Construct Validity of a New Health Assessment Questionnaire for the National Screening Program of Older Adults in Japan: The SONIC Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. The Health Assessment Questionnaire for Old-Old Adults
2.3. Basic Characteristics of the Participants
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
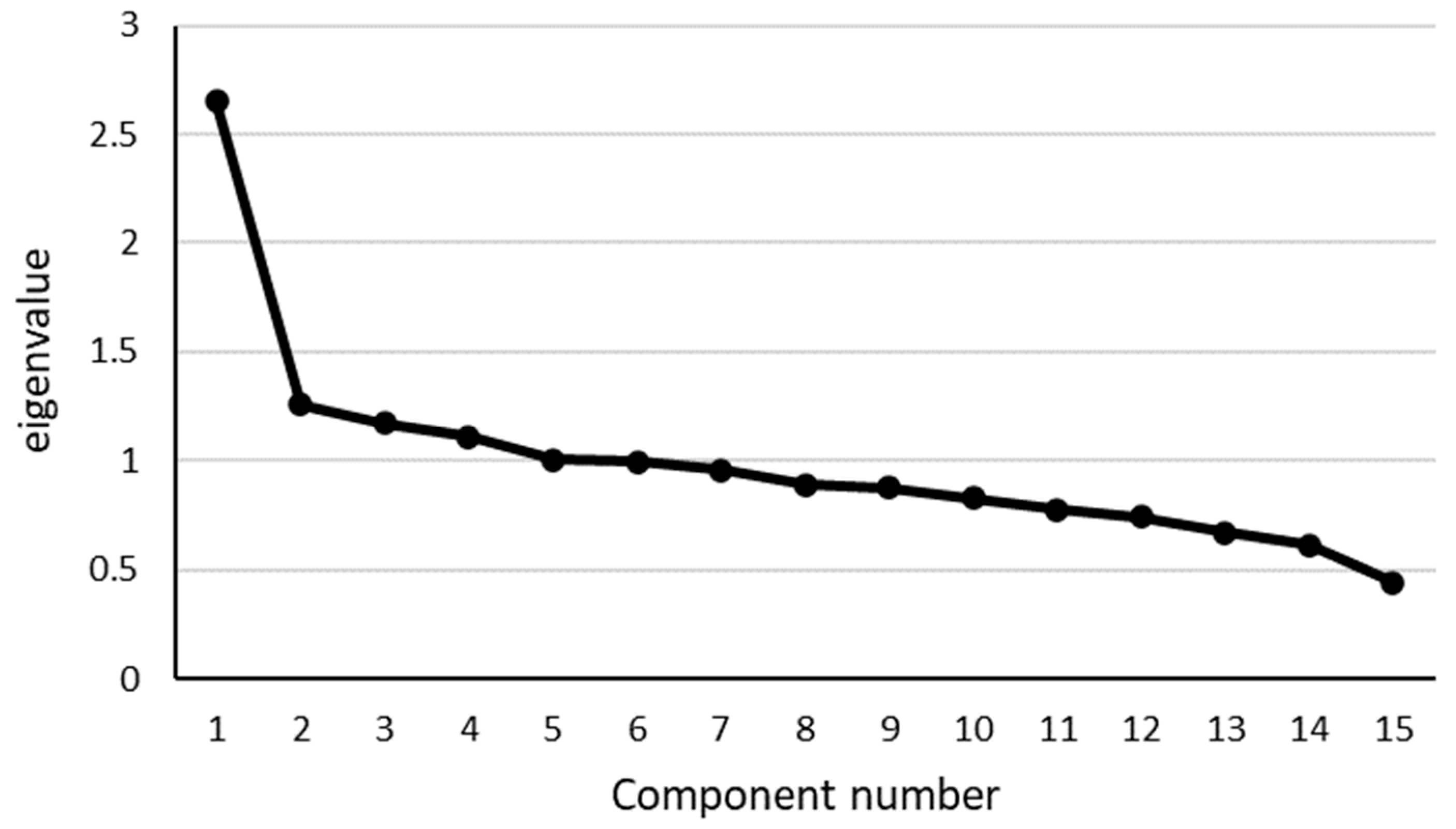
3.2. EFA
3.3. CFA
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fukuma, S.; Iizuka, T.; Ikenoue, T.; Tsugawa, Y. Association of the National Health Guidance Intervention for Obesity and Cardiovascular Risks with Health Outcomes among Japanese Men. JAMA Intern. Med. 2020, 180, 1630–1637. [Google Scholar] [CrossRef] [PubMed]
- Mitsutake, S.; Ishizaki, T.; Teramoto, C.; Shimizu, S.; Ito, H. Patterns of Co-Occurrence of Chronic Disease among Older Adults in Tokyo, Japan. Prev. Chronic Dis. 2019, 16, E11. [Google Scholar] [CrossRef] [PubMed]
- Ishizaki, T.; Mitsutake, S.; Hamada, S.; Teramoto, C.; Shimizu, S.; Akishita, M.; Ito, H. Drug Prescription Patterns and Factors Associated with Polypharmacy in >1 Million Older Adults in Tokyo. Geriatr. Gerontol. Int. 2020, 20, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Mitsutake, S.; Ishizaki, T.; Tsuchiya-Ito, R.; Teramoto, C.; Shimizu, S.; Yamaoka, T.; Kitamura, A.; Ito, H. Association of Pharmacological Treatments for Hypertension, Diabetes, and Dyslipidemia with Health Checkup Participation and Identification of Disease Control Factors Among Older Adults in Tokyo, Japan. Prev. Med. Rep. 2020, 17, 101033. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare, Japan. Guideline for Public Health Program for Older Adults; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2019. (In Japanese) [Google Scholar]
- Kim, H.K.; Ishizaki, T. Prevention Strategy for Frailty. In Health Issues and Care System for the Elderly, Current Topics in Environmental Health and Preventive Medicine; Washio, M., Kiyohara, C., Eds.; Springer: Singapore, 2019; pp. 45–68. ISBN 978-981-13-1761-3. [Google Scholar]
- Satake, S.; Arai, H. Questionnaire for Medical Checkup of Old-Old (QMCOO). Geriatr. Gerontol. Int. 2020, 20, 991–992. [Google Scholar] [CrossRef]
- Ishizaki, T. Integrated Implementation of Public Health Program and Long-Term Care Needs Prevention of Older Adults. Kokuho Miyagi 2020, 242, 8–10. (In Japanese) [Google Scholar]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A.; Higuchi, D. Construct Validity of the Questionnaire for Older Senior Citizens Based on A Confirmatory Factor Analysis: A Study During the Period of Self-restraint to Prevent the Spread of Coronavirus Disease 2019. Geriatr. Gerontol. Int. 2021, 21, 1018–1025. [Google Scholar] [CrossRef]
- Guadagnoli, E.; Velicer, W.F. Relation of Sample Size to the Stability of Component Patterns. Psychol. Bull. 1988, 103, 265–275. [Google Scholar] [CrossRef]
- Gondo, Y.; Masui, Y.; Kamide, K.; Ikebe, K.; Arai, Y.; Ishizaki, T. A Longitudinal Cohort Study of The Older People as Part of A Centenarian Study. In Encyclopedia of Geropsychology; Pachana, N.A., Ed.; Springer: Singapore, 2016; ISBN 978-981-28-7081-0. [Google Scholar]
- Koyano, W.; Shibata, H.; Nakazato, K.; Haga, H.; Suyama, Y. Measurement of Competence: Reliability and Validity of The TMIG Index of Competence. Arch. Gerontol. Geriatr. 1991, 13, 103–116. [Google Scholar] [CrossRef]
- Tsutsui, T.; Muramatsu, N. Care-Needs Certification in the Long-Term Care Insurance System of Japan. J. Am. Geriatr. Soc. 2005, 53, 522–527. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis; SAGE: Thousand Oaks, CA, USA, 2003; ISBN 0-7619-1950-3. [Google Scholar]
- de Vries, N.M.; Staal, J.B.; van Ravensberg, C.D.; Hobbelen, J.S.; Olde Rikkert, M.G.; Nijhuis-van der Sanden, M.W. Outcome instruments to measure frailty: A systematic review. Ageing Res. Rev. 2011, 10, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, D.; O’Donovan, M.; Cornally, N.; Liew, A.; O’Caoimh, R. Defining frailty for healthcare practice and research: A qualitative systematic review with thematic analysis. Int. J. Nurs. Stud. 2019, 92, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Gabrovec, B.; Veninšek, G.; Samaniego, L.L.; Carriazo, A.M.; Antoniadou, E.; Jelenc, M. The role of nutrition in ageing: A narrative review from the perspective of the European joint action on frailty—ADVANTAGE JA. Eur. J. Intern. Med. 2018, 56, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Parisius, K.G.H.; Wartewig, E.; Schoonmade, L.J.; Aarab, G.; Gobbens, R.; Lobbezoo, F. Oral frailty dissected and conceptualized: A scoping review. Arch. Gerontol. Geriatr. 2022, 100, 104653. [Google Scholar] [CrossRef] [PubMed]
- Blunch, N.J. Introduction to Structural Equation Modeling Using IBM SPSS Statistics and AMOS; SAGE: London, UK, 2013. [Google Scholar]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of Frailty: Opportunities, Challenges, And Future Directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Steverink, N.S.J.; Schuurmans, H.; van Lis, M. Measuring Frailty: Developing and Testing of the Groningen Frailty Indicator (GFI). Gerontologists 2001, 41, 236–237. [Google Scholar]
- Bieldermanm, A.; van der Schansm, C.P.; van Lieshout, M.R.; de Greef, M.H.; Boersma, F.; Krijnen, W.P.; Steverink, N. Multidimensional Structure of the Groningen Frailty Indicator in Community-Dwelling Older People. BMC Geriatr. 2013, 13, 86. [Google Scholar]
- Peters, L.L.; Boter, H.; Burgerhof, J.G.; Slaets, J.P.; Buskens, E. Construct validity of the Groningen Frailty Indicator established in a large sample of home-dwelling elderly persons: Evidence of stability across age and gender. Exp. Gerontol. 2015, 69, 129–141. [Google Scholar] [CrossRef]
- Rolfson, D.B.; Majumdar, S.R.; Tsuyuki, R.T.; Tahir, A.; Rockwood, K. Validity and reliability of the Edmonton Frail Scale. Age Ageing 2006, 35, 526–529. [Google Scholar] [CrossRef]
- Perna, S.; Francis, M.D.; Bologna, C.; Moncaglieri, F.; Riva, A.; Morazzoni, P.; Allegrini, P.; Isu, A.; Vigo, B.; Guerriero, F.; et al. Performance of Edmonton Frail Scale on frailty assessment: Its association with multi-dimensional geriatric conditions assessed with specific screening tools. BMC Geriatr. 2017, 17, 2. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. The Tilburg Frailty Indicator: Psychometric Properties. J. Am. Med Dir. Assoc. 2010, 11, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tan, S.S.; Bilajac, L.; Alhambra-Borrás, T.; Garcés-Ferrer, J.; Verma, A.; Koppelaar, E.; Markaki, A.; Mattace-Raso, F.; Franse, C.B.; et al. Reliability and Validity of the Tilburg Frailty Indicator in 5 European Countries. J. Am. Med Dir. Assoc. 2020, 21, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Sánchez, J.J.; Urpí-Fernández, A.M.; Sastre-Rus, M.; Lumillo-Gutiérrez, I.; Gea-Caballero, V.; Jodar-Fernández, L.; Julián-Rochina, I.; Zabaleta-Del-Olmo, E. The Tilburg Frailty Indicator: A psychometric systematic review. Ageing Res. Rev. 2022, 76, 101588. [Google Scholar] [CrossRef] [PubMed]
- Arai, H.; Satake, S. English Translation of The Kihon Checklist. Geriatr. Gerontol. Int. 2015, 15, 518–519. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for Assessing Frailty Status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Shinkai, S.; Yoshida, H.; Taniguchi, Y.; Murayama, H.; Nishi, M.; Amano, H.; Nofuji, Y.; Seino, S.; Fujiwara, Y. Public Health Approach to Preventing Frailty in The Community and its Effect on Healthy Aging in Japan. Geriatr. Gerontol. Int. 2016, 16 (Suppl. S1), 87–97. [Google Scholar] [CrossRef]
- Daniels, R.; van Rossum, E.; Beurskens, A.; van den Heuvel, W.; de Witte, L. The predictive validity of three self-report screening instruments for identifying frail older people in the community. BMC Public Health 2012, 12, 69. [Google Scholar] [CrossRef]
- Si, H.; Jin, Y.; Qiao, X.; Tian, X.; Liu, X.; Wang, C. Comparing diagnostic properties of the FRAIL-NH Scale and 4 frailty screening instruments among Chinese institutionalized older adults. J. Nutr. Health Aging 2020, 24, 188–193. [Google Scholar] [CrossRef]
- Brundle, C.; Heaven, A.; Brown, L.; Teale, E.; Young, J.; West, R.; Clegg, A. Convergent validity of the electronic frailty index. Age Ageing 2019, 48, 152–156. [Google Scholar] [CrossRef]
- Ambagtsheer, R.C.; Visvanathan, R.; Dent, E.; Yu, S.; Schultz, T.J.; Beilby, J. Commonly used screening instruments to identify frailty among community-dwelling older people in a general practice (primary care) setting: A study of diagnostic test accuracy. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1134–1142. [Google Scholar] [CrossRef]
- Kojima, G.; Taniguchi, Y.; Kitamura, A.; Shinkai, S. Are the Kihon Checklist and the Kaigo-Yobo Checklist Compatible with the Frailty Index? J. Am. Med Dir. Assoc. 2018, 19, 797–800. [Google Scholar] [CrossRef] [PubMed]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Ogita, M.; Arai, H. Validation and translation of the Kihon Checklist (frailty index) into Brazilian Portuguese. Geriatr. Gerontol. Int. 2014, 14, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare, Japan. National Survey of Implementation Status of the Public Health Program for Old-Old Adults in 2021; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2022. (In Japanese) [Google Scholar]
- All-Japan Federation of National Health Insurance Organizations. Kokuho Database (KDB) System. Available online: https://www.kokuho.or.jp/hoken/kdb.html (accessed on 18 July 2022).

| Domain | Item | Score |
|---|---|---|
| Health condition | 1. How is your health condition? | Excellent = 0; good = 1; fair = 2; poor = 3; very poor = 4 |
| Mental health | 2. Are you satisfied with your daily life? | Satisfied = 0; moderately satisfied = 1; moderately dissatisfied = 2; dissatisfied = 3 |
| Eating behavior | 3. Do you eat three meals a day? | Yes = 0; no = 1 |
| Oral function | 4. Do you have any difficulties eating tough foods when compared to 6 months ago? | No = 0; yes = 1 |
| 5. Have you choked on your tea or soup recently? | No = 0; yes = 1 | |
| Bodyweight loss | 6. Have you lost 2 kg or more in the past 6 months? | No = 0; yes = 1 |
| Physical function and falls | 7. Do you think you walk slower than before? | No = 0; yes = 1 |
| 8. Have you experienced a fall in the past year? | No = 0; yes = 1 | |
| 9. Do you go for a walk for your health at least once a week? | Yes = 0; no = 1 | |
| Cognitive function | 10. Do your family or friends point out your memory loss? (e.g., “You ask the same questions over and over again.”) | No = 0; yes = 1 |
| 11. Do you find yourself not knowing today’s date? | No = 0; yes = 1 | |
| Smoking | 12. Do you smoke? | Yes = 2; no = 0; I quit = 1 |
| Social participation and support | 13. Do you go out at least once a week? | Yes = 0; no = 1 |
| 14. Do you maintain regular communications with your family and friends? | Yes = 0; no = 1 | |
| 15. When you feel ill, do you have anyone to reach out/talk to? | Yes = 0; no = 1 |
| Total | Men | Women | |
|---|---|---|---|
| n = 1576 | n = 742 | n = 834 | |
| Mean age (standard deviation) (years) | 85.6 (5.9) | 85.7 (5.9) | 85.4 (5.9) |
| Educational attainment (years) (mean (SD)) | 11.6 (2.8) | 12.1 (3.1) | 11.2 (2.3) |
| Place of living (% home) | 95.1% | 95.8% | 94.4% |
| Living arrangement (% living alone) | 26.2% | 15.1% | 36.1% |
| LTC need certification (% LTC need Level 1 or more) | 10.6% | 10.0% | 11.0% |
| Instrumental activities of daily living (points) (mean (SD)) | 4.6 (1.3) | 4.3 (1.3) | 4.4 (1.3) |
| Total (n = 1576) | Men (n = 742) | Women (n = 834) | 70s Group (n = 733) | 80s Group (n = 509) | 90s Group (n = 334) | |
|---|---|---|---|---|---|---|
| 1. How is your health condition? | 1.61 (0.98) | 1.56 (1.00) | 1.65 (0.96) | 1.50 (0.98) | 1.70 (0.95) | 1.72 (1.00) |
| 2. Are you satisfied with your daily life? | 0.82 (0.70) | 0.80 (0.69) | 0.84 (0.72) | 0.85 (0.68) | 0.79 (0.72) | 0.78 (0.74) |
| 3. Do you eat three meals a day? | 0.06 (0.24) | 0.05 (0.22) | 0.07 (0.25) | 0.04 (0.19) | 0.07 (0.26) | 0.10 (0.30) |
| 4. Do you have any difficulties eating tough foods when compared to 6 months ago? | 0.32 (0.47) | 0.28 (0.45) | 0.35 (0.48) | 0.24 (0.43) | 0.36 (0.48) | 0.42 (0.49) |
| 5. Have you choked on your tea or soup recently? | 0.22 (0.42) | 0.20 (0.40) | 0.25 (0.43) | 0.21 (0.41) | 0.22 (0.41) | 0.27 (0.44) |
| 6. Have you lost 2 kg or more in the past 6 months? | 0.17 (0.37) | 0.17 (0.38) | 0.16 (0.37) | 0.13 (0.34) | 0.19 (0.39) | 0.21 (0.41) |
| 7. Do you think you walk slower than before? | 0.74 (0.44) | 0.73 (0.44) | 0.74 (0.44) | 0.64 (0.48) | 0.79 (0.41) | 0.86 (0.35) |
| 8. Have you experienced a fall in the past year? | 0.25 (0.44) | 0.25 (0.43) | 0.26 (0.44) | 0.19 (0.39) | 0.26 (0.44) | 0.38 (0.49) |
| 9. Do you go for a walk for your health at least once a week? | 0.43 (0.50) | 0.42 (0.50) | 0.43 (0.50) | 0.34 (0.48) | 0.47 (0.50) | 0.55 (0.50) |
| 10. Do your family or friends point out your memory loss? (e.g., “You ask the same questions over and over again.”) | 0.17 (0.38) | 0.17 (0.38) | 0.17 (0.38) | 0.10 (0.30) | 0.20 (0.40) | 0.30 (0.46) |
| 11. Do you find yourself not knowing today’s date? | 0.31 (0.46) | 0.30 (0.46) | 0.33 (0.47) | 0.24 (0.43) | 0.33 (0.47) | 0.44 (0.50) |
| 12. Do you smoke? | 0.25 (0.51) | 0.46 (0.60) | 0.06 (0.31) | 0.30 (0.57) | 0.17 (0.42) | 0.25 (0.48) |
| 13. Do you go out at least once a week? | 0.17 (0.38) | 0.16 (0.37) | 0.18 (0.39) | 0.09 (0.29) | 0.20 (0.41) | 0.28 (0.45) |
| 14. Do you maintain regular communications with your family and friends? | 0.06 (0.25) | 0.09 (0.28) | 0.04 (0.21) | 0.05 (0.21) | 0.07 (0.25) | 0.10 (0.30) |
| 15. When you feel ill, do you have anyone to reach out/talk to? | 0.06 (0.23) | 0.07 (0.25) | 0.05 (0.22) | 0.06 (0.25) | 0.06 (0.24) | 0.04 (0.20) |
| Items | F1 | F2 | F3 | F4 | F5 | Estimated Communality |
|---|---|---|---|---|---|---|
| 1. How is your health condition? (reversed) | 0.80 | 0.07 | 0.07 | −0.03 | −0.03 | 0.72 |
| 2. Are you satisfied with your daily life? (reversed) | 0.65 | −0.03 | −0.06 | 0.05 | 0.05 | 0.40 |
| 13. Do you go out at least once a week? (reversed) | 0.00 | 0.71 | −0.04 | −0.03 | −0.06 | 0.44 |
| 9. Do you go for a walk for your health at least once a week? (reversed) | 0.05 | 0.39 | 0.02 | 0.00 | 0.00 | 0.18 |
| 4. Do you have any difficulties eating tough foods when compared to 6 months ago? | −0.04 | −0.02 | 0.44 | −0.03 | −0.03 | 0.15 |
| 5. Have you choked on your tea or soup recently? | −0.04 | 0.03 | 0.36 | 0.03 | −0.05 | 0.13 |
| 6. Have you lost 2 kg or more in the past six months? | 0.08 | −0.13 | 0.31 | −0.03 | 0.13 | 0.13 |
| 7. Do you think you walk slower than before? | 0.11 | 0.04 | 0.28 | 0.02 | 0.00 | 0.15 |
| 8. Have you experienced a fall in the past year? | 0.01 | 0.09 | 0.21 | 0.08 | 0.02 | 0.11 |
| 10. Do your family or friends point out your memory loss? (e.g., “You ask the same questions over and over again.”) | −0.02 | 0.00 | 0.04 | 0.63 | −0.10 | 0.40 |
| 11. Do you find yourself not knowing today’s date? | 0.05 | −0.03 | −0.03 | 0.54 | 0.07 | 0.30 |
| 15. When you feel ill, do you have someone to reach out/talk to? (reversed) | 0.08 | −0.06 | −0.11 | 0.00 | 0.53 | 0.27 |
| 14. Do you maintain regular communications with your family and friends? (reversed) | −0.10 | 0.19 | 0.05 | 0.04 | 0.42 | 0.27 |
| 3. Do you eat three meals a day? (reversed) | −0.02 | 0.03 | 0.16 | −0.01 | 0.23 | 0.11 |
| 12. Do you smoke? | 0.00 | −0.07 | 0.03 | −0.05 | 0.15 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishizaki, T.; Masui, Y.; Nakagawa, T.; Yoshida, Y.; Ishioka, Y.L.; Hori, N.; Inagaki, H.; Ito, K.; Ogawa, M.; Kabayama, M.; et al. Construct Validity of a New Health Assessment Questionnaire for the National Screening Program of Older Adults in Japan: The SONIC Study. Int. J. Environ. Res. Public Health 2022, 19, 10330. https://doi.org/10.3390/ijerph191610330
Ishizaki T, Masui Y, Nakagawa T, Yoshida Y, Ishioka YL, Hori N, Inagaki H, Ito K, Ogawa M, Kabayama M, et al. Construct Validity of a New Health Assessment Questionnaire for the National Screening Program of Older Adults in Japan: The SONIC Study. International Journal of Environmental Research and Public Health. 2022; 19(16):10330. https://doi.org/10.3390/ijerph191610330
Chicago/Turabian StyleIshizaki, Tatsuro, Yukie Masui, Takeshi Nakagawa, Yuko Yoshida, Yoshiko L. Ishioka, Noriko Hori, Hiroki Inagaki, Kae Ito, Madoka Ogawa, Mai Kabayama, and et al. 2022. "Construct Validity of a New Health Assessment Questionnaire for the National Screening Program of Older Adults in Japan: The SONIC Study" International Journal of Environmental Research and Public Health 19, no. 16: 10330. https://doi.org/10.3390/ijerph191610330
APA StyleIshizaki, T., Masui, Y., Nakagawa, T., Yoshida, Y., Ishioka, Y. L., Hori, N., Inagaki, H., Ito, K., Ogawa, M., Kabayama, M., Kamide, K., Ikebe, K., Arai, Y., & Gondo, Y. (2022). Construct Validity of a New Health Assessment Questionnaire for the National Screening Program of Older Adults in Japan: The SONIC Study. International Journal of Environmental Research and Public Health, 19(16), 10330. https://doi.org/10.3390/ijerph191610330







