Depression, Anxiety and Quality of Life among Online Responders in Poland: A Cross-Sectional Study Covering Four Waves of the COVID-19 Pandemic
Abstract
:1. Introduction
- Following adaptation to the situation and more lenient restrictions, the intensity of anxiety and depressive disorders during the fourth wave of infections was less severe than in the previous pandemic waves;
- Women and youth were more prone to mental disorders during the pandemic;
- The economic situation is an important predictor of mental health during the pandemic.
2. Materials and Methods
2.1. Methods
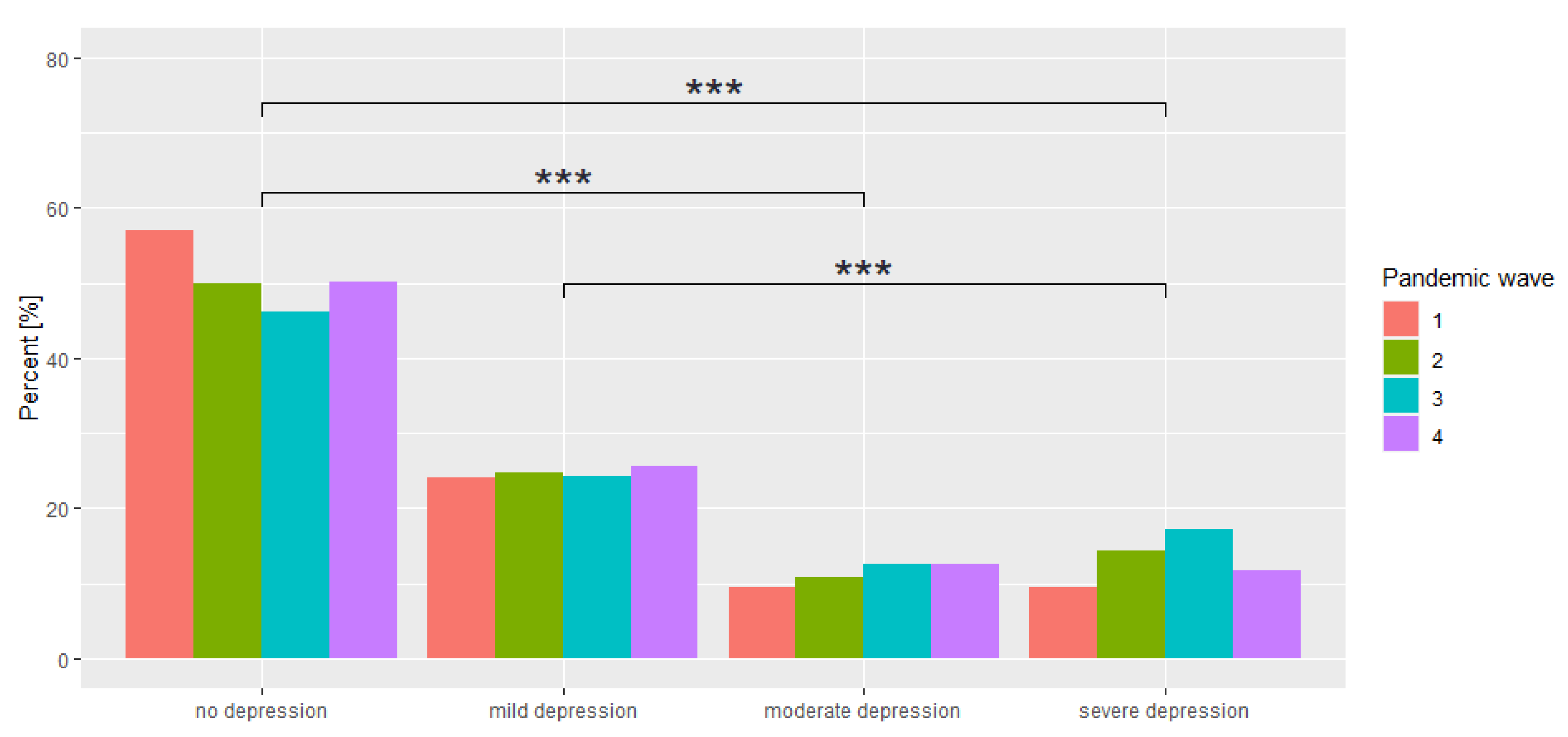
- Beck Depression Inventory (BDI) is a commonly used tool to measure depression. It consists of 21 questions, with responses on a 0–3 scale. Interpretation of the tool is based on the summed point value where the following cut-off points were applied: 0–11—no depression, 12–26 points—mild depression; 27–49—moderate depression; and 50–63—severe depression [37,38];
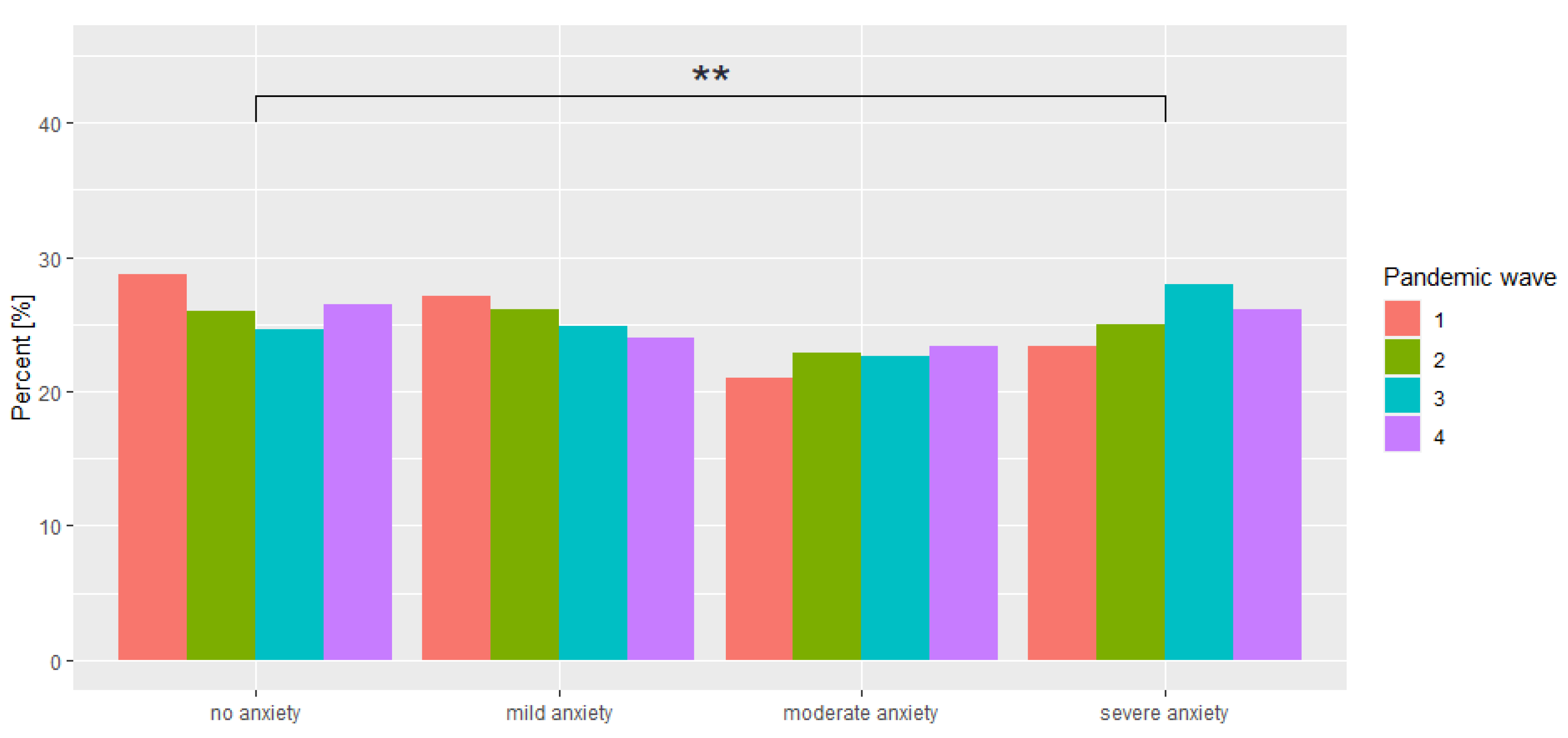
- Generalised Anxiety Disorder Assessment (GAD-7) is a psychometric tool for assessing anxiety. The tool consists of 7 questions based on a 4-grade Likert scale, where respondents rate the frequency of occurrence of a given psychological state over the past 14 days (0—does not occur, 1—a few days, 2—more than half the time, 3—almost always). The analysis is based on summed scores, with cut-off points of 5, 10 and 15 indicating the presence of mild, moderate and severe anxiety, respectively [39];
- Manchester Short Assessment of Quality of Life (MANSA) is a commonly used psychometric tool for the subjective assessment of the quality of life by evaluating 16 aspects of life. When creating the survey, questions based on a 7-point Likert scale were used (1—could not be worse, 7—could not be better). The higher the total score, the higher the quality of life is assessed [40,41].
2.2. Participants
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Group
3.2. Analysis of BDI, GAD-7 and MANSA for Each Wave of the COVID-19 Pandemic
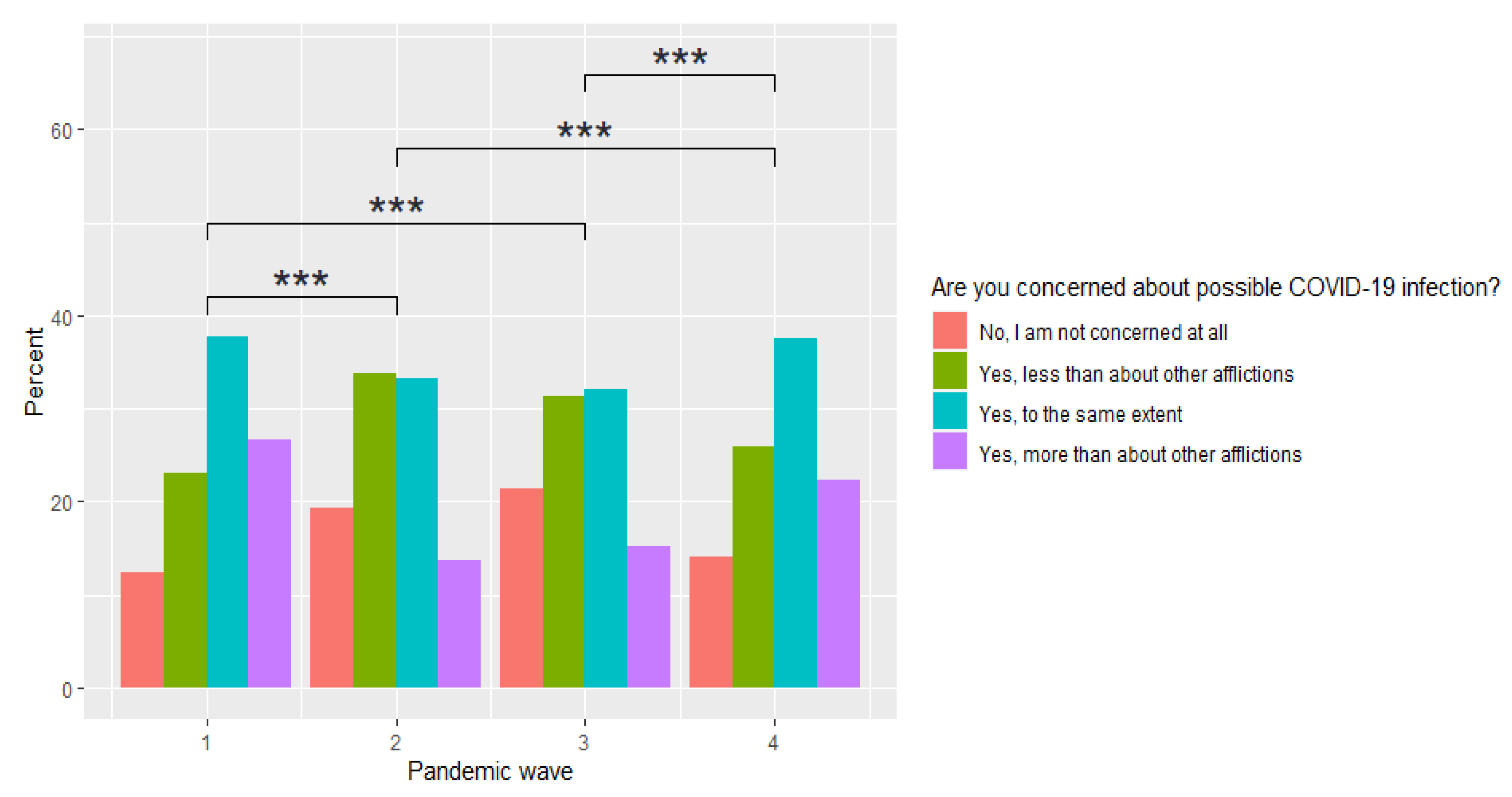
3.3. Subjective Experience of Anxiety about Contracting COVID-19, and Being Quarantined or Infected by a Neighbour
3.4. The Influence of Sociodemographic Variables on the Mean Scores of BDI, GAD-7 and MANSA
3.5. The Relationship between GAD-7, BDI and MANSA Scales
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, K.; et al. A Longitudinal Study on the Mental Health of General Population during the COVID-19 Epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Andrés, C.; Piñana, M.; Borràs-Bermejo, B.; González, A.; García-Cehic, D.; Esperalba, J.; Rando, A.; Zules-Oña, G.; Campos, C.; Codina, M.G. A Year Living with SARS-CoV-2: An Epidemiological Overview of Viral Lineage Circulation by Whole- Genome Sequencing in Barcelona City (Catalonia Spain). Emerg. Microbes Infect. 2022, 11, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Suwono, B.; Steffen, A.; Schweickert, B.; Schönfeld, V.; Brandl, M.; Sandfort, M.; Willrich, N.; Eckmanns, T.; Haller, S. SARS-CoV-2 Outbreaks in Hospitals and Long-Term Care Facilities in Germany: A National Observational Study. Lancet Reg. Health-Eur. 2022, 14, 100303. [Google Scholar] [CrossRef] [PubMed]
- Cui, Z.; Liu, P.; Wang, N.; Wang, L.; Fan, K.; Zhu, Q.; Wang, K.; Chen, R.; Feng, R.; Jia, Z. Structural and Functional Characterizations of Infectivity and Immune Evasion of SARS-CoV-2 Omicron. Cell 2022, 185, 860–871.e13. [Google Scholar] [CrossRef]
- Campbell, F.; Archer, B.; Laurenson-Schafer, H.; Jinnai, Y.; Konings, F.; Batra, N.; Pavlin, B.; Van Kerkhove, M.D.; Jombart, T.; Morgan, O. Increased Transmissibility and Global Spread of SARS- CoV-2 Variants of Concern as at June 2021. Eurosurveillance 2021, 26, 1–6. [Google Scholar] [CrossRef]
- Ministry of Health. Strategy to Combat the COVID-19 Pandemic. Winter/Spring 2022; Ministry of Health: Warsaw, Poland, 2022.
- Fisman, D.N.; Tuite, A.R. Age-Specific Changes in Virulence Associated with SARS-CoV-2 Variants of Concern. Clin. Infect. Dis. 2022. [Google Scholar] [CrossRef]
- Babicki, M.; Bogudzińska, B.; Kowalski, K.; Mastalerz-Migas, A. Anxiety and Depressive Disorders and Quality of Life Assessment of Poles-A Study Covering Two Waves of the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 704248. [Google Scholar] [CrossRef]
- Elliott, P.; Haw, D.; Wang, H.; Eales, O.; Walters, C.E.; Ainslie, K.E.C.; Atchison, C.; Fronterre, C.; Diggle, P.J.; Page, A.J.; et al. Exponential Growth, High Prevalence of SARS-CoV-2, and Vaccine Effectiveness Associated with the Delta Variant. Science 2021, 374, eabl9551. [Google Scholar] [CrossRef]
- Planas, D.; Veyer, D.; Baidaliuk, A.; Staropoli, I.; Guivel-Benhassine, F.; Rajah, M.M.; Planchais, C.; Porrot, F.; Robillard, N.; Puech, J. Reduced Sensitivity of SARS-CoV-2 Variant Delta to Antibody Neutralization. Nature 2021, 596, 276–280. [Google Scholar] [CrossRef]
- Wilson, J.M.; Lee, J.; Shook, N.J. COVID-19 Worries and Mental Health: The Moderating Effect of Age. Aging Ment. Health 2021, 25, 1289–1296. [Google Scholar] [CrossRef]
- Manca, R.; De Marco, M.; Venneri, A. The Impact of COVID-19 Infection and Enforced Prolonged Social Isolation on Neuropsychiatric Symptoms in Older Adults with and without Dementia: A Review. Front. Psychiatry 2020, 11, 585540. [Google Scholar] [CrossRef]
- Cénat, J.M.; Felix, N.; Blais-Rochette, C.; Rousseau, C.; Bukaka, J.; Derivois, D.; Noorishad, P.-G.; Birangui, J.-P. Prevalence of Mental Health Problems in Populations Affected by the Ebola Virus Disease: A Systematic Review and Meta-Analysis. Psychiatry Res. 2020, 289, 113033. [Google Scholar] [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and Associated Psychological Problems. Asian J. Psychiatry 2020, 51, 102092. [Google Scholar] [CrossRef]
- Olagoke, A.A.; Olagoke, O.O.; Hughes, A.M. Exposure to Coronavirus News on Mainstream Media: The Role of Risk Perceptions and Depression: COVID-19 News, Risk Perceptions and Depression. Br. J. Health Psychol. 2020, 25, 865–874. [Google Scholar] [CrossRef]
- Gambin, M.; Sękowski, M.; Woźniak-Prus, M.; Wnuk, A.; Oleksy, T.; Cudo, A.; Hansen, K.; Huflejt-Łukasik, M.; Kubicka, K.; Łyś, A.E. Generalized Anxiety and Depressive Symptoms in Various Age Groups during the COVID-19 Lockdown in Poland. Specific Predictors and Differences in Symptoms Severity. Compr. Psychiatry 2021, 105, 152222. [Google Scholar] [CrossRef]
- Salfi, F.; Lauriola, M.; Amicucci, G.; Corigliano, D.; Viselli, L.; Tempesta, D.; Ferrara, M. Gender-Related Time Course of Sleep Disturbances and Psychological Symptoms during the COVID-19 Lockdown: A Longitudinal Study on the Italian Population. Neurobiol. Stress 2020, 13, 100259. [Google Scholar] [CrossRef]
- Avena, N.M.; Simkus, J.; Lewandowski, A.; Gold, M.S.; Potenza, M.N. Substance Use Disorders and Behavioral Addictions during the COVID-19 Pandemic and COVID-19-Related Restrictions. Front. Psychiatry 2021, 12, 653674. [Google Scholar] [CrossRef]
- Chick, J. Alcohol and COVID-19. Alcohol Alcohol. 2020, 55, 341–342. [Google Scholar] [CrossRef]
- Jané-Llopis, E.; Matytsina, I. Mental Health and Alcohol, Drugs and Tobacco: A Review of the Comorbidity between Mental Disorders and the Use of Alcohol, Tobacco and Illicit Drugs. Drug Alcohol Rev. 2006, 25, 515–536. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The Impact of Physical Activity on Psychological Health during Covid-19 Pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Babicki, M.; Malchrzak, W.; Hans-Wytrychowska, A.; Mastalerz-Migas, A. Impact of Vaccination on the Sense of Security, the Anxiety of COVID-19 and Quality of Life among Polish. A Nationwide Online Survey in Poland. Vaccines 2021, 9, 1444. [Google Scholar] [CrossRef]
- Oral, T.; Gunlu, A. Adaptation of the Social Distancing Scale in the Covid-19 Era: Its Association with Depression, Anxiety, Stress, and Resilience in Turkey. Int. J. Ment. Health Addict. 2021, 1–18, 1336–1353. [Google Scholar] [CrossRef]
- Orzeszak, K. The Impact of Lockdown Policy on the Functioning of the Accomomodation and Gastronomy Industry in Poland [Author’s Translation]. Współczesna Gospodarka 2022, 1, 39–57. [Google Scholar]
- Available online: https://serwisy.gazetaprawna.pl/zdrowie/artykuly/8297387,mandat-odmowa-przyjecia-maseczka-kara-obostrzenia.html (accessed on 20 June 2022).
- Sekścińska, K.; Trzcińska, A.; Pankowski, D.; Pisula, E.; Wytrychiewicz-Pankowska, K. Financial Factors and Psychological Distress during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2022, 19, 1798. [Google Scholar] [CrossRef]
- Central Statistical Office. Price Indices of Consumer Goods and Services in November 2021; Central Statistical Office: Warsaw, Poland, 2021.
- Włostowska, K.; Trylińska-Tekielska, E.; Drewnik, M.; Pietraszewska, D. Selected Factors of Psychological Reactions among Polish Respondents to the Outbreak of Covid-19 Pandemic. OMEGA-J. Death Dying 2022, 302228221077484. [Google Scholar] [CrossRef]
- Available online: https://www.worldometers.info/coronavirus/country/poland/ (accessed on 26 October 2021).
- Dziennik Ustaw Rzeczpospolitej Polski z Dnia 19.04.2020 w Sprawie Określonych, Ograniczeń, Nakazów i Zakazów w Związku z Występowaniem Stanu Epidemii. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20200000697/O/D20200697.pdf (accessed on 14 April 2020).
- Rozporządzenie Rady Ministrów z Dnia 1 Grudnia 2020 r. w Sprawie Ustanowienia Określonych Ograniczeń, Nakazów i Zakazów w Związku z Wystąpieniem Stanu Epidemii. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20200002132 (accessed on 20 June 2022).
- Gov. Koronawirus: Informacje i Zalecenia. Available online: https://www.gov.pl/web/koronawirus/od-27-marca-zmiany-w-zasadach-bezpieczenstwa (accessed on 25 March 2021).
- Gov. Koronawirus: Informacje i Zalecenia. Available online: https://www.gov.pl/web/koronawirus/zmiany-w-zasadach-bezpieczenstwa--nowe-limity-osob-i-nauka-zdalna (accessed on 7 December 2021).
- Björkman, T.; Svensson, B. Quality of Life in People with Severe Mental Illness. Reliability and Validity of the Manchester Short Assessment of Quality of Life (MANSA). Nord. J. Psychiatry 2005, 59, 302–306. [Google Scholar] [CrossRef]
- Williams, N. The GAD-7 Questionnaire. Occup. Med. 2014, 64, 224. [Google Scholar] [CrossRef]
- Wang, Y.-P.; Gorenstein, C. Psychometric Properties of the Beck Depression Inventory-II: A Comprehensive Review. Rev. Bras. Psiquiatr. 2013, 35, 416–431. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 53–63. [Google Scholar] [CrossRef]
- Beck, A.T.; Beck, R.W. Screening Depressed Patients in Family Practice. Postgrad. Med. 1972, 52, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Wiliams, J.B.W. A Brief Measure for Assessing Generalized Anxiety Disorder. The GAD–7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Oliver, J.P.J.; Huxley, P.J.; Priebe, S.; Kaiser, W. Measuring the Quality of Life of Severely Mentally Ill People Using the Lancashire Quality of Life Profile. Soc. Psychiatry Psychiatr. Epidemiol. 1997, 32, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Priebe, S.; Huxley, P.; Knight, S.; Evans, S. Application and Results of the Manchester Short Assessment of Quality of Life (MANSA). Int. J. Soc. Psychiatry 1999, 45, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Tracz-Dral, J. Zdrowie Psychiczne w Unii Europejskiej Opracowanie tematyczna OT-674; Kancelaria Senatu: Warsaw, Poland, 2019.
- Moskalewicz, J.; Kiejna, K.; Wojtyniak, B. Epidemiologia Zaburzeń Psychiatrycznych i Dostęp do Psychiatrycznej Opieki Zdrowotnej—EZOP Polska; Instytut Psychiatrii i Neurologii: Warsaw, Poland, 2012. [Google Scholar]
- Marzo, R.R.; Vinay, V.; Bahari, R.; Chauhan, S.; Ming, D.A.F.; Fernandez, S.; Fernandez, N.; Johnson, C.C.P.; Thivakaran, A.Q.; Rahman, M.M.; et al. Depression and Anxiety in Malaysian Population during Third Wave of the COVID-19 Pandemic. CEGH 2021, 12, 100868. [Google Scholar] [CrossRef]
- Daly, M.; Sutin, A.; Robinson, E. Longitudinal Changes in Mental Health and the COVID-19 Pandemic: Evidence from the UK Household Longitudinal Study. Psychol. Med. 2020, 1–10. [Google Scholar] [CrossRef]
- Choi, H.P.E.; Hui, B.P.H.; Wan, E.Y.F. Depression and Anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation. COVID-19 Projections—Social Distancing. Available online: https://covid19.healthdata.org/global?view=social-distancing&tab=map (accessed on 27 July 2022).
- Gieroba, B. Wpływ Aktywności Fizycznej Na Zdrowie Psychiczne i Funkcje Poznawcze. MONZ 2019, 25, 153–161. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Humer, E.; Probst, T. Comparing Mental Health During the COVID-19 Lockdown a Nd 6 Months After the Lockdown in Austria: A Longitudinal Study. Front. Psychiatry 2021, 12, 625973. [Google Scholar] [CrossRef]
- Fancourt, D.; Dphil, A.S.; Bu, F. Trajectories of Anxiety and Depressive Symptoms during Enforced Isolation Due to COVID-19 in England: A Longitudinal Observational Study. Lancet 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Duan, H.; Yan, L.; Ding, X.; Gan, Y.; Kohn, N.; Wu, J. Impact of the COVID-19 Pandemic on Mental Health in the General Chinese Population: Changes, Predictors and Psychosocial Correlates. Psychiatry Res. 2020, 293, 113396. [Google Scholar] [CrossRef]
- Miszewski, K. Adaptacja do Warunków Więziennych Skazanych Długoterminowych; Repozytorium UM: Warsaw, Poland, 2015. [Google Scholar]
- Bults, M.; Beaujean, D.J.; Zwart, O.D.; Kok, G.; Empelen, P.V.; Steenbergen, J.E.V.; Richardus, J.H.; Voeten, H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health 2011, 11, 2. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2020, 136, 603–609. [Google Scholar] [CrossRef]
- Van der Velden, P.G.; Hyland, P.; Contino, C.; von Gaudecker, H.M.; Muffels, R.; Das, M. Anxiety and depression symptoms, the recovery from symptoms, and loneliness before and after the COVID-19 outbreak among the general population: Findings from a dutch population-based longitudinal study. PLoS ONE 2021, 16, e0245057. [Google Scholar] [CrossRef]
- Emodi-Perlman, A.; Eli, I.; Uziel, N.; Smardz, J.; Khehra, A.; Gilon, E.; Wieckiewicz, G.; Levin, L.; Wieckiewicz, M. Public Concerns during the COVID-19 Lockdown: A Multicultural Cross-Sectional Study among Internet Survey Respondents in Three Countries. J. Clin. Med. 2021, 10, 1577. [Google Scholar] [CrossRef]
- Ishikawa, H.; Kato, M.; Kiuchi, T. Declines in Health Literacy and Health-Related Quality of Life during the COVID-19 Pandemic: A Longitudinal Study of the Japanese General Population. BMC Public 2021, 21, 1029. [Google Scholar] [CrossRef]
- Czapiński, J. Ekonomia Szczęścia i Psychologia Bogactwa. Nauka 2012, 1, 51–88. [Google Scholar]
- Medda, E.; Toccaceli, V.; Gigantesco, A.; Picardi, A.; Fagnani, C.; Stazi, M.A. The COVID-19 Pandemic in Italy: Depressive Symptoms Immediately before and after the First Lockdown. J. Affect. Disord. 2022, 298, 202–208. [Google Scholar] [CrossRef]
- Barcella, C.A.; Polcwiartek, C.; Mohr, G.H.; Hodges, G.; Søndergaard, K.; Niels Bang, C.; Andersen, M.P.; Fosbøl, E.; Køber, L.; Schou, M.; et al. Severe Mental Illness Is Associated with Increased Mortality and Severe Course of COVID-19. Acta Psychiatr. Scand. 2021, 144, 82–91. [Google Scholar] [CrossRef]
- Diaz, A.; Baweja, R.; Bonatakis, J.K.; Baweja, R. Global Health Disparities in Vulnerable Populations of Psychiatric Patients during the COVID-19 Pandemic. WJP 2021, 11, 94. [Google Scholar] [CrossRef]
- Hao, F.; Tan, W.; Jiang, L.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y. Do Psychiatric Patients Experience More Psychiatric Symptoms during COVID-19 Pandemic and Lockdown? A Case-Control Study with Service and Research Implications for Immunopsychiatry. Brain Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef]
- Bendau, A.; Kunas, S.L.; Wyka, S.; Petzold, B.M.; Plag, J.; Asselmann, E.; Ströhle, A. Longitudinal Changes of Anxiety and Depressive Symptoms during the COVID-19 Pandemic in Germany: The Role of Pre-Existing Anxiety, Depressive, and Other Mental Disorders. J. Anxiety Disord. 2021, 79, 102377. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef]
- Kobos, E.; Knoff, B.; Dziedzic, B.; Maciąg, R.; Idzik, A. Loneliness and Mental Well-Being in the Polish Population during the COVID-19 Pandemic: A Cross-Sectional Study. BMJ Open 2022, 12, e056368. [Google Scholar] [CrossRef]
- Luhmann, M.; Hawkley, L.C. Age Differences in Loneliness from Late Adolescence to Oldest Old Age. Dev. Psychol. 2016, 52, 943–959. [Google Scholar] [CrossRef]
- Golberstein, E.; Wen, H.; Miller, B.F. Coronavirus Disease 2019 (COVID- 19) and Mental Health for Children and Adolescents. JAMA Pediatr. 2020, 174, 819–920. [Google Scholar] [CrossRef]
- Sokół-Szawłowska, M. Mental Health Impact of Quarantine during the COVID-19 Pandemic. Psychiatria 2021, 18, 57–62. [Google Scholar] [CrossRef]
| Variable | Stage 1 (n = 2467) M ± SD/N (%) | Stage 2 (n = 1627) M ± SD/N (%) | Stage 3 (n = 1696) M ± SD/N (%) | Stage 4 (n = 949) M ± SD/N (%) | p | |
|---|---|---|---|---|---|---|
| Age | 32.2 ± 10.72 | 24.6 ± 7.06 | 27.83 ± 9.55 | 29.7 ± 9.60 | <0.001 | |
| Sex | Female | 2037 (82.5) | 1295 (79.6) | 1394 (82.2) | 789 (83.1) | 0.003 |
| Male | 430 (17.5) | 332 (20.4) | 302 (17.8) | 160 (16.9) | ||
| Place of residence | Rural area | 461 (18.7) | 287 (17.6) | 326 (19.2) | 184 (19.4) | 0.002 |
| Town of up to 50,000 inhabitants | 377 (15.3) | 233 (14.4) | 268 (15.8) | 136 (14.3) | ||
| City of 50,000–250,000 inhabitants | 449 (18.2) | 303 (18.6) | 353 (20.8) | 215 (22.7) | ||
| City of over 250,000 inhabitants | 1180 (47.8) | 804 (49.4) | 744 (44.2) | 414 (43.6) | ||
| Level of education | Higher (university degree) | 1481 (60.0) | 513 (31.5) | 654 (38.6) | 493 (52.0) | <0.001 |
| Incomplete higher | 514 (20.8) | 646 (39.6) | 543 (32.1) | 222 (23.4) | ||
| Secondary | 429 (17.4) | 437 (26.9) | 445 (26.4) | 227 (23.9) | ||
| Vocational | 26 (1.0) | 8 (0.5) | 9 (0.5) | 4 (0.4) | ||
| Lower secondary | 13 (0.6) | 19 (1.2) | 24 (1.4) | 2 (0.2) | ||
| Primary | 4 (0.2) | 4 (0.3) | 9 (0.5) | 1 (0.1) | ||
| Marital status | Married | 867 (35.1) | 163 (10.0) | 323 (19.0) | 352 (37.1) | <0.001 |
| Partnership | 556 (22.6) | 446 (27.5) | 475 (28.0) | 226 (23.8) | ||
| Widowed | 30 (1.2) | 7 (0.4) | 14 (0.8) | 3 (0.3) | ||
| Divorced | 108 (4.4) | 25 (1.5) | 50 (3.0) | 21 (2.2) | ||
| Single | 905 (36.7) | 986 (60.6) | 834 (49.2) | 347 (36.6) | ||
| Healthcare professional | Yes | 632 (25.6) | 203 (12.5) | 245 (14.5) | 163 (17.2) | <0.001 |
| Prior psychiatric treatment | Yes | 516 (20.9) | 333 (20.5) | 340 (20.1) | 168 (17.7) | 0.209 |
| Psychiatric medication treatment | Yes | 443 (18.0) | 268 (16.5) | 283 (16.7) | 157 (16.5) | 0.543 |
| Recent Suspicion of COVID-19 | Yes | 78 (3.2) | 323 (19.9) | 352 (20.8) | 162 (17.1) | <0.001 |
| Compulsory quarantine in the current wave | Yes, I am under quarantine | 23 (0.9) | 29 (1.8) | 31 (1.8) | 22 (2.3) | <0.001 |
| Yes, I was under quarantine | 59 (2.4) | 243 (14.9) | 314 (18.5) | 125 (13.2) | ||
| COVID-19 diagnosis | In the course of the disease | 189 (7.9) | 33 (2.0) | 39 (2.3) | 18 (1.9) | <0.001 |
| Yes, I was infected with COVID-19 in the past | 143 (6.0) | 248 (15.2) | 298 (17.6) | 96 (10.1) | ||
| COVID-19 diagnosed in closest relatives | Yes | 117 (4.7) | 1036 (63.7) | 1122 (66.2) | 452 (47.6) | <0.001 |
| Information retrieval | Yes | 1530 (62.0) | 776 (47.7) | 767 (45.22) | 547 (57.6) | <0.001 |
| Tracking statistics on COVID-19 | Yes | 1562 (63.3) | 781 (48.0) | 710 (41.9) | 478 (50.4) | <0.001 |
| Loss of income opportunities | Yes | 610 (24.7) | 340 (20.9) | 359 (21.2) | 124 (13.1) | <0.001 |
| Beck’s Depression Inventory (BDI) | |||||
|---|---|---|---|---|---|
| Wave | Wave | Difference in Means | Lower End of the Range for Differences | Upper End of the Range for Differences | p # |
| 1 | 2 | 0.0972 | 0.0583 | 0.136 | <0.001 |
| 1 | 3 | 0.138 | 0.0984 | 0.178 | <0.001 |
| 1 | 4 | 0.0806 | 0.0325 | 0.129 | <0.001 |
| 2 | 3 | 0.0413 | −0.00367 | 0.0862 | 0.085 |
| 2 | 4 | −0.0166 | −0.0689 | 0.0357 | 0.848 |
| 3 | 4 | −0.0578 | −0.111 | −0.00465 | 0.027 |
| GAD-7 | |||||
| 1 | 2 | 0.0560 | −0.0155 | 0.127 | 0.183 |
| 1 | 3 | 0.101 | 0.0286 | 0.173 | 0.002 |
| 1 | 4 | 0.0916 | 0.00335 | 0.180 | 0.038 |
| 2 | 3 | 0.0447 | −0.0335 | 0.123 | 0.456 |
| 2 | 4 | 0.0357 | −0.0577 | 0.129 | 0.759 |
| 3 | 4 | −0.00905 | −0.103 | 0.0849 | 0.995 |
| MANSA | |||||
| 1 | 2 | 0.0575 | −0.00747 | 0.122 | 0.104 |
| 1 | 3 | −0.0271 | −0.0927 | 0.0384 | 0.711 |
| 1 | 4 | 0.0444 | −0.0347 | 0.124 | 0.473 |
| 2 | 3 | −0.0846 | −0.156 | −0.0131 | 0.013 |
| 2 | 4 | −0.0131 | −0.0973 | 0.0711 | 0.979 |
| 3 | 4 | 0.0716 | −0.0131 | 0.156 | 0.131 |
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | p * | |
|---|---|---|---|---|---|
| Anxiety about being infected with COVID-19 disease | |||||
| Mean | 5.51 | 4.86 | 4.92 | 5.77 | <0.0001 |
| Comparison of individual COVID-19 pandemic waves | x | x | <0.0001 | ||
| x | x | <0.0001 | |||
| x | x | 0.0372 | |||
| x | x | 0.9996 | |||
| x | x | <0.0001 | |||
| x | x | <0.0001 | |||
| Anxiety about neighbours being infected with COVID-19 | |||||
| Mean | 5.73 | 3.63 | 3.59 | 3.91 | <0.0001 |
| Comparison of individual COVID-19 pandemic waves | x | x | <0.0001 | ||
| x | x | <0.0001 | |||
| x | x | <0.0001 | |||
| x | x | 0.3327 | |||
| x | x | 0.1562 | |||
| x | x | 0.0009 | |||
| Anxiety about neighbours in quarantine | |||||
| Mean | 4.64 | 3.03 | 2.93 | 3.23 | <0.0001 |
| Comparison of individual COVID-19 pandemic waves | x | x | <0.0001 | ||
| x | x | <0.0001 | |||
| x | x | <0.0001 | |||
| x | x | 0.4537 | |||
| x | x | 0.7136 | |||
| x | x | 0.0371 | |||
| Adherence to the Ministry of Health recommendations regarding COVID-19 prevention | |||||
| Mean | 8.67 | 7.63 | 7.10 | 7.49 | <0.0001 |
| Comparison of individual COVID-19 pandemic waves | x | x | <0.0001 | ||
| x | x | <0.0001 | |||
| x | x | <0.0001 | |||
| x | x | <0.0001 | |||
| x | x | 0.9641 | |||
| x | x | <0.0001 | |||
| BDI | GAD-7 | MANSA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | SD | t | p | Value | SD | t | p | Value | SD | t | p | ||
| Age | −0.097 | 0.019 | −5.15 | 0.0000 | −0.035 | 0.011 | −3.10 | 0.0020 | −0.002 | 0.024 | −0.11 | 0.9145 | |
| Sex | Male | −1.601 | 0.323 | −4.96 | 0.0000 | −2.020 | 0.194 | −10.38 | 0.0000 | −0.218 | 0.406 | −0.54 | 0.5917 |
| Place of residence | Rural area | 0.230 | 0.340 | 0.68 | 0.4986 | 0.084 | 0.206 | 0.41 | 0.6817 | −0.184 | 0.427 | −0.43 | 0.6656 |
| Town of up to 50,000 inhabitants | 0.157 | 0.368 | 0.43 | 0.6699 | −0.020 | 0.223 | −0.09 | 0.9268 | −0.409 | 0.463 | −0.88 | 0.3764 | |
| City of 50,000–250,000 inhabitants | −0.118 | 0.335 | −0.35 | 0.7236 | −0.120 | 0.203 | −0.59 | 0.5547 | 0.339 | 0.420 | 0.81 | 0.4204 | |
| Level of education | Higher (university degree) | −9.487 | 2.798 | −3.39 | 0.0007 | −3.544 | 0.826 | −4.29 | 0.0000 | 8.701 | 1.707 | 5.10 | 0.0000 |
| Incomplete higher | −7.110 | 2.821 | −2.52 | 0.0118 | −2.880 | 0.829 | −3.47 | 0.0005 | 6.480 | 1.713 | 3.78 | 0.0002 | |
| Secondary | −5.925 | 2.828 | −2.09 | 0.0362 | −2.702 | 0.832 | −3.25 | 0.0012 | 5.758 | 1.719 | 3.35 | 0.0008 | |
| Vocational | −8.500 | 3.412 | −2.49 | 0.0128 | −1.288 | 1.146 | −1.12 | 0.2612 | 2.692 | 2.367 | 1.14 | 0.2554 | |
| Primary | 6.250 | 5.7446 | 1.09 | 0.2766 | −2.900 | 1.634 | −1.77 | 0.0760 | 8.115 | 3.375 | 2.40 | 0.0162 | |
| Marital status | Married | −2.824 | 0.48 | −5.88 | 0.0000 | −0.384 | 1.723 | −0.22 | 0.8235 | 2.950 | 0.606 | 4.87 | 0.0000 |
| Partnership | −1.392 | 0.544 | −2.56 | 0.0106 | −0.168 | 0.332 | −0.51 | 0.6120 | 2.869 | 0.684 | 4.19 | 0.0000 | |
| Medic | Yes | −1.939 | 0.467 | −4.14 | 0.0000 | −0.037 | 0.285 | −0.13 | 0.8949 | 2.356 | 0.406 | 5.81 | 0.0000 |
| Earnings reduction | Yes | 3.249 | 0.467 | 6.95 | 0.0000 | 1.267 | 0.286 | 4.43 | 0.0000 | −4.757 | 0.587 | −8.10 | 0.0000 |
| Psychiatric treatment | Yes | 5.681 | 0.302 | 18.80 | 0.0000 | 2.945 | 0.301 | 9.79 | 0.0000 | −6.364 | 0.624 | −10.2 | 0.0000 |
| Vaccinations against COVID-19 | No | −0.897 | 0.212 | 4.23 | 0.00001 | 0.038 | 0.123 | 0.31 | 0.755 | −0.727 | 9.255 | −2.85 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babicki, M.; Bogudzińska, B.; Kowalski, K.; Mastalerz-Migas, A. Depression, Anxiety and Quality of Life among Online Responders in Poland: A Cross-Sectional Study Covering Four Waves of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 9934. https://doi.org/10.3390/ijerph19169934
Babicki M, Bogudzińska B, Kowalski K, Mastalerz-Migas A. Depression, Anxiety and Quality of Life among Online Responders in Poland: A Cross-Sectional Study Covering Four Waves of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(16):9934. https://doi.org/10.3390/ijerph19169934
Chicago/Turabian StyleBabicki, Mateusz, Bogna Bogudzińska, Krzysztof Kowalski, and Agnieszka Mastalerz-Migas. 2022. "Depression, Anxiety and Quality of Life among Online Responders in Poland: A Cross-Sectional Study Covering Four Waves of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 16: 9934. https://doi.org/10.3390/ijerph19169934
APA StyleBabicki, M., Bogudzińska, B., Kowalski, K., & Mastalerz-Migas, A. (2022). Depression, Anxiety and Quality of Life among Online Responders in Poland: A Cross-Sectional Study Covering Four Waves of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(16), 9934. https://doi.org/10.3390/ijerph19169934








