Factors Associated with Behavioral and Psychological Symptoms of Dementia during COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort
2.2. Outcomes
2.3. Explanatory Variables
2.4. Other Variables
2.5. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steinman, M.A.; Perry, L.; Perissinotto, C.M. Meeting the Care Needs of Older Adults Isolated at Home During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 819–820. [Google Scholar] [CrossRef] [PubMed]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Christof, C.; Zachariah, C.; et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020, 4, CD013574. [Google Scholar] [PubMed]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, D.L.; Garay, J.R.; Deamond, S.L.; Moran, M.K.; Gold, W.; Styra, R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008, 136, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Armitage, R.; Nellums, L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef]
- Bartels, S.J.; Horn, S.D.; Smout, R.J.; Dums, A.R.; Flaherty, E.; Jones, J.K.; Monane, M.; Taler, G.A.; Voss, A.C. Agitation and depression in frail nursing home elderly patients with dementia: Treatment characteristics and service use. Am. J. Geriatr. Psychiatry 2003, 11, 231–238. [Google Scholar] [CrossRef]
- Fukui, C.; Fujisaki-Sueda-Sakai, M.; Yokouchi, N.; Sumikawa, Y.; Horinuki, F.; Baba, A.; Suto, M.; Okada, H.; Ogino, R.; Park, H.; et al. Needs of persons with dementia and their family caregivers in dementia cafés. Aging Clin. Exp. Res. 2019, 31, 1807–1816. [Google Scholar] [CrossRef]
- Takechi, H.; Yabuki, T.; Takahashi, M.; Osada, H.; Kato, S. Dementia Cafés as a Community Resource for Persons with Early-Stage Cognitive Disorders: A Nationwide Survey in Japan. J. Am. Med. Dir. Assoc. 2019, 20, 1515–1520. [Google Scholar] [CrossRef]
- Etters, L.; Goodall, D.; Harrison, B.E. Caregiver burden among dementia patient caregivers: A review of the literature. J. Am. Acad. Nurse Pract. 2008, 20, 423–428. [Google Scholar] [CrossRef]
- Tible, O.P.; Riese, F.; Savaskan, E.; von Gunten, A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther. Adv. Neurol. Disord. 2017, 10, 297–309. [Google Scholar] [CrossRef]
- Suzuki, Y.; Kazui, H.; Yoshiyama, K.; Azuma, S.; Kanemoto, H.; Sato, S.; Suehiro, T.; Ikeda, M. Advantages of different care services for reducing neuropsychiatric symptoms in dementia patients. Psychogeriatrics 2018, 18, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Lehtisalo, J.; Palmer, K.; Mangialasche, F.; Solomon, A.; Kivipelto, M.; Ngandu, T. Changes in Lifestyle, Behaviors, and Risk Factors for Cognitive Impairment in Older Persons During the First Wave of the Coronavirus Disease 2019 Pandemic in Finland: Results from the FINGER Study. Front. Psychiatry 2021, 12, 624125. [Google Scholar] [CrossRef] [PubMed]
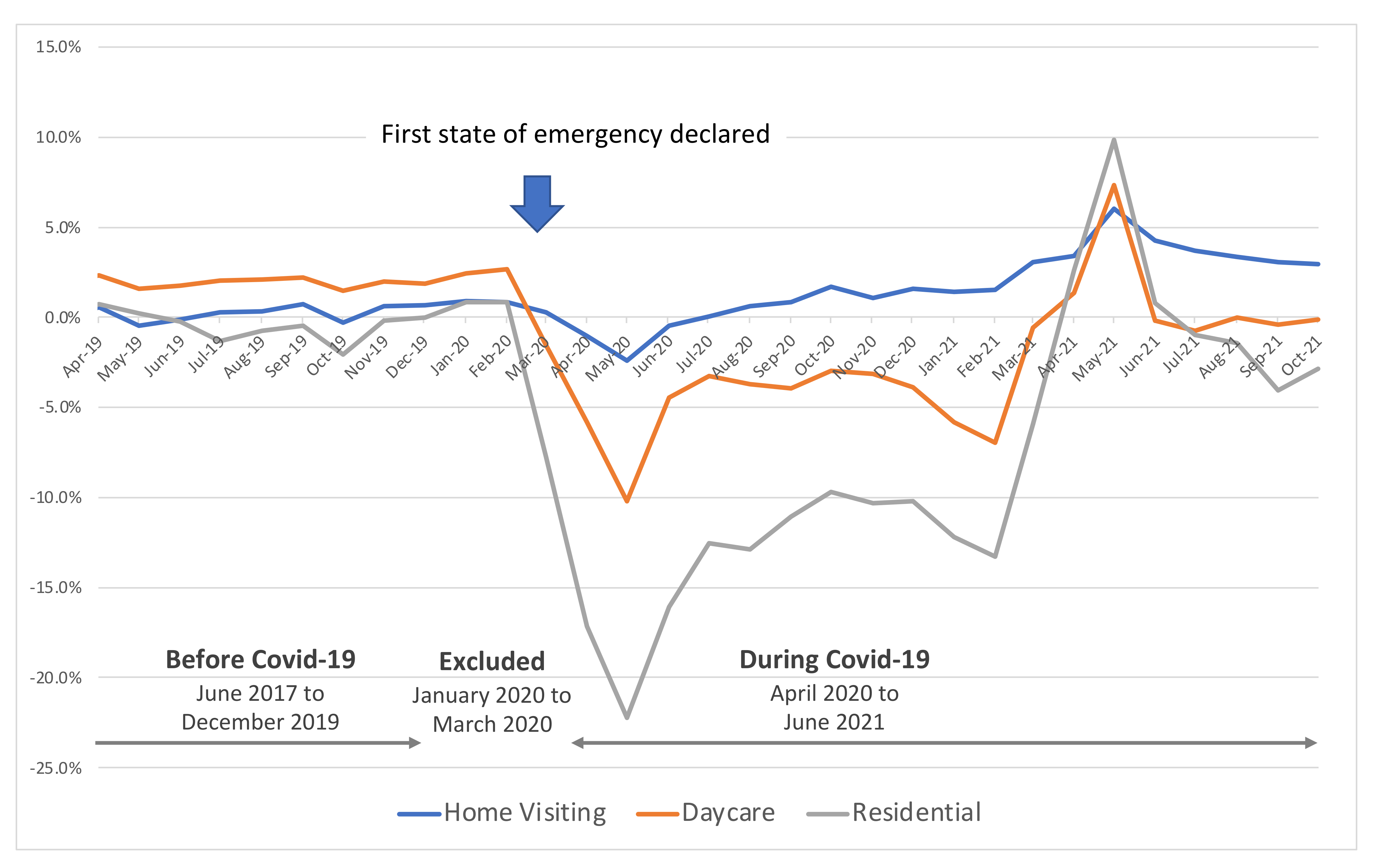
- Ito, T.; Hirata-Mogi, S.; Watanabe, T.; Sugiyama, T.; Jin, X.; Kobayashi, S.; Tamiya, N. Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan. Int. J. Environ. Res. Public Health 2021, 18, 1148. [Google Scholar] [CrossRef] [PubMed]
- Kazawa, K.; Kodama, A.; Sugawara, K.; Hayashi, M.; Ota, H.; Son, D.; Ishii, S. Person-centered dementia care during COVID-19: A qualitative case study of impact on and collaborations between caregivers. BMC Geriatr. 2022, 22, 107. [Google Scholar] [CrossRef] [PubMed]
- Canevelli, M.; Valletta, M.; Toccaceli Blasi, M.; Remoli, G.; Sarti, G.; Nuti, F.; Sciancalepore, F.; Ruberti, E.; Cesari, M.; Bruno, G. Facing Dementia During the COVID-19. J. Am. Geriatr. Soc. 2020, 68, 1673–1676. [Google Scholar] [CrossRef] [PubMed]
- Tsugawa, A.; Sakurai, S.; Inagawa, Y.; Hirose, D.; Kaneko, Y.; Ogawa, Y.; Serisawa, S.; Takenoshita, N.; Sakurai, H.; Kanetaka, H.; et al. Awareness of the COVID-19 Outbreak and Resultant Depressive Tendencies in Patients with Severe Alzheimer’s Disease. JAD 2020, 77, 539–541. [Google Scholar] [CrossRef] [PubMed]
- Cagnin, A.; Di Lorenzo, R.; Marra, C.; Bonanni, L.; Cupidi, C.; Laganà, V.; Rubino, E.; Vacca, A.; Provero, P.; Isella, V.; et al. Behavioral and Psychological Effects of Coronavirus Disease-19 Quarantine in Patients with Dementia. Front Psychiatry 2020, 11, 578015. [Google Scholar] [CrossRef]
- Kuroda, Y.; Sugimoto, T.; Matsumoto, N.; Uchida, K.; Kishino, Y.; Suemoto, C.K.; Sakurai, T. Prevalence of Behavioral and Psychological Symptoms in Patients with Cognitive Decline Before and During the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 839683. Available online: https://www.frontiersin.org/article/10.3389/fpsyt.2022.839683 (accessed on 25 March 2022). [CrossRef]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef]
- McKeith, I.G.; Boeve, B.F.; Dickson, D.W.; Halliday, G.; Taylor, J.P.; Weintraub, D.; Aarsland, D.; Galvin, J.; Attems, J.; Ballard, C.G.; et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 2017, 89, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Emre, M.; Aarsland, D.; Brown, R.; Burn, D.J.; Duyckaerts, C.; Mizuno, Y.; Broe, G.A.; Cummings, J.; Dickson, D.W.; Gauthier, S.; et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov. Disord. 2007, 22, 1689–1707, quiz 1837. [Google Scholar] [CrossRef] [PubMed]
- Román, G.C.; Tatemichi, T.K.; Erkinjuntti, T.; Cummings, J.L.; Masdeu, J.C.; Garcia, J.H.; Amaducci, L.; Orgogozo, J.-M.; Brun, A.; Hofman, A.; et al. Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology 1993, 43, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, M.; Becker, R.; Gauthier, S. Validity and Reliability of the Dementia Behavior Disturbance Scale. J. Am. Geriatr. Soc. 1990, 38, 221–226. [Google Scholar] [CrossRef]
- Mizoguchi, T.; Iijima, S.; Eto, F.; Ishizuka, A.; Orimo, H. Reliability and validity of a Japanese version of the Dementia Behavior Disturbance Scale. Nihon Ronen Igakkai Zasshi Japanese. J. Geriatr. 1993, 835–840. [Google Scholar] [CrossRef]
- Ikegami, N.; Yamauchi, K.; Yamada, Y. The long term care insurance law in Japan: Impact on institutional care facilities. Int. J. Geriatr. Psychiatry 2003, 18, 217–221. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Gnjidic, D.; Hilmer, S.N.; Blyth, F.M.; Naganathan, V.; Waite, L.; Seibel, M.J.; McLachlan, A.J.; Cumming, R.G.; Handelsman, D.J.; Le Couteur, D.G. Polypharmacy cutoff and outcomes: Five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J. Clin. Epidemiol. 2012, 65, 989–995. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Femia, E.E.; Zarit, S.H.; Stephens, M.A.P.; Greene, R. Impact of adult day services on behavioral and psychological symptoms of dementia. Gerontologist 2007, 47, 775–788. [Google Scholar] [CrossRef]
- Zarit, S.H.; Kim, K.; Femia, E.E.; Almeida, D.M.; Savla, J.; Molenaar, P.C.M. Effects of adult day care on daily stress of caregivers: A within-person approach. J. Gerontol. B Psychol. Sci. Soc. Sci. 2011, 66, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Logsdon, R.G.; Pike, K.C.; Korte, L.; Goehring, C. Memory Care and Wellness Services: Efficacy of Specialized Dementia Care in Adult Day Services. Gerontologist 2016, 56, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Kasai, M.; Meguro, K.; Akanuma, K.; Yamaguchi, S. Alzheimer’s disease patients institutionalized in group homes run by long-term care insurance exhibit fewer symptoms of behavioural problems as evaluated by the Behavioural Pathology in Alzheimer’s Disease Rating Scale. Psychogeriatrics 2015, 15, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Kawagoe, M.; Hotta, S. Older Adults Used Fewer Home Care Services during the COVID-19 Pandemic: Findings from a Secondary Analysis of an Urgent Survey in Japan. Ann. Geriatr. Med. Res. 2021, 25, 286–293. [Google Scholar] [CrossRef]
- Omura, T.; Araki, A.; Shigemoto, K.; Toba, K. Geriatric practice during and after the COVID-19 pandemic. Geriatr. Gerontol. Int. 2020, 20, 735–737. [Google Scholar] [CrossRef]
- Lim, W.S.; Liang, C.K.; Assantachai, P.; Auyeung, T.W.; Kang, L.; Lee, W.J.; Lim, J.-Y.; Sugimoto, K.; Akishita, M.; Chia, S.; et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr. Gerontol. Int. 2020, 20, 547–558. [Google Scholar] [CrossRef]
- Center for Long-Term Care Work Stability. Challenges and Measures for Long-Term Care Services in the Corona Disaster: Toward the Continuous Provision of Care Services. Available online: http://www.kaigo-center.or.jp/report/pdf/20210727r01_fukyukeihatsu.pdf (accessed on 24 February 2022).
- Kindell, J.; Keady, J.; Sage, K.; Wilkinson, R. Everyday conversation in dementia: A review of the literature to inform research and practice. Int. J. Lang. Commun. Disord. 2017, 52, 392–406. [Google Scholar] [CrossRef]
- Kuiper, J.S.; Zuidersma, M.; Oude Voshaar, R.C.; Zuidema, S.U.; van den Heuvel, E.R.; Stolk, R.P.; Smidt, N. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2015, 22, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Visser, M.; Schaap, L.A.; Wijnhoven, H.A.H. Self-Reported Impact of the COVID-19 Pandemic on Nutrition and Physical Activity Behaviour in Dutch Older Adults Living Independently. Nutrients 2020, 12, 3708. [Google Scholar] [CrossRef] [PubMed]
- Kimura, A.; Sugimoto, T.; Kitamori, K.; Saji, N.; Niida, S.; Toba, K.; Sakurai, T. Malnutrition is Associated with Behavioral and Psychiatric Symptoms of Dementia in Older Women with Mild Cognitive Impairment and Early-Stage Alzheimer’s Disease. Nutrients 2019, 11, 1951. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, T.; Ono, R.; Kimura, A.; Saji, N.; Niida, S.; Toba, K.; Sakurai, T.; Physical Frailty Correlates with Behavioral and Psychological Symptoms of Dementia and Caregiver Burden in Alzheimer’s Disease. J. Clin. Psychiatry 2018, 79. Available online: https://www.psychiatrist.com/JCP/article/Pages/2018/v79/17m11991.aspx (accessed on 25 October 2021).
- Taylor, D.J.; Lichstein, K.L.; Durrence, H.H.; Reidel, B.W.; Bush, A.J. Epidemiology of insomnia, depression, and anxiety. Sleep 2005, 28, 1457–1464. [Google Scholar] [CrossRef]
- Yaffe, K.; Laffan, A.M.; Harrison, S.L.; Redline, S.; Spira, A.P.; Ensrud, K.E.; Ancoli-Israel, S.; Stone, K.L. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011, 306, 613–619. [Google Scholar] [CrossRef]
- Grandner, M.A.; Hale, L.; Moore, M.; Patel, N.P. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med. Rev. 2010, 14, 191–203. [Google Scholar] [CrossRef]
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Dolenc Groselj, L.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700. [Google Scholar] [CrossRef]
- Pirie, K.; Peto, R.; Reeves, G.K.; Green, J.; Beral, V. Million Women Study Collaborators. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet 2013, 381, 133–141. [Google Scholar] [CrossRef]
- Amorim, J.S.C.; de Salla, S.; Trelha, C.S. Factors associated with work ability in the elderly: Systematic review. Rev. Bras. Epidemiol. 2014, 17, 830–841. [Google Scholar] [CrossRef]
- Kojima, G.; Iliffe, S.; Walters, K. Smoking as a predictor of frailty: A systematic review. BMC Geriatr. 2015, 15, 131. [Google Scholar] [CrossRef]
- Durazzo, T.C.; Mattsson, N.; Weiner, M.W. Alzheimer’s Disease Neuroimaging Initiative. Smoking and increased Alzheimer’s disease risk: A review of potential mechanisms. Alzheimers Dement. 2014, 10, S122–S145. [Google Scholar] [CrossRef] [PubMed]
| MCI Patients | Dementia Patients | |||||
|---|---|---|---|---|---|---|
| Before | During | p-Value | Before | During | p-Value | |
| (n = 740) | (n = 237) | (n = 1041) | (n = 339) | |||
| n (%) | n (%) | n (%) | n (%) | |||
| Socioeconomic status | ||||||
| Age group | ||||||
| Under 64 years | 40 (5.4) | 11 (4.6) | 0.226 | 31 (3.0) | 19 (5.6) | 0.079 |
| 65–74 years | 194 (26.2) | 50 (21.1) | 175 (16.8) | 54 (15.9) | ||
| 75 years and over | 506 (68.4) | 176 (74.3) | 835 (80.2) | 266 (78.5) | ||
| Gender (male) | 336 (45.4) | 111 (46.8) | 0.757 | 354 (34.0) | 128 (37.8) | 0.233 |
| Education (mean ± SD) | 11.6 ± 4.3 | 11.5 ± 2.4 | 0.783 | 10.5 ± 3.2 | 10.7 ± 2.4 | 0.28 |
| Living with family | 641 (87.1) | 209 (88.9) | 0.528 | 843 (81.6) | 290 (85.5) | 0.115 |
| Use of care services | ||||||
| Home visiting | 16 (2.2) | 3 (1.3) | 0.549 | 42 (4.0) | 7 (2.1) | 0.125 |
| Daycare | 56 (7.6) | 21 (8.9) | 0.614 | 266 (25.6) | 83 (24.5) | 0.748 |
| Residential | 7 (0.9) | 1 (0.4) | 0.715 | 68 (6.5) | 14 (4.1) | 0.135 |
| Medical condition | ||||||
| Clinical diagnosis | ||||||
| AD | – | – | – | 867 (83.3) | 279 (82.3) | 0.844 |
| DLB/PD | – | – | – | 114 (11.0) | 41 (12.1) | |
| VaD | – | – | – | 60 (5.8) | 19 (5.6) | |
| Polypharmacy (5 or more) | 260 (35.3) | 75 (31.6) | 0.344 | 401 (38.7) | 132 (38.9) | 0.981 |
| Comorbidity (2 or more) | 230 (31.1) | 64 (27.0) | 0.267 | 323 (31.0) | 103 (30.4) | 0.877 |
| Lifestyle-related variables | ||||||
| Light exercise/physical training | 214 (29.2) | 78 (33.1) | 0.292 | 205 (19.9) | 63 (18.7) | 0.685 |
| Quality of sleep (better) | 641 (88.2) | 214 (91.5) | 0.203 | 921 (90.0) | 297 (88.1) | 0.376 |
| Weight loss (N/A) | 605 (82.1) | 198 (84.3) | 0.507 | 840 (81.4) | 274 (81.5) | 1 |
| Non-smoking | 688 (93.6) | 222 (94.5) | 0.747 | 981 (94.8) | 320 (94.4) | 0.891 |
| MNA-SF (11 or above) | 453 (71.5) | 169 (71.6) | 1 | 517 (57.5) | 184 (54.3) | 0.338 |
| Physical functioning | ||||||
| IADL (Lawton Index Score) | ||||||
| Male (mean ± SD) | 4.4 ± 1.0 | 4.3 ± 1.0 | 0.291 | 3.0 ± 1.4 | 2.9 ± 1.5 | 0.644 |
| Female (mean ± SD) | 7.2 ± 1.3 | 7.2 ± 1.2 | 0.991 | 5.0 ± 2.2 | 5.1 ± 2.2 | 0.648 |
| Barthel index (mean ± SD) | 98.2 ± 6.5 | 97.7 ± 7.2 | 0.355 | 92.4 ± 14.8 | 91.4 ± 14.5 | 0.284 |
| Cognitive functioning | ||||||
| MMSE (mean ± SD) | 24.7 ± 3.3 | 23.8 ± 3.2 | 0.001 | 17.9 ± 4.9 | 17.8 ± 4.9 | 0.599 |
| DBD | ||||
|---|---|---|---|---|
| MCI Patients | Dementia Patients | |||
| Variable | β (95% CI) | p-Value | β (95% CI) | p-Value |
| Use of care services | ||||
| Home visiting | −0.57 (−4.88–3.74) | 0.794 | 2.99 (−1.06–7.05) | 0.148 |
| Daycare | −0.47 (−2.87–1.94) | 0.704 | −0.43 (−2.22–1.36) | 0.638 |
| Residential | −2.69 (−8.96–3.59) | 0.401 | −4.03 (−7.14–−0.93) | 0.011 |
| Lifestyle-related variables | ||||
| Light exercise/physical training | −0.60 (−1.95–0.76) | 0.386 | −0.64 (−2.44–1.16) | 0.489 |
| Quality of sleep (better) | −5.27 (−7.20–−3.35) | <0.001 | −3.04 (−5.50–−0.57) | 0.016 |
| Weight loss (N/A) | 1.01 (−0.64–2.67) | 0.23 | 0.15 (−1.78–2.07) | 0.882 |
| Non-smoking | −0.59 (−3.07–1.89) | 0.639 | −4.52 (−7.62–−1.41) | 0.004 |
| MNA-SF (11 or above) | −2.19 (−3.62–−0.76) | 0.003 | −1.59 (−3.12–−0.07) | 0.04 |
| Interaction terms with period (during COVID-19) | ||||
| Home visiting | 0.46 (−11.21–12.12) | 0.938 | −4.45 (−14.72–5.82) | 0.395 |
| Daycare | 5.80 (1.59–10.01) | 0.007 | 3.66 (0.47–6.85) | 0.025 |
| Residential | −2.95 (−19.23–13.34) | 0.723 | 6.39 (−0.15–12.94) | 0.056 |
| Light exercise/physical training | −0.78 (−3.26–1.70) | 0.535 | −0.04 (−3.54–3.45) | 0.981 |
| Quality of sleep (better) | −0.16 (−4.25–3.93) | 0.937 | −3.68 (−8.16–0.80) | 0.107 |
| Weight loss | 0.12 (−3.11–3.35) | 0.943 | −0.97 (−4.61–2.67) | 0.601 |
| Non-smoking | −1.46 (−6.40–3.47) | 0.561 | 4.21 (−1.59–10.01) | 0.155 |
| MNA-SF (11 or above) | −0.33 (−3.03–2.37) | 0.811 | −1.65 (−3.12–−0.07) | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuroda, Y.; Sugimoto, T.; Satoh, K.; Suemoto, C.K.; Matsumoto, N.; Uchida, K.; Kishino, Y.; Sakurai, T. Factors Associated with Behavioral and Psychological Symptoms of Dementia during COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 10094. https://doi.org/10.3390/ijerph191610094
Kuroda Y, Sugimoto T, Satoh K, Suemoto CK, Matsumoto N, Uchida K, Kishino Y, Sakurai T. Factors Associated with Behavioral and Psychological Symptoms of Dementia during COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(16):10094. https://doi.org/10.3390/ijerph191610094
Chicago/Turabian StyleKuroda, Yujiro, Taiki Sugimoto, Kenichi Satoh, Claudia K. Suemoto, Nanae Matsumoto, Kazuaki Uchida, Yoshinobu Kishino, and Takashi Sakurai. 2022. "Factors Associated with Behavioral and Psychological Symptoms of Dementia during COVID-19" International Journal of Environmental Research and Public Health 19, no. 16: 10094. https://doi.org/10.3390/ijerph191610094
APA StyleKuroda, Y., Sugimoto, T., Satoh, K., Suemoto, C. K., Matsumoto, N., Uchida, K., Kishino, Y., & Sakurai, T. (2022). Factors Associated with Behavioral and Psychological Symptoms of Dementia during COVID-19. International Journal of Environmental Research and Public Health, 19(16), 10094. https://doi.org/10.3390/ijerph191610094







