The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
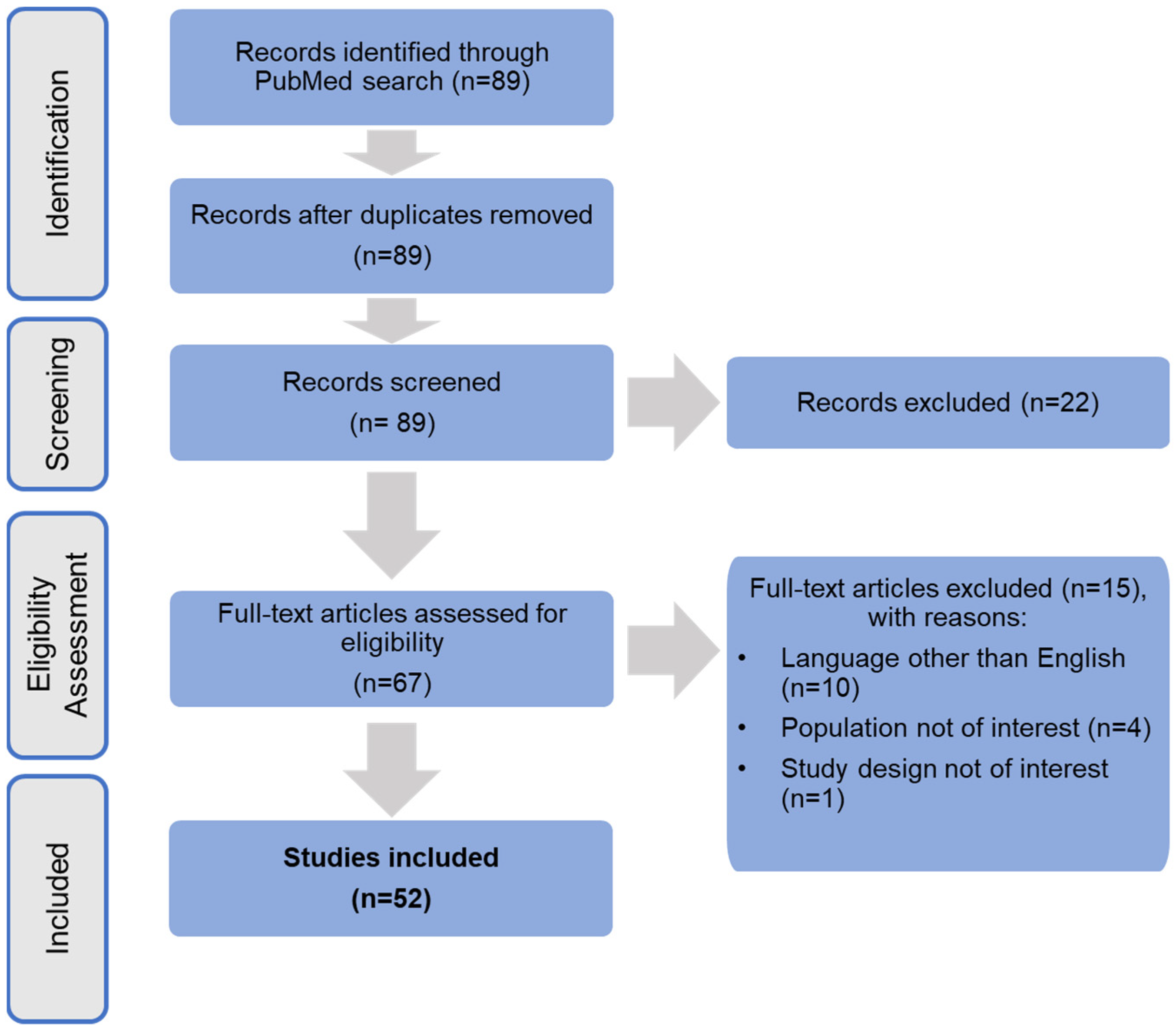
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection Process
2.3. The Rationale for the Study
2.4. Dependent Variables Studied
2.4.1. Fracture Classification
2.4.2. Patient Age
2.4.3. Meta-Analysis
2.4.4. AVN Incidence and Time Interval from Injury to Surgery
3. Results
3.1. Study Selection
3.2. Overview of Included Studies
| Study ID | Country | Study Design * | Cohort Size, N | Intervention | Post-Surgery Follow-Up | Baseline Age | Displaced Fractures, N (%) | Undisplaced, N (%) |
|---|---|---|---|---|---|---|---|---|
| Bajada 2015 [19] | United Kingdom | Retrospective study | 111 fractures in 108 patients | Internal fixation with cannulated screws | ≥90 days | Mean 79 years (range; 60–96 years) | NA | 111, (100%) |
| Bali 2011 [18] | India | Retrospective study | 36 | Closed or open reduction and internal fixation. Implants included partially threaded cancellous screws or pediatric dynamic hip screw | Mean 2.7 years (range, 1.1–9.5 years) | Mean 10 years (range, 3–16 years) | 28, (77.8%) | 8, (22.2%) |
| Chen 2017 [33] | China | Retrospective study | 86 | Closed reduction with cannulated compression screw or dynamic hip system blade | Mean 27 months (range, 24–36 months) | Mean 53.8 years (range, 26–83 years) | 42, (48.8%) | 44, (51.2%) |
| Do 2016 [34] | Norway | Retrospective cohort study | 383 | Fixation with 2 parallel screws or 3 screws | Median 77 months (range 23–125 months) | Median 81 years (range 72–86 years) | NA | 383, (100%) |
| Duckworth 2011 [35] | United Kingdom | Prospective single-arm study | 122 | Closed or open reduction and fixation using three cannulated screws | Mean 58 months (18–155 months) | Mean age 49 years (range, 17–60 years) | 122, (100%) | NA |
| Elgeidi 2017 [36] | Egypt | Retrospective study | 35 | Closed reduction and internal fixation using dynamic hip screw and fibular strut graft | 27.2 months (range 6–41 months) | 37 years (range 20–50 years) | 35, (100%) | NA |
| Fan 2017 [37] | China | Retrospective study | 65 | Closed reduction and internal fixation with 3 screws | ≤2 years | Median age 61 years (range, 19–84 years) | 26, (40%) | 39, (60%) |
| Gregersen 2015 [20] | Denmark | Case–cohort study | 322 | Fixation with 3 cannulated screws | 2 years | All patients ≥ 65 years, mean 82 years (±8.3) | 155, (48%) | 167, (52%) |
| Han 2017 [38] | Korea | Retrospective study | 53 | Closed reduction and internal fixation with 3 cannulated screws | Mean 29.5 months | Mean age 59.1 years (range, 31–82 years) | 14, (26.4%) | 39, (63.6%) |
| Hoelsbrekken 2012 [39] | Norway | Retrospective study | 337 | Closed reduction and internal fixation with hip pins | >3 months | Median age 82 years | 220, (65.3%) | 117, (34.7%) |
| Huang 2011 [40] | Taiwan | Retrospective study | 146 | Closed reduction and internal fixation with parallel cannulated screws in inverted triangle or diamond configurations | Mean 4.76 years (range, 2–6 years) | Mean 46.6 years (range, 17–60 years) | 42, (28.8%) | 104, (71.2%) |
| Huang 2020 [41] | China | Retrospective study | 67 | Gotfried closed reduction and internal fixation with cannulated cancellous screws | Mean 22.5 ± 11.3 months (range, 11–34 months) | All patients ≤65 years, mean 48.9 years | 30, (44.8%) | 37, (55.2%) |
| Jo 2016 [42] | Korea | Retrospective study | 45 | Closed reduction in displaced fractures and internal fixation with multiple screws or compression hip screw for all fractures | ≥2 years (range, 24–75 months) | Mean 48 years (range 19–69 years) | 27, (60%) | 18, (40%) |
| Ju 2016 [16] | China | Retrospective study | 58 | Closed reduction internal fixation (group 1) and open reduction internal fixation (group 2); several types of implants were used | Mean 35.1 months (range, 17–61 months) | Mean 9.1 years (range, 1 year and 8 months–15 years and 7 months) | NR | NR |
| Ju 2020 [21] | China | Retrospective study | 73 | Closed reduction and internal fixation with cannulated screws | Mean 61 months, (range, 13–128 months) | Mean 68.22 years (range, 60–85 years) | 38, (52.1%) | 35, (47.9%) |
| Kang 2016 [43] | Korea | Retrospective study | 84 | Internal fixation with cannulated screws | Mean 36.8 months (range, 24–148 months) | Mean 55.8 years (range, 16–88 years) | 35, (41.7%) | 49, (58.3%) |
| Kilian 2018 [44] | Slovakia | Retrospective study | 82 | Fixation using a locking plate system with telescoping sliding screws (Targon FN implants) | Mean 29 ± 7.1 (range, 24–62) months | Mean 71.6 years (range, 30–90 years) | 40, 48.8%). | 42, (51.2%) |
| Kim 2014 [22] | Korea | Retrospective study | 58 | Internal fixation with multiple screws | Mean 46.8 months (range; 12–151 months) | Mean 77.5 years (range 65–96 years) | NA | 58, (100%) |
| Kim 2021 [45] | Korea | Retrospective study | 58 | Internal fixation with cannulated screw, compressive hip screw fixation or nailing | Mean 23.9 months (range, 4–242 months) | Mean 40.0 years (range, 9–80 years) | 41, (70.1%) | 17, (29.3%) |
| Kumar 2014 [46] | India | Retrospective study | 62 | Closed or open reduction and internal fixation with cannulated screws, or open reduction and fixation with a dynamic hip screw and a derotation screw | ≥2 years (range, 2.5–4 years) | Mean 57.2 years (range, 45–82 years) | 38, (61.3%) | 24, (38.7%) |
| Li 2018 [47] | China | Retrospective study | 185 | Study group (group A, treated with three cannulated screws with DCIABG) Control group (group B, treated with traditional three cannulated screws without DCIABG) | Mean 29.26 months in group A and 28.74 months in group B | Mean 39.1 years in group A and 35.5 years in group B | 185, (100%) | NA |
| Liu 2013 [48] | China | Prospective study | 45 | Internal fixation with 3 cannulated screws | Mean 39.8 months | Mean 45.4 years (±14.2 years) | 24, (53.3%) | 20, (44.4%) |
| Luo 2017 [49] | China | Retrospective study | 17 | Open reduction and internal fixation with a modified dynamic hip screw loaded with autologous bone graft | ≥24 months (range, 24–36 months) | Mean 37.2 years (range, 27–52 years) | NR | NR |
| Manohara 2014 [23] | Singapore | Retrospective study | 100 | Internal fixation with cancellous screws | Mean 39 months (range, 25–76 months) | Mean 78 years, (range, 61–94) | NA | 100, (100%) |
| Min 2011 [28] | Korea | Retrospective study | 146 | Open or closed reduction and fixation with a sliding hip screw or cannulated screws | mean 5.2 years (range, 3 months–7 years) | mean 45.7 years (range, 17–70 years) | 91, (62%) | 55, (38%) |
| Mukka 2020 [24] | Sweden | Prospective pilot study | 235, including 65 patients treated with internal fixation and of interest to the review | Internal fixation with two cannulated screws | Median 26 months (range, 0–56 months) | Median 83 years (range 61–98 years) | NA | 65, (100%) |
| Novoa 2019 [29] | Spain | Case-control study | 121 | Internal fixation with cannulated titanium screws with a diameter of 6.5 mm | Mean 76.2 ± 31.6 months in ANFH group and 52.6 ± 25.1 months in the control group | Mean 63.7 years (range,44–83) in the ANFH group and 69.7 years (range, 18–93) in the control group | NA | 121, (100%) |
| Osarumwense 2015 [50] | United Kingdom | Retrospective study | 43 | Closed reduction (displaced fractures only) and fixation with the Targon FN implant | ≥24 months (range, 24–47 months) | Mean 66 years (range, 24–94 years) | 12, (28%) | 31, (72%) |
| Park 2015 [25] | Korea | Retrospective study | 19 | Fixation with Proximal Femoral Nail Antirotation | Mean 53.3 months (range, 30–72 months) | Mean 77 years (range, 71–82 years) | NA | 19, (100%) |
| Park 2021 [51] | Korea | Retrospective study | 55 | In situ or post-reduction internal fixation with three parallel screws | Mean 36.3 (median 29.5, range: 12–85) months and 36.2 (median 26.0, range: 13–120) months for the in situ and reduction groups, respectively | Mean 52.6 ± 10.3 year for the in-situ group and 51.3 ± 9.8 years for the reduction group | NA | 55, (100%) |
| Parker 2013 [52] | United Kingdom | Retrospective study | 320 | Fixation with a dynamic locking plate (Targon FN) | Mean 2.5 years (range, 2.0–10) | Mean 76.0 years (range, 22–103) | 208, (65%) | 112, (35%) |
| Pei 2020 [31] | China | Retrospective study | 250 | Closed or open reduction and fixation with 2–3 hollow compression screws | Mean 7.5 years (range, 1–15 years) | Mean 56.4 ± 6.8 years (range, 18–59 years) | 142, (56.8%) | 108, (43.2%) |
| Razik 2012 [53] | United Kingdom | Retrospective study | 92 | Fixation using cannulated screws, dynamic hip screws, or a dynamic hip screw with a derotation screw | Mean 2 years | Mean 44.7 years (range, 11–59), (median age, 50 years) | 68, (73.9%) | 24, (26.1%) |
| Riaz 2016 [26] | United Kingdom | Retrospective study | 251 | Fixation with cannulated hip screws | NR | Mean 77 years (range 60–101 years) | NA | 251, (100%) |
| Şahin 2020 [54] | Turkey | Retrospective study | 78 | Closed reduction and internal fixation, (Dynamic hip screw and antirotation screw—group 1, Cannulated screw—group 2) | Mean 18.1 months (range, 12–36 months) for group 1 and 14.2 months (range, 12–25 months) for group 2 | Group 1- (mean age 45.7 years; range, 19–62 years), group 2—(mean age 41.9 years; range, 17–75 years) | 34, (43.6%) | 44, (56.4%) |
| Sales 2012 [55] | Iran | Prospective cohort study | 51 | Fixation using 3 cancellous screws in a reverse triangle arrangement | ≤1 year | Mean 49.12 ± 16.8 years | NR | NR |
| Samy 2015 [56] | Egypt | Prospective study | 60 | Group A—closed reduction and internal fixation with three cannulated screws Group B—addition of PRP to internal fixation | 12–48 months with a mean of 28 months | Range 20–45 for both groups; mean age 30 ± 7.8:32 ± 6.4 for group A and 28 ± 8.4 for group B | 60, (100%) | NA |
| Schweitzer 2012 [57] | Chile | Retrospective study | 29 | Closed or open reduction and internal fixation with cannulated screws | Median 28 months (range 24–144 months) | Mean 46.45 ± 11.59 years | 29, (100%) | NA |
| Sjöholm 2019 [58] | Sweden | Retrospective cohort study | 417 | Closed reduction and internal fixation | Mean 3.4 years (range, 2–14) | Median 78 years (range, 50–108 years) | NA | 417, (100%) |
| Su 2011 [59] | China | Retrospective study | 25 | Minimally traumatic reduction with K-wires or Steinman pins and fixation with three cannulated screws | Mean 4.6 years (range, 3–5 years) | Mean 35 years (range, 19–54 years) | 25, (100%) | NA |
| Sun 2021 [60] | China | Prospective cohort study | 75 | Closed reduction and internal fixation using three parallel FTHCS | ≥2 years | Mean 48.76 years, (range,18–65 years) | 48, (64%) | 27, (36%) |
| Wang 2014 [30] | China | Retrospective study | 146 | Open or closed reduction and internal fixation with 2 or 3 cannulated cancellous screws | Mean 52 months (range, 9–84 months) | Mean 47.5 years (range, 18–68 years) | 90, (61.6%) | 56, (38.4%) |
| Wang 2018 [32] | Taiwan | Single-centre retrospective study | 117 | Closed reduction and unilateral internal fixation with cannulated screws | ≥2 years (range, 2–8 years) | Mean 55.4 years (range, 50–60 years) | 69, (59%) | 48, (41%) |
| Wang 2019 [61] | China | Retrospective study | 241 | Closed reduction and internal fixation | >18 months | Mean 53.46 years | NR | NR |
| Wei 2021 [62] | Taiwan | Retrospective study | 22 | Fixation with single construct with/without an antirotational screw or dual constructs | Median 12 months (interquartile range, 12–24 months) | Mean 45.18 years ± 16.00 years | NR | NR |
| Wu 2020 [17] | China | Retrospective study | 16 patients, 17 hips | Open or closed reduction and internal fixation using K-wire pinning or screw | Mean 23.2 months (range 10–58months) | Mean 10.4 years, (range, 1–14 years) | 16, (94.1%) | 1, (5.9%) |
| Xiao 2018 [27] | China | Single-centre, retrospective study | 36 | Closed reduction and fixation with dynamic compression locking system | Mean 21.58 ± 5.41 months, (range, 12–29 months) | Mean 65.33 ± 9.30 years (range,53–82) | 27, (75%) | 9, (25%) |
| Xiong 2019 [63] | China | Retrospective study | 46 | Closed reduction and fixation with multiple cannulated screws (6.5 mm in diameter) in inverted triangle or diamond configuration | Mean 22.0 months (range, 12–36 months) | Mean 50.3 years (range, 19–60 years) | 46, (100%) | NA |
| Ye 2017 [64] | China | Retrospective study | 28 | Open reduction and internal fixation using cannulated screws and medial buttress plate fixation | Mean 13.6 months (range, 12–18 months) | Mean 42.1 years (range, 29–57 years) | NR | NR |
| Zahid 2012 [65] | India | Retrospective study | 33 | Closed reduction and fixation using 7.0-mm cannulated cancellous screws and fibular strut grafts | Mean 2 (range, 1–4) years | 40–60 years (mean, 52 years) | 33, (100%) | NA |
| Zeng 2017 [66] | China | Case-control study | 325 | Closed reduction and internal fixation with cancellous screws | Mean 42 months (range 37–46 months) | Mean 74 years (range 50–94 years) | 220, (67.7%) | 105, (32.3%) |
| Zhuang 2019 [67] | China | Retrospective study | 26 | Open reduction and fixation with anteromedial femoral neck plate with cannulated screws | Mean 18 months (range 12–30 months) | Mean 36.5 years (range 19–44 years) | 26, (100%) | NA |
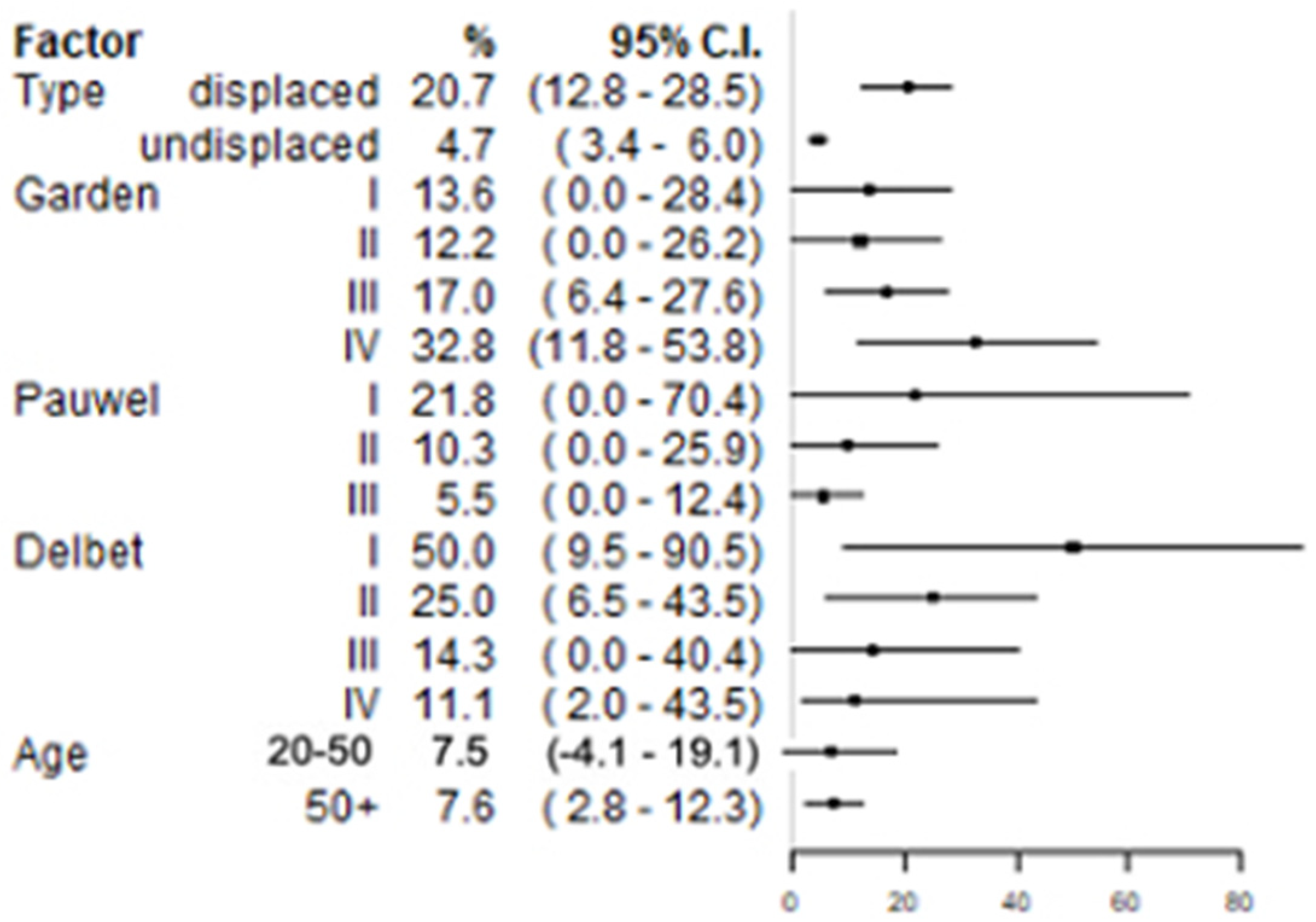
3.3. Incidence of AVN
3.3.1. AVN Incidence in Displaced and Undisplaced Fractures
3.3.2. AVN Incidence by Garden Stage
3.3.3. AVN Incidence by Pauwels’ Degree
3.3.4. AVN Incidence by Delbet’s Type
3.3.5. AVN Incidence by Age Category
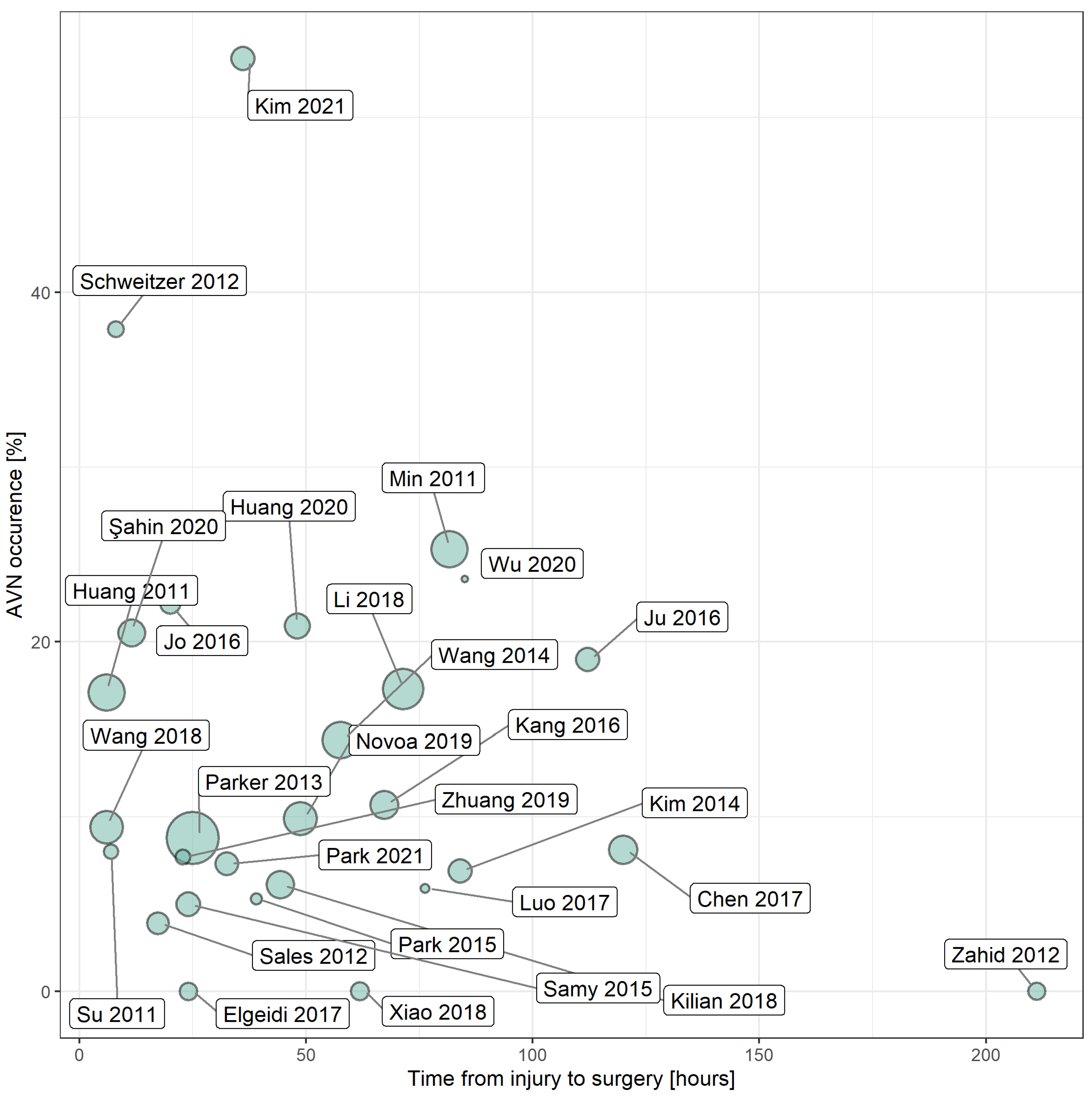
3.4. The Relationship between AVN Incidence and Time Interval from Injury to Surgery
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barney, J.; Piuzzi, N.S.; Akhondi, H. Femoral Head Avascular Necrosis; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Matthews, A.H.; Davis, D.D.; Fish, M.J.; Stitson, D. Avascular Necrosis; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Shah, K.N.; Racine, J.; Jones, L.C.; Aaron, R.K. Pathophysiology and risk factors for osteonecrosis. Curr. Rev. Musculoskelet. Med. 2015, 8, 201–209. [Google Scholar] [CrossRef]
- Moya-Angeler, J. Current concepts on osteonecrosis of the femoral head. World J. Orthop. 2015, 6, 590–601. [Google Scholar] [CrossRef] [PubMed]
- Arbab, D.; König, D.P. Atraumatic Femoral Head Necrosis in Adults. Dtsch. Arztebl. Int. 2016, 113, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Parker, M.J.; Gurusamy, K.S. Internal fixation implants for intracapsular hip fractures in adults. Cochrane Database Syst. Rev. 2001, CD001467. [Google Scholar] [CrossRef]
- Garden, R.S. Low-Angle Fixation in Fractures of the Femoral Neck. J. Bone Jt. Surg. Br. Vol. 1961, 43, 647–663. [Google Scholar] [CrossRef]
- Lutnick, E.; Kang, J.; Freccero, D.M. Surgical Treatment of Femoral Neck Fractures: A Brief Review. Geriatrics 2020, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Bartonícek, J. Pauwels’ Classification of Femoral Neck Fractures: Correct Interpretation of the Original. J. Orthop. Trauma 2001, 15, 358–360. [Google Scholar] [CrossRef]
- Caviglia, H.A.; Osorio, P.Q.; Comando, D. Classification and Diagnosis of Intracapsular Fractures of the Proximal Femur. Clin. Orthop. Relat. Res. 2002, 399, 17–27. [Google Scholar] [CrossRef]
- Boardman, M.J.; Herman, M.J.; Buck, B.; Pizzutillo, P.D. Hip Fractures in Children. JAAOS J. Am. Acad. Orthop. Surg. 2009, 17, 162–173. [Google Scholar] [CrossRef]
- Dial, B.L.; Lark, R.K. Pediatric proximal femur fractures. J. Orthop. 2018, 15, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Wendt, K.; Heim, D.; Josten, C.; Kdolsky, R.; Oestern, H.-J.; Palm, H.; Sintenie, J.B.; Komadina, R.; Copuroglu, C. Recommendations on hip fractures. Eur. J. Trauma Emerg. Surg. 2016, 42, 425–431. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Orthopaedic Surgeons. Management of Hip Fractures in the Elderly Evidence-Based Clinical Practice Guideline. 5 September 2014. Available online: https://www.aaos.org/globalassets/quality-and-practice-resources/hipfractures-in-the-elderly/hip-fractures-elderly-clinical-practice-guideline-4-24-19--2.pdf (accessed on 19 August 2021).
- Ju, L.; Jiang, B.; Lou, Y.; Zheng, P. Delayed treatment of femoral neck fractures in 58 children: Open reduction internal fixation versus closed reduction internal fixation. J. Pediatr. Orthop. B 2016, 25, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Ning, B.; Xu, P.; Song, J.; Wang, D. Efficacy and complications after delayed fixation of femoral neck fractures in children. J. Orthop. Surg. 2020, 28, 2309499019889682. [Google Scholar] [CrossRef]
- Bali, K.; Sudesh, P.; Patel, S.; Kumar, V.; Saini, U.; Dhillon, M.S. Pediatric Femoral Neck Fractures: Our 10 Years of Experience. Clin. Orthop. Surg. 2011, 3, 302–308. [Google Scholar] [CrossRef]
- Bajada, S.; Smith, A.; Morgan, D. Pre-operative nutritional serum parameters as predictors of failure after internal fixation in undisplaced intracapsular proximal femur fractures. Injury 2015, 46, 1571–1576. [Google Scholar] [CrossRef]
- Gregersen, M.; Krogshede, A.; Brink, O.; Damsgaard, E.M. Prediction of Reoperation of Femoral Neck Fractures Treated with Cannulated Screws in Elderly Patients. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 322–327. [Google Scholar] [CrossRef]
- Ju, F.-X.; Hou, R.-X.; Xiong, J.; Shi, H.-F.; Chen, Y.-X.; Wang, J.-F. Outcomes of Femoral Neck Fractures Treated with Cannulated Internal Fixation in Elderly Patients: A Long-Term Follow-Up Study. Orthop. Surg. 2020, 12, 809–818. [Google Scholar] [CrossRef]
- Kim, J.W.; Byun, S.-E.; Chang, J.S. The clinical outcomes of early internal fixation for undisplaced femoral neck fractures and early full weight-bearing in elderly patients. Arch. Orthop. Trauma Surg. 2014, 134, 941–946. [Google Scholar] [CrossRef]
- Manohara, R.; Liang, S.; Huang, D.; Krishna, L. Cancellous Screw Fixation for Undisplaced Femoral Neck Fractures in the Elderly. J. Orthop. Surg. 2014, 22, 282–286. [Google Scholar] [CrossRef]
- Mukka, S.; Sjöholm, P.; Aziz, A.; Eisler, T.; Kadum, B.; Krupic, F.; Morberg, P.; Sayed-Noor, A. A cohort study comparing internal fixation for undisplaced versus hip arthroplasty for displaced femoral neck fracture in the elderly: A pilot study for a clinical trial. Pilot Feasibility Stud. 2020, 6, 98. [Google Scholar] [CrossRef]
- Park, B.-J.; Cho, H.-M.; Min, W.-B. Surgical Treatment of Undisplaced Femur Neck Fractures in Dementia Patients Using Proximal Femoral Nail Antirotation. Hip Pelvis 2015, 27, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Riaz, O.; Arshad, R.; Nisar, S.; Vanker, R. Serum albumin and fixation failure with cannulated hip screws in undisplaced intracapsular femoral neck fracture. Ann. R. Coll. Surg. Engl. 2016, 98, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.-P.; Shu, D.-P.; Bei, M.-J.; Ji, T.; Kan, W.-S.; Li, S.-G. The clinical application of a novel method of internal fixation for femoral neck fractures-dynamic locking compression system. J. Orthop. Surg. Res. 2018, 13, 131. [Google Scholar] [CrossRef] [PubMed]
- Min, B.-W.; Kim, S.-J. Avascular Necrosis of the Femoral Head after Osteosynthesis of Femoral Neck Fracture. Orthopedics 2011, 34, 349. [Google Scholar] [CrossRef]
- Novoa-Parra, C.; Pérez-Ortiz, S.; López-Trabucco, R.; Blas-Dobón, J.; Rodrigo-Pérez, J.; Lizaur-Utrilla, A. Factores asociados al desarrollo de necrosis avascular de cabeza femoral tras fractura del cuello femoral no desplazada tratada con fijación interna. Rev. Esp. Cir. Orthop. Traumatol. 2019, 63, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Sun, J.-Y.; Zha, G.-C.; Jiang, T.; You, Z.-J.; Yuan, D.-J. Analysis of Risk Factors for Femoral Head Necrosis after Internal Fixation in Femoral Neck Fractures. Orthopedics 2014, 37, e1117–e1123. [Google Scholar] [CrossRef]
- Pei, F.; Zhao, R.; Li, F.; Chen, X.; Guo, K.; Zhu, L. Osteonecrosis of femoral head in young patients with femoral neck fracture: A retrospective study of 250 patients followed for average of 7.5 years. J. Orthop. Surg. Res. 2020, 15, 238. [Google Scholar] [CrossRef]
- Wang, C.-T.; Chen, J.-W.; Wu, K.; Chen, C.-S.; Chen, W.-C.; Pao, J.-L.; Chang, C.-H.; Lan, T.-Y. Suboptimal outcomes after closed reduction and internal fixation of displaced femoral neck fractures in middle-aged patients: Is internal fixation adequate in this age group? BMC Musculoskelet. Disord. 2018, 19, 190. [Google Scholar] [CrossRef]
- Chen, C.; Yu, L.; Tang, X.; Liu, M.-Z.; Sun, L.-Z.; Liu, C.; Zhang, Z.; Li, C.-Z. Dynamic hip system blade versus cannulated compression screw for the treatment of femoral neck fractures: A retrospective study. Acta Orthop. Traumatol. Turc. 2017, 51, 381–387. [Google Scholar] [CrossRef]
- Do, L.N.D.; Kruke, T.M.; Foss, O.A.; Basso, T. Reoperations and mortality in 383 patients operated with parallel screws for Garden I-II femoral neck fractures with up to ten years follow-up. Injury 2016, 47, 2739–2742. [Google Scholar] [CrossRef] [PubMed]
- Duckworth, A.D.; Bennet, S.J.; Aderinto, J.; Keating, J.F. Fixation of intracapsular fractures of the femoral neck in young patients. J. Bone Jt. Surg. Br. Vol. 2011, 93, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Elgeidi, A.; El Negery, A.; Abdellatif, M.S.; El Moghazy, N. Dynamic hip screw and fibular strut graft for fixation of fresh femoral neck fracture with posterior comminution. Arch. Orthop. Trauma Surg. 2017, 137, 1363–1369. [Google Scholar] [CrossRef] [PubMed]
- Fan, W.; Zhu, L.; Chen, J.; Guo, C.; Yan, Z. Identifying Patients Who Will Most Benefit from Single Photon Emission Computerized Tomography and Computerized Tomography After Femoral Neck Fracture. Med. Sci. Monit. 2017, 23, 5669–5674. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Oh, M.; Yoon, S.; Kim, J.; Kim, J.-W.; Chang, J.-S.; Ryu, J.-S. Risk Stratification for Avascular Necrosis of the Femoral Head after Internal Fixation of Femoral Neck Fractures by Post-Operative Bone SPECT/CT. Nucl. Med. Mol. Imaging 2017, 51, 49–57. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoelsbrekken, S.; Opsahl, J.-H.; Stiris, M.; Paulsrud, Ø.; Strømsøe, K. Behandlingssvikt ved osteosyntese av lårhalsbrudd. Tidsskr. Den Nor. Legeforening 2012, 132, 1343–1347. [Google Scholar] [CrossRef][Green Version]
- Huang, T.-W.; Hsu, W.-H.; Peng, K.-T.; Lee, C.-Y. Effect of integrity of the posterior cortex in displaced femoral neck fractures on outcome after surgical fixation in young adults. Injury 2011, 42, 217–222. [Google Scholar] [CrossRef]
- Huang, K.; Fang, X.; Li, G.; Yue, J. Assessing the effect of Gotfried reduction with positive buttress pattern in the young femoral neck fracture. J. Orthop. Surg. Res. 2020, 15, 511. [Google Scholar] [CrossRef]
- Jo, S.; Lee, S.H.; Lee, H.J. The Correlation between the Fracture Types and the Complications after Internal Fixation of the Femoral Neck Fractures. Hip Pelvis 2016, 28, 35–42. [Google Scholar] [CrossRef]
- Kang, J.S.; Moon, K.H.; Shin, J.S.; Shin, E.H.; Ahn, C.H.; Choi, G.H. Clinical Results of Internal Fixation of Subcapital Femoral Neck Fractures. Clin. Orthop. Surg. 2016, 8, 146–152. [Google Scholar] [CrossRef]
- Kilian, M.; Csörgő, P.; Šajter, M.; Šimkovic, P.; Vajcziková, S.; Zamborský, R. Locking Plate Fixation with Multiple Telescoping Sliding Screws for Femoral Neck Fractures. Ortop. Traumatol. Rehabil. 2018, 20, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-H.; Shin, M.; Lee, D.; Choi, S.J.; Moon, D.H. Hidden osteonecrosis of the femoral head after healed femoral neck fractures: Magnetic resonance imaging study of 58 consecutive patients. Arch. Orthop. Trauma Surg. 2021, 142, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.N.; Belehalli, P.; Ramachandra, P. PET/CT Study of Temporal Variations in Blood Flow to the Femoral Head Following Low-energy Fracture of the Femoral Neck. Orthopedics 2014, 37, e563–e570. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Jin, D.; Shao, X.; Liu, Z.; Duan, J.; Akileh, R.; Cao, S.; Liu, T. Effect of cannulated screws with deep circumflex iliac artery-bone grafting in the treatment of femoral neck fracture in young adults. Injury 2018, 49, 1587–1593. [Google Scholar] [CrossRef]
- Liu, Y.; Li, M.; Zhang, M.; Sun, K.; Wang, H.; Yuan, X.; Cai, L. Femoral neck fractures: Prognosis based on a new classification after superselective angiography. J. Ortop. Sci. 2013, 18, 443–450. [Google Scholar] [CrossRef]
- Luo, D.; Zou, W.; He, Y.; Xian, H.; Wang, L.; Shen, J.; Lian, K.; Lin, D. Modified dynamic hip screw loaded with autologous bone graft for treating Pauwels type-3 vertical femoral neck fractures. Injury 2017, 48, 1579–1583. [Google Scholar] [CrossRef]
- Osarumwense, D.; Tissingh, E.; Wartenberg, K.; Aggarwal, S.; Ismail, F.; Orakwe, S.; Khan, F. The Targon FN System for the Management of Intracapsular Neck of Femur Fractures: Minimum 2-Year Experience and Outcome in an Independent Hospital. Clin. Orthop. Surg. 2015, 7, 22–28. [Google Scholar] [CrossRef]
- Park, Y.-C.; Um, K.-S.; Kim, D.-J.; Byun, J.; Yang, K.-H. Comparison of femoral neck shortening and outcomes between in situ fixation and fixation after reduction for severe valgus-impacted femoral neck fractures. Injury 2021, 52, 569–574. [Google Scholar] [CrossRef]
- Parker, M.; Cawley, S.; Palial, V. Internal fixation of intracapsular fractures of the hip using a dynamic locking plate. Bone Jt. J. 2013, 95, 1402–1405. [Google Scholar] [CrossRef]
- Razik, F.; Alexopoulos, A.-S.; El-Osta, B.; Connolly, M.J.; Brown, A.; Hassan, S.; Ravikumar, K. Time to internal fixation of femoral neck fractures in patients under sixty years—Does this matter in the development of osteonecrosis of femoral head? Int. Orthop. 2012, 36, 2127–2132. [Google Scholar] [CrossRef]
- Şahin, A.; Agar, A.; Gülabi, D.; Ertürk, C. Comparison of dynamic hip screw and antirotation screw with cannulated screw in the treatment of transcervical collum femoris fractures. Jt. Dis. Relat. Surg. 2020, 31, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Sales, J.G.; Soleymaopour, J.; Sadeghpour, A.; Sharifi, S.; Rouhani, S.; Goldust, M. Efficacy of Reverse Triangle Screw Fixation in Patients Suffering from Femoral Neck Fractures. Pak. J. Biol. Sci. 2012, 15, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Samy, A.M. The role of platelet rich plasma in management of fracture neck femur: New insights. Int. Orthop. 2016, 40, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, D.; Melero, P.; Zylberberg, A.; Salabarrieta, J.; Urrutia, J. Factors associated with avascular necrosis of the femoral head and nonunion in patients younger than 65 years with displaced femoral neck fractures treated with reduction and internal fixation. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 61–65. [Google Scholar] [CrossRef]
- Sjöholm, P.; Otten, V.; Wolf, O.; Gordon, M.; Karsten, G.; Sköldenberg, O.; Mukka, S. Posterior and anterior tilt increases the risk of failure after internal fixation of Garden I and II femoral neck fracture. Acta Orthop. 2019, 90, 537–541. [Google Scholar] [CrossRef]
- Su, Y.; Chen, W.; Zhang, Q.; Li, B.; Li, Z.; Guo, M.; Pan, J.; Zhang, Y. An irreducible variant of femoral neck fracture: A minimally traumatic reduction technique. Injury 2011, 42, 140–145. [Google Scholar] [CrossRef]
- Sun, H.; Shu, L.-Y.; Sherrier, M.C.; Zhu, Y.; Liu, J.-W.; Zhang, W. Decreased complications but a distinctive fixation loosening mechanism of fully threaded headless cannulated screw fixation for femoral neck fractures in young adults. J. Orthop. Surg. Res. 2021, 16, 234. [Google Scholar] [CrossRef]
- Wang, Y.; Ma, J.; Yin, T.; Han, Z.; Cui, S.; Liu, Z.; Ma, X. Correlation Between Reduction Quality of Femoral Neck Fracture and Femoral Head Necrosis Based on Biomechanics. Orthop. Surg. 2019, 11, 318–324. [Google Scholar] [CrossRef]
- Wei, Y.P.; Lin, K.C. Dual-construct fixation is recommended in ipsilateral femoral neck fractures with infra-isthmus shaft fracture. Medicine 2021, 100, e25708. [Google Scholar] [CrossRef]
- Xiong, W.-F.; Chang, S.-M.; Zhang, Y.-Q.; Hu, S.-J.; Du, S.-C. Inferior calcar buttress reduction pattern for displaced femoral neck fractures in young adults: A preliminary report and an effective alternative. J. Orthop. Surg. Res. 2019, 14, 70. [Google Scholar] [CrossRef]
- Ye, Y.; Chen, K.; Tian, K.; Li, W.; Mauffrey, C.; Hak, D.J. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury 2017, 48, 2189–2193. [Google Scholar] [CrossRef]
- Zahid, M.; Sabir, A.B.; Asif, N.; Julfiqar, M.; Khan, A.; Ahmad, S.; Siddiqui, Y.S. Fixation Using Cannulated Screws and Fibular Strut Grafts for Fresh Femoral Neck Fractures with Posterior Comminution. J. Orthop. Surg. 2012, 20, 191–195. [Google Scholar] [CrossRef]
- Zeng, X.; Zhan, K.; Zhang, L.; Zeng, D.; Yu, W.; Zhang, X.; Zhao, M.; Lai, Z.; Chen, R. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J. Orthop. Surg. Res. 2017, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, L.; Wang, L.; Xu, D.; Wang, Z. Anteromedial femoral neck plate with cannulated screws for the treatment of irreducible displaced femoral neck fracture in young patients: A preliminary study. Eur. J. Trauma Emerg. Surg. 2019, 45, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.-L.; Liang, Z.-R.; Xiong, B.-L.; Zou, Q.-Z.; Lin, T.-Y.; Yang, P.; Chen, D.; Zhang, Q.-W. Risk factors associated with osteonecrosis of femoral head after internal fixation of femoral neck fracture:a systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 632. [Google Scholar] [CrossRef] [PubMed]
- Papakostidis, C.; Panagiotopoulos, A.; Piccioli, A.; Giannoudis, P.V. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury 2015, 46, 459–466. [Google Scholar] [CrossRef] [PubMed]
| Studies Included in the Review | Studies Excluded from the Review |
|---|---|
|
|
| Classification | Type | Description | Other |
|---|---|---|---|
| Garden | Stage I | incomplete fracture; undisplaced, valgus impacted |  |
| Stage II | complete fracture; undisplaced | ||
| Stage III | complete fracture; partially displaced | ||
| Stage IV | complete fracture; fully displaced | ||
| Pauwel’s | Angle between fracture line and horizontal plane | Dominant forces | |
| Degree I | Up to 30 degrees | Compressive forces predominate | |
| Degree II | 30–50 degrees | Shearing stress is present and may adversely impact healing | |
| Degree III | 50 degrees and more | Shearing stress dominates | |
| Delbet’s | Type I | Transphyseal fracture, with or without dislocation of the capital femoral epiphysis |  |
| Type II | Transcervical fracture | ||
| Type III | Cervicotrochanteric fracture. | ||
| Type IV | Intertrochanteric fracture | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konarski, W.; Poboży, T.; Kotela, A.; Śliwczyński, A.; Kotela, I.; Hordowicz, M.; Krakowiak, J. The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 10050. https://doi.org/10.3390/ijerph191610050
Konarski W, Poboży T, Kotela A, Śliwczyński A, Kotela I, Hordowicz M, Krakowiak J. The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(16):10050. https://doi.org/10.3390/ijerph191610050
Chicago/Turabian StyleKonarski, Wojciech, Tomasz Poboży, Andrzej Kotela, Andrzej Śliwczyński, Ireneusz Kotela, Martyna Hordowicz, and Jan Krakowiak. 2022. "The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 16: 10050. https://doi.org/10.3390/ijerph191610050
APA StyleKonarski, W., Poboży, T., Kotela, A., Śliwczyński, A., Kotela, I., Hordowicz, M., & Krakowiak, J. (2022). The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(16), 10050. https://doi.org/10.3390/ijerph191610050







