Domains of Physical and Mental Workload in Health Work and Unpaid Domestic Work by Gender Division: A Study with Primary Health Care Workers in Brazil
Abstract
1. Introduction
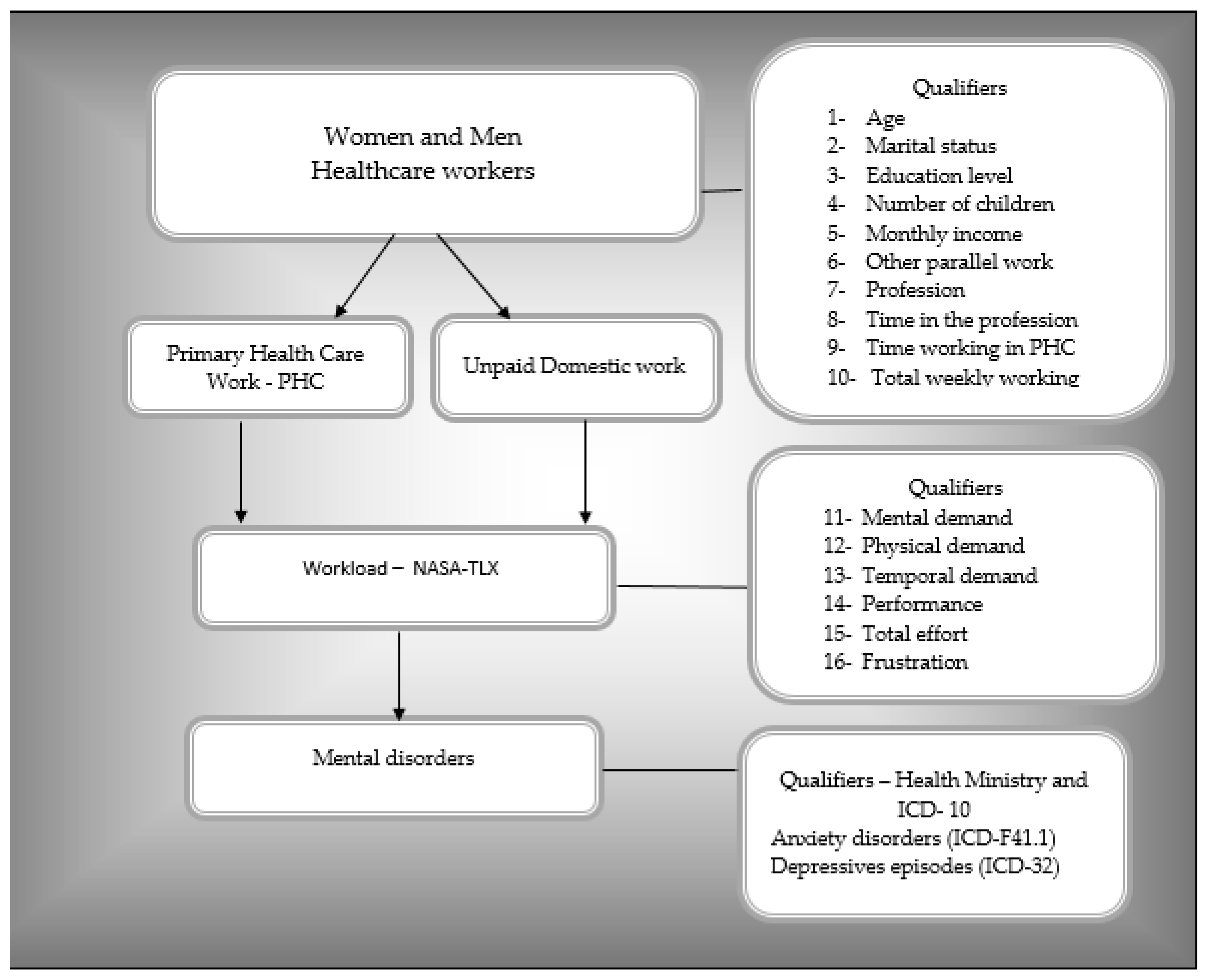
2. Materials and Methods
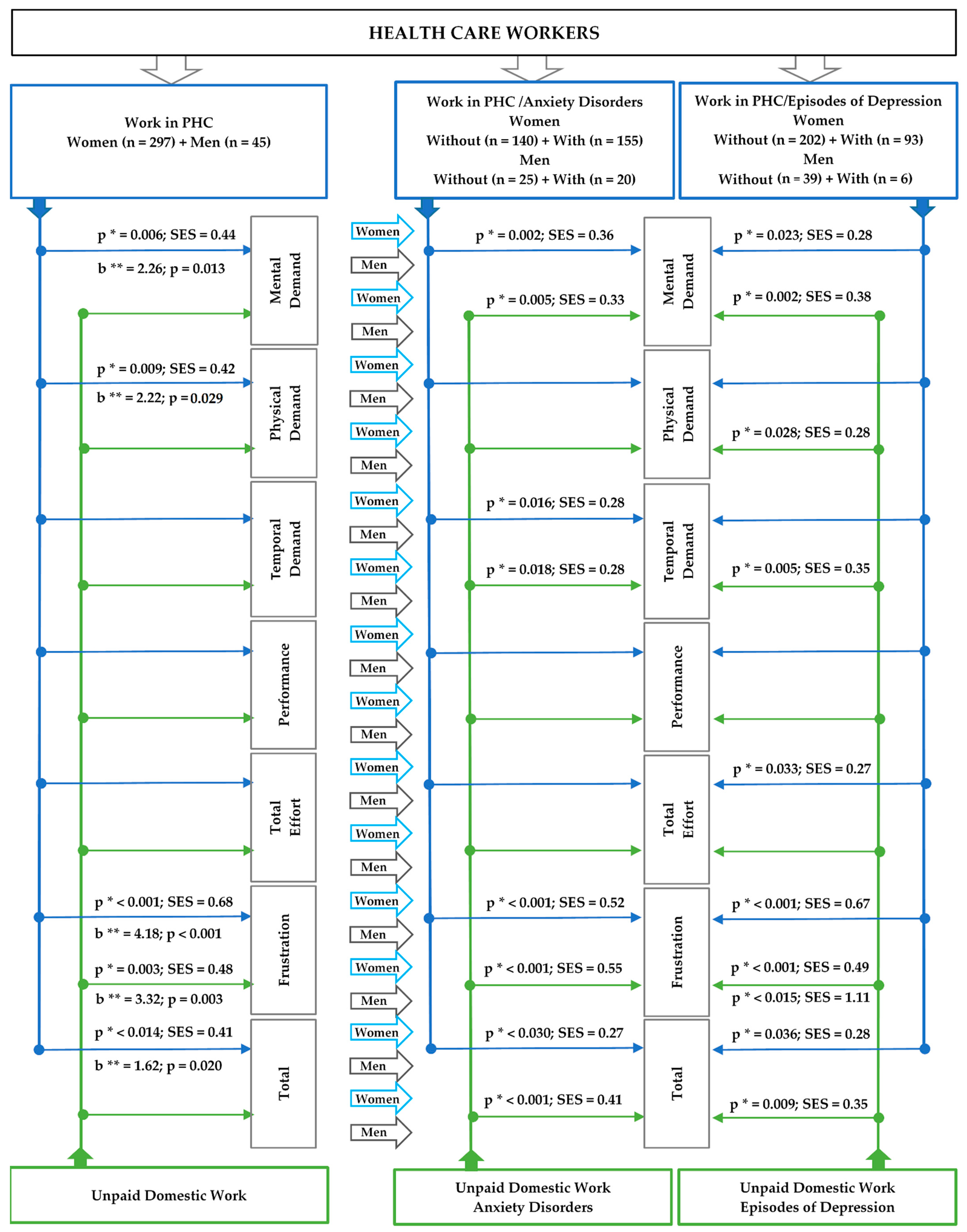
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


References
- World Health Organization (WHO). Primary Health Care. World Health Organization. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/primary-health-care#:~:text=%22PHC%20is%20a%20whole%2Dof,to%20treatment%2C%20rehabilitation%20and%20palliative (accessed on 20 July 2022).
- Brazil. Ministério da Saúde. Secretaria de Atenção Primária à Saúde. O que é Atenção Primária? Available online: https://aps.saude.gov.br/smp/smpoquee (accessed on 23 May 2022).
- Brazil Law, Nº 7.602. Dispõe Sobre a Política Nacional de Segurança e Saúde no Trabalho. Diário Oficial da União: Brasília, DF, Brazil. 2011. Available online: http://www.planalto.gov.br/ccivil_03/_ato2011-2014/2011/decreto/d7602.htm#:~:text=DECRETO%20N%C2%BA%207.602%2C%20DE%207,e%20Sa%C3%BAde%20no%20Trabalho%20%2D%20PNSST (accessed on 22 May 2022).
- World Health Organization (WHO). Delivered by Women, Led by Men: A Gender and Equity Analysis of the Global Health and Social Workforce. World Health Organization; (Human Resources for Health Observer Series; 24). 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/311322/9789241515467-eng.pdf?sequence=1&isAllowed=y (accessed on 23 May 2022).
- Shannon, G.; Minckas, N.; Tan, D.; Haghparast-Bidgoli, H.; Batura, N.; Mannell, J. Feminisation of the health workforce and wage conditions of health professions: An exploratory analysis. Hum. Resour. Health 2019, 17, 72. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization (ILO). The Gender Division of Labour; GLOPP/OIT: Genebra, Switzerland, 2008. [Google Scholar]
- International Labor Organization—ILO. Relatório Regional Trabalho e Família: Rumo a Novas Formas de Conciliação com Corresponsabilidade Social. Brasilia: Escritório da OIT no Brasil e a Secretaria Especial de Políticas para as Mulheres da Presidência da República. 2009. Available online: https://www.ilo.org/wcmsp5/groups/public/---americas/---ro-lima/---ilo-brasilia/documents/publication/wcms_233473.pdf (accessed on 20 July 2022).
- Addati, L.; Cattaneo, U.; Esquivel, V.; Valarino, I. Care Work and Care Jobs for the Future of Decent Work; International Labor Oganization—ILO: Geneva, Switzerland, 2018; Available online: http://www.ilo.org/global/publications/books/WCMS_633135/lang--en/index.htm (accessed on 20 July 2022).
- Stoll, R.; Kreuzfeld, S.; Weippert, M.; Vilbrandt, R.; Stoll, N. System for flexible field measurement of physiological data of operators working in automated labs. J. Lab. Autom. 2007, 12, 110–114. [Google Scholar] [CrossRef]
- Johnson, C.; Smith, E.C. A mid-term terminal concept of operations: Evaluation and evolution analysis. In Proceedings of the 2008 Integrated Communications, Navigation and Surveillance Conference, Bethesda, MD, USA, 5–7 May 2008; pp. 1–10. [Google Scholar] [CrossRef]
- Balch, C.M.; Shanafelt, T.D.; Dyrbye, L.; Sloan, J.A.; Russell, T.R.; Bechamps, G.J.; Freischlag, J.A. Surgeon distress as calibrated by hours worked and nights on call. J. Am. Coll. Surg. 2010, 211, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (task load index): Results of experimental and theoretical research. Adv. Psychol. 1988, 52, 139–183. [Google Scholar] [CrossRef]
- Hart, S.G. NASA-Task Load Index (NASA-TLX): 20 years later. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2006, 50, 904–908. [Google Scholar] [CrossRef]
- Fernández-Aguilar, C.; Casado-Aranda, L.A.; Farrés, F.M.; Minué, L.S. Has COVID-19 changed the workload for primary care physicians? The case of Spain. Fam. Pract. 2021, 38, 780–785. [Google Scholar] [CrossRef]
- Ayaz, B.; Martimianakis, M.A.; Muntaner, C.; Nelson, S. Participation of women in the health workforce in the fragile and conflict-affected countries: A scoping review. Hum. Resour. Health 2021, 19, 94. [Google Scholar] [CrossRef]
- Alobaid, A.M.; Gosling, C.M.; Khasawneh, E.; McKenna, L.; Williams, B. Challenges Faced by Female Healthcare Professionals in the Workforce: A Scoping Review. J. Multidiscip. Health 2020, 13, 681–691. [Google Scholar] [CrossRef]
- Park, J.; Han, B.-Y.; Kim, Y. Gender differences in occupations and complaints of musculoskeletal symptoms: Representative sample of South Korean workers. Am. J. Ind. Med. 2017, 60, 342–349. [Google Scholar] [CrossRef]
- Beauregard, N.; Marchand, A.; Bilodeau, J.; Durand, P.; Demers, A.; Haines, V.Y. Gendered pathways to burnout: Results from the SALVEO study. Ann. Work. Expo. Health 2018, 62, 426–437. [Google Scholar] [CrossRef]
- Bilodeau, J.; Marchand, A.; Demers, A. Psychological distress inequality between employed men and women: A gendered exposure model SSM. Popul. Health 2020, 11, 100626. [Google Scholar] [CrossRef] [PubMed]
- Győrffy, Z.; Dweik, D.; Girasek, E. Workload, mental health and burnout indicators among female physicians. Hum. Resour. Health 2016, 14, 12. [Google Scholar] [CrossRef] [PubMed]
- Alegría, M.; NeMoyer, A.; Falgàs, I.; Wang, Y.; Alvarez, K. Social Determinants of Mental Health: Where We Are and Where We Need to Go. Curr. Psychiatry Rep. 2018, 20, 95. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Genebra, Switzerland, 1992; Available online: https://apps.who.int/iris/handle/10665/37958 (accessed on 2 April 2022).
- Habib, R.R.; Halwani, D.A.; Mikati, D.; Hneiny, L. Sex and Gender in Research on Healthcare Workers in Conflict Settings: A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 4331. [Google Scholar] [CrossRef]
- Morgan, R.; Tan, H.L.; Oveisi, N.; Memmott, C.; Korzuchowski, A.; Hawkins, K.; Smith, J. Women healthcare workers’ experiences during COVID-19 and other crises: A scoping review. Int. J. Nurs. Stud. Adv. 2022, 4, 100066. [Google Scholar] [CrossRef]
- Rai, R.; El-Zaemey, S.; Dorji, N.; Rai, B.D.; Fritschi, L. Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 2603. [Google Scholar] [CrossRef]
- López-Atanes, M.; Recio-Barbero, M.; Sáenz-Herrero, M. Are women still “the other”? Gendered mental health interventions for health care workers in Spain during COVID-19. Psychol. Trauma 2020, 12, S243–S244. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional por Amostra de Domicílios Contínua—Outras Formas de Trabalho. 2019. Available online: https://www.ibge.gov.br/estatisticas/sociais/trabalho/9171-pesquisa-nacional-por-amostra-de-domicilios-continua-mensal.html?=&t=destaques (accessed on 18 July 2022).
- Brazil Law, Nº 2.436, 21 September 2017. Aprova a Política Nacional de Atenção Básica, Estabelecendo a Revisão de Diretrizes para a Organização da Atenção Básica, no Âmbito do Sistema Único de Saúde (SUS); Diário Oficial da União: Brasília, Brazil, 2017. Available online: https://www.in.gov.br/materia/-/asset_publisher/Kujrw0TZC2Mb/content/id/19308123/do1-2017-09-22-portaria-n-2-436-de-21-de-setembro-de-2017-19308031 (accessed on 20 April 2022).
- Brazil. Organização Pan-Americana Da Saúde No Brasil. Doenças Relacionadas Ao Trabalho: Manual De Procedimentos Para Os Services de Saúde; Organização Pan-Americana da Saúde no Brasil: Brasília, Brazil, 2001. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/doencas_relacionadas_trabalho_manual_procedimentos.pdf (accessed on 20 March 2022).
- Hoonakker, P.; Carayon, P.; Gurses, A.P.; Brown, R.; Khunlertkit, A.; McGuire, K.; Walker, J.M. Measuring workload of ICU nurses with a questionnaire survey: The NASA Task Load Index (TLX). IIE Trans. Healthc. Syst. Eng. 2011, 1, 131–143. [Google Scholar] [CrossRef]
- Noyes, J.M.; Bruneau, D.P.J. A self-analysis of the NASA-TLX workload measure. Ergonomics 2007, 50, 514–519. [Google Scholar] [CrossRef]
- Sasso, G.M.; Barra, D.C. Cognitive workload of computerized nursing process in intensive care units. Comput. Inform. Nurs. 2015, 33, 339–345. [Google Scholar] [CrossRef]
- Shoja, E.; Aghamohammadi, V.; Bazyar, H.; Moghaddam, H.R.; Nasiri, K.; Dashti, M.; Choupani, A.; Garaee, M.; Aliasgharzadeh, S.; Asgari, A. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health 2020, 20, 1636. [Google Scholar] [CrossRef] [PubMed]
- Masci, F.; Spatari, G.; Bortolotti, S.; Giorgianni, C.M.; Antonangeli, L.M.; Rosecrance, J.; Colosio, C. Assessing the Impact of Work Activities on the Physiological Load in a Sample of Loggers in Sicily (Italy). Int. J. Environ. Res. Public Health 2022, 19, 7695. [Google Scholar] [CrossRef] [PubMed]
- Cezar-Vaz, M.R.; Bonow, C.A.; Silva, M.R.S. Mental and Physical Symptoms of Female Rural Workers: Relation between Household and Rural Work. Int. J. Environ. Res. Public Health 2015, 12, 11037–11049. [Google Scholar] [CrossRef] [PubMed]
- Cezar-Vaz, M.R.; Bonow, C.A.; Almeida, M.C.V.; Sant’Anna, C.F.; Cardoso, L.S. Workload and associated factors: A study in maritime port in Brazil. Rev. Lat. Am. Enferm. 2016, 24, e2837. [Google Scholar] [CrossRef] [PubMed]
- Ballardin, L.; Guimarães, L.B.M. Evaluation of an oil distributor company operator’s workload. Produção 2009, 19, 581–592. [Google Scholar] [CrossRef]
- Cardoso, M.S.; Gontijo, L.A. Evaluation of mental workload and performance measurement: NASA TLX and SWAT. Gest. Prod. 2012, 19, 873–884. [Google Scholar] [CrossRef]
- Dorrian, J.; Baulk, S.D.; Dawson, D. Work hours, workload, sleep and fatigue in Australian Rail Industry employees. Appl. Ergon. 2011, 42, 202–209. [Google Scholar] [CrossRef]
- Safari, S.; Akbari, J.; Kazemi, M.; Mououdi, M.A.; Mahaki, B. Personnel’s health surveillance at work: Effect of age, body mass index, and shift work on mental workload and work ability index. J. Environ. Public Health 2013, 2013, 289498. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research; Chapman & Hall: London, UK, 1991; pp. 403–4071. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Nasirizad, M.K.; Chehrzad, M.M.; Reza, M.S.; Maleki, M.; Mardani, A.; Atharyan, S.; Harding, C. Nursing physical workload and mental workload in intensive care units: Are they related? Nurs. Open 2021, 8, 1625–1633. [Google Scholar] [CrossRef]
- Sriharan, A.; Ratnapalan, S.; Tricco, A.C.; Lupea, D.; Ayala, A.P.; Pang, H.; Lee, D.D. Occupational Stress, Burnout, and Depression in Women in Healthcare During COVID-19 Pandemic: Rapid Scoping Review. Front. Glob. Womens Health 2020, 1, 596690. [Google Scholar] [CrossRef] [PubMed]
- Ornek, O.K.; Esin, M.N. Effects of a work-related stress model based mental health promotion program on job stress, stress reactions and coping profiles of women workers: A control groups study. BMC Public Health 2020, 20, 1658. [Google Scholar] [CrossRef] [PubMed]
- Croxson, C.H.; Ashdown, H.F.; Hobbs, F.R. GPs’ perceptions of workload in England: A qualitative interview study. Br. J. Gen. Pract. 2017, 67, e138–e147. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Francisco, D.H.; Duarte-Clíments, G.; Del Rosario-Melián, J.M.; Gómez-Salgado, J.; Romero-Martín, M.; Sánchez-Gómez, M.B. Influence of Workload on Primary Care Nurses’ Health and Burnout, Patients’ Safety, and Quality of Care: Integrative Review. Healthcare 2020, 8, 12. [Google Scholar] [CrossRef]
- Glenton, C.; Javadi, D.; Perry, H.B. Community health workers at the dawn of a new era: Roles and tasks. Health Res. Policy Syst. 2021, 19, 128. [Google Scholar] [CrossRef]
- European Commission. Report on Progress on Equality between Women and Men in 2013 Accompanying the Document Report from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions 2013 Report on the Application of the EU Charter of Fundamental Rights. 2014. Available online: https://eur-lex.europa.eu/legal-content/en/TXT/?uri=CELEX:52014SC0142 (accessed on 20 March 2022).
- Cerrato, J.; Cifre, E. Gender Inequality in Household Chores and Work-Family Conflict. Front. Psychol. 2018, 9, 1330. [Google Scholar] [CrossRef]
- Rostami, F.; Babaei-Pouya, A.; Teimori-Boghsani, G.; Jahangirimehr, A.; Mehri, Z.; Feiz-Arefi, M. Mental Workload and Job Satisfaction in Healthcare Workers: The Moderating Role of Job Control. Front. Public Health 2021, 9, 683388. [Google Scholar] [CrossRef]
- Nikeghbal, K.; Kouhnavard, B.; Shabani, A.; Zamanian, Z. Covid-19 Effects on the Mental Workload and Quality of Work Life in Iranian Nurses. Ann. Glob. Health 2021, 87, 79. [Google Scholar] [CrossRef]
- Suto, M.; Balogun, O.O.; Dhungel, B.; Kato, T.; Takehara, K. Effectiveness of Workplace Interventions for Improving Working Conditions on the Health and Wellbeing of Fathers or Parents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 4779. [Google Scholar] [CrossRef]
- Kokoroko, E.; Sanda, M.A. Effect of Workload on Job Stress of Ghanaian OPD Nurses: The Role of Coworker Support. Saf. Health Work 2019, 10, 341–346. [Google Scholar] [CrossRef]
- Marina, A.M.; Rubio-Valdehitab, S.; Díaz-Ramirob, E.M. Trait-anxiety and job psychosocial conditions as determinants of mental health in nursing. Ansiedad Estrés 2020, 26, 167–173. [Google Scholar] [CrossRef]
- Akova, İ.; Kiliç, E.; Özdemir, M.E. Prevalence of Burnout, Depression, Anxiety, Stress, and Hopelessness Among Healthcare Workers in COVID-19 Pandemic in Turkey. Inquiry 2022, 59, 469580221079684. [Google Scholar] [CrossRef]
- Monterrosa-Castro, A.; Redondo-Mendoza, V.; Mercado-Lara, M. Psychosocial factors associated with symptoms of generalized anxiety disorder in general practitioners during the COVID-19 pandemic. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 2020, 68, 1228–1234. [Google Scholar] [CrossRef]
- Van der Molen, H.F.; Vries, S.; Sluiter, J.K. Occupational diseases among workers in lower and higher socioeconomic positions. Int. J. Environ. Res. Public Health 2018, 15, 2849. [Google Scholar] [CrossRef] [PubMed]
- Jerg-Bretzke, L.; Limbrecht-Ecklundt, K.; Walter, S.; Spohrs, J.; Beschoner, P. Correlations of the “Work-Family Conflict” With Occupational Stress-A Cross-Sectional Study among University Employees. Front. Psychiatry 2020, 11, 134. [Google Scholar] [CrossRef] [PubMed]
- Svedberg, P.; Mather, L.; Bergström, G.; Lindfors, P.; Blom, V. Work-Home Interference, Perceived Total Workload, and the Risk of Future Sickness Absence Due to Stress-Related Mental Diagnoses Among Women and Men: A Prospective Twin Study. Int. J. Behav. Med. 2018, 25, 103–111. [Google Scholar] [CrossRef]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L.; et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef]
- Catton, H. Global challenges in health and health care for nurses and midwives everywhere. Int. Nurs. Rev. 2020, 67, 4–6. [Google Scholar] [CrossRef]
- Viertiö, S.; Kiviruusu, O.; Piirtola, M.; Kaprio, J.; Korhonen, T.; Marttunen, M.; Suvisaari, J. Factors contributing to psychological distress in the working population, with a special reference to gender difference. BMC Public Health 2021, 21, 611. [Google Scholar] [CrossRef]
- Hiesinger, K.; Tophoven, S. Job requirement level, work demands, and health: A prospective study among older workers. Int. Arch. Occup. Environ. Health 2019, 92, 1139–1149. [Google Scholar] [CrossRef]
- Organização Mundial da Saúde (OMS). Ambientes de Trabalho Saudáveis: Um Modelo para Ação: Para Empregadores, Trabalhadores, Formuladores de Política e Profissionais. OMS; Tradução do Serviço Social da Indústria: Brasília, Brazil, 2010; Available online: http://apps.who.int/iris/bitstream/handle/10665/44307/9789241599313_por.pdf;jsessionid=7AD90DACF40CAC5BE72F50630F75C232?sequence=2 (accessed on 23 July 2022).
| Variables | Total Sample (n = 342) | Men (n = 45) | Women (n = 297) | p |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age (years) * | 41.5 ± 10.0 | 38.6 ± 11.8 | 42.0 ± 9.7 | 0.033 a |
| Skin color | 0.137 b | |||
| Caucasian | 262 (77.5) | 31 (70.5) | 231 (78.6) | |
| African descendant | 37 (10.9) | 4 (9.1) | 33 (11.2) | |
| Mixed race | 39 (11.5) | 9 (20.5) | 30 (10.2) | |
| Marital status | 0.093 b | |||
| Single | 99 (28.9) | 20 (44.4) | 79 (26.6) | |
| Married/stable union | 200 (58.5) | 21 (46.7) | 179 (60.3) | |
| Separated/divorced | 37 (10.8) | 3 (6.7) | 34 (11.4) | |
| Widowed | 6 (1.8) | 1 (2.2) | 5 (1.7) | |
| Level of education | 0.002 b | |||
| Incomplete high school/complete high school | 83 (24.3) | 4 (8.9) | 79 (26.6) # | |
| Technical course | 47 (13.7) | 3 (6.7) | 44 (14.8) | |
| Incomplete higher education | 39 (11.4) | 5 (11.1) | 34 (11.4) | |
| Complete higher education/technology course | 98 (28.7) | 24 (53.3) # | 74 (24.9) | |
| Specialization | 59 (17.3) | 6 (13.3) | 53 (17.8) | |
| Master’s/doctorate | 16 (4.7) | 3 (6.7) | 13 (4.4) | |
| Number of children ** | 1 (0–2) | 0 (0–2) | 1 (1–2) | 0.002 c |
| Monthly income (m.w.) | <0.001 b | |||
| Up to 2 | 130 (38.7) | 11 (25.0) | 119 (40.8) # | |
| From 2 to 4 | 116 (34.5) | 10 (22.7) | 106 (36.3) | |
| From 4 to 8 | 41 (12.2) | 6 (13.6) | 35 (12.0) | |
| More than 8 | 49 (14.6) | 17 (38.6) # | 32 (11.0) | |
| Location | 0.998 b | |||
| Municipality 1 | 286 (83.6) | 38 (84.4) | 248 (83.5) | |
| Municipality 2 | 56 (16.4) | 7 (15.6) | 49 (16.5) | |
| Other work parallel to that of PHC | <0.001 b | |||
| Yes | 63 (18.5) | 19 (43.2) | 44 (14.9) | |
| No | 277 (81.5) | 25 (56.8) | 252 (85.1) | |
| Sector-PHU | 0.918 b | |||
| PHU—traditional | 26 (7.6) | 4 (8.9) | 22 (7.4) | |
| FHU | 282 (82.5) | 37 (82.2) | 245 (82.5) | |
| PHU—24 h | 34 (9.9) | 4 (8.9) | 30 (10.1) | |
| Profession | <0.001 b | |||
| Nurse | 53 (15.5) | 2 (4.4) | 51 (17.2) # | |
| Doctor | 43 (12.6) | 18 (40.0) # | 25 (8.4) | |
| Nursing technician/assistant | 73 (21.3) | 9 (20.0) | 64 (21.5) | |
| Community health agent | 139 (40.6) | 12 (26.7) | 127 (42.8) # | |
| Dentist | 13 (3.8) | 4 (8.9) | 9 (3.0) | |
| Oral health technician/assistant | 15 (4.4) | 0 (0.0) | 15 (5.1) | |
| Other | 6 (1.8) | 0 (0.0) | 6 (2.0) | |
| Length of time in the profession (years) ** | 11 (4–16) | 5 (0–16) | 11.5 (7–16) | 0.011 c |
| Time working in PHC (years) ** | 8 (1–13) | 2 (0–9) | 9 (2–14) | <0.001 c |
| Weekly workload | 44.4 ± 13.2 | 48.3 ± 13.8 | 43.8 ± 13.0 | 0.033 a |
| Work period in PHC | 0.916 b | |||
| Day shift | 304 (89.4) | 41 (91.1) | 263 (89.2) | |
| Night shift | 8 (2.4) | 1 (2.2) | 7 (2.4) | |
| Night/day | 28 (8.2) | 3 (6.7) | 25 (8.5) |
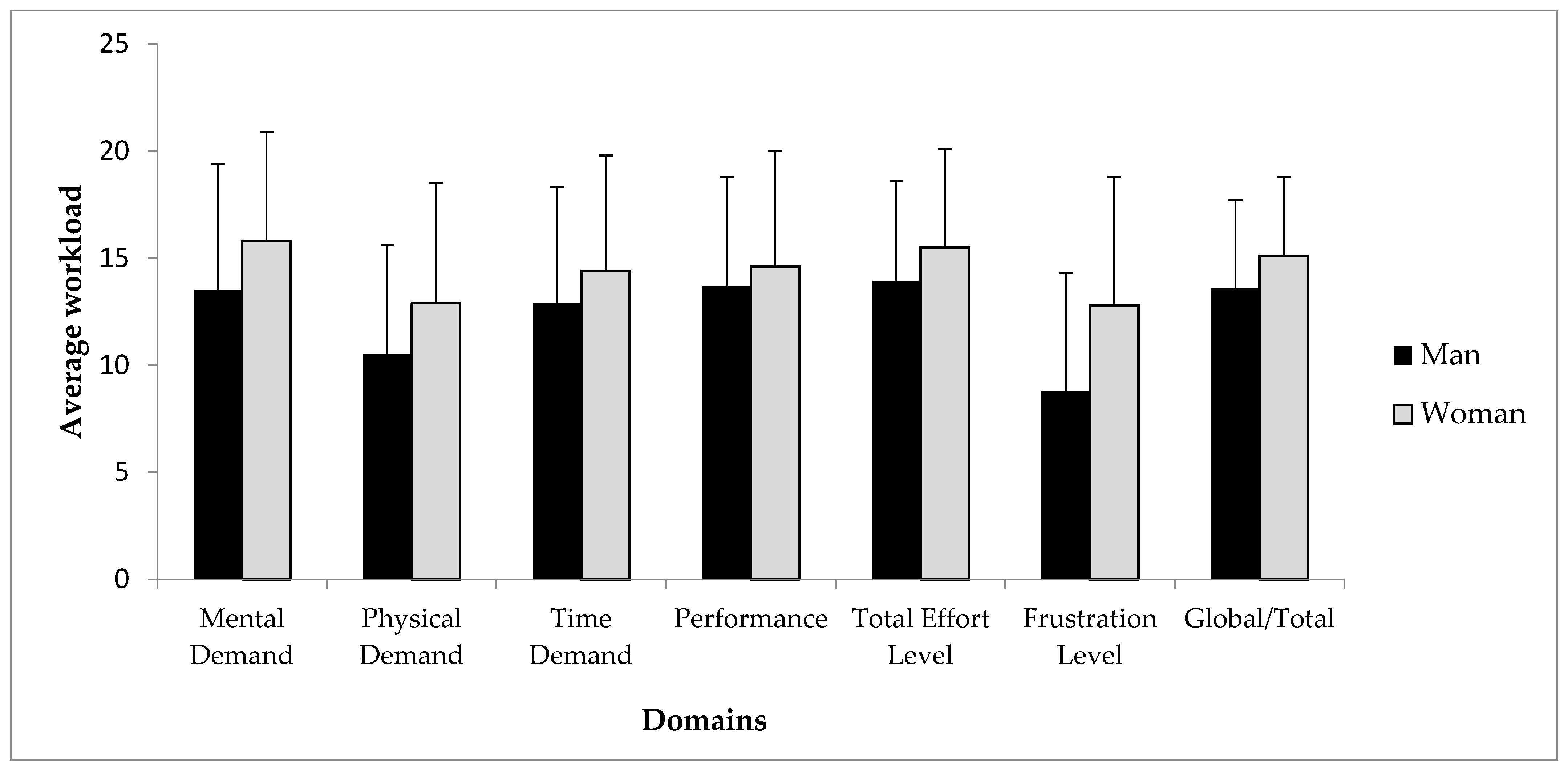
| Workload Domains | Men (n = 45) | Women (n = 297) | p * | Cohen’s SES | b (95%CI) ** | p |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||||
| Workload in PHC work | ||||||
| Mental demand | 13.5 ± 5.9 | 15.8 ± 5.1 | 0.006 | 0.44 | 2.26 (0.47 to 4.04) | 0.013 |
| Physical demand | 10.5 ± 5.1 | 12.9 ± 5.6 | 0.009 | 0.42 | 2.22 (0.23 to 4.20) | 0.029 |
| Temporal demand | 12.9 ± 5.4 | 14.4 ± 5.4 | 0.089 | 0.28 | 1.81 (−0.08 to 3.71) | 0.061 |
| Performance | 13.7 ± 5.1 | 14.6 ± 5.4 | 0.303 | 0.17 | 0.88 (−1.00 to 2.77) | 0.359 |
| Total effort | 13.9 ± 4.7 | 15.5 ± 4.6 | 0.024 | 0.36 | 1.54 (−0.11 to 3.20) | 0.067 |
| Frustration | 8.8 ± 5.5 | 12.8 ± 6.0 | <0.001 | 0.68 | 4.18 (2.17 to 6.19) | <0.001 |
| Total | 13.6 ± 4.1 | 15.1 ± 3.7 | 0.014 | 0.41 | 1.62 (0.25 to 2.98) | 0.020 |
| Workload in unpaid domestic work | ||||||
| Mental demand | 12.1 ± 5.8 | 13.2 ± 6.0 | 0.241 | 0.19 | 1.28 (−0.88 to 3.43) | 0.244 |
| Physical demand | 9.2 ± 4.9 | 11.5 ± 5.8 | 0.007 | 0.39 | 1.95 (−0.08 to 3.98) | 0.059 |
| Temporal demand | 12.3 ± 4.7 | 13.5 ± 5.5 | 0.148 | 0.24 | 1.34 (−0.65 to 3.33) | 0.187 |
| Performance | 13.0 ± 5.4 | 13.0 ± 5.4 | 0.958 | 0.01 | 0.15 (−1.79 to 2.09) | 0.878 |
| Total effort | 12.6 ± 5.5 | 14.2 ± 4.9 | 0.050 | 0.32 | 1.03 (−0.76 to 2.82) | 0.259 |
| Frustration | 7.3 ± 5.6 | 10.2 ± 6.2 | 0.003 | 0.48 | 3.32 (1.12 to 5.52) | 0.003 |
| Total | 12.0 ± 4.2 | 13.4 ± 4.2 | 0.049 | 0.33 | 1.42 (−0.13 to 2.97) | 0.073 |
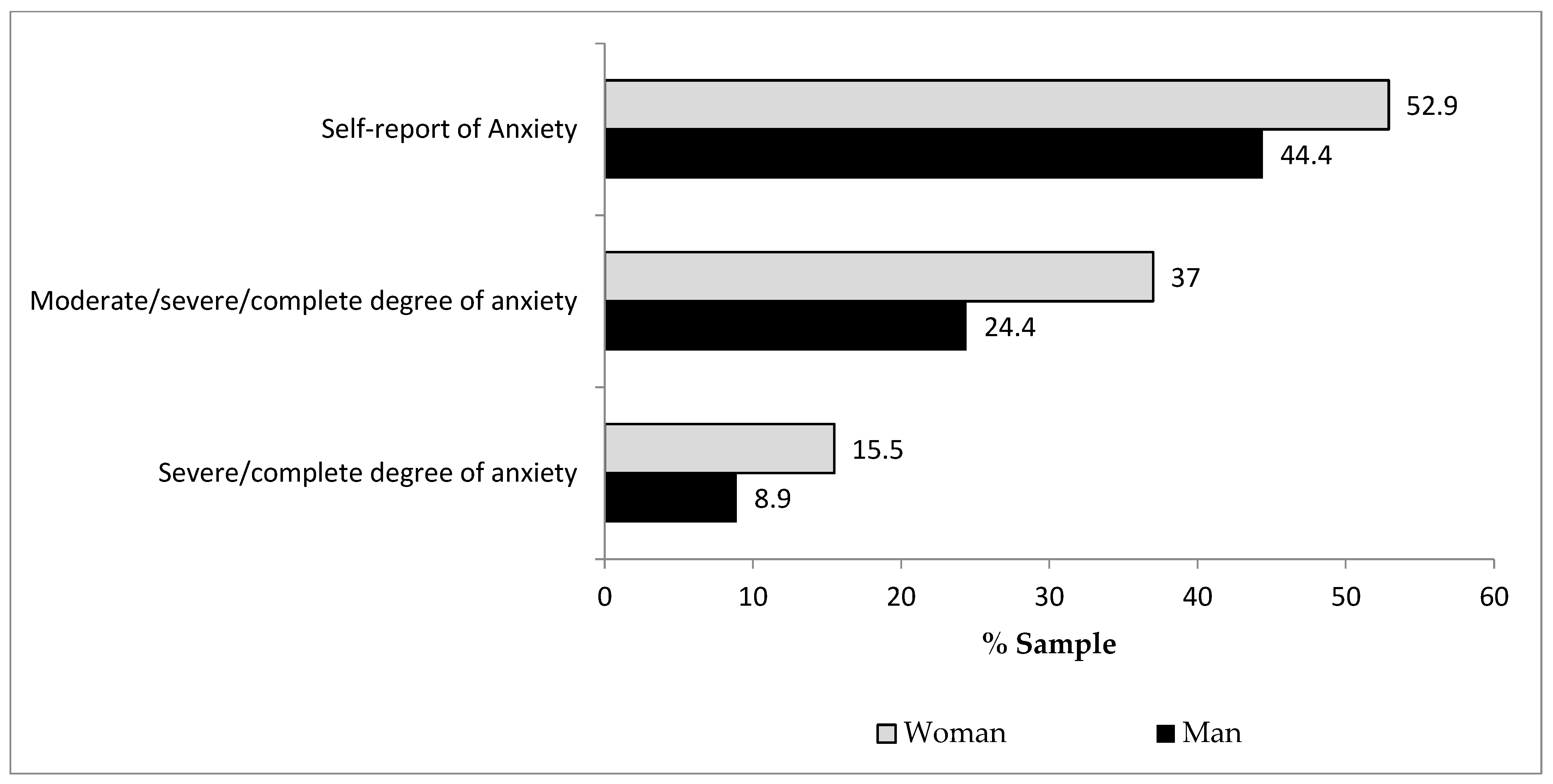
| Women (n = 295) | Men (n = 45) | |||||||
|---|---|---|---|---|---|---|---|---|
| Workload Domains | Without Anxiety Disorders (n = 140) | With Anxiety Disorders (n = 155) | p * | Cohen’s SES | Without Anxiety Disorders (n = 25) | With Anxiety Disorders (n = 20) | p * | Cohen’s SES |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||
| Workload in PHC work | ||||||||
| Mental demand | 14.8 ± 5.3 | 16.6 ± 4.7 | 0.002 | 0.36 | 13.1 ± 5.5 | 13.9 ± 6.5 | 0.644 | 0.14 |
| Physical demand | 12.5 ± 5.9 | 13.2 ± 5.3 | 0.256 | 0.13 | 11.0 ± 5.5 | 10.0 ± 4.6 | 0.536 | 0.19 |
| Temporal demand | 13.6 ± 5.4 | 15.1 ± 5.2 | 0.016 | 0.28 | 13.3 ± 5.0 | 12.5 ± 5.9 | 0.630 | 0.15 |
| Performance | 14.6 ± 5.2 | 14.6 ± 5.5 | 0.889 | 0.02 | 13.4 ± 5.5 | 14.2 ± 4.7 | 0.614 | 0.15 |
| Total effort | 15.0 ± 4.6 | 16.0 ± 4.6 | 0.062 | 0.22 | 13.6 ± 4.4 | 14.3 ± 5.1 | 0.629 | 0.15 |
| Frustration | 11.2 ± 6.0 | 14.2 ± 5.6 | <0.001 | 0.52 | 9.3 ± 5.7 | 8.2 ± 5.2 | 0.496 | 0.21 |
| Total | 14.6 ± 3.8 | 15.6 ± 3.5 | 0.030 | 0.27 | 13.5 ± 4.2 | 13.8 ± 4.1 | 0.819 | 0.07 |
| Workload in unpaid domestic work | ||||||||
| Mental demand | 12.2 ± 5.9 | 14.1 ± 6.0 | 0.005 | 0.33 | 10.9 ± 5.5 | 13.6 ± 6.0 | 0.134 | 0.46 |
| Physical demand | 10.8 ± 5.8 | 12.1 ± 5.8 | 0.052 | 0.23 | 10.1 ± 5.0 | 8.2 ± 4.6 | 0.201 | 0.39 |
| Temporal demand | 12.7 ± 5.4 | 14.3 ± 5.5 | 0.018 | 0.28 | 11.4 ± 4.5 | 13.5 ± 4.9 | 0.142 | 0.46 |
| Performance | 13.3 ± 5.2 | 12.8 ± 5.6 | 0.456 | 0.09 | 13.3 ± 4.7 | 12.6 ± 6.3 | 0.682 | 0.12 |
| Total effort | 13.6 ± 4.9 | 14.7 ± 4.9 | 0.043 | 0.24 | 12.1 ± 5.1 | 13.3 ± 6.0 | 0.500 | 0.20 |
| Frustration | 8.5 ± 5.5 | 11.7 ± 6.4 | <0.001 | 0.55 | 6.0 ± 4.8 | 8.8 ± 6.2 | 0.101 | 0.50 |
| Total | 12.5 ± 4.1 | 14.2 ± 4.2 | <0.001 | 0.41 | 11.4 ± 4.1 | 12.8 ± 4.3 | 0.286 | 0.33 |
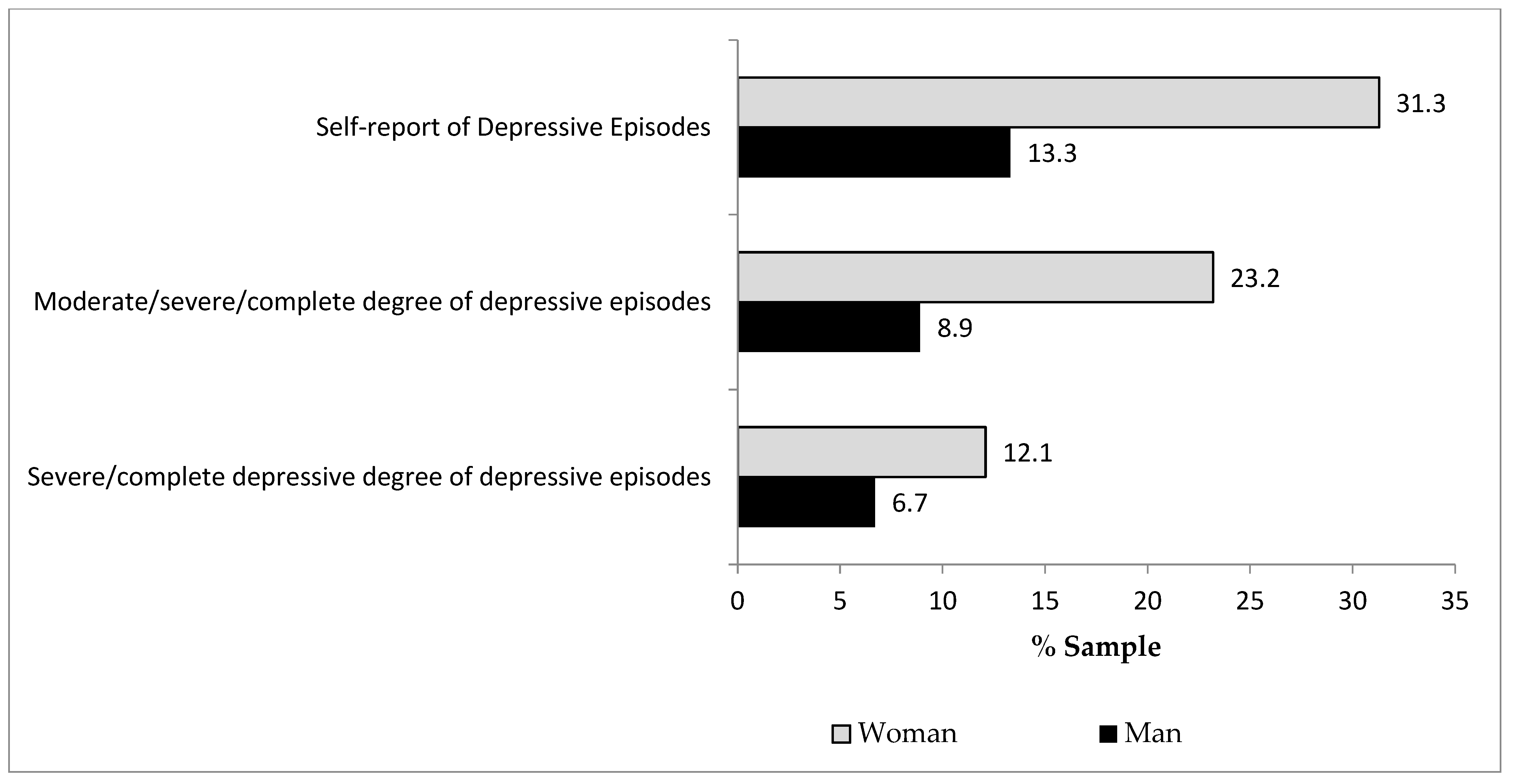
| Women (n = 295) | Men (n = 45) | |||||||
|---|---|---|---|---|---|---|---|---|
| Workload Domains | Without Episodes of Depression (n = 202) | With Episodes of Depression (n = 93) | p * | Cohen’s SES | Without Episodes of Depression (n = 39) | With Episodes of Depression (n = 6) | p * | Cohen’s SES |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||
| Workload in PHC work | ||||||||
| Mental demand | 15.3 ± 5.2 | 16.7 ± 4.6 | 0.023 | 0.28 | 13.4 ± 5.9 | 14.2 ± 6.6 | 0.766 | 0.13 |
| Physical demand | 12.8 ± 5.9 | 13.0 ± 5.1 | 0.767 | 0.04 | 10.7 ± 5.4 | 9.5 ± 2.3 | 0.370 | 0.23 |
| Temporal demand | 14.1 ± 5.3 | 15.0 ± 5.4 | 0.165 | 0.18 | 13.2 ± 5.4 | 11.2 ± 5.6 | 0.407 | 0.37 |
| Performance | 14.6 ± 5.2 | 14.6 ± 5.8 | 0.986 | 0.00 | 13.4 ± 5.3 | 15.7 ± 3.2 | 0.323 | 0.44 |
| Total effort | 15.2 ± 4.6 | 16.4 ± 4.5 | 0.033 | 0.27 | 14.1 ± 4.8 | 12.5 ± 3.8 | 0.449 | 0.34 |
| Frustration | 11.6 ± 5.7 | 15.4 ± 5.7 | <0.001 | 0.67 | 9.0 ± 5.6 | 7.5 ± 4.7 | 0.544 | 0.27 |
| Total | 14.8 ± 3.7 | 15.8 ± 3.5 | 0.036 | 0.28 | 13.5 ± 4.3 | 13.9 ± 2.9 | 0.840 | 0.09 |
| Workload in unpaid domestic work | ||||||||
| Mental demand | 12.5 ± 5.8 | 14.8 ± 6.2 | 0.002 | 0.38 | 11.5 ± 5.7 | 15.8 ± 5.6 | 0.091 | 0.76 |
| Physical demand | 11.0 ± 5.8 | 12.6 ± 5.8 | 0.028 | 0.28 | 9.3 ± 4.6 | 9.2 ± 7.1 | 0.967 | 0.02 |
| Temporal demand | 12.9 ± 5.4 | 14.9 ± 5.7 | 0.005 | 0.35 | 11.8 ± 4.5 | 15.2 ± 5.5 | 0.106 | 0.73 |
| Performance | 13.2 ± 5.2 | 12.7 ± 5.9 | 0.536 | 0.08 | 12.6 ± 5.4 | 15.5 ± 5.5 | 0.227 | 0.54 |
| Total effort | 13.8 ± 4.9 | 15.0 ± 4.9 | 0.071 | 0.23 | 12.7 ± 5.2 | 11.8 ± 7.7 | 0.710 | 0.16 |
| Frustration | 9.3 ± 5.9 | 12.2 ± 6.4 | <0.001 | 0.49 | 6.5 ± 5.1 | 12.3 ± 6.4 | 0.015 | 1.11 |
| Total | 12.9 ± 4.1 | 14.4 ± 4.3 | 0.009 | 0.35 | 11.6 ± 4.1 | 14.3 ± 4.7 | 0.156 | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cezar-Vaz, M.R.; Xavier, D.M.; Bonow, C.A.; Vaz, J.C.; Cardoso, L.S.; Sant’Anna, C.F.; da Costa, V.Z. Domains of Physical and Mental Workload in Health Work and Unpaid Domestic Work by Gender Division: A Study with Primary Health Care Workers in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 9816. https://doi.org/10.3390/ijerph19169816
Cezar-Vaz MR, Xavier DM, Bonow CA, Vaz JC, Cardoso LS, Sant’Anna CF, da Costa VZ. Domains of Physical and Mental Workload in Health Work and Unpaid Domestic Work by Gender Division: A Study with Primary Health Care Workers in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(16):9816. https://doi.org/10.3390/ijerph19169816
Chicago/Turabian StyleCezar-Vaz, Marta Regina, Daiani Modernel Xavier, Clarice Alves Bonow, Jordana Cezar Vaz, Letícia Silveira Cardoso, Cynthia Fontella Sant’Anna, and Valdecir Zavarese da Costa. 2022. "Domains of Physical and Mental Workload in Health Work and Unpaid Domestic Work by Gender Division: A Study with Primary Health Care Workers in Brazil" International Journal of Environmental Research and Public Health 19, no. 16: 9816. https://doi.org/10.3390/ijerph19169816
APA StyleCezar-Vaz, M. R., Xavier, D. M., Bonow, C. A., Vaz, J. C., Cardoso, L. S., Sant’Anna, C. F., & da Costa, V. Z. (2022). Domains of Physical and Mental Workload in Health Work and Unpaid Domestic Work by Gender Division: A Study with Primary Health Care Workers in Brazil. International Journal of Environmental Research and Public Health, 19(16), 9816. https://doi.org/10.3390/ijerph19169816









