Temperature Asymmetry Analysis between Left and Right Wrist with Sensory and Infrared Thermography
Abstract
:1. Introduction
Study Justification
2. Materials and Methods
2.1. Stage One: Sampling
2.2. Stage Two: Obtaining the Information
2.3. Stage Three: Protocol
- A personal computer with Intel Core i5 (3rd Gen) 3340 M at 2.7 GHz with 4 Gb of DDR3 SDRAM memory.
- A sensor at 1600 MHz; two calibrated Sköll sensory thermographs (Ensenada, BC, Mexico), based on an NTC thermistor, whose resistance is highly dependent on temperature, with a range of 0 to 40 °C, precision ± 0.3 °C, resolution of 0.1 °C to collect the data [5].
- For programming the sensory thermographs, the Akela program is used (Longmont, CO, USA).
- Program the Sköll thermographs using the Akela program.
- Once the pertinent information was collected, the ambient temperature in the study laboratory was taken to maintain it in an ideal range of 20–25 °C [43,44,45]. Although it is a wide temperature range, according to information from the company’s human resources department, these are the real conditions where operators perform operations on the production lines.
- After the stabilization time, the operator was asked to sit in a chair, and the Sköll thermographs were immediately placed on both hands, specifically on the wrist area (in the region of the median nerve). Once the Sköll thermographs were placed, the operator was asked to rest his arms on a flat table adjusted to the height of the ribs for a space of 20 min and with a pelvic angle of 90° [44]. This is done at the beginning and the end of the test.
- Place the Sköll thermographs on the wrist area (on the left and right hand).
- Emulation of assembling the cuff of a t-shirt is a highly repetitive operation carried out in the company for one hour.
- Surveillance and identification during the test about anomalies or pain presented by the operators.
- Withdrawal of the Sköll thermographers and concentration of the data obtained in Microsoft® Office Excel for manipulation and interpretation.
- An infrared thermography camera Thermal brand FLIR® (Wilsonville, OR, USA) E25 (Longwave IR camera at 7.5 to 13 µm spectral range, Focal Plane Array sensor of 160 × 120, Noise Equivalent Temperature Difference of <100 mK at 30 °C and measurement uncertainty of ± 2% of overall reading) was used. The camera was calibrated by the FLIR company according to a standard calibration to manufacturer specifications and with 17,025 accreditations, because they are the only ones accredited to do that.
- The images were analyzed with the FLIR® ThermaCAM Researcher Pro software v.2.10 from Teledyne FLIR company at Wilsonville OR (USA), which allows the drawing of regions of interest (ROI) and extracting the average temperatures from them. The ROIs used were the inner canthi of the eyes (for estimating body core temperature [20]), hands, and fingers.
- People were chosen to participate voluntarily in the emulated tests. A vital characteristic to consider was that they would be participants of productive age and all participants were registered in a database to keep track of them.
- In the laboratory where the tests were carried out, the temperature was controlled between 20 to 25 °C, and the relative humidity did not exceed 50% [42,46,47,48], replicating real factory conditions. For the IRT tests, the emissivity of the chamber was kept at 98%, which is the value for human skin [49,50].
- Each participant would be assigned approximately one hour to take the thermographic images. Thermograms were taken and recorded in a database.
- They explained the movement they had to carry out in which they emulated the movements of the operators of the manufacturing company for 10 min winding cables, which involved the 10 fingers of the hand. A thermogram was taken before starting the task, and the hands maintained the same position on a base (see Figure 2) after 10 min at the end of the repetitive activity. The hands were then kept at rest, and temperatures were recorded at 15 and 20 min.
2.4. Stage Four: Information Analysis
3. Results
3.1. Sample Descriptives
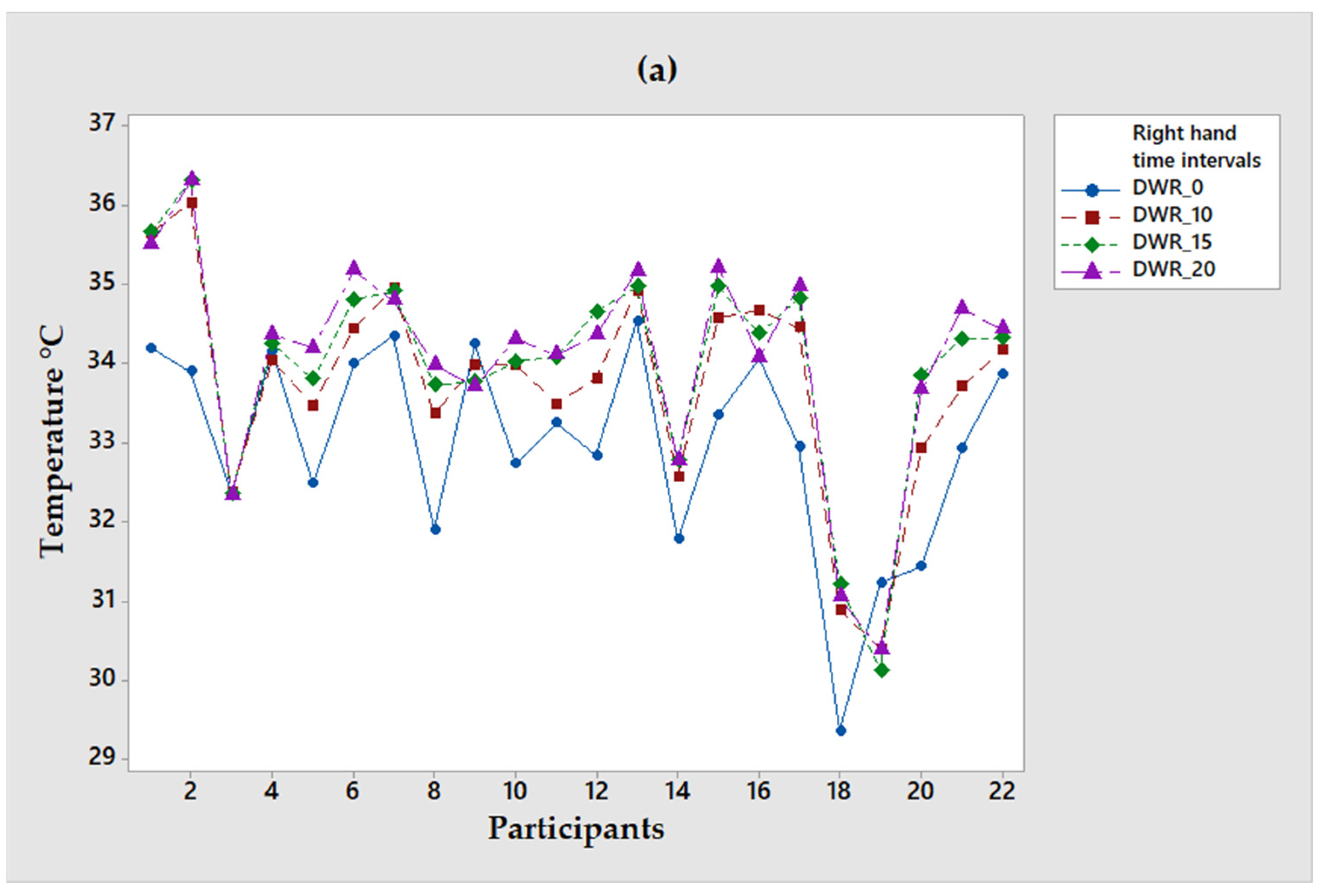
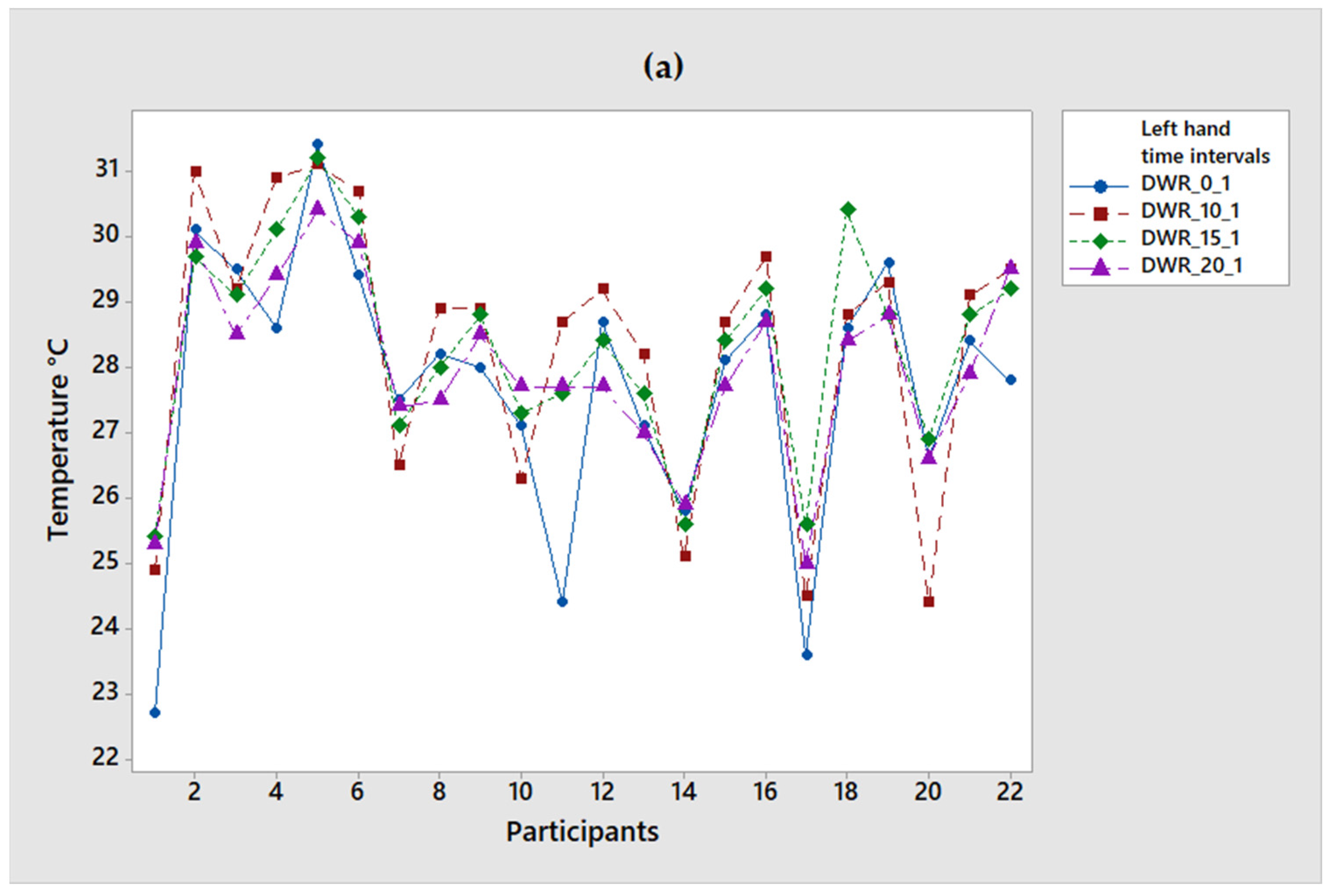
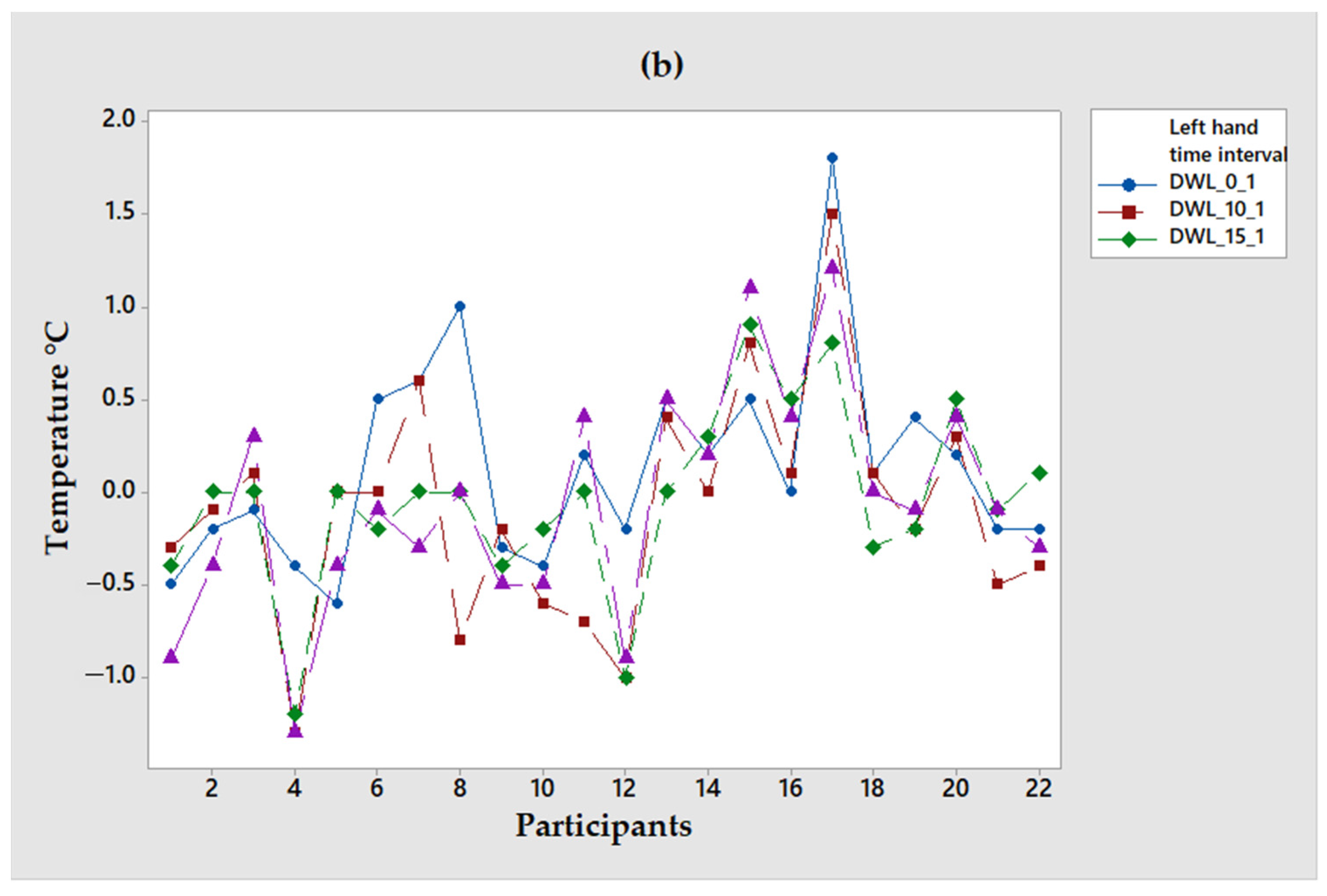
3.2. Statistical Analysis of Both Groups with the Two Techniques
3.3. Qualitative Comparison of the Two Techniques
4. Discussion and Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Andrade Fernandes, A.; dos Santos Amorim, P.R.; Brito, C.J.; De Moura, A.G.; Moreira, D.G.; Costa, C.M.A.; Sillero-Quintana, M.; Marins, J.C.B. Measuring skin temperature before, during and after exercise: A comparison of thermocouples and infrared thermography. Physiol. Meas. 2014, 35, 189–203. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.F.; Plassmann, P. Digital infrared thermal imaging of human skin. IEEE Eng. Med. Biol. Mag. 2002, 21, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Tortora, G.J.; Derrickson, B.H. Principles of Anatomy and Physiology; John Wiley & Sons: Hoboken, NJ, USA, 2018. [Google Scholar]
- Vardasca, R.Â.R. The Effect of Work Related Mechanical Stress on the Peripheral Temperature of the Hand; University of South Wales: Cardiff, UK, 2010. [Google Scholar]
- Camargo-Wilson, C. Temperature Prediction Models in the Wrist Area through Sensorial Thermography (In Spanish). Ph.D. Thesis, Autonomous University of Baja California, Ensenada, México, 2013. Available online: https://repositorioinstitucional.uabc.mx/bitstream/20.500.12930/68/1/ENS074076.pdf (accessed on 20 May 2022).
- Hardy, J.D.; Muschenheim, C. The radiation of heat from the human body. J. Clin. Investig. 1934, 13, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Rajmanova, P.; Nudzikova, P.; Vala, D. Application and Technology of Thermal Imagine Camera in Medicine. IFAC-PapersOnLine 2015, 48, 492–497. [Google Scholar] [CrossRef]
- Camargo, C.; Enrique, J.; Olguín, J.E.; López, J.A. Application of Sensory Thermography on Workers with Carpal Tunnel Syndrome of a Textile Industry in Mexico. Adv. Soc. Organ. Factors 2014, 12, 479. [Google Scholar]
- Ammer, K. Diagnosis of Raynaud’s phenomenon by thermography. Ski. Res. Technol. 1996, 2, 182–185. [Google Scholar] [CrossRef]
- Ring, E.F.J.; Ammer, K. Infrared thermal imaging in medicine. Physiol. Meas. 2012, 33, R33–R46. [Google Scholar] [CrossRef]
- Sousa, E.; Vardasca, R.; Teixeira, S.; Seixas, A.; Mendes, J.; Costa-Ferreira, A. A review on the application of medical infrared thermal imaging in hands. Infrared Phys. Technol. 2017, 85, 315–323. [Google Scholar] [CrossRef]
- Medica, E.M. Musculoskeletal applications of infrared thermography on back and neck syndromes: Systematic review. Eur. J. Phys. Rehabil. Med. 2020, 57, 386–396. [Google Scholar] [CrossRef]
- Ming, Z.; Zaproudina, N.; Siivola, J.; Nousiainen, U.; Pietikainen, S. Sympathetic pathology evidenced by hand thermal anomalies in carpal tunnel syndrome. Pathophysiology 2005, 12, 137–141. [Google Scholar] [CrossRef]
- Herrick, R.T.; Herrick, S.K. Thermography in the detection of carpal tunnel syndrome and other compressive neuropathies. J. Hand Surg. 1987, 12, 943–949. [Google Scholar] [CrossRef]
- Esmaeilzadeh, S.; Ozcan, E.; Capan, N. Effects of ergonomic intervention on work-related upper extremity musculoskeletal disorders among computer workers: A randomized controlled trial. Int. Arch. Occup. Environ. Health 2012, 87, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Palfy, M.; Papež, B.J. Diagnosis of Carpal Tunnel Syndrome from Thermal Images Using Artificial Neural Networks. In Proceedings of the twentieth IEEE International Symposium on Computer-Based Medical Systems (CBMS’07), Aveiro, Portugal, 20–22 June 2007; pp. 59–64. [Google Scholar]
- Cázares-Manríquez, M.A.; Camargo-Wilson, C.; Vardasca, R.; García-Alcaraz, J.L.; Olguín-Tiznado, J.E.; López-Barreras, J.A.; García-Rivera, B.R. Quantitative Models for Prediction of Cumulative Trauma Disorders Applied to the Maquiladora Industry. Int. J. Environ. Res. Public Health 2021, 18, 3830. [Google Scholar] [CrossRef] [PubMed]
- Vardasca, R.; Ring, E.; Plassmann, P.; Jones, C.D. Thermal symmetry of the upper and lower extremities in healthy subjects. Thermol. Int. 2012, 22, 53–60. [Google Scholar]
- Schuhfried, O.; Herceg, M.; Reichel-Vacariu, G.; Paternostro-Sluga, T. Infrared Thermographic Pattern of Lower Limb Complex Regional Pain Syndrome (Type I) and its Correlation with Pain, Disease Duration and Clinical Signs. Phys. Med. Rehabil. Kurortmed. 2016, 26, 288–292. [Google Scholar] [CrossRef]
- Suominen, S.; Asko-Seljavaara, S. Thermography of hands after a radial forearm flap has been raised. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1996, 30, 307–314. [Google Scholar] [CrossRef]
- Camargo, C.; Ordorica, J.; De la Vega, E.; Olguín, J.; López, O.; López, J. Analysis of temperature on the surface of the wrist due to repetitive movements using sensory thermography. Work 2012, 41 (Suppl. S1), 2569–2575. [Google Scholar] [CrossRef]
- Villalvazo, J.O.; Wilson, C.C.; Enrique, J.; Bonilla, O.R.L.; Tiznado, J.E.O.; Barreras, J.A.L. Validación de un sistema de medición aplicado a un estudio de termografía sensorial para la detección de desórdenes de traumas acumulados. Rev. Ing. Ind. 2011, 10, 69–84. [Google Scholar]
- Burbano, D.A.C. Desarrollo de un Sistema Multi-Sensorial Para la Medición de Variables Subacuáticas. Bachelor’s Thesis, Universidad del Valle, Cali, Colombia, 2012. Available online: http://hdl.handle.net/10893/15724 (accessed on 20 May 2022).
- Charlton, M.; Stanley, S.A.; Whitman, Z.; Wenn, V.; Coats, T.J.; Sims, M.; Thompson, J.P. The effect of constitutive pigmentation on the measured emissivity of human skin. PLoS ONE 2020, 15, e0241843. [Google Scholar] [CrossRef]
- Bouzida, N.; Bendada, A.; Maldague, X.P. Visualization of body thermoregulation by infrared imaging. J. Therm. Biol. 2009, 34, 120–126. [Google Scholar] [CrossRef]
- Merla, A.; Di Donato, L.; Farina, G.; Pisarri, S.; Proietti, M.; Salsano, F.; Romani, G.L. Study of Raynaud’s phenomenon by means of infrared functional imaging. In Proceedings of the 23rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Istanbul, Turkey, 25–28 October 2001; IEEE: New York, NY, USA, 2001; Volume 3, pp. 2856–2859. [Google Scholar]
- Amaro, A.M.; Paulino, M.F.; Neto, M.A.; Roseiro, L. Hand-Arm Vibration Assessment and Changes in the Thermal Map of the Skin in Tennis Athletes during the Service. Int. J. Environ. Res. Public Health 2019, 16, 5117. [Google Scholar] [CrossRef] [PubMed]
- Roldan, K.E.; Piedrahita, M.A.O.; Benitez, H.D. Spatial-temporal features of thermal images for Carpal Tunnel Syndrome detection. In Image Processing: Algorithms and Systems XII; International Society for Optics and Photonics: Bellingham, WA, USA, 2014; Volume 9019. [Google Scholar]
- Brioschi, M.L.; Okimoto, M.L.L.R.; Vargas, J.V.C. The utilization of infrared imaging for occupational disease study in industrial work. Work 2012, 41, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, D.; Prieto, M.; Beaumont, F.; Taiar, R.; Polidori, G. Wearing lead aprons in surgical operating rooms: Ergonomic injuries evidenced by infrared thermography. J. Surg. Res. 2017, 209, 227–233. [Google Scholar] [CrossRef]
- David, G.C. Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occup. Med. 2005, 55, 190–199. [Google Scholar] [CrossRef]
- Hutson, M. Work related upper limb disorders. Indian J. Rheumatol. 2014, 9, S6–S12. [Google Scholar] [CrossRef]
- Lasanen, R.; Malo, M.K.; Airaksinen, O.; Karhu, J.; Töyräs, J.; Julkunen, P. Infrared thermography reveals effect of working posture on skin temperature in office workers. Int. J. Occup. Saf. Ergon. 2017, 24, 457–463. [Google Scholar] [CrossRef]
- Madeleine, P.; Voigt, M.; Arendt-Nielsen, L. Subjective, physiological and biomechanical responses to prolonged manual work performed standing on hard and soft surfaces. Eur. J. Appl. Physiol. Occup. Physiol. 1997, 77, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Muggleton, J.; Allen, R.; Chappell, P. Hand and arm injuries associated with repetitive manual work in industry: A review of disorders, risk factors and preventive measures. Ergonomics 1999, 42, 714–739. [Google Scholar] [CrossRef]
- Tse, J.; Rand, C.; Carroll, M.; Charnay, A.; Gordon, S.; Morales, B.; Vitez, S.; Le, M.; Weese-Mayer, D. Determining peripheral skin temperature: Subjective versus objective measurements. Acta Paediatr. 2015, 105, e126–e131. [Google Scholar] [CrossRef]
- Vardasca, R. Symmetry of temperature distribution in the upper and lower extremities. Thermol. Int. 2008, 18, 154–155. [Google Scholar]
- Rossignoli, I.; Benito, P.J.; Herrero, A.J. Reliability of infrared thermography in skin temperature evaluation of wheelchair users. Spinal Cord 2014, 53, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Tchou, S.; Costich, J.F.; Burgess, R.C.; Wexler, C.E. Thermographic observations in unilateral carpal tunnel syndrome: Report of 61 cases. J. Hand Surg. 1992, 17, 631–637. [Google Scholar] [CrossRef]
- Ríos, M.M.; Chacón, E.M.; Fernández, A.C.; Guillén, E.O. Termografía infrarroja y el estudio de riesgos de lesiones músculo esqueléticas. Rev. Ing. Ind. 2011, 10, 55–67. [Google Scholar]
- Pichot, C. Aplicación de la termografía en el dolor lumbar crónico. Rev. Soc. Esp. Dolor 2001, 8, 43–47. [Google Scholar]
- Vecchio, P.C.; Adebajo, A.O.; Chard, M.D.; Thomas, P.P.; Hazleman, B.L. Thermography of frozen shoulder and rotator cuff tendinitis. Clin. Rheumatol. 1992, 11, 382–384. [Google Scholar] [CrossRef]
- Gold, J.E.; Cherniack, M.; Buchholz, B. Infrared thermography for examination of skin temperature in the dorsal hand of office workers. Eur. J. Appl. Physiol. 2004, 93, 245–251. [Google Scholar] [CrossRef]
- Gold, J.E.; Cherniack, M.; Hanlon, A.; Dennerlein, J.T.; Dropkin, J. Skin temperature in the dorsal hand of office workers and severity of upper extremity musculoskeletal disorders. Int. Arch. Occup. Environ. Health 2009, 82, 1281–1292. [Google Scholar] [CrossRef]
- Jiang, L.J.; Ng, E.Y.K.; Yeo, A.C.B.; Wu, S.; Pan, F.; Yau, W.Y.; Chen, J.H.; Yang, Y. A perspective on medical infrared imaging. J. Med. Eng. Technol. 2005, 29, 257–267. [Google Scholar] [CrossRef]
- Hunold, S.; Mietzsch, E.; Werner, J. Thermographic studies on patterns of skin temperature after exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 550–554. [Google Scholar] [CrossRef]
- Ammer, K.; Ring, E.F. Repeatability of the standard view both dorsal hands. Results from a training course on medical infrared imaging. Thermol. Int. 2004, 14, 100–103. [Google Scholar]
- Ring, E.; Ammer, K. The technique of infrared imaging in medicine. Thermol. Int. 2000, 10, 7–14. [Google Scholar]
- Fernández-Cuevas, I.; Marins, J.C.; Carmona, P.G.; García-Concepción, M.A.; Lastras, J.A.; Quintana, M.S. Reliability and reproducibility of skin temperature of overweight subjects by an infrared thermography software designed for human beings. Thermol. Int. 2012, 22, 95–96. [Google Scholar]
- Ng, Y.K.; Ung, L.N.; Ng, F.C.; Sim, E.L.S.J. Statistical analysis of healthy and malignant breast thermography. J. Med. Eng. Technol. 2001, 25, 253–263. [Google Scholar] [PubMed]
- Soares, A.L.; Xavier, A.A.D.P.; Michaloski, A.O. Occupational Risk Evaluation through Infrared Thermography: Development and Proposal of a Rapid Screening Tool for Risk Assessment Arising from Repetitive Actions of the Upper Limbs. Int. J. Environ. Res. Public Health 2020, 17, 3390. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Gonzálvez, P.; Rodríguez-Martín, M.; Rodríguez-Miró, I.; Fernández-Iglesias, S.; Bernal, M.Á.d.A.; Alvear-Ordenes, I. Technique to evaluate the thermoregulatory capacity before thermal stress. Application case of thermographic images to blood flow monitoring. In Proceedings of the Seventh International Conference on Technological Ecosystems for Enhancing Multiculturality, León, Spain, 16–18 October 2019; pp. 416–422. [Google Scholar]

| Group | Gender | N | Age | BMI | Fractures |
|---|---|---|---|---|---|
| Sensorial | F | 15 | 27.1 + 3.4 | 25.4 + 5.5 | 2 |
| M | 7 | 28.8 + 6.5 | 28 + 4.8 | 10 | |
| Infrared | F | 15 | 24.7 + 6.6 | 24.8 + 4.8 | 0 |
| M | 7 | 21.4 + 1.6 | 25.6 + 4.5 | 1 |
| Stretch Techniques | Gender | BMI | Fractures | |||||
|---|---|---|---|---|---|---|---|---|
| p | Decision | p | Conclusion | p | Decision | p | Conclusion | |
| WR_0 | 0 | Influential | 0.241 | Not influential | 0.12 | Not influential | 0.004 | Influential |
| WL_0 | 0 | Influential | 0.98 | Not influential | 0.07 | Not influential | 0.003 | Influential |
| WR_10 | 0 | Influential | 0.212 | Not influential | 0.198 | Not influential | 0.006 | Influential |
| WL_10 | 0 | Influential | 0.96 | Not influential | 0.066 | Not influential | 0.001 | Influential |
| WR_15 | 0 | Influential | 0.371 | Not influential | 0.185 | Not influential | 0.007 | Influential |
| WL_15 | 0 | Influential | 0.374 | Not influential | 0.103 | Not influential Not influential | 0.001 | Influential |
| WR_20 | 0 | Influential | 0.29 | Not influential | 0.149 | Not influential | 0.01 | Influential |
| WL_20 | 0 | Influential | 0.724 | Not influential | 0.09 | Not influential | 0.03 | Influential |
| Time | Average Temperature °C | |
|---|---|---|
| Right | Left | |
| 0 | 30.4 ± 3 | 30.1 ± 3 |
| 10 | 31 ± 3.2 | 30.7 ± 2.9 |
| 15 | 31.2 ± 3.2 | 30.7 ± 2.8 |
| 20 | 31 ± 3.4 | 30.6 ± 3 |
| Time (min) | ST | IRT | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| 0 | 33 ± 1.2 | 32.4 ± 1.2 | 27.8 ± 1.9 | 27.7 ± 2 |
| 10 | 33.8 ± 1.3 | 33.1 ± 1.18 | 28.2 ± 1.8 | 28.3 ± 2 |
| 15 | 34 ± 1.3 | 33.1 ± 1.3 | 28.3 ± 1.4 | 28.3 ± 1.5 |
| 20 | 34.1 ± 1.3 | 33.2 ± 1.2 | 27.9 ± 1.3 | 27.9 ± 1.4 |
| Period | Participants | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
| 0 | 1.3 | 2 | 1.4 | 2.8 | 1.2 | 2.5 | 1.9 | −0.4 | 0 | 0.4 | 0.4 | −0.4 | 0.1 | −0.5 | 1.5 | 0.4 | −0.1 | 0 | 0.1 | −1 | −1.2 | −0.1 |
| 10 | 2 | 2.6 | 1.3 | 2.6 | 1.2 | 2.7 | 2.2 | 0 | 0.4 | 0.5 | −0.3 | −0.2 | 0.5 | −1.2 | 1.8 | 0.4 | −0.5 | 0.1 | −0.7 | −0.1 | −0.6 | 0 |
| 15 | 2 | 2.8 | 2.3 | 2.9 | 1.4 | 2.7 | 2.3 | −0.2 | 0.6 | 0.4 | −0.3 | 0.4 | 0.7 | −1 | 2 | 0.7 | −0.4 | 0.2 | −0.6 | 0.2 | −0.3 | 0.3 |
| 20 | 2 | 2.9 | 2.3 | 2.8 | 1.9 | 2.8 | 2.2 | −0.2 | 0.4 | 0.6 | 0 | 0.3 | 1.4 | −1.2 | 2 | 0.5 | −0.2 | −0.3 | −1.3 | −0.6 | −0.3 | 0.2 |
| Period | Participants | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
| 0 | −0.5 | −0.2 | −0.1 | −0.4 | −0.6 | 0.5 | 0.6 | 1 | −0.3 | −0.4 | 0.2 | −0.2 | 0.5 | 0.2 | 0.5 | 0 | 1.8 | 0.1 | 0.4 | 0.2 | −0.2 | −0.2 |
| 10 | −0.3 | −0.1 | 0.1 | −1.3 | 0 | 0 | 0.6 | −0.8 | −0.2 | −0.6 | −0.7 | −1 | 0.4 | 0 | 0.8 | 0.1 | 1.5 | 0.1 | −0.2 | 0.3 | −0.5 | −0.4 |
| 15 | −0.4 | 0 | 0 | −1.2 | 0 | −0.2 | 0 | 0 | −0.4 | −0.2 | 0 | −1 | 0 | 0.3 | 0.9 | 0.5 | 0.8 | −0.3 | −0.2 | 0.5 | −0.1 | 0.1 |
| 20 | −0.9 | −0.4 | 0.3 | −1.3 | −0.4 | −0.1 | −0.3 | 0 | −0.5 | −0.5 | 0.4 | −0.9 | 0.5 | 0.2 | 1.1 | 0.4 | 1.2 | 0 | −0.1 | 0.4 | −0.1 | −0.3 |
| Cost | Relevant Points | Invisibility Level | |
|---|---|---|---|
| Sensory Thermography | USD 1000 | Do not consume alcohol; No Smoking; Do not play sports before; There is no limitation in maintaining fixed humidity. | The sensors are affixed to the skin during the evaluation. |
| Infrared thermography | USD 1500 or more | Do not consume alcohol; Do not smoke; Do not play sports before; Maintain a specific humidity and luminosity in the place. The emissivity of the camera for the skin must always be 98%. | Contact with the participant is not necessary. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García Becerra, A.; Olguín Tiznado, J.E.; García Alcaraz, J.L.; Camargo Wilson, C.; López Barreras, J.A.; Cano Gutiérrez, J.C.; Garcia-Rivera, R.B. Temperature Asymmetry Analysis between Left and Right Wrist with Sensory and Infrared Thermography. Int. J. Environ. Res. Public Health 2022, 19, 10240. https://doi.org/10.3390/ijerph191610240
García Becerra A, Olguín Tiznado JE, García Alcaraz JL, Camargo Wilson C, López Barreras JA, Cano Gutiérrez JC, Garcia-Rivera RB. Temperature Asymmetry Analysis between Left and Right Wrist with Sensory and Infrared Thermography. International Journal of Environmental Research and Public Health. 2022; 19(16):10240. https://doi.org/10.3390/ijerph191610240
Chicago/Turabian StyleGarcía Becerra, Alejandra, Jesús Everardo Olguín Tiznado, Jorge Luis García Alcaraz, Claudia Camargo Wilson, Juan Andrés López Barreras, Julio Cesar Cano Gutiérrez, and Rosa Blanca Garcia-Rivera. 2022. "Temperature Asymmetry Analysis between Left and Right Wrist with Sensory and Infrared Thermography" International Journal of Environmental Research and Public Health 19, no. 16: 10240. https://doi.org/10.3390/ijerph191610240
APA StyleGarcía Becerra, A., Olguín Tiznado, J. E., García Alcaraz, J. L., Camargo Wilson, C., López Barreras, J. A., Cano Gutiérrez, J. C., & Garcia-Rivera, R. B. (2022). Temperature Asymmetry Analysis between Left and Right Wrist with Sensory and Infrared Thermography. International Journal of Environmental Research and Public Health, 19(16), 10240. https://doi.org/10.3390/ijerph191610240











