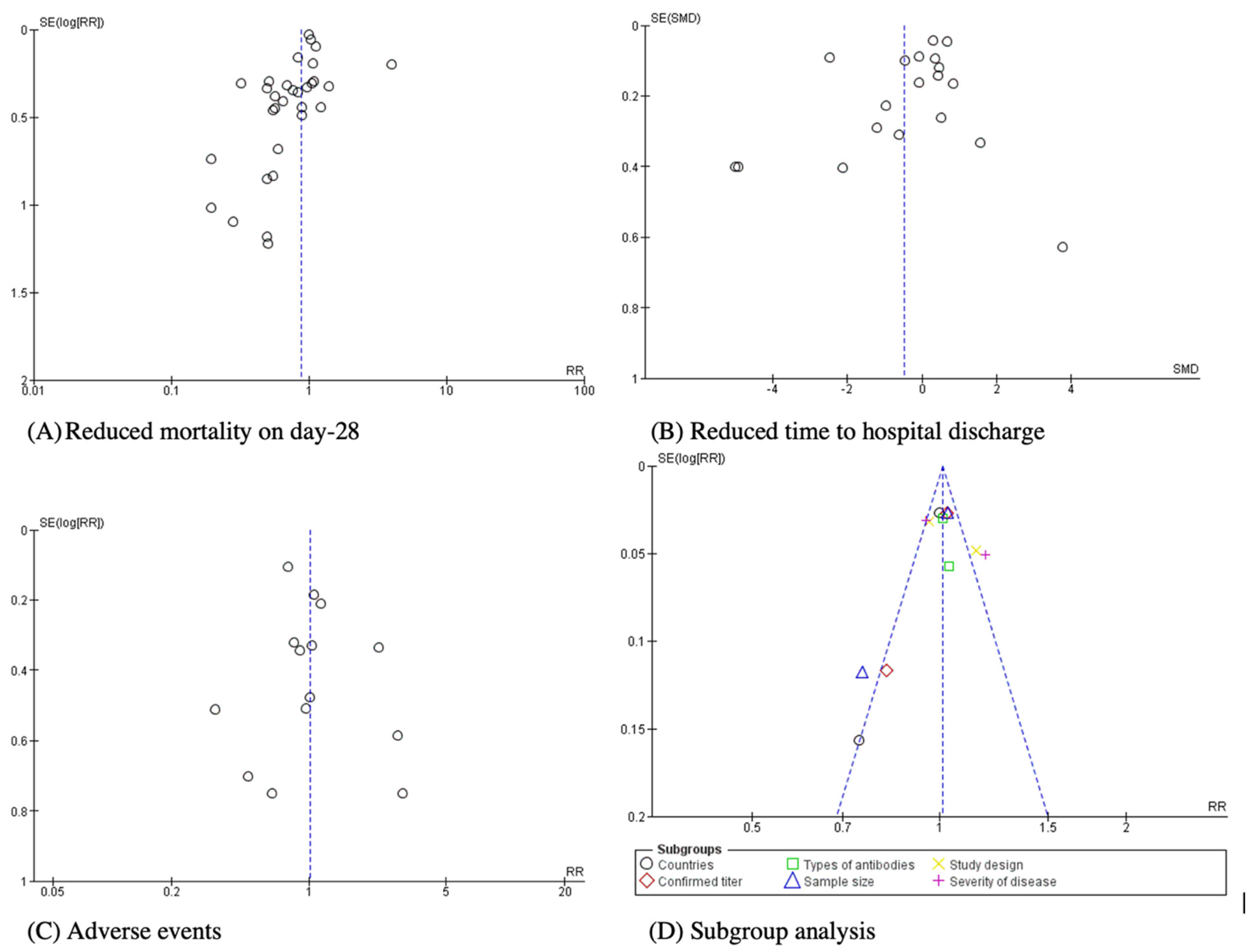
3.4. Analysis Bias
4. Discussion
5. Limitations of Study
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Esakandari, H.; Nabi-Afjadi, M.; Fakkari-Afjadi, J.; Farahmandian, N.; Miresmaeili, S.-M.; Bahreini, E. A comprehensive review of COVID-19 characteristics. Biol. Proced. Online 2020, 22, 19. [Google Scholar] [CrossRef]
- Chen, H.-X.; Chen, Z.-H.; Shen, H.-H. Structure of SARS-CoV-2 and treatment of COVID-19. Acta Physiol. Sin. 2020, 72, 617–630. [Google Scholar]
- Malik, Y.A. Properties of Coronavirus and SARS-CoV-2. Malays. J. Pathol. 2020, 42, 3–11. [Google Scholar] [PubMed]
- Wang, M.; Wu, T.; Zuo, Z.; You, Y.; Yang, X.; Pan, L.; Hu, Y.; Luo, X.; Jiang, L.; Xia, Z. Evaluation of current medical approaches for COVID-19: A systematic review and meta-analysis. BMJ Support. Palliat. Care 2020, 11, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Olivares-Gazca, J.C.; Priesca-Marín, J.M.; Ojeda-Laguna, M.; Garces-Eisele, J.; Soto-Olvera, S.; Palacios-Alonso, A.; Izquierdo-Vega, J.; Chacon-Cano, R.; Arizpe-Bravo, D.; López-Trujillo, M.A.; et al. Infusion of Convalescent Plasma Is Associated With Clinical Improvement in Critically Ill Patients With COVID-19: A Pilot Study. Rev. Investig. Clin. 2020, 72, 159–164. [Google Scholar] [CrossRef]
- Omrani, A.S.; Zaqout, A.; Baiou, A.; Daghfal, J.; Elkum, N.; Alattar, R.A.; Bakdach, D.; Abusriwil, H.; Mostafa, A.M.; Alhariri, B.; et al. Convalescent plasma for the treatment of patients with severe coronavirus disease 2019: A preliminary report. J. Med. Virol. 2020, 3, 1678–1686. [Google Scholar] [CrossRef]
- Abolghasemi, H.; Eshghi, P.; Majid, A.; Ali, A.; Fooladi, I. Clinical efficacy of convalescent plasma for treatment of COVID-19 infections: Results of a multicenter clinical study. Transfus. Apher. Sci. 2020, 59, 102875. [Google Scholar] [CrossRef]
- Agarwal, A.; Mukherjee, A.; Kumar, G.; Chatterjee, P.; Bhatnagar, T.; Malhotra, P. Convalescent plasma in the management of moderate COVID-19 in adults in India: Open label phase II multicentre randomised controlled trial (PLACID Trial). BMJ 2020, 371, m3939. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 10, e1–e34. [Google Scholar]
- Le Ngoc, T.N.; Oh, Y.-K.; Lee, Y.-J.; Lee, Y.-C. Effects of Sparassis crispa in Medical Therapeutics: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Mol. Sci. 2018, 19, 1487. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Ngoc, L.T.N.; Park, D.; Lee, Y.; Lee, Y.-C. Systematic review and meta-analysis of human skin diseases due to particulate matter. Int. J. Environ. Res. Public Health 2017, 14, 1458. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019; ISBN 1119536618. [Google Scholar]
- Kirenga, B.; Byakika-Kibwika, P.; Muttamba, W.; Kayongo, A.; Loryndah, N.O.; Mugenyi, L.; Kiwanuka, N.; Lusiba, J.; Atukunda, A.; Mugume, R.; et al. Efficacy of convalescent plasma for treatment of COVID-19 in Uganda. BMJ Open Respir. Res. 2021, 8, e001017. [Google Scholar] [CrossRef]
- Korley, F.K.; Durkalski-Mauldin, V.; Yeatts, S.D.; Schulman, K.; Davenport, R.D.; Dumont, L.J.; El Kassar, N.; Foster, L.D.; Hah, J.M.; Jaiswal, S.; et al. Early Convalescent Plasma for High-Risk Outpatients with COVID-19. N. Engl. J. Med. 2021, 385, 1951–1960. [Google Scholar] [CrossRef]
- Sullivan, D.J.; Gebo, K.A.; Shoham, S.; Bloch, E.M.; Lau, B.; Shenoy, A.G.; Mosnaim, G.S.; Gniadek, T.J.; Fukuta, Y.; Patel, B. Randomized controlled trial of early outpatient COVID-19 treatment with high-titer convalescent plasma. medRxiv 2021. [Google Scholar] [CrossRef]
- Simonovich, V.A.; Burgos Pratx, L.D.; Scibona, P.; Beruto, M.V.; Vallone, M.G.; Vázquez, C.; Savoy, N.; Giunta, D.H.; Pérez, L.G.; Sánchez, M.D.L.; et al. A Randomized Trial of Convalescent Plasma in COVID-19 Severe Pneumonia. N. Engl. J. Med. 2021, 384, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Pouladzadeh, M.; Safdarian, M.; Eshghi, P.; Abolghasemi, H.; bavani, A.G.; Sheibani, B.; Moradi Choghakabodi, P.; Feghhi, A.; Ghafourian Boroujerdnia, M.; Forouzan, A.; et al. A randomized clinical trial evaluating the immunomodulatory effect of convalescent plasma on COVID-19-related cytokine storm. Intern. Emerg. Med. 2021, 16, 2181–2191. [Google Scholar] [CrossRef]
- O’Donnell, M.R.; Grinsztejn, B.; Cummings, M.J.; Justman, J.E.; Lamb, M.R.; Eckhardt, C.M.; Philip, N.M.; Cheung, Y.K.; Gupta, V.; João, E.; et al. A randomized double-blind controlled trial of convalescent plasma in adults with severe COVID-19. J. Clin. Investig. 2021, 131, e150646. [Google Scholar] [CrossRef] [PubMed]
- Ortigoza, M.B.; Yoon, H.; Goldfeld, K.S.; Troxel, A.B.; Daily, J.P.; Wu, Y.; Li, Y.; Wu, D.; Cobb, G.F.; Baptiste, G.; et al. Efficacy and Safety of COVID-19 Convalescent Plasma in Hospitalized Patients: A Randomized Clinical Trial. JAMA Intern. Med. 2022, 182, 115–126. [Google Scholar] [CrossRef]
- Avendaño-Solà, C.; Ramos-Martínez, A.; Muñez-Rubio, E.; Ruiz-Antorán, B.; de Molina, R.M.; Torres, F.; Fernández-Cruz, A.; Callejas-Díaz, A.; Calderón, J.; Payares-Herrera, C.; et al. Convalescent Plasma for COVID-19: A multicenter, randomized clinical trial. medRxiv 2020. [Google Scholar] [CrossRef]
- Jordans, C.; Gharbharan, A.; Geurts van Kessel, C.H.; Van Kampen, J.J.; Rockx, B.; Haagmans, B.; Swaneveld, F.; Mueller, Y.; Katsikis, P.; Koopmans, M.; et al. Potent neutralizing antibodies for severe COVID-19: A randomized clinical trial. Top. Antivir. Med. 2021, 29, 34. [Google Scholar]
- Baldeón, M.E.; Maldonado, A.; Ochoa-Andrade, M.; Largo, C.; Pesantez, M.; Herdoiza, M.; Granja, G.; Bonifaz, M.; Espejo, H.; Mora, F. Effect of convalescent plasma as complementary treatment in patients with moderate COVID-19 infection. Transfus. Med. 2022, 32, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Bargay-Lleonart, J.; Sarubbo, F.; Arrizabalaga, M.; Guerra, J.M.; Borràs, J.; El Haji, K.; Flexas, M.; Perales, J.; Fernández-Baca, V.; Gallegos, C. Reinforcement of the Standard Therapy with Two Infusions of Convalescent Plasma for Patients with COVID-19: A Randomized Clinical Trial. J. Clin. Med. 2022, 11, 3039. [Google Scholar] [CrossRef] [PubMed]
- Gharbharan, A.; Jordans, C.C.E.; GeurtsvanKessel, C.; den Hollander, J.G.; Karim, F.; Mollema, F.P.N.; Stalenhoef-Schukken, J.E.; Dofferhoff, A.; Ludwig, I.; Koster, A.; et al. Effects of potent neutralizing antibodies from convalescent plasma in patients hospitalized for severe SARS-CoV-2 infection. Nat. Commun. 2021, 12, 3189. [Google Scholar] [CrossRef] [PubMed]
- Avendaño-Solá, C.; Ramos-Martínez, A.; Muñez-Rubio, E.; Ruiz-Antorán, B.; De Molina, R.M.; Torres, F.; Fernández-Cruz, A.; Calderón-Parra, J.; Payares-Herrera, C.; De Santiago, A.D.; et al. A multicenter randomized open-label clinical trial for convalescent plasma in patients hospitalized with COVID-19 pneumonia. J. Clin. Investig. 2021, 131, e152740. [Google Scholar] [CrossRef]
- Millat-Martinez, P.; Gharbharan, A.; Alemany, A.; Rokx, C.; GeurtsvanKessel, C.; Papageourgiou, G.; van Geloven, N.; Jordans, C.; Groeneveld, G.; Swaneveld, F. Convalescent plasma for outpatients with early COVID-19. medRxiv 2021. [Google Scholar] [CrossRef]
- Bégin, P.; Callum, J.; Jamula, E.; Cook, R.; Heddle, N.M.; Tinmouth, A.; Zeller, M.P.; Beaudoin-Bussières, G.; Amorim, L.; Bazin, R.; et al. Convalescent plasma for hospitalized patients with COVID-19: An open-label, randomized controlled trial. Nat. Med. 2021, 27, 2012–2024. [Google Scholar] [CrossRef]
- Libster, R.; Pérez Marc, G.; Wappner, D.; Coviello, S.; Bianchi, A.; Braem, V.; Esteban, I.; Caballero, M.T.; Wood, C.; Berrueta, M.; et al. Early High-Titer Plasma Therapy to Prevent Severe COVID-19 in Older Adults. N. Engl. J. Med. 2021, 384, 610–618. [Google Scholar] [CrossRef]
- Van den Berg, K.; Glatt, T.N.; Vermeulen, M.; Little, F.; Swanevelder, R.; Barrett, C.; Court, R.; Bremer, M.; Nyoni, C.; Swarts, A. Convalescent plasma in the treatment of moderate to severe COVID-19 pneumonia: A randomized controlled trial (PROTECT-Patient Trial). Sci. Rep. 2022, 12, 2552. [Google Scholar] [CrossRef]
- Bajpai, M.; Maheshwari, A.; Dogra, V.; Kumar, S.; Gupta, E.; Saluja, V.; Thomas, S.S.; Trehanpati, N.; Bihari, C.; Agarwal, R. Efficacy of convalescent plasma therapy in the patient with COVID-19: A randomised control trial (COPLA-II trial). BMJ Open 2022, 12, e055189. [Google Scholar] [CrossRef]
- Salazar, E.; Christensen, P.A.; Graviss, E.A.; Nguyen, D.T.; Castillo, B.; Chen, J.; Lopez, B.V.; Eagar, T.N.; Yi, X.; Zhao, P.; et al. Significantly Decreased Mortality in a Large Cohort of Coronavirus Disease 2019 (COVID-19) Patients Transfused Early with Convalescent Plasma Containing High-Titer Anti–Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein IgG. Am. J. Pathol. 2021, 191, 90–107. [Google Scholar] [CrossRef]
- Devos, T.; Van Thillo, Q.; Compernolle, V.; Najdovski, T.; Romano, M.; Dauby, N.; Jadot, L.; Leys, M.; Maillart, E.; Loof, S. Early high antibody titre convalescent plasma for hospitalised COVID-19 patients: DAWn-plasma. Eur. Respir. J. 2022, 59, 2101724. [Google Scholar] [CrossRef]
- Ray, Y.; Paul, S.R.; Bandopadhyay, P.; D’Rozario, R.; Sarif, J.; Raychaudhuri, D.; Bhowmik, D.; Lahiri, A.; Vasudevan, J.S.; Maurya, R. A phase 2 single center open label randomised control trial for convalescent plasma therapy in patients with severe COVID-19. Nat. Commun. 2022, 13, 383. [Google Scholar] [CrossRef] [PubMed]
- Sekine, L.; Arns, B.; Fabro, B.R.; Cipolatt, M.M.; Machado, R.R.G.; Durigon, E.L.; Parolo, E.; Pellegrini, J.A.S.; Viana, M.V.; Schwarz, P. Convalescent plasma for COVID-19 in hospitalised patients: An open-label, randomised clinical trial. Eur. Respir. J. 2022, 59, 2101471. [Google Scholar] [CrossRef] [PubMed]
- Abani, O.; Abbas, A.; Abbas, F.; Abbas, M.; Abbasi, S.; Abbass, H.; Abbott, A.; Abdallah, N.; Abdelaziz, A.; Abdelfattah, M. Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): A randomised controlled, open-label, platform trial. Lancet 2021, 397, 2049–2059. [Google Scholar]
- AlQahtani, M.; Abdulrahman, A.; Almadani, A.; Alali, S.Y.; Al Zamrooni, A.M.; Hejab, A.H.; Conroy, R.M.; Wasif, P.; Otoom, S.; Atkin, S.L.; et al. Randomized controlled trial of convalescent plasma therapy against standard therapy in patients with severe COVID-19 disease. Sci. Rep. 2021, 11, 9927. [Google Scholar] [CrossRef]
- Bar, K.J.; Shaw, P.A.; Choi, G.H.; Aqui, N.; Fesnak, A.; Yang, J.B.; Soto-Calderon, H.; Grajales, L.; Starr, J.; Andronov, M.; et al. A randomized controlled study of convalescent plasma for individuals hospitalized with COVID-19 pneumonia. J. Clin. Investig. 2021, 131, 2–10. [Google Scholar] [CrossRef]
- Bennett-Guerrero, E.; Romeiser, J.L.; Talbot, L.R.; Ahmed, T.; Mamone, L.J.; Singh, S.M.; Hearing, J.C.; Salman, H.; Holiprosad, D.D.; Freedenberg, A.T.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 Convalescent Plasma Versus Standard Plasma in Coronavirus Disease 2019 Infected Hospitalized Patients in New York: A Double-Blind Randomized Trial∗. Crit. Care Med. 2021, 49, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Estcourt, L.J.; Turgeon, A.F.; McQuilten, Z.K.; McVerry, B.J.; Al-Beidh, F.; Annane, D.; Arabi, Y.M.; Arnold, D.M.; Beane, A.; Bégin, P.; et al. Effect of Convalescent Plasma on Organ Support-Free Days in Critically Ill Patients with COVID-19: A Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2021, 326, 1690–1702. [Google Scholar]
- Holm, K.; Lundgren, M.N.; Kjeldsen-Kragh, J.; Ljungquist, O.; Böttiger, B.; Wikén, C.; Öberg, J.; Fernström, N.; Rosendal, E.; Överby, A.K.; et al. Convalescence plasma treatment of COVID-19: Results from a prematurely terminated randomized controlled open-label study in Southern Sweden. BMC Res. Notes 2021, 14, 440. [Google Scholar] [CrossRef]
- Körper, S.; Weiss, M.; Zickler, D.; Wiesmann, T.; Zacharowski, K.; Corman, V.M.; Grüner, B.; Ernst, L.; Spieth, P.; Lepper, P.M.; et al. Results of the CAPSID randomized trial for high-dose convalescent plasma in patients with severe COVID-19. J. Clin. Investig. 2021, 131, e152264. [Google Scholar] [CrossRef] [PubMed]
- Menichetti, F.; Popoli, P.; Puopolo, M.; Alegiani, S.S.; Tiseo, G.; Bartoloni, A.; De Socio, G.V.; Luchi, S.; Blanc, P.; Puoti, M.; et al. Effect of High-Titer Convalescent Plasma on Progression to Severe Respiratory Failure or Death in Hospitalized Patients With COVID-19 Pneumonia A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2136246. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, W.; Hu, Y.; Tong, X.; Zheng, S.; Yang, J.; Kong, Y.; Ren, L.; Wei, Q.; Mei, H.; et al. Effect of Convalescent Plasma Therapy on Time to Clinical Improvement in Patients with Severe and Life-threatening COVID-19: A Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2020, 324, 460–470. [Google Scholar] [CrossRef]
- Alemany, A.; Millat-Martinez, P.; Corbacho-Monné, M.; Malchair, P.; Ouchi, D.; Ruiz-Comellas, A.; Ramírez-Morros, A.; Codina, J.R.; Simon, R.A.; Videla, S. High-titre methylene blue-treated convalescent plasma as an early treatment for outpatients with COVID-19: A randomised, placebo-controlled trial. Lancet Respir. Med. 2022, 10, 278–288. [Google Scholar] [CrossRef]
- Rasheed, A.M.; Fatak, D.F.; Hashim, H.A.; Maulood, M.F.; Kabah, K.K.; Almusawi, Y.A.; Abdulamir, A.S. The therapeutic potential of convalescent plasma therapy on treating critically-ill COVID-19 patients residing in respiratory care units in hospitals in baghdad, Iraq. Infez. Med. 2020, 28, 357–366. [Google Scholar] [PubMed]
- Axfors, C.; Janiaud, P.; Schmitt, A.M.; van’t Hooft, J.; Smith, E.R.; Haber, N.A.; Abayomi, A.; Abduljalil, M.; Abdulrahman, A.; Acosta-Ampudia, Y. Association between convalescent plasma treatment and mortality in COVID-19: A collaborative systematic review and meta-analysis of randomized clinical trials. BMC Infect. Dis. 2021, 21, 1170. [Google Scholar] [CrossRef] [PubMed]
- Gupta, T.; Kannan, S.; Kalra, B.; Thakkar, P. Systematic review and meta-analysis of randomised controlled trials testing the safety and efficacy of convalescent plasma in the treatment of coronavirus disease 2019 (COVID-19): Evidence-base for practise and implications for research. Transfus. Med. 2021, 31, 409–420. [Google Scholar] [CrossRef]
- Kloypan, C.; Saesong, M.; Sangsuemoon, J.; Chantharit, P.; Mongkhon, P. Convalescent plasma for COVID-19: A meta-analysis of clinical trials and real-world evidence. Eur. J. Clin. Investig. 2021, 51, e13663. [Google Scholar] [CrossRef]

 ) RR of individual studies; (◆) RR summary of the comparison.
) RR of individual studies; (◆) RR summary of the comparison.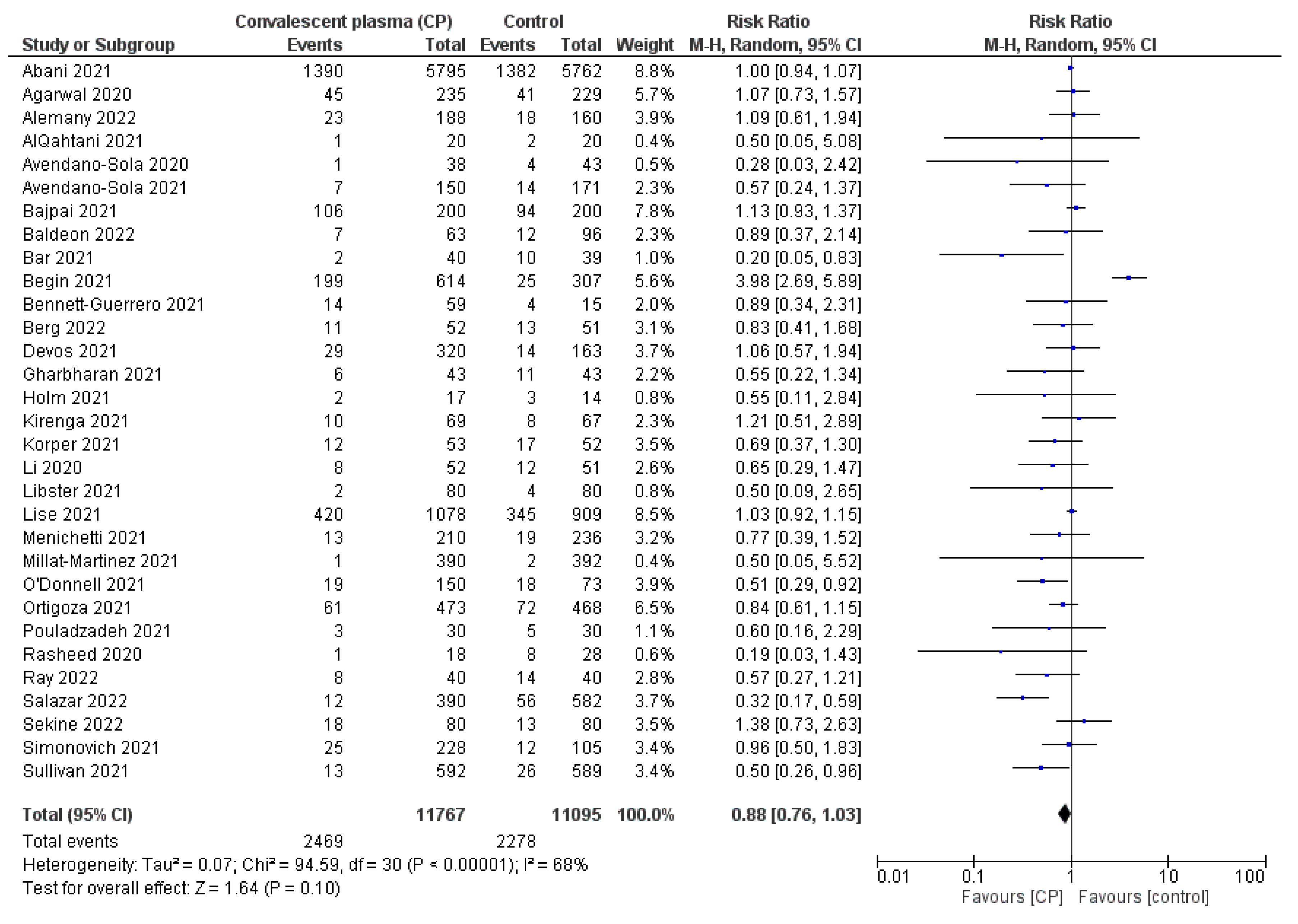
 ) SMD of individual studies; (◆) SMD summary of the comparison.
) SMD of individual studies; (◆) SMD summary of the comparison.
 ) RR of individual studies; (◆) RR summary of the comparison.
) RR of individual studies; (◆) RR summary of the comparison.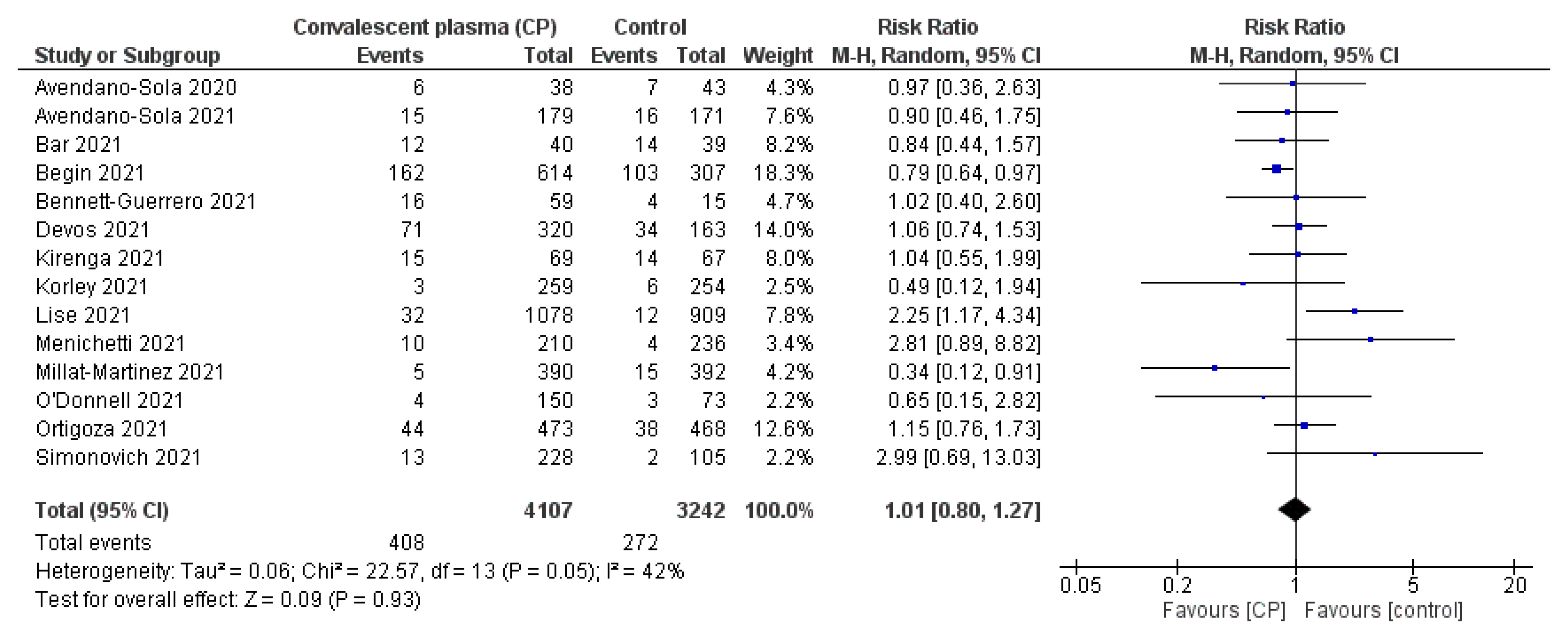
| Author | Region | No. of Patients | Age (Years) | Clinical Design | Treatment Arm | CP Transfusion | Measurement Outcomes | Main Results |
|---|---|---|---|---|---|---|---|---|
| Abani et al. 2021 [36] | United Kingdom | 11558 | ~63 | Open-label RCT | CP transfusion Placebo transfusion | Two units of 275 mL CP on consecutive 2 days Median SARS-CoV-2 neutralizing antibodies titer of 1:400 | All-cause mortality on day 28 Time to hospital discharge | High-titer CP did not improve survival or other prespecified clinical outcomes |
| Agarwal et al. 2020 [8] | India | 464 | ~52 | Open label, parallel arm, phase II, multicenter RCT | CP transfusion plus SOC SOC | Two units of 200 mL CP, transfused 24 h apart SARS-CoV-2 neutralizing antibodies titer > 1:160 | All-cause mortality on day 28 Time to hospital discharge | CP was not associated with a reduction in progression to severe COVID-19 or all-cause mortality |
| Alemany et al. 2022 [45] | Spain | 376 | ~56 | Multicenter, double-blind, placebo-controlled RCT | CP transfusion Placebo transfusion | One unit of 250 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:250 | All-cause mortality on day 28 | CP did not prevent progression from mild to severe illness and did not reduce viral load in outpatients with COVID -19 |
| AlQahtani et al. 2021 [37] | Bahrain | 40 | ~52 | Prospective, open-label RCT | CP transfusion plus SOC SOC | Two units of 200 mL CP over 2 h over 2 successive days Median SARS-CoV-2 neutralizing antibodies titer of 84.95 AU/mL | All-cause mortality on day 28 Time to hospital discharge | There were no significant differences in the primary and secondary outcome measures between the two groups |
| Avendano-sola et al. 2020 [21] | Spain | 81 | ~59 | Multicenter RCT | CP transfusion plus SOC SOC | One unit of 250–300 mL CP SARS-CoV-2 neutralizing antibodies titer > 1:80 | All-cause mortality on day 28 Adverse events | No significant differences were found in secondary endpoints |
| Avendano-sola et al. 2021 [26] | Spain | 350 | ~62 | Open-label RCT | CP transfusion plus SOC SOC | One unit of 250–300 mL CP Median SARS-CoV-2 neutralizing antibodies of 1:157 | All-cause mortality on day 28 Adverse events | CP showed a significant benefit in preventing progression to noninvasive ventilation or high-flow oxygen or death at 28 days. |
| Bajpai et al. 2022 [31] | India | 400 | ~55 | Open-label, multicenter, phase-III RCT | CP transfusion plus SOC SOC | Two units of 250 mL CP on two consecutive days Median SARS-CoV-2 neutralizing antibodies titer ≥ 1:640 | All-cause mortality on day 28 Time to hospital discharge | CP should be transfused in COVID-19 patients along with SOC in the initial 3 days of hospitalization for better clinical outcomes |
| Baldeon et al. 2022 [23] | Ecuador | 158 | ~56 | Double-blind, placebo-controlled RCT | CP transfusion plus SOC SOC | One unit of 100 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:1350 | All-cause mortality on day 28 Time to hospital discharge | CP was safe and its early use could decrease the length of hospital staying and improve respiratory function |
| Bar et al. 2021 [38] | United States | 79 | ~63 | Open-label RCT | CP transfusion plus SOC SOC | Two units of 200 mL CP on the 1st day of administration Median SARS-CoV-2 neutralizing antibodies of 8.189 AU/mL | All-cause mortality on day 28 Adverse events | CP was generally safe and well-tolerated |
| Bargay-Lleonart et al. 2022 [24] | Balearic Islands | 54 | ~59 | Open-label, multicenter RCT | CP transfusion Placebo transfusion | Two units of 300 mL CP within 48 h Median SARS-CoV-2 IgG antibodies titer > 1:160 | Time to hospital discharge | CP was a safe therapy for COVID-19 treatment, and could effectively help restore physical condition earlier than the standard treatment |
| Begin et al. 2021 [28] | Canada | 921 | ~69 | Open-label RCT | CP transfusion plus SOC SOC | One unit of 500 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:160 | All-cause mortality on day 28 Time to hospital discharge Adverse events | CP did not reduce the risk of death at 30 days in hospitalized patients |
| Bennett-Guerrero et al. 2021 [39] | United States | 74 | ~67 | Double-blind RCT | CP transfusion plus SOC SOC | Two units of total volume 480 mL CP Median SARS-CoV-2 neutralizing antibodies titer of 1:526 | All-cause mortality on day 28 Adverse events | CP administration increased antibodies to severe acute respiratory syndrome COVID-19 disease but was not associated with improved outcome |
| Berg et al. 2022 [30] | South Africa | 103 | ~56 | Double-blinded, multicenter RCT | CP transfusion Placebo transfusion | One unit of 200 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:160 | All-cause mortality on day 28 | CP transfusion effectively reduced progression to severe COVID-19 among older people |
| Devos et al. 2022 [33] | Belgium | 483 | ~62 | Open-label, multicenter RCT | CP transfusion plus SOC SOC | Two units of 200–250 mL CP with 36 h Median SARS-CoV-2 neutralizing antibodies titer > 1:320 | All-cause mortality on day 28 Adverse effects | Transfusion of CP with high titer early did not result in a significant improvement in clinical status or reduced mortality |
| Gharbharan et al. 2021 [25] | Netherlands | 86 | ~62 | RCT | CP transfusion plus SOC SOC | Two units of 300 mL CP within 5 days Median SARS-CoV-2 neutralizing antibodies titer of 1:160 | All-cause mortality on day 28 | CP did not improve clinical outcome 10 days after symptom onset |
| Holm et al. 2021 [41] | Netherlands | 31 | ~60 | Open-label RCT | CP transfusion plus SOC SOC | Three units of 200–250 mL CP during 30 min on 3 consecutive days Median SARS-CoV-2 neutralizing antibodies titer of 1:116 | All-cause mortality on day 28 Time to hospital discharge | CP did not improve clinical outcome after the treatment period. |
| Jordans et al. 2021 [22] | Netherlands | 86 | ~63 | Multicenter open-label RCT | CP transfusion plus SOC SOC | One unit of 300 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:160 | Time to hospital discharge | CP treatment did not improve survival or disease course, nor did it alter relevant virological and immunological parameters |
| Kirenga et al. 2021 [14] | Uganda | 136 | ~50 | Open-label RCT | CP transfusion plus SOC SOC | One unit of 300 mL CP. Median IgG anti-SARS-CoV-2 titer of 1:160 | All-cause mortality on day 28 Adverse events | CP did not result in beneficial virological or clinical improvements |
| Korley et al. 2021 [15] | United States | 511 | ~54 | Multicenter, single-blind RCT | CP transfusion Placebo transfusion | One unit 250 mL of CP Median SARS-CoV-2 neutralizing antibodies 2 titer of 1:641 | Time to hospital discharge Adverse events | CP transfusion did not prevent disease progression Adverse effects often occurred with dyspnea in the placebo group compared to CP group |
| Korper et al. 2021 [42] | Germany | 105 | ~62 | Open-label, multicenter RCT | CP transfusion plus SOC SOC | Three units of total volume 846 mL CP Median SARS-CoV-2 neutralizing antibodies titer of 1:160 | Clinical improvement All-cause mortality on day 28 Time to hospital discharge | CP added to standard treatment was not associated with a significant improvement in the primary and secondary outcomes |
| Li et al. 2020 [44] | China | 103 | ~70 | Open-label, multicenter RCT | CP transfusion plus SOC SOC | One unit of 10 mL for the 1st 15 min, then 100 mL per hour with close monitoring SARS-CoV-2 IgG antibodies titer ≥ 1:640 | All-cause mortality on day 28 Time to hospital discharge | CP treatment did not result in a statistically significant improvement in time to clinical improvement within 28 days Interpretation was limited by early termination of the trial |
| Libster et al. 2021 [29] | Argentina | 160 | ~75 | Double-blind, placebo-controlled RCT | CP transfusion Placebo transfusion | One unit of 250 mL CP over a period of 1.5–2 h SARS-CoV-2 IgG antibodies titer > 1:1000 | All-cause mortality on day 28 | Early administration of CP reduced the progression of COVID-19 No solicited adverse events were observed |
| Lise et al. 2021 [40] | United Kingdom | 1988 | ~61 | Multicenter, open-label RCT | CP transfusion plus SOC SOC | Two units of total volume 250 mL CP Median SARS-CoV-2 IgG antibodies titer of 1:160 | All-cause mortality on day 28 Time to hospital discharge Adverse events | Only 1 event was considered to be possibly or probably related to convalescent plasma CP had a low likelihood of providing improvement in the number of organ support-free days |
| Menichetti et al. 2021 [43] | Italia | 447 | ~64 | Open-label RCT | CP transfusion plus SOC SOC | Three units of 200 mL CP over a period of 2 h daily SARS-CoV-2 neutralizing antibodies titer ≥1:160 | All-cause mortality on day 28 Adverse events | CP did not reduce the progression to respiratory failure or death within 30 days among these patients vs. those receiving standard treatment |
| Millat-Martinez et al. 2021 [27] | Spain | 782 | ~58 | Two-double blind RCT | CP transfusion plus SOC SOC | One unit of 300 mL CP Median SARS-CoV-2 neutralizing antibodies titer > 1:320 | All-cause mortality on day 28 Adverse events | Treatment with CP did not improve the outcome of COVID-19 patients |
| O’Donnell et al. 2021 [19] | United States | 223 | ~70 | Double-blind RCT | CP transfusion Placebo transfusion | One unit of 300 mL CP Median SARS-CoV-2 neutralizing antibodies titer of 1:160 | All-cause mortality on day 28 Time to hospital discharge Adverse events | No significant improvement in the clinical scale at day 28 CP was associated with significantly improved survival |
| Ortigoza et al. 2021 [20] | United States | 941 | ~63 | Double-blind, placebo-controlled RCT | CP transfusion Placebo transfusion | One unit of 250 mL CP within 24 h Median SARS-CoV-2 neutralizing antibodies titer of 1:175 | All-cause mortality on day 28 Adverse events | CP did not meet the prespecified outcomes for CP efficacy. The high-titer CP may have benefited participants early in pandemic |
| Pouladzadeh et al. 2021 [18] | Iran | 60 | ~63 | Parallel-group, single-blind, and RCT | CP transfusion plus SOC SOC | One unit of 500 mL CP on the admission day Median SARS-CoV-2 IgG antibodies titer > 1:160 | All-cause mortality on day 28 Time to hospital discharge | CP therapy did not have any serious side effects on patients CP did not considerably affect the mortality rate |
| Rasheed et al. 2020 [46] | Iraq | 49 | ~60 | Open-label RCT | CP transfusion plus SOC SOC | One unit of 400 mL CP over 2 h SARS-CoV-2 IgG antibodies titer ≥ 1:160 | All-cause mortality on day 28 Time to hospital discharge | CP therapy was an effective therapy if there were donors with high level of SARS-CoV-2 antibodies, and if recipients were at their early stage of critical illness |
| Ray et al. 2022 [34] | India | 80 | ~60 | Open label, single center, phase II RCT | CP transfusion plus SOC SOC | Two units of 200 mL CP on 2 consecutive days Median SARS-CoV-2 neutralizing antibodies titer of 1:250 | All-cause mortality on day 28 | No adverse effect was reported with CP treatment. The CP treatment did not improve the survival of patients |
| Salazar et al. 2021 [32] | United States | 903 | ~65 | Open-label RCT | CP transfusion Placebo transfusion | Two units of 300 mL CP within 74 h Median SARS-CoV-2 neutralizing antibodies titer > 1:1350 | All-cause mortality on day 28 | CP transfusion of COVID-19 patients soon after hospitalization with high-titer anti-spike protein RBD IgG present in convalescent plasma significantly reduced mortality |
| Sekine et al. 2022 [35] | Brazil | 160 | ~60.5 | Open-label, parallel RCT | CP transfusion plus SOC SOC | Two units of 300 mL CP within 48 h Median SARS-CoV-2 neutralizing antibodies titer of 1:320 | All-cause mortality on day 28 Time to hospital discharge | CP with SOC did not result in a higher proportion of clinical improvement on day 28 in hospitalized patients |
| Simonovich et al. 2021 [17] | Argentina | 333 | ~62 | Open-label, RCT | CP transfusion Placebo transfusion | One unit of a median 500 mL CP Median SARS-CoV-2 neutralizing antibodies titer of 1:3200 | All-cause mortality on day 28 Time to hospital discharge Adverse events | At day 30, no significant difference was noted between 2 groups Adverse events and serious adverse events were similar in the two group |
| Sullivan et al. 2021 [16] | United States | 1225 | ~44 | Multicenter, double-blind RCT | CP transfusion Placebo transfusion | One unit of 250 mL CP Median SARS-CoV-2 IgG antibodies titer > 1:160 | All-cause mortality on day 28 | High-titer CP was an effective early outpatient COVID-19 treatment with the advantages of low cost, wide availability, and rapid resilience |
| References | Random Sequence Generation | Allocation Concealment | Selective Reporting | Blinding of Participants | Blinding of Outcome Assessment | Incomplete Outcome Data |
|---|---|---|---|---|---|---|
| Abani et al. 2021 [36] | ||||||
| Agarwal et al. 2020 [8] | ||||||
| Alemany et al. 2022 [45] | ||||||
| AlQahtani et al. 2021 [37] | ||||||
| Avendano-sola et al. 2020 [21] | ||||||
| Avendano-sola et al. 2021 [26] | ||||||
| Bajpai et al. 2022 [31] | ||||||
| Baldeon et al. 2022 [23] | ||||||
| Bar et al. 2021 [38] | ||||||
| Bargay-Lleonart et al. 2022 [24] | ||||||
| Begin et al. 2021 [28] | ||||||
| Bennett-Guerrero et al. 2021 [39] | ||||||
| Berg et al. 2022 [30] | ||||||
| Devos et al. 2022 [33] | ||||||
| Gharbharan et al. 2021 [25] | ||||||
| Holm et al. 2021 [41] | ||||||
| Jordans et al. 2021 [22] | ||||||
| Kirenga et al. 2021 [14] | ||||||
| Korley et al. 2021 [15] | ||||||
| Korper et al. 2021 [42] | ||||||
| Li et al. 2020 [44] | ||||||
| Libster et al. 2021 [29] | ||||||
| Lise et al. 2021 [40] | ||||||
| Menichetti et al. 2021 [43] | ||||||
| Millat-Martinez et al. 2021 [27] | ||||||
| O’Donnell et al. 2021 [19] | ||||||
| Ortigoza et al. 2021 [20] | ||||||
| Pouladzadeh et al. 2021 [18] | ||||||
| Rasheed et al. 2020 [46] | ||||||
| Ray et al. 2022 [34] | ||||||
| Salazar et al. 2021 [32] | ||||||
| Sekine et al. 2022 [35] | ||||||
| Simonovich et al. 2021 [17] | ||||||
| Sullivan et al. 2021 [16] | ||||||
| Total low risk of bias (%) | 73.5 | 79.4 | 82.4 | 82.4 | 79.4 | 79.4 |
| Total high risk of bias (%) | 2.9 | 11.8 | 5.9 | 5.9 | 8.8 | 17.7 |
| Total uncertain risk of bias (%) | 23.6 | 8.8 | 11.7 | 11.7 | 11.8 | 2.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-J.; Lee, J.-H.; Cho, Y.; Ngoc, L.T.N.; Lee, Y.-C. Efficacy and Safety of COVID-19 Treatment Using Convalescent Plasma Transfusion: Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 10622. https://doi.org/10.3390/ijerph191710622
Lee H-J, Lee J-H, Cho Y, Ngoc LTN, Lee Y-C. Efficacy and Safety of COVID-19 Treatment Using Convalescent Plasma Transfusion: Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2022; 19(17):10622. https://doi.org/10.3390/ijerph191710622
Chicago/Turabian StyleLee, Hyun-Jun, Jun-Hyeong Lee, Yejin Cho, Le Thi Nhu Ngoc, and Young-Chul Lee. 2022. "Efficacy and Safety of COVID-19 Treatment Using Convalescent Plasma Transfusion: Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 19, no. 17: 10622. https://doi.org/10.3390/ijerph191710622
APA StyleLee, H.-J., Lee, J.-H., Cho, Y., Ngoc, L. T. N., & Lee, Y.-C. (2022). Efficacy and Safety of COVID-19 Treatment Using Convalescent Plasma Transfusion: Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health, 19(17), 10622. https://doi.org/10.3390/ijerph191710622






