First Nations Peoples’ Eating and Physical Activity Behaviors in Urban Areas: A Mixed-Methods Approach
Abstract
:1. Introduction
1.1. Diet and PA among First Nations People
1.2. Health Representation
1.3. Context and Objective
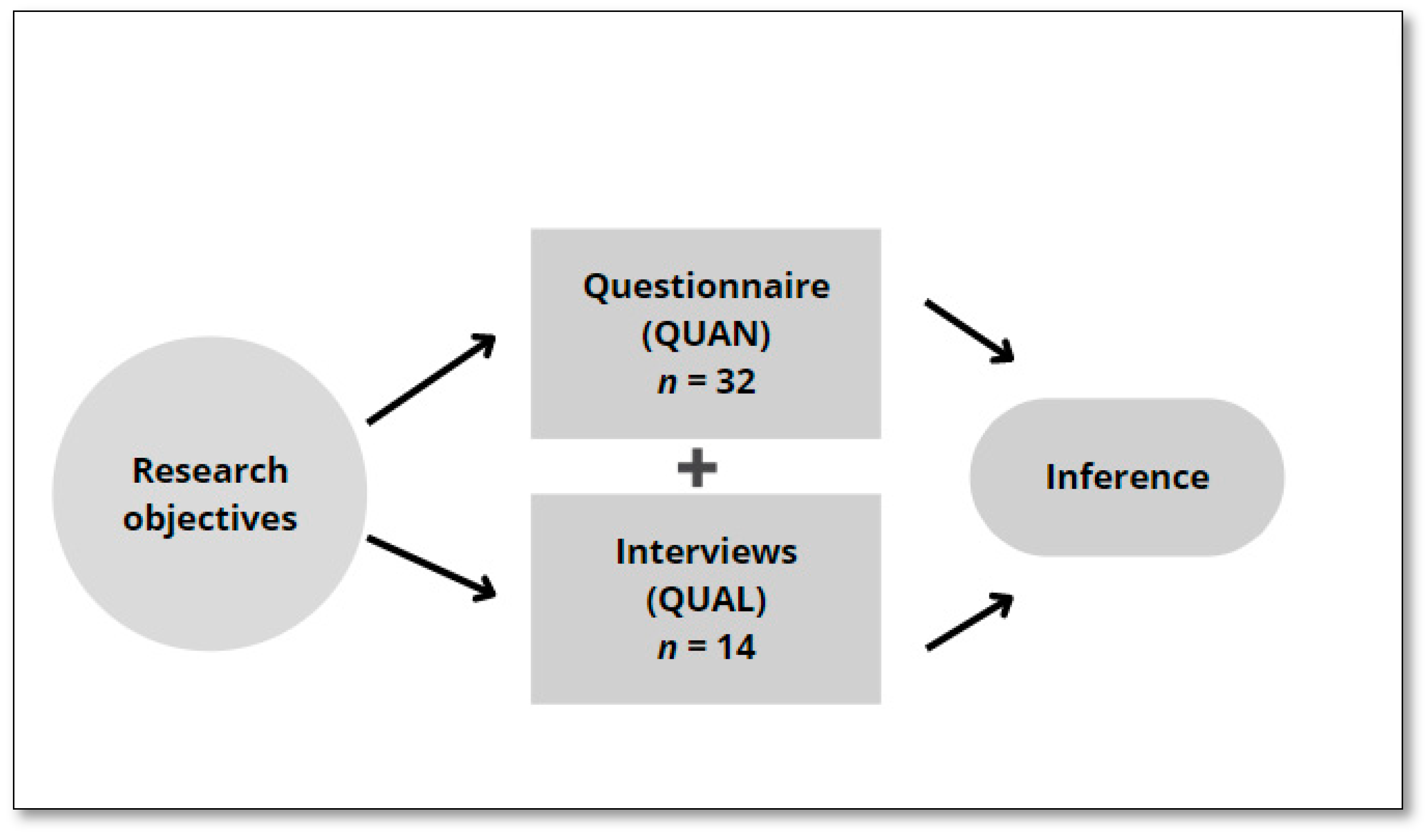
2. Methods
2.1. Questionnaire
- (1)
- To obtain a portrait of nutrition, open-ended questions from the Canadian Food Guide (First Nations, Inuit, and Métis) were used to learn the daily recommendations associated with the four food groups: fruits and vegetables, grain products, milk and alternatives, and meat and alternatives [13]. The questions were inspired by a local questionnaire used in the Waban-Aki community. For example, “How many servings per day, on average, do you get from the following food groups (fruits and vegetables, grain products, dairy products, meat, and alternatives)?”
- (2)
- The questionnaire used to measure participants’ motivation toward nutrition was the Regulation of Eating Behaviors Scale (REBS) [30], which is based on Self-Determination Theory (SDT) [31,32]). The questionnaire contained 24 items (eight items per subscale) divided into five types of motivation: intrinsic (I take pleasure in fixing healthy meals), identified (I believe it will eventually allow me to feel better), introjected (I feel I must absolutely be thin), external (It is expected of me), and amotivation (I don’t know. I can’t see how my efforts to eat healthily are helping my health situation). Participants indicated the extent to which they agreed with each item using a Likert scale ranging from 1 (Does not correspond at all) to 7 (Corresponds exactly).
- (3)
- The questionnaire used to describe participants’ PA practice was the Godin Leisure Time Exercise Questionnaire (GLTEQ), developed by Godin and Shephard (1985). It describes the duration (minutes per week) and frequency of PA practiced at low intensity (e.g., slow walking), moderate intensity (e.g., walking), or high intensity (e.g., running) [33]. The GLTEQ questionnaire is easy to use and reliable [33]. It has been used among Indigenous participants [34,35,36]. Overall, three questions assessed each type of PA intensity on a Likert scale ranging from 1 (Not at all true) to 7 (Completely true) [37].
- (4)
- The questionnaire used to measure motivation toward PA was the Behavioural Regulation in Exercise Questionnaire-2 (BREQ-2) [38]. This questionnaire is also based on SDT [31,32] and includes 19 items divided into five types of motivation: intrinsic (I exercise because it’s fun), identified (I value the benefits of exercise), introjected (I feel guilty when I don’t exercise), external (I exercise because other people say I should), and amotivation (I don’t see why I should have to exercise) (measured on a 5-point Likert scale). Participants indicated the extent to which they agreed with each of the BREQ-2 items using a Likert scale ranging from 0 (Not true for me) to 4 (Very true for me).
- (5)
- Participants’ sociodemographic characteristics, such as gender, age, marital status, education, income, place of residence, and nation of origin, were also measured.
2.2. Semi-Directed Interviews
2.3. Ethical Considerations
2.4. Analyses
3. Results
3.1. Results of the Questionnaire (QUAN)
3.1.1. Portrait of Nutrition
3.1.2. Motivation toward Eating Behavior
3.1.3. PA Profile
3.1.4. Motivation toward PA
3.2. Results of the Semi-Directed Interviews (QUAL)
3.2.1. The Population’s State of Health
At three (on a scale of ten) right now. Yes, it is not great because I work a lot, and I do not do a lot of physical activity. Then, right now, I am not sleeping much because I am working all the time.Participant 2 (Atikamekw, Women, 24 years old)
I would say 9.5 (on a scale of ten). […] I am very disciplined. I get up at 5:00 in the morning to train, and then I work from 8:00 in the morning until 5:00 at night. My meal planning for the week is always done on the weekends. We prepare meals ahead of time to minimize [food] deviations as much as possible.Participant 1 (Innu, Women, 47 years old)
Someone who is healthy is someone who takes care of himself, psychologically and physically, who pays attention to everything, who never touches drugs, or, maybe, who smokes a cigarette now and then. Who may consume alcohol sometimes, but not too much, not too over the top, in moderation, as they say.Participant 7 (Atikamekw, Man, 18 years old)
3.2.2. Individual Characteristics
Since my wife is sick, I learn things there—not to eat too much poutine [fries, gravy, and cheese]—because she tends to want to order in the restaurants all the time. I tell her, “You can have fries once in a while, but not every day.” I bring either fruit or vegetables. I tell them to eat things with the rest of us—to eat together and then talk about our day.Participant 3 (Atikamekw, Man, 68 years old)
When I started to work, I neglected this sport, this practice, this way of life, and then slowly, well, the other things took over. The children were born. […] When I was young, I went to the training camp, and then they saw the little “Indian boy” with his bag of equipment arrive, everyone was looking at me.Participant 12 (Atikamekw, Man, 49 years old)
3.2.3. Living Environments
My mom […] is there a lot at my (hockey) games. She tells me things like to shoot when it’s a good time. […] You know, she encourages me a lot. My brother encourages me, too, like he really, really, really encourages me. I love everything he says. He actually inspires me. It’s an inspiration for me not to give up hockey.Participant 7 (Atikamekw, Man, 18 years old)
My mother always says to us, “I’d like you to cook. But we don’t take the initiative […]. We want to cook, but no, she can’t digest that. For her, it’s too spicy or too fatty, and she can’t digest it. That’s…So we do not take the initiative; it is just too complicated. Makes us lose hope.Participant 14 (Waban-Aki, Women, 27 years old)
We’re doing more collective kitchens. Then, we really invite people to go there. The world sees this and prefers to stay at home and do nothing. Maybe we should advertise it more. With the Native Friendship Centre, a health walk was organized. There were only two participants.Participant 2 (Atikamekw, Women, 24 years old)
Sometimes people here cook. Then it’s really vegetables that I don’t know or haven’t eaten yet. And it’s good when you taste it. It smells good, and that’s it.Participant 5 (Atikamekw, Women, 47 years old)
3.2.4. Systems
If you get sick inside the enclosure (in the community), the [Federal] government will take care of you, treat you, accommodate you, or transport you to a hospital. But if you get sick outside the paddock, you have to manage in another Quebec system […]. So, you become a bit of a hot potato for the government.Participant 12 (Atikamekw, Man, 49 years old)
Yes, well, there are certainly a lot of areas here that are scary. Like in the area where I live, I don’t go out after eight […]. My area is like a darker part of the city because they often say that there are a lot of drug dealers and not many lights.Participant 13 (Innu, Women, 27 years old)
4. Discussion
4.1. Diet
4.2. PA
4.3. Diet and PA
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistics Canada. First Nations Peoples, Métis, and Inuit in Canada: Diverse and Growing Populations; Minister of Industry: Ottawa, ON, Canada, 2018.
- The Constitution Acts 1867 to 1982; Part II Rights of the Aboriginal Peoples of Canada §Art 35. 2021. Available online: https://lois-laws.justice.gc.ca/PDF/CONST_TRD.pdf (accessed on 14 August 2022).
- Statistics Canada. Aboriginal peoples in Canada: Key results from the 2016 Census. The Daily 2017, 11-001-X. Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/171025/dq171025a-eng.pdf?st=7qHREhiD (accessed on 14 August 2022).
- Rotenberg, C. Social Determinants of Health for the Off-Reserve First Nations Population, 15 Years of Age and Older, 2012; Statistics Canada: Ottawa, ON, Canada, 2016.
- Public Health Agency of Canada. What We Heard: Indigenous Peoples and COVID-19; Government of Canada: Ottawa, ON, Canada, 2021.
- Bergeron, O.; Désilets, G.; Roberge, M.-C.; Laforest, J. COVID-19: Indigenous Resilience, a Lever to Support; Institut National de Santé Publique du Québec: Quebec, QC, Canada, 2020. [Google Scholar]
- First Nations of Quebec and Labrador Health and Social Services Commission. RHS Quebec First Nations Regional Health Survey/Health Status and Chronic Conditions; First Nations of Quebec and Labrador Health and Social Services Commission: Wendake, QC, Canada, 2018. [Google Scholar]
- First Nations of Quebec and Labrador Health and Social Services Commission. RHS Quebec First Nations Regional Health Survey/Diabetes and Obesity; First Nations of Quebec and Labrador Health and Social Services Commission: Wendake, QC, Canada, 2018. [Google Scholar]
- Batal, M.; Chan, H.M.; Fediuk, K.; Ing, A.; Berti, P.; Sadik, T.; Johnson-Down, L. Associations of Health Status and Diabetes Among First Nations Peoples Living On-reserve in Canada. Can. J. Public Health 2021, 112, 154–167. [Google Scholar] [CrossRef] [PubMed]
- Batal, M.; Decelles, S. A Scoping Review of Obesity Among Indigenous Peoples in Canada. J. Obes. 2019, 2019, 9741090. [Google Scholar] [CrossRef] [PubMed]
- Wharton, S.; Lau, D.C.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in Adults: A Clinical Practice Guideline. Can. Med. Assoc. J. 2020, 192, E875–E891. [Google Scholar] [CrossRef] [PubMed]
- Institut National de Santé Publique du Quebec. The Diet of Quebec First Nations and Inuit Peoples; Institut National de Santé Publique du Quebec: Quebec, QC, Canada, 2015. [Google Scholar]
- Health Canada. Eating Well with Canada’s Food Guide: First Nations, Inuit, and Métis. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/fnihb-dgspni/pdf/pubs/fnim-pnim/2007_fnim-pnim_food-guide-aliment-eng.pdf (accessed on 31 May 2021).
- Chan, L.; Batal, M.; Receveur, O.; Sadik, T.; Schwartz, H.; Ing, A.; Fediuk, K.; Tikhonow, C.; Lindhorst, K. First Nations Food, Nutrition, and Environment Study (FNFNES): Results from Quebec (2016); University of Ottawa: Ottawa, ON, Canada, 2019. [Google Scholar]
- Batal, M.; Chan, H.M.; Fediuk, K.; Ing, A.; Berti, P.; Sadik, T.; Johnson-Down, L. Importance of the Traditional Food Systems for First Nations Adults Living on Reserves in Canada. Can. J. Public Health 2021, 112, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Gaudin, V.L.; Receveur, O.; Walz, L.; Girard, F.; Potvin, L. A Mixed Methods Inquiry into the Determinants of Traditional Food Consumption among Three Cree Communities of Eeyou Istchee from an Ecological Perspective. Int. J. Circumpolar Health 2014, 73, 663–692. [Google Scholar] [CrossRef]
- First Nations Education Council and First Nations of Quebec and Labrador Health and Social Services Commission. First Nations Sports, Recreation, and Physical Activities: Between Tradition and Performance; First Nations Education Council and First Nations of Quebec and Labrador Health and Social Services Commission: Wendake, QC, Canada, 2018. [Google Scholar]
- National Collaborating Centre for Aboriginal Health. Physical Activity Fact Sheet; National Collaborating Centre for Aboriginal Health: Prince George, BC, Canada, 2013. [Google Scholar]
- Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines: Glossary of Terms. Available online: http://csepguidelines.ca/ (accessed on 23 June 2022).
- Leclerc, A.M.; Busque, A.; Miquelon, P.; Rivard, M.C. Cardiovascular Prevention: A Scoping Review of Healthy Eating and Physical Activity among Indigenous Peoples in Canada. CJCN 2019, 29, 26–37. [Google Scholar]
- Douglas, V.K. Introduction to Aboriginal Health and Health Care in Canada: Bridging Health and Healing; Springer Publishing Compagny: New York, NY, USA, 2013. [Google Scholar]
- Périllat-Amédée, S.; Delormier, T.; Flamand, S.; Ottawa, G.; Flamand, D.; McBeath, B.; McComber, A.; Macaulay, A.; Lévesque, L. Atikamekw Nehirowisiw Mirowatisiwin: Identifying the Strengths of the Manawan Community to Promote Wellness and Healthy Lifestyles. Turt. Isl. J. Indig. Health 2021, 1, 37–49. [Google Scholar] [CrossRef]
- Lévesque, C.; Gagnon, M.; Desbiens, C.; Apparicio, P.; Cloutier, É.; Sirois, T. Profil Démographique de la Population des Premières Nations et du Peuple Inuit dans les Villes du Québec, 2001 à 2016. [Demographic Profile of the First Nations and Inuit Population in Quebec Cities, 2001 to 2016]; Alliance de Recherche ODENA, Réseau de Recherche et de Connaissances Relatives aux Peuples Autochtones (DIALOG) et Regroupement des Centres D’amitié Autochtones du Québec: Montréal, QC, Canada, 2019. [Google Scholar]
- Place, J. The Health of Aboriginal People Residing in Urban Areas; National Collaborating Centre for Aboriginal Heath: Prince George, BC, Canada, 2012. [Google Scholar]
- Poirier, S.; Jérôme, L. La Société D’histoire Atikamekw (Nehirowisiw Kitci Atisokan). Présentation: Les Atikamekw Nehirowisiwok: Territorialités et savoirs [Presentation: The Atikamekw Nehirowisiwok: Territorialities and knowledge]. Rech. Amérindiennes Qué. 2014, 44, 3–10. [Google Scholar] [CrossRef]
- Plano Clark, V.; Ivankova, N. Mixed Methods Research: A Guide to the Field; SAGE: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Creswell, J.; Plano Clark, V.L. Designing and Conducting Mixed Methods Research, 3rd ed.; SAGE Publications: Los Angeles, CA, USA, 2018. [Google Scholar]
- Vedel, I.; Kaur, N.; Hong, Q.N.; El Sherif, R.; Khanassov, V.; Godard-Sebillotte, C.; Sourial, N.; Yang, X.Y.; Pluye, P. Why and how to use mixed methods in primary health care research. Fam. Pract. 2019, 36, 365–368. [Google Scholar] [CrossRef]
- Leclerc, A.-M. Étude Descriptive sur la Santé des Premières Nations de la Mauricie et Centre-du-Québec: Perspectives Croisées sur les Habitudes de Vie et les Services de Santé [Descriptive Health Study of the First Nations of Mauricie and Centre-du-Québec: Crossed Perspectives on Lifestyle and Health Services]; Université de Montréal/Université du Québec à Trois-Rivières: Trois-Rivières, QC, Canada, 2021. [Google Scholar]
- Pelletier, L.G.; Dion, S.C.; Slovinec-D’Angelo, M.; Reid, R. Why Do you Regulate What you Eat? Relationships Between Forms of Regulation, Eating Behaviors, Sustained Dietary Behavior Change, and Psychological Adjustment. Motiv. Emot. 2004, 28, 245–277. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Plenum: New York, NY, USA, 1985. [Google Scholar]
- Deci, E.L.; Ryan, R.M. The “What” and “Why” of Goal Pursuits: Human Needs and the Self-Determination of Behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Godin, G.; Shephard, R. A Simple Method to Assess Exercise Behavior in the Community. Can. J. Appl. Sport Sci. 1985, 10, 141–146. [Google Scholar] [PubMed]
- Coble, J.D.; E Rhodes, R.; Higgins, J.W. Physical Activity Behaviors and Motivations in an Adult First Nation Population: A Pilot Study. Ethn. Dis. 2009, 19, 42–48. [Google Scholar]
- Ironside, A.K.; Ferguson, L.J.; Katapally, T.R.; Foulds, H.J. Cultural Connectedness as a Determinant of Physical Activity among Indigenous Adults in Saskatchewan. Appl. Physiol. Nutr. Metab. 2020, 45, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Kirby, A.M.; Lévesque, L.; Wabano, V.; Robertson-Wilson, J. Perceived Community Environment and Physical Activity Involvement in a Northern-Rural Aboriginal Community. IJBNPA 2007, 4, 63. [Google Scholar] [CrossRef]
- Castonguay, A.; Miquelon, P.; Michaud, M. Access to Physical Activity Possibilities Improves the Frequency of its Practice: Effect of Level of Motivation. Can. J. Diabetes 2015, 39, 170–171. [Google Scholar] [CrossRef]
- Markland, D.; Tobin, V. A Modification to the Behavioural Regulation in Exercise Questionnaire to Include an Assessment of Amotivation. J. Sport Exerc. Psychol. 2004, 26, 191–196. [Google Scholar] [CrossRef]
- Ministry of Health and Social Services of Quebec. Health’s Determinants: Better Understanding for Better Acting; Ministry of Health and Social Services of Quebec: Quebec, QC, Canada, 2012. [Google Scholar]
- Leclerc, A.-M.; De Montigny, F.; Cloutier, L. L’expérience des Hommes Atteints d’Hypertension Artérielle [The Experience of Men Living with Hypertension]. CJCN 2015, 25, 29–35. [Google Scholar]
- Fortin, M.-F.; Gagnon, J. Fondements et Étapes du Processus de Recherche: Méthodes Quantitatives et Qualitatives [Foundations and Steps of the Research Process: Quantitative and Qualitative Methods], 4th ed.; Chenelière Éducation: Montréal, QC, Canada, 2022. [Google Scholar]
- Giorgi, A. From the phenomenological method used as a qualitative research mode in human sciences: Theory, practice, and evaluation. In Qualitative Research: Epistemological and Methodological Issues; Poupart, J., Ed.; Gaétan Morin: Boucherville, QC, Canada, 1997; pp. 341–364. [Google Scholar]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage: Beverly Hills, CA, USA, 1985. [Google Scholar]
- Woo, K. Polit & Beck: Canadian Essentials of Nursing Research, 4th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2019. [Google Scholar]
- The First Nations Information Governance Centre (FNIGC). Ownership, Control, Access, and Possession (OCAPTM): The Path to First Nations Information Governance; FNIGC: Ottawa, ON, Canada, 2014.
- Pluye, P.; Bengoechea, E.G.; Granikov, V.; Kaur, N.; Tang, D.L. A World of Possibilities in Mixed Methods: Review of the Combinations of Strategies Used to Integrate the Phases, Results, and Qualitative and Quantitative Data. Int. J. Mult. Res. Approaches 2018, 10, 41–56. [Google Scholar] [CrossRef]
- Colapinto, C.K.; Graham, J.; St-Pierre, S. Trends and Correlates of Frequency of Fruit and Vegetable Consumption, 2007 to 2014. Health Rep. 2018, 29, 9–14. [Google Scholar]
- Trofholz, A.C.; Schulte, A.K.; Berge, J.M. How Parents Describe Picky Eating and Its Impact on Family Meals: A Qualitative analysis. Appetite 2017, 110, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Tanguay, N.; de Grosbois, S.; Saint-Charles, J. Land Health, Indicators of Animal Health and Holism. Rech. Amérindiennes Au Québec 2013, 43, 3–19. [Google Scholar] [CrossRef]
- Thompson, C.; Cummins, S.; Brown, T.; Kyle, R. What Does it Mean to Be a ‘Picky Eater’? A Qualitative Study of Food Related Identities and Practices. Appetite 2015, 84, 235–239. [Google Scholar] [CrossRef]
- Blanchet, R.; Willows, N.; Johnson, S.; Initiatives, O.N.S.R.; Batal, M. Traditional Food, Health, and Diet Quality in Syilx Okanagan Adults in British Columbia, Canada. Nutrients 2020, 12, 927. [Google Scholar] [CrossRef]
- Verstuyf, J.; Patrick, H.; Vansteenkiste, M.; Teixeira, P.J. Motivational Dynamics of Eating Regulation: A Self-Determination Theory Perspective. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 21. [Google Scholar] [CrossRef]
- Gropper, S.S.; Arsiwalla, D.D.; Lord, D.C.; Huggins, K.W.; Simmons, K.P.; Ulrich, P.V. Associations Among Eating Regulation and Body Mass Index, Weight, and Body Fat in College Students: The Moderating Role of Gender. Eat. Behav. 2014, 15, 321–327. [Google Scholar] [CrossRef]
- Otis, N.; Pelletier, L. Women’s Regulation Styles for Eating Behaviors and Outcomes: The Mediating Role of Approach and Avoidance Food Planning. Motiv. Emot. 2008, 32, 55–67. [Google Scholar] [CrossRef]
- Mead, E.; Gittelsohn, J.; Roache, C.; Sharma, S. Healthy Food Intentions and Higher Socioeconomic Status are Associated with Healthier Food Choices in an Inuit Population. J. Hum. Nutr. Diet. 2010, 23, 83–91. [Google Scholar] [CrossRef]
- Sutherland, J. Indigenous Sports and Recreation Programs and Partnerships Across Canada: A Literature Review and Environmental Scan; National Collaborating Centre of Indigenous Health: Prince George, BC, Canada, 2021. [Google Scholar]
- Paraschak, V.; Thompson, K. Finding Strength(s): Insights on Aboriginal Physical Cultural Practices in Canada. Sport Soc. 2014, 17, 1046–1060. [Google Scholar] [CrossRef]
- McHugh, T.-L.F. Physical Activity Experiences of Aboriginal Youth. Nativ. Stud. Rev. 2011, 20, 7–26. [Google Scholar]
- Tang, K.; Jardine, C.G. Our Way of Life: Importance of Indigenous Culture and Tradition to Physical Activity Practices. Int. J. Indig. Health 2016, 11, 211–227. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, Physical Activity, and Self-Determination Theory: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef]
- Sport for Life Society, & Aboriginal Sport Circle. Indigenous Sport for Life: Long-Term Participant Development Pathway 1.2; Sport for Life Society: Victoria, BC, Canada, 2019. [Google Scholar]
- Physical Literacy. What is Physical Literacy. Available online: http://physicalliteracy.ca/physical-literacy/ (accessed on 31 May 2021).
- Ahmed, F.; Zuk, A.; Tsuji, L. The Impact of Land-Based Physical Activity Interventions on Self-Reported Health and Well-Being of Indigenous Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7099. [Google Scholar] [CrossRef]
- Dyrstad, S.M.; Hansen, B.H.; Holme, I.M.; Anderssen, S.A. Comparison of Self-Reported Versus Accelerometer-Measured Physical Activity. Med. Sci. Sports Exerc. 2014, 46, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Poitras, M.-E.; Canapé, A.; Bacon, K.; Vaillancourt, V.T.; Hatcher, S.; Boudreault, A. The COVID-19 Pandemic: Challenges and Needs Experienced by Indigenous People in Urban Areas. Int. J. Indig. Health 2022, 17, 87–101. [Google Scholar] [CrossRef]
- Watson, A.; Purkey, E.; Davison, C.M.; Fu, M.; Nolan, D.; Mitchell, D.; Kehoe, J.; Traviss, S.; Bayoumi, I. Indigenous Strength: Braiding Culture, Ceremony and Community as a response to the COVID-19 pandemic. Int. J. Indig. Health 2022, 17, 111–121. [Google Scholar] [CrossRef]
- Statistics Canada. Consumer Price Index, June 2022. The Daily 2022, 11-001-X. Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/220720/dq220720a-eng.pdf?st=k1YtyyTA (accessed on 14 August 2022).
- Adams, E. Can Scientists and Knowledge Keepers Sit Comfortably Together? An Indigenous Physician’s Reflections on a Decade of Participatory Research into First Nations Nutrition, Environment, and Health. Can. J. Public Health 2021, 112, 3–7. [Google Scholar] [CrossRef]
- Health Canada. Canada’s Dietary Guidelines for Health Professionals and Policy Makers; Minister of Health: Ottawa, ON, Canada, 2019.
| Variables | n (%) |
|---|---|
| Age (years) | |
| Younger than 30 | 11 (34.3) |
| Between 31 and 40 | 6 (18.8) |
| Between 41 and 50 | 8 (25.0) |
| Over 50 | 7 (21.9) |
| Gender | |
| Women | 25 (78.1) |
| Men | 7 (21.9) |
| Marital status | |
| Single (separated, divorced or widowed) | 14 (43.8) |
| In relationship (common law relationship or married) | 18 (56.2) |
| Highest Attained Education | |
| Elementary school | 7 (21.9) |
| High school diploma | 9 (28.1) |
| College/university degree | 16 (50.0) |
| Income (CAD $) | |
| <20,000 | 13 (40.6) |
| 20,000–39,999 | 8 (25.0) |
| 40,000–59,999 | 3 (9.4) |
| 60,000–79,999 | 1 (3.1) |
| More than 80,000 | 5 (15.6) |
| Prefer not to answer | 2 (6.3) |
| Number of children | |
| None | 10 (31.2) |
| 1–2 | 10 (31.2) |
| 3–4 | 7 (21.9) |
| More than 4 | 5 (15.6) |
| Job situation | |
| Unemployed (included sick or pregnancy leave, retired) | 7 (21.9) |
| Student | 4 (12.5) |
| Employed | 21 (65.6) |
| Indigenous origin | |
| Waban-Aki | 6 (18.8) |
| Algonquian | 4 (12.5) |
| Atikamekw Nehirowisiwok | 18 (56.2) |
| Cree | 1 (3.1) |
| Innu | 3 (9.4) |
| Compliance with Canadian Daily Recommendations | n (%) |
|---|---|
| Fuits and vegetables | 11 (34.4%) |
| Grain products | 4 (12.5%) |
| Milk and alternatives | 26 (81.3%) |
| Meat and alternatives | 29 (90.6%) |
| Type of Motivation | α | M | SD |
|---|---|---|---|
| 1. Intrinsic motivation | 0.84 | 4.89 | 1.56 |
| 2. Identified motivation | 0.86 | 5.70 | 1.20 |
| 3. Introjected motivation | 0.73 | 2.94 | 1.41 |
| 4. External motivation | 0.79 | 2.61 | 1.51 |
| 5. Amotivation | 0.76 | 1.91 | 1.06 |
| Weekly PA Practice during Leisure Time According to Intensity | Weekly M in Minutes M (SD) | Average Accessibility M (SD) |
|---|---|---|
| Low-intensity PA | 258 (579) | 6.6 (0.98) |
| Moderate-intensity PA | 104 (154) | 5.3 (1.69) |
| High-intensity PA | 46 (79) | 4.3 (2.18) |
| Type of Motivation | α | M | SD |
|---|---|---|---|
| 1. Intrinsic motivation | 0.94 | 3.16 | 0.90 |
| 2. Identified motivation | 0.61 | 2.89 | 0.67 |
| 3. Introjected motivation | 0.70 | 1.69 | 1.17 |
| 4. External motivation | 0.86 | 0.95 | 0.93 |
| 5. Amotivation | 0.48 | 0.48 | 0.59 |
| Variables | n (%) |
|---|---|
| Age (years) | |
| Younger than 30 | 5 (35.7) |
| Between 31 and 40 | 1 (7.1) |
| Between 41 and 50 | 4 (28.6) |
| Over 50 | 4 (28.6) |
| Gender | |
| Women | 7 (50.0) |
| Men | 7 (50.0) |
| Marital status | |
| Single (separated, divorced or widowed) | 9 (64.3) |
| In relationship (common law relationship or married) | 5 (35.7) |
| Highest Attained Education | |
| Elementary school | 2 (14.3) |
| High school diploma | 2 (14.3) |
| College/university degree | 10 (71.4) |
| Income (CAD $) | |
| <20,000 | 7 (50.0) |
| 20,000–39,999 | 1 (7.1) |
| 40,000–59,999 | 4 (28.6) |
| 60,000–79,999 | 1 (7.1) |
| More than 80,000 | 1 (7.1) |
| Number of children | |
| None | 4 (28.6) |
| 1–2 | 6 (42.8) |
| 3–4 | 2 (14.3) |
| More than 4 | 2 (14.3) |
| Job situation | |
| Unemployed (included sick or pregnancy leave, retired) | 5 (35.7) |
| Student | 1 (7.1) |
| Employed | 8 (57.1) |
| Indigenous origin | |
| Waban-Aki | 2 (14.3) |
| Atikamekw Nehirowisiwok | 8 (57.1) |
| Innu | 4 (28.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leclerc, A.-M.; Boulanger, M.; Miquelon, P.; Rivard, M.-C. First Nations Peoples’ Eating and Physical Activity Behaviors in Urban Areas: A Mixed-Methods Approach. Int. J. Environ. Res. Public Health 2022, 19, 10390. https://doi.org/10.3390/ijerph191610390
Leclerc A-M, Boulanger M, Miquelon P, Rivard M-C. First Nations Peoples’ Eating and Physical Activity Behaviors in Urban Areas: A Mixed-Methods Approach. International Journal of Environmental Research and Public Health. 2022; 19(16):10390. https://doi.org/10.3390/ijerph191610390
Chicago/Turabian StyleLeclerc, Anne-Marie, Maude Boulanger, Paule Miquelon, and Marie-Claude Rivard. 2022. "First Nations Peoples’ Eating and Physical Activity Behaviors in Urban Areas: A Mixed-Methods Approach" International Journal of Environmental Research and Public Health 19, no. 16: 10390. https://doi.org/10.3390/ijerph191610390
APA StyleLeclerc, A.-M., Boulanger, M., Miquelon, P., & Rivard, M.-C. (2022). First Nations Peoples’ Eating and Physical Activity Behaviors in Urban Areas: A Mixed-Methods Approach. International Journal of Environmental Research and Public Health, 19(16), 10390. https://doi.org/10.3390/ijerph191610390






