Abstract
Informal caregivers are at risk of caregiver burden, and physical proximity to the care recipient may add to this negative outcome. Yet, individual differences in emotional proximity to the care recipient such as attachment orientations may contribute to caregivers’ comfort towards different degrees of physical proximity, leading to varying levels of burden. The current study is the first to explore the role of physical proximity on caregiver burden as moderated by attachment orientations. A sample of 162 Israeli caregivers who are active users of the Camoni website completed our online survey. Sociodemographic characteristics, including a self-reported questionnaire on the physical proximity to the care recipient, were collected. Caregivers’ attachment orientations were assessed with the Experiences in Close Relationships–Relationship Structures questionnaire. Caregiver burden was assessed using the Caregiver Burden Inventory. Multiple regression and simple slope analyses were conducted. Attachment anxiety and avoidance were positively associated with burden, whereas physical proximity was not. Attachment avoidance, but not attachment anxiety, moderated the association between physical proximity and caregiver burden, with caregivers who live closer to their care recipient experiencing greater burden when high levels of avoidance were present. Our findings reveal the complex dynamics between attachment orientations and physical proximity in the context of informal care, highlighting the need for better integration of these two interlinked constructs in both care research and practice.
1. Introduction
With the growth in ageing populations and increasing prevalence of chronic illness, the number of care-dependent adults is rising [1,2,3,4,5]. Informal caregivers, who provide unpaid care to family members or friends with a chronic illness, play a vital societal role in sustaining long-term care settings and maintaining outpatient care [6,7]. Caregiving encompasses a wide variety of activities and tasks including social and emotional support, assistance with activities of daily living (e.g., bathing, toileting) and household tasks, management of financial affairs and monitoring of healthcare services [7].
Caregivers can experience both positive and negative outcomes as a result of their caretaking responsibilities [8,9,10]. Informal care can lead to an enhanced relationship with the care recipient and feelings of personal growth and satisfaction for the care provided and the skills obtained [8,11,12,13]. At the same time, many caregivers are at risk of experiencing adverse health and psychosocial effects related to their caregiving role, such as poor physical and mental health [13,14,15,16,17], financial problems [18], loneliness and social isolation [19]. A negative appraisal of the caregiving situation can increase caregiver burden, an experience described as a multidimensional response to the physical, psychological and emotional toll of caring [15,16,17].
1.1. Physical Proximity and Caregiving
The physical proximity between caregivers and their care recipient is an important structural factor that might determine the care provided and shape the caregiving experience [20,21]. In recent decades, demographic and social changes such as increased societal mobility and population migration have affected the traditional patterns of providing informal care [20,21]. While several caregivers continue to live with their care recipient, many others provide care from a geographic distance [21,22].
Geographically diverse caregiving samples may present with different caretaking responsibilities and unique needs and burdens associated with the physical proximity to their care recipient. Prior studies have found that those who live with their care recipient or very close to them experience high levels of burden and emotional distress, potentially resulting from greater competition between caretaking responsibilities and other time-demanding activities when co-residing or living within a proximal distance [23,24]. On the other hand, geographic distance can create additional burdens for what is already often stressful care work. In the few studies conducted, distance caregivers (DCGs) reported high levels of burden and emotional distress related to feelings of inadequacy on how to assess the needs of their loved one from afar and uncertainty regarding the progression of their illness [21,25]. Experiencing the added challenges of caring from afar—such as the need of travelling back and forth to provide hands-on care to their loved one—DGCs also reported that caring was taxing on their finances, job accomplishments and social and familial relationships [26,27].
Despite evidence on the unique complications and challenges experienced by geographically diverse caregiving populations, research on the role of physical proximity on caregiver burden remains scarce. In their recent study, Li et al. found that DCGs who live more than 30 min away from their frail elderly parents are more distressed by subjective burden than those who co-reside or live closer to the care recipient [21]. However, another comparative study found that caregivers who live closer to the care recipient experience greater levels of social and emotional strain [28].
1.2. Emotional Proximity and Caregiving
Individual differences among caregivers, and particularly differences in personal characteristics related to the ability and willingness to perform the caregiving role, may affect caregivers’ comfort and appraisals towards their physical proximity or distance from the care recipient, leading to varying degrees of caregiver burden [6]. One such personal characteristic is attachment orientation. According to the theory of attachment, during the early years of life, an emotional bond is formed between infants and their primary caregivers [29]. This early attachment towards the primary caregiver influences interpersonal relationships and individuals’ ability to form and maintain new emotional bonds with others later in life [29,30,31]. Attachment is commonly conceptualized as two orientations: attachment anxiety (“hyper-activation of the attachment system”) and attachment avoidance (“deactivation of this system”). Anxious–ambivalent people are clingier in their relationships and worry that the attachment figure will not be available in times of need, whereas avoidant people prefer not to rely on others, seeking independence and avoiding intimate and close relationships [31]. Individuals who score low on both orientations are considered securely attached. Securely attached individuals tend to be more comfortable with their significant others and feel competent in their ability to regulate affect in stressful situations [31].
A major stressor such as a chronic health condition of a significant other is likely to activate the attachment system, shaping caregivers’ reaction to the care recipient’s needs [32,33]. Individuals with greater attachment security tend to provide informal care that is sensitive, cooperative, and warm [6]. Conversely, insecurely attached individuals are less likely to provide sensitive care. For example, avoidant individuals’ rigid self-reliance and discomfort with closeness seem to moderate their ability to provide responsive caregiving. Anxious caregivers tend to provide a kind of care that is focused more on self-needs than their care recipient’s needs, perhaps due to their own anxiety of receiving less attention than their significant other who is ill [6]. Empirical findings have also indicated that insecure attachment patterns of caregivers positively correlate with poorer mental health [34,35,36,37,38,39]. Specifically, higher attachment anxiety has been related to higher levels of caregiver burden [37,38], depression and anxiety [36,37], whereas attachment avoidance has been positively related to health problems [38] and negatively related to self-esteem [36,39]. In contrast, higher levels compared with lower levels of attachment security have been found to be associated with lower levels of burden and better wellbeing [34,35,36,37,38,39].
1.3. The Current Study
Attachment towards a significant other is closely interlinked with physical proximity. In fact, spatial concepts such as closeness, distance and proximity seeking appear prominently in attachment theory, with the starting point of the theory being the presumption of a biologically based drive for physical proximity with primary caregivers [40,41,42]. In both infants and adults, physical closeness to an attachment figure is considered to provide a safe haven, fostering a fundamental sense of security and alleviating distress and anxiety during stressful situations [40,41]. In contrast, physical distance and long separation from the attachment figure are potentially disruptive and disorienting, as proximity in attachment relationships has been argued to activate a neuro-psychobiological process by which individuals reciprocally regulate one another’s mental and physical states [40,41]. Previous studies on the associations between adults’ attachment orientations and physical proximity have focused on romantic relationships [42,43,44,45]. For example, Feeney (1998) revealed that securely attached individuals have more positive perceptions of their relationship and are more likely to use viable coping strategies when dealing with physical separation [43]. Conversely, individuals with higher levels of attachment anxiety tend to experience more severe reactions of discomfort when separated from their partners and are more likely to respond to this physical separation with feelings of insecurity [43].
Differences in caregivers’ attachment orientations may moderate the relationship between physical proximity and caregiver burden. For example, highly anxious caregivers who live far away from the care recipient may be more stressed because of vigilance to their loved one’s accessibility. Therefore, high anxious attachment may uniquely interact with physical distance, predicting higher levels of burden for those who live further away, but not for proximate caregivers. In contrast, highly avoidant caregivers who eschew intimate relationships and seek independence may report higher levels of burden when they are physically proximate to their care recipient compared with being physically distant. Knowledge on the associations between physical proximity to the care recipient, attachment orientations and caregiver burden can provide unique and valuable insights into the translation of these aspects in the caregiving experience. Considering the interlinked nature of structural and individual factors in the context of care might help us to better understand the complexities of care provision and shed light on the experiences of caregiver burden among diverse caregiving populations. This is in line with the integrative framework proposed by Revenson et al. [6], suggesting that for studying caregiving in the illness context we should examine both the individual characteristics of caregivers and their living environment and broader context.
Therefore, in this study, we examined the relationship between physical proximity to the care recipient and caregiver burden as moderated by caregivers’ attachment orientations. Specifically, the study aimed to answer the following questions:
- Does caregiver burden differ according to the physical proximity to the care recipient?
- Does caregiver burden differ according to caregivers’ attachment orientations?
- Do caregivers’ attachment orientations moderate the relationship between physical proximity and caregiver burden?
2. Materials and Methods
2.1. Study Design and Site
An online cross-sectional survey was conducted among users of the Camoni website [46]. Launched in 2009, Camoni is the first Hebrew-language, nonprofit social support network site for patients with a chronic illness and their caregivers. Camoni—which in Hebrew means “Like me”—is comprised of 40 communities defined according to specific health conditions (e.g., heart disease, memory impairment, stroke, different types of cancer, etc.) and consists of 70,000 registered users. The website offers free-of-charge advice and medical recommendations as well as connection with other caregivers and care recipients who face the same health conditions. It includes online tools, blogs, forums, support groups and internal e-mail options.
2.2. Procedure
Ethical approval for the study was granted on 2 December 2019 by the Gertner institute review board. Data collection took part between the beginning of January 2020 and the end of March 2020. During the recruitment period, a web-based version of the self-reported questionnaire was sent to the email addresses that Camoni users had provided on registration. The survey link was also made available on the “Camoni” homepage of each of the chronic illness communities and the general caregiving community. Participation in the study was voluntary. Individuals interested to participate had to click on the survey link and provide informed written consent before taking part in the survey. Participants had the right to withdraw from the study at any time.
2.3. Participants
A total of 162 informal caregivers who were active users of the Camoni website gave their consent to participate in the online survey and completed the relevant demographics and outcome measures used for the current study. There were no missing data in the final sample size as participants could answer a question only if they had completed the previous ones. Participants could be primary or secondary caregivers and live with or separately from the care recipient. Eligibility criteria were as follows: (i) age 18 or over; (ii) being able to answer the survey in Hebrew; (iii) providing unpaid care to a family member or friend with a chronic illness, disability or frailty.
2.4. Survey Development
The self-reported questionnaire was developed by the authors with survey items and psychometric instruments informed by the research questions and the current caregiving literature. Specifically, previous research studies investigating attachment orientations [34,36], physical proximity to the care recipient [21] and caregiver burden [34] were used as resources. A short description of the survey items used for this study is presented in the following section.
3. Measures
3.1. Sociodemographic Characteristics
A self-reported questionnaire was used to gather the sociodemographic characteristics of informal caregivers and their care recipient. These included caregivers’ age, gender, relationship status, ethnicity, religiosity, socioeconomic status, highest level of education and existing health conditions. Caregivers were also asked to specify the type of relationship with the care recipient and the care recipient’s health condition.
3.2. Physical Proximity to the Care Recipient
Caregivers’ physical proximity to their care recipient was conceptualized as a continuous variable and measured by two self-reported items. First, participants were asked whether they co-reside with their care recipient: “Do you share a household with your loved one? Yes/No”. For those who replied Yes, proximity was coded as 0, indicating co-residence. If participants replied No, they were then asked to specify in minutes how long it takes them to arrive at the care recipient’s home: “How far (in minutes) is your home from the place where your loved one lives?”. For those participants, their answer was coded as the exact number of minutes reported. Travel time in minutes was chosen instead of miles or kilometers, because caregivers who reside a similar distance from their care recipient but use different modes of transportation may differ in the time needed to reach the care recipient’s place of residence [22].
3.3. Attachment Orientations
Caregivers’ attachment orientations were assessed using the Experiences in Close Relationships–Relationship Structures questionnaire (ECR-RS) [47]. The ECR-RS is a self-reported questionnaire designed to assess the two dimensions of attachment anxiety and avoidance using 9 items: 3 for the anxiety subscale (e.g., “I often worry that this person doesn’t really care for me”); 6 for the avoidance subscale (e.g., “I prefer not to show a partner how I feel deep down”). Caregivers were asked to rate the extent to which each item of the questionnaire was descriptive of their feelings, on a scale ranging from 1 (not at all) to 7 (very much). Scores were computed separately for each of the two subscales by averaging their item responses. Higher scores denote higher levels of attachment anxiety or avoidance. The measure has been shown to have good reliability and validity [46]. In the present study, Cronbach’s alpha was 0.74 for attachment anxiety and 0.70 for avoidance.
3.4. Caregiver Burden
Caregiver burden was measured using the Caregiver Burden Inventory (CBI) developed by Novak and Guest (1989) [48]. CBI is a 24-item multidimensional questionnaire evaluating caregiver burden with five subscales: (a) time dependence; (b) development; (c) physical burden; (d) social burden; (e) and emotional burden. Sample items include the following: (a) “I don’t get a minute of rest”; (b) “I feel that I am missing experiences in life”; (c) “I am sleep-deprived”; (d) “My functioning at work is not at the same level as it was in the past”; (e) “I am angry about our relationship”. Caregivers were asked to rate the extent to which each of the 24 items describe their feelings on a 5-point Likert scale ranging from 0 (not at all) to 4 (very much). A total burden score was obtained by summing item responses (range 0–96), with higher scores reflecting higher levels of burden. Overall, total scores nearly or slightly above 24 are considered to indicate a need of respite, whereas scores above 36 are considered to indicate a risk of burnout. The Hebrew version of the self-reported questionnaire has been previously validated using an Israeli sample of wives of war veterans, diagnosed with post-traumatic stress disorder and brain injuries [49]. Scores of the Hebrew version have previously shown high reliability [34,49]. In the present sample, Cronbach’s alpha was 0.94.
3.5. Statistical Analysis
Statistical analyses were conducted using IBM SPSS Statistics v25 software (IBM Corp, Armonk, NY, USA). Descriptive statistics were used for summarizing participant sociodemographic characteristics. Correlation analyses, independent-samples t-tests and one-way analysis of variance (ANOVA) were performed for examining the association of sociodemographic characteristics with CBI total score. For significant ANOVAs, Tukey post hoc analyses were performed to determine which group was significantly different from the others. Correlation analyses also examined the interrelationships of attachment orientations, physical proximity to the care recipient and caregiver burden.
Multiple linear regression was performed to test the direct effects of attachment and physical proximity, and the interaction effects of attachment × physical proximity on caregiver burden. In step 1, selected demographic characteristics were entered as potential confounding variables. In step 2, caregiver attachment and physical proximity to the care recipient were entered. To predict the interaction effects of attachment and physical proximity on caregiver burden, two interaction terms—attachment anxiety × physical proximity; attachment avoidance × physical proximity—were entered in centered scores in step 3. All three continuous variables—attachment anxiety, avoidance and physical proximity—were mean-centered prior to creating the two interaction terms. The interaction terms were then created by taking the product of the two mean-centered main effects, respectively. Statistical significance was set at p < 0.05.
4. Results
4.1. Sociodemographic Characteristics
Sociodemographic characteristics are presented in Table 1. The sample consisted of 162 Israeli Jewish caregivers, the majority of them women (67.3%), with a mean age of 57 ± 15.2 years. The caregivers’ age varied with the youngest being 18 years and the oldest 90 years. Majority of the caregivers had obtained a university degree (34.6% had a Bachelor’s degree and 24.1% had a Master’s or PhD degree) and were married or had a partner (75.9%). Consistent with the Israeli Jewish society, most caregivers described themselves as secular (70.4%) [50]. More than a third of the sample (40.8%) reported a low socioeconomic status and had a physical impairment/disability (45.1%). Caregivers were most commonly providing care for their spouse/partner (41.4%) or parent (27.2%). The largest group of the care recipients had some type of cancer or heart disease (34%), followed by care recipients with multiple chronic conditions (26.5%) and those with a physical disability or impairment (13%).

Table 1.
Sociodemographic characteristics.
4.2. Univariate Analyses
Table 2 presents the means, SDs and intercorrelations between the study’s main variables. Participants displayed a relatively high mean score on the CBI as well as high variance. The mean of physical proximity between caregivers and their care recipient also varied. The minimum distance to the care recipient was 0 min, indicating co-residence ((60.4%) of the sample reported co-residence, n = 98), whereas the maximum was 180 min. Among caregivers who did not co-reside with the care recipient (n = 64), the mean of physical proximity was 30.02 ± 32.59 min. Correlational analyses showed significant positive associations between caregiver burden with attachment anxiety and avoidance but not with physical proximity.

Table 2.
Means, SDs and intercorrelations between caregiver burden, attachment anxiety, attachment avoidance and physical proximity to the care recipient.
Independent-samples t-tests and ANOVAs were performed when analyzing demographic characteristics in relation to CBI total score. As illustrated in Table 3, three variables were found to be associated with caregiver burden: caregiver’s health condition; relationship to the care recipient; and care recipient’s health condition. Tukey post hoc analyses revealed that caregivers with multiple health conditions were significantly more burdened than those who reported no condition, p = 0.016. Furthermore, caregivers who cared for a spouse/partner (p = 0.013), parent (p < 0.001) or child (p = 0.004) presented with significantly higher levels of burden than those whose care recipient was a nonrelative member. Post hoc analyses did not reveal any differences on caregiver burden depending on the care recipient’s disease. Gender, education, socioeconomic and relationship status were not associated with caregiver burden. Correlation of caregiver age with burden was also not significant, r (160) = −0.108, p > 0.05.

Table 3.
Differences in caregiver burden depending on sociodemographic variables.
4.3. Multivariate Analyses
Table 4 shows the results of the multiple regression analysis, utilized to determine predictors of caregiver burden. In the first block of variables, the significant sociodemographic characteristics from ANOVAs, presented in Table 3, were entered as confounding variables. All three variables, caregiver’s health condition (four category variable), relationship to the care recipient (five category variable) and care recipient’s health condition (seven category variable) were recoded into three, four and six dummy variables, respectively (the number of dummy-coded variables is the number of levels minus one). Caregivers with no health conditions or disabilities, those who provided care to a nonrelative member and those who stated that their care recipient had another condition from the ones presented served as the reference categories for these three, four and six dummy variables, respectively. Based on former findings [51,52,53], age and gender were also factored as potential confounders in the regression model, despite not being found significant in the univariate analyses.

Table 4.
Summary of multiple regression model for caregiver burden.
The results of the regression model indicated that sociodemographic characteristics, added in step 1, accounted for a significant 22.3% of the total variance and that the model was a significant predictor of caregiver burden, F (15,146) = 2.99, p < 0.001. Specifically, caregivers with a physical impairment or disability, and those with multimorbidity, were more likely to present with higher levels of burden compared with those who had no health conditions or difficulties. Additionally, providing care to a spouse/partner, parent or child was also associated with higher burden than caring for a nonrelative member.
In step 2 of the regression analysis, attachment anxiety, avoidance and physical proximity were factored in the model. The increase in R2 was significant and explained an additional 21.4% of variance in caregiver burden, F change (3143) = 17.06, p < 0.001. Within step 2, attachment anxiety and avoidance, were significantly and positively associated with burden. However, physical proximity to the care recipient was not.
Finally, the two interaction terms, attachment anxiety × physical proximity and attachment avoidance × physical proximity, were entered into the equation. The increase in R2 was significant, explaining an additional 2.7% of variance in caregiver burden—F change (2141) = 3.55, p < 0.031. The attachment avoidance × physical proximity interaction term was significantly and negatively associated with burden whereas the anxiety × physical proximity term was not. To examine the direction of the significant interaction effect, a simple slope analysis was performed. Figure 1 presents the associations between physical proximity to the care recipient (ranging from low to high proximity) and caregiver burden, for high versus low levels of attachment avoidance (attachment avoidance was plotted at ±1 SD around the mean). Caregivers who live closer to their care recipient (including co-residing caregivers) presented higher burden at high (B = −0.36, p =0.017) but not low levels of attachment avoidance (B = 0.04, p > 0.05).
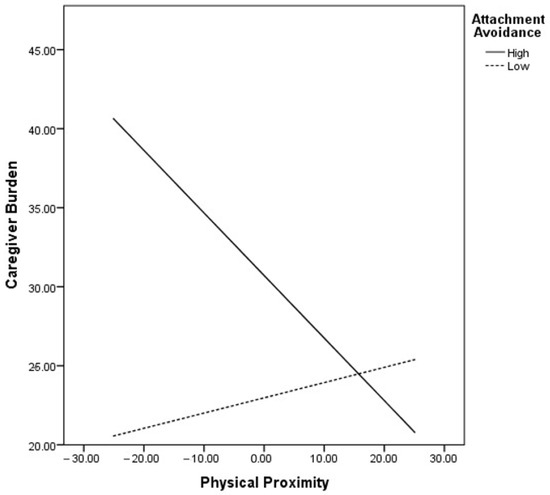
Figure 1.
Moderating effect of attachment avoidance in the relationship between physical proximity to the care recipient and caregiver burden (mean-centered variables).
A sensitivity analysis was performed to test the moderating effect of attachment avoidance only among non-co-residing caregivers. The results were similar to those of the main analysis, revealing that caregivers who live closer to their care recipient experience greater burden at high (B = −0.23, p =0.029) but not low levels of attachment avoidance (B = 0.01, p > 0.05).
5. Discussion
5.1. Sociodemographic Characteristics
Approximately two thirds of our sample reported physical and mental health problems or multimorbidity. This finding is consistent with previous studies suggesting that caregivers are at risk of poor health [54,55,56,57,58,59]. Caregivers who had a physical impairment/disability or multiple health conditions experienced higher burden than those with no health condition. Caring for a loved one in the midst of your own deteriorating health may create additional burdens and lead to greater strain. Our results are in line with prior research indicating that caregivers’ health and burden are associated [58,59].
Participants who provided care to a spouse/partner, parent or child presented with higher levels of burden than those who cared for a nonrelative member. Family caregivers have been previously found to report greater perceived strain and lower self-rated health than nonfamily caregivers [60,61]. This might be explained by the fact that caregivers related by blood or marriage are more likely to be primary caregivers, whereas caregivers of friends and neighbors have usually less primary caretaking responsibilities [62,63,64,65]. However, in this study, the amounts of care provision and caregiver involvement were not assessed.
Prior reports have suggested that caregivers who are advanced in age [66], women caregivers [67], those with lower levels of socioeconomic status [68,69] and those caring for a care recipient with cognitive impairment [70,71], cancer [72,73,74] and heart disease [75,76] experience greater burden; however, our results did not reveal any significant differences. However, the effect of some of these sociodemographic variables may be mediated by other caregiving or care-receiving characteristics [77].
5.2. Main Findings
Attachment anxiety and avoidance were found to be directly and positively associated with caregiver burden, after controlling for several sociodemographic characteristics. Empirical findings have suggested that insecure attachment relates to adverse health outcomes and is predictive of emotional distress in the context of caregiving [34,35,36,37,38,39]. In line with our findings, a previous systematic review found that attachment anxiety was associated with poor mental health including increased levels of burden, depression and anxiety in 66.6% of mental health outcomes assessed across caregiving studies [36]. Anxiously attached individuals engage in more compulsive and hypervigilant forms of care provision [34,36,38]. This pattern of care is reported to be often motivated by self-focused attention and worries; it is also reported to overwhelm caregivers, physically and emotionally, as they feel deprived from having their own needs fulfilled [34,38]. The strains accompanying the caregiving role may further exacerbate those caregivers’ feelings that they are consumed by their care recipient’s needs, which must take precedence over their own [34,36].
Caregivers high on the attachment avoidance scale differed significantly from those with a lower avoidant attachment and reported higher levels of burden. The rigid self-reliance and use of cognitive and behavioral deactivating strategies in order to suppress negative affect have been previously suggested to protect avoidant caregivers from experiencing interpersonal distress and reduce the likelihood that mental health issues such as burden manifest [36]. In their review, Karantzas and colleagues [36] found that caregivers with attachment avoidance demonstrated a more controlling manner of caregiving and lacked emotional and physical closeness. Attachment avoidance was not associated with mental health outcomes in any of the reviewed studies [36]. However, as the authors highlight, the strategies that caregivers who show a high degree of attachment avoidance adopt, may not be sustainable for long periods [36]. Experiencing a significant other’s chronic illness and being placed in the role of caregiver, may make it more difficult for highly avoidant caregivers to suppress their distress and remain emotionally detached. This is in line with previous findings, revealing that in time of crisis and when facing a major stressor such a chronic health condition, deactivating strategies are not effective in regulating distressing emotions [34,78,79].
Physical proximity to the care recipient was not associated directly with burden in the correlation analyses. However, the moderation analyses revealed that the relationship between proximity and burden was moderated by attachment avoidance. Specifically, it was found that living closer to the care recipient was associated with increased levels of burden for caregivers with high but not low levels of attachment avoidance. These results support our hypothesis that comfort with interpersonal physical proximity may be related to comfort with interpersonal emotional proximity in caregiving. Consistent with the theory of attachment, caregivers may tolerate physical proximity in accordance with their attachment orientations, with those who are highly avoidant and seek emotional distance being less tolerant to physical closeness and thus more vulnerable to the pressures of caring when living closer to their care recipient [40,41,42]. Our finding is also in line with prior studies of attachment orientations and physical proximity in romantically involved adults, suggesting that more securely attached individuals are more able to seek proximity with their partner, whereas more avoidantly attached individuals may retract from their partner, both emotionally and physically [30,80,81].
Attachment anxiety did not moderate the association between physical proximity and caregiver burden. One possible explanation could be that interaction effects between attachment anxiety and physical proximity need more geographic heterogeneity and longer distances to appear. In our sample, only 7 caregivers had to travel a very long distance to reach their care recipient (>1 h), with majority of participants co-residing with the care recipient (n = 98) or living less than 30 min away (n = 47). Highly anxious DCGs who have to travel long distances may be more distressed because of vigilance to their loved one’s accessibility when compared with proximate caregivers who live closer or co-residing caregivers. Conversely, proximate and co-residing caregivers high on the attachment anxiety scale may present with comparable levels of burden as they access their care recipient in similar ways.
5.3. Strengths and Limitations
To the authors’ knowledge, the present study is the first to provide evidence on the moderating role of attachment orientations in the relationship between physical proximity and caregiver burden, highlighting the need for better integration of these two interlinked constructs—attachment and physical proximity—in the context of care, and serving as the foundation for future research in the field. In addition, the study includes the use of a diverse cohort of caregivers assisting care recipients with different health conditions. The sample diversity allows for broader generalization of results. Furthermore, adjustment for significant confounders, including age, gender and caregiver and care recipient characteristics, allows for more confidence in the associations reported.
Despite the strengths of this study, several limitations merit comment. First, the relatively small sample size might not be representative for exploring the role of varying degrees of physical proximities and their interaction with attachment orientations, as most caregivers co-resided with their care recipient or lived in short distances from them. Future studies should use larger samples including caregivers of various and more diverse geographic settings (e.g., countries with long travel distances) to gain a better understanding of how different proximities interact with attachment orientations and their impact on caregiver burden. Second, we conceptualized physical proximity by focusing exclusively on the travel time needed to the care recipient’s house and without assessing other—closely interlinked with time—geographic aspects such as accessibility and mode of transportation, travel costs, personal mobility problems, etc. Future research could adopt a more nuanced approach into the factors which constitute physical proximities and distances in caregiving, to adequately map these factors and enable the identification of diverse caregiving profiles. Third, our study used a cross-sectional design which precludes forming clear cause-and-effect inferences about the relationship between our study variables and caregiver burden. Future studies should use longitudinal designs to understand causal mechanisms of caregiver burden over time. Finally, the amount of care provision and caregiver involvement were not explored in this study. It is recommended that future research on physical proximities controls for the time spent in caregiving and the involvement in various care tasks, as previous studies have demonstrated significant relationships between these factors and caregiver outcomes [58,82].
6. Conclusions
Despite the above limitations, the present study has important implications for clinical practice. We found that attachment anxiety and avoidance are positively associated with burden, whereas physical proximity is not. Attachment avoidance moderated the association between physical proximity and caregiver burden, with caregivers who live closer to their care recipient experiencing greater burden when high levels of avoidance are present.
Pursuant to our findings, interventions for caregivers should adopt an integrative approach, encompassing interlinked dispositional and structural factors such as caregivers’ attachment orientations and physical proximity to their care recipient. Coping strategies adopted by highly avoidant individuals who are less tolerant to physical closeness may be less effective in lowering distress and burden when facing a significant other’s health condition and being placed in the role of proximal caregiver. Support and training skills interventions considering the interlinked nature of attachment orientations with physical proximity could identify and help insecurely attached caregivers in coping with the specific care demands of proximal living arrangements—such as co-residence—to alleviate burden. In addition, highly avoidant caregivers who live with the care recipient or close to them may benefit from interventions which aim to increase attachment security and comfort with physical closeness [31,83]. Security-enhancing interventions may be also beneficial for anxiously attached caregivers, given our finding that attachment anxiety is associated with caregiver burden. Lastly, our results show that individual caregiver and care recipient characteristics—including caregivers’ health status and the type of relationship with the care recipient—should also be considered when designing support interventions as they could further inform the implementation of sustainable solutions for diverse groups of informal caregivers with different needs and burdens.
Author Contributions
Conceptualization, E.B. and N.V.; data curation, E.B., K.M., S.G.-S. and N.V.; project administration, E.B., O.K.-L., T.S. and N.V.; formal analysis, E.B., K.M. and N.V.; investigation, E.B., K.M., O.R.-M. and N.V.; methodology, E.B., K.M. and N.V.; validation; E.B., K.M., O.R.-M., S.G.-S. and N.V.; visualization, E.B. and N.V.; writing—original draft preparation, E.B.; supervision, O.R.-M., O.K.-L., T.S. and N.V.; writing—review and editing, E.B., K.M., O.R.-M., S.G.-S., O.K.-L., T.S. and N.V. All authors have read and agreed to the published version of the manuscript.
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 814072 and is part of The European Training Network on Informal Care (ENTWINE).
Institutional Review Board Statement
This study was approved by the IRB at the Gertner Institute (No: 6426-19-SMC) and was conducted according to the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Data will be available upon reasonable request to the corresponding author.
Acknowledgments
This study was undertaken as part of postgraduate study conducted by author Eva Bei.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rodríguez, B.C.; Castiñeira, B.R.; Nunes, L.C. Alzheimer’s disease and the quality of life of the informal caregiver. Rev. Esp. Geriatr. Y Gerontol. 2019, 54, 81–87. [Google Scholar] [CrossRef]
- Li, J.; Han, X.; Zhang, X.; Wang, S. Spatiotemporal evolution of global population ageing from 1960 to 2017. BMC Public Health 2019, 19, 127. [Google Scholar] [CrossRef] [PubMed]
- Spasova, S.; Baeten, R.; Coster, S.; Ghailani, D.; Peña-Casas, R.; Vanhercke, B. Challenges in Long-Term Care in Europe: A Study of National Policies 2018; European Commission: Brussels, Belgium, 2018; ISBN 92-79-87174-9.
- Verbakel, E. How to understand informal caregiving patterns in Europe? The role of formal long-term care provisions and family care norms. Scand. J. Public Health 2018, 46, 436–447. [Google Scholar] [CrossRef] [Green Version]
- Colombo, F.; Llena-Nozal, A.; Mercier, J. Help Wanted? Providing and Paying for Long-Term Care; OECD Publishing: Paris, France, 2011. [Google Scholar]
- Revenson, T.; Griva, K.; Luszczynska, A.; Morrison, V.; Panagopoulou, E.; Vilchinsky, N.; Hagedoorn, M. Caregiving in the Illness Context; Springer: London, UK, 2016. [Google Scholar]
- Roth, D.L.; Fredman, L.; Haley, W.E. Informal caregiving and its impact on health: A reappraisal from population-based studies. Gerontologist 2015, 55, 309–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Loke, A.Y. The positive aspects of caregiving for cancer patients: A critical review of the literature and directions for future research. Psycho-Oncology 2013, 22, 2399–2407. [Google Scholar] [CrossRef]
- Lambert, S.D.; Levesque, J.V.; Girgis, A. The impact of cancer and chronic conditions on caregivers and family members. In Cancer and Chronic Conditions; Springer: Singapore, 2016; pp. 159–202. [Google Scholar] [CrossRef]
- Wang, Z.; Ma, C.; Han, H.; He, R.; Zhou, L.; Liang, R.; Yu, H. Caregiver burden in Alzheimer’s disease: Moderation effects of social support and mediation effects of positive aspects of caregiving. Int. J. Geriatr. Psychiatry 2018, 33, 1198–1206. [Google Scholar] [CrossRef]
- Parveen, S.; Morrison, V. Predicting caregiver gains: A longitudinal study. Br. J. Health Psychol. 2012, 17, 711–723. [Google Scholar] [CrossRef]
- Kim, Y.; Schulz, R.; Carver, C.S. Benefit finding in the cancer caregiving experience. Psychosom. Med. 2007, 69, 283–291. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. J. Soc. Work. Educ. 2008, 44 (Suppl. S3), 105–113. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef]
- Allen, A.P.; Curran, E.A.; Duggan, Á.; Cryan, J.F.; Chorcoráin, A.N.; Dinan, T.G.; Molloy, D.W.; Kearney, P.M.; Clarke, G. A systematic review of the psychobiological burden of informal caregiving for patients with dementia: Focus on cognitive and biological markers of chronic stress. Neurosci. Biobehav. Rev. 2017, 73, 123–164. [Google Scholar] [CrossRef] [PubMed]
- Chiao, C.Y.; Wu, H.S.; Hsiao, C.Y. Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int. Nurs. Rev. 2015, 62, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Faronbi, J.O.; Faronbi, G.O.; Ayamolowo, S.J.; Olaogun, A.A. Caring for the seniors with chronic illness: The lived experience of caregivers of older adults. Arch. Gerontol. Geriatr. 2019, 82, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Cipollone, A.; Patacchini, E.; Vallanti, G. Female labour market participation in Europe: Novel evidence on trends and shaping factors. IZA J. Eur. Labor Stud. 2014, 3, 18. [Google Scholar] [CrossRef] [Green Version]
- Vasileiou, K.; Barnett, J.; Barreto, M.; Vines, J.; Atkinson, M.; Lawson, S.; Wilson, M. Experiences of loneliness associated with being an informal caregiver: A qualitative investigation. Front. Psychol. 2017, 8, 585. [Google Scholar] [CrossRef] [Green Version]
- Baldassar, L.; Baldock, C.V.; Wilding, R. Families Caring across Borders: Migration, Ageing and Transnational Caregiving; Springer: Berlin, Germany, 2016. [Google Scholar]
- Li, M.; Mao, W.; Chi, I.; Lou, V.W. Geographical proximity and depressive symptoms among adult child caregivers: Social support as a moderator. Aging Ment. Health 2019, 23, 205–213. [Google Scholar] [CrossRef]
- Bei, E.; Rotem-Mindali, O.; Vilchinsky, N. Providing care from afar: A growing yet understudied phenomenon in the caregiving field. Front. Psychol. 2020, 11, 681. [Google Scholar] [CrossRef]
- Rokicka, M.; Zajkowska, O. Informal elderly caregiving and time spent on leisure: Evidence from time use survey. Ageing Int. 2020, 45, 393–410. [Google Scholar] [CrossRef]
- Mao, W.; Lou, V.W.; Li, M.; Chi, I. Coresidence and Well-Being among Adult Child Caregivers in Urban China: Impacts of the Domain-Specific Caregiver Burden. Soc. Work Res. 2022, 46, 44–52. [Google Scholar] [CrossRef]
- Edwards, M. Distance caregivers of people with Alzheimer’s disease and related dementia: A phenomenological study. Br. J. Occup. Ther. 2014, 77, 174–180. [Google Scholar] [CrossRef]
- Douglas, S.L.; Mazanec, P.; Lipson, A.; Leuchtag, M. Distance caregiving a family member with cancer: A review of the literature on distance caregiving and recommendations for future research. World J. Clin. Oncol. 2016, 7, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Cagle, J.G.; Munn, J.C. Long-distance caregiving: A systematic review of the literature. J. Gerontol. Soc. Work 2012, 55, 682–707. [Google Scholar] [CrossRef] [PubMed]
- National Alliance for Caregiving & AARP Public Policy Institute. Caregiving in the U.S. 2015. Available online: https://www.caregiving.org/research/caregivingusa/ (accessed on 15 May 2022).
- Bowlby, J. A Secure Base: Parent-Child Attachment and Healthy Human Development; Basic Books: New York, NY, USA, 1988. [Google Scholar]
- Ainsworth, M.D.S.; Blehar, M.C.; Waters, E.; Wall, S.N. Patterns of Attachment: A Psychological Study of the Strange Situation; Psychology Press: New York, NY, USA, 2015. [Google Scholar]
- Mikulincer, M.; Shaver, P.R. Boosting attachment security to promote mental health, prosocial values, and inter-group tolerance. Psychol. Inq. 2007, 18, 139–156. [Google Scholar] [CrossRef]
- Sroufe, L.A.; Carlson, E.A.; Levy, A.K.; Egeland, B. Implications of attachment theory for developmental psychopathology. Dev. Psychopathol. 1999, 11, 1–13. [Google Scholar] [CrossRef]
- Collins, N.L.; Feeney, B.C. A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. J. Pers. Soc. Psychol. 2000, 78, 1053–1073. [Google Scholar] [CrossRef]
- Vilchinsky, N.; Dekel, R.; Revenson, T.A.; Liberman, G.; Mosseri, M. Caregivers’ burden and depressive symptoms: The moderational role of attachment orientations. Health Psychol. 2015, 34, 262–269. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Sohn, B.K.; Lee, H.; Seong, S.J.; Park, S.; Lee, J.Y. Attachment style and filial obligation in the burden of caregivers of dementia patients. Arch. Gerontol. Geriatr. 2018, 75, 104–111. [Google Scholar] [CrossRef]
- Karantzas, G.C.; Romano, D.; Lee, J. Attachment and aged care: A systematic review of current research. Curr. Opin. Psychol. 2019, 25, 37–46. [Google Scholar] [CrossRef]
- Kuscu, M.K.; Dural, U.; Önen, P.; Yaşa, Y.; Yayla, M.; Basaran, G.; Turhal, S.; Bekiroğlu, N. The association between individual attachment patterns, the perceived social support, and the psychological well-being of Turkish informal caregivers. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. 2009, 18, 927–935. [Google Scholar] [CrossRef]
- Ávila, M.; Brandão, T.; Coimbra, J.L.; Lopez, F.; Matos, P.M. Experiencing an intimate partner’s breast cancer: Attachment, caregiving, and burden in men. Psychiatry 2016, 79, 236–248. [Google Scholar] [CrossRef]
- Porter, L.S.; Keefe, F.J.; Davis, D.; Rumble, M.; Scipio, C.; Garst, J. Attachment styles in patients with lung cancer and their spouses: Associations with patient and spouse adjustment. Support. Care Cancer 2012, 20, 2459–2466. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and Loss: Loss, Sadness and Depression; Basic Books: New York, NY, USA, 1980; Volume 3. [Google Scholar]
- Takano, T.; Mogi, K. Adult attachment style and lateral preferences in physical proximity. Biosystems 2019, 181, 88–94. [Google Scholar] [CrossRef]
- Fraley, R.C.; Shaver, P.R. Airport separations: A naturalistic study of adult attachment dynamics in separating couples. J. Pers. Soc. Psychol. 1998, 75, 1198–1212. [Google Scholar] [CrossRef]
- Feeney, J.A. Adult attachment and relationship-centered anxiety: Responses to physical and emotional distancing. In Attachment Theory and Close Relationships; Simpson, J.A., Rholes, W.S., Eds.; Guilford Press: New York, NY, USA, 1998; pp. 189–218. [Google Scholar]
- Shrivastava, A.; Burianova, A. Attachment styles, physical proximity, and relational satisfaction: A study of working professionals. Aviat. Psychol. Appl. Hum. Factors 2014, 4, 106–112. [Google Scholar] [CrossRef]
- Diamond, L.M.; Hicks, A.M.; Otter-Henderson, K.D. Every time you go away: Changes in affect, behavior, and physiology associated with travel-related separations from romantic partners. J. Pers. Soc. Psychol. 2008, 95, 385–403. [Google Scholar] [CrossRef] [Green Version]
- Camoni. Available online: https://www.camoni.co.il (accessed on 1 June 2022).
- Fraley, R.C.; Heffernan, M.E.; Vicary, A.M.; Brumbaugh, C.C. The experiences in close relationships—Relationship Structures Questionnaire: A method for assessing attachment orientations across relationships. Psychol. Assess. 2011, 23, 615–625. [Google Scholar] [CrossRef] [Green Version]
- Novak, M.; Guest, C. Application of a multidimensional caregiver burden inventory. Gerontol. 1989, 29, 798–803. [Google Scholar] [CrossRef]
- Ben-Arzi, N.; Solomon, Z.; Dekel, R. Secondary traumatization among wives of PTSD and post-concussion casualties: Distress, caregiver burden and psychological separation. Brain Inj. 2000, 14, 725–736. [Google Scholar] [CrossRef]
- Central Bureau of Statistics. Persons Aged 20 and Over, by Religiosity and by Selected Characteristics. 2020. Available online: https://www.cbs.gov.il/en/subjects/Pages/Population-by-Religion-and-Population-Group.aspx (accessed on 22 May 2022).
- Tseliou, F.; Rosato, M.; Maguire, A.; Wright, D.; O’Reilly, D. Variation of caregiver health and mortality risks by age: A census-based record linkage study. Am. J. Epidemiol. 2018, 187, 1401–1410. [Google Scholar] [CrossRef]
- Penning, M.J.; Wu, Z. Caregiver stress and mental health: Impact of caregiving relationship and gender. Gerontologist 2016, 56, 1102–1113. [Google Scholar] [CrossRef]
- Ge, L.; Mordiffi, S.Z. Factors associated with higher caregiver burden among family caregivers of elderly cancer patients: A systematic review. Cancer Nurs. 2017, 40, 471–478. [Google Scholar] [CrossRef]
- Berglund, E.; Lytsy, P.; Westerling, R. Health and wellbeing in informal caregivers and non-caregivers: A comparative cross-sectional study of the Swedish general population. Health Qual. Life Outcomes 2015, 13, 109. [Google Scholar] [CrossRef]
- Sallim, A.B.; Sayampanathan, A.A.; Cuttilan, A.; Ho, R.C.M. Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. J. Am. Med. Dir. Assoc. 2015, 16, 1034–1041. [Google Scholar] [CrossRef]
- Calvó-Perxas, L.; Vilalta-Franch, J.; Litwin, H.; Mira, P.; Garre-Olmo, J. A longitudinal study on public policy and the health of in-house caregivers in Europe. Health Policy 2021, 125, 436–441. [Google Scholar] [CrossRef]
- Yuda, M.; Lee, J. Effects of informal caregivers’ health on care recipients. Jpn. Econ. Rev. 2016, 67, 192–210. [Google Scholar] [CrossRef] [Green Version]
- Riffin, C.; Van Ness, P.H.; Wolff, J.L.; Fried, T. Multifactorial examination of caregiver burden in a national sample of family and unpaid caregivers. J. Am. Geriatr. Soc. 2019, 67, 277–283. [Google Scholar] [CrossRef]
- Limpawattana, P.; Theeranut, A.; Chindaprasirt, J.; Sawanyawisuth, K.; Pimporm, J. Caregivers burden of older adults with chronic illnesses in the community: A cross-sectional study. J. Community Health 2013, 38, 40–45. [Google Scholar] [CrossRef]
- Badana, A.N.; Marino, V.; Haley, W.E. Racial differences in caregiving: Variation by relationship type and dementia care status. J. Aging Health 2019, 31, 925–946. [Google Scholar] [CrossRef]
- Neal, M.B.; Ingersoll-Dayton, B.; Starrels, M.E. Gender and relationship differences in caregiving patterns and consequences among employed caregivers. Gerontologist 1997, 37, 804–816. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, A.; Figueiredo, D.; Sousa, L.; Demain, S. Coping with the caregiving role: Differences between primary and secondary caregivers of dependent elderly people. Aging Ment. Health 2011, 15, 490–499. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Mendiondo, M.; Smith, C.D.; Schmitt, F.A. Secondary dementia caregiving and its consequences. Am. J. Alzheimer’s Dis. Other Dement. 2003, 18, 300–308. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Families Caring for an Aging America. 2016. Available online: https://www.nap.edu/read/23606/chapter/1 (accessed on 2 May 2022).
- Himes, C.L.; Reidy, E.B. The role of friends in caregiving. Res. Aging 2000, 22, 315–336. [Google Scholar] [CrossRef]
- Viñas-Diez, V.; Turró-Garriga, O.; Portellano-Ortiz, C.; Gascón-Bayarri, J.; Reñé-Ramírez, R.; Garre-Olmo, J.; Conde-Sala, J.L. Kinship and cohabitation in relation to caregiver burden in the context of Alzheimer’s disease: A 24-month longitudinal study. Int. J. Geriatr. Psychiatry 2017, 32, e72–e82. [Google Scholar] [CrossRef] [PubMed]
- Verbakel, E.; Tamlagsrønning, S.; Winstone, L.; Fjær, E.L.; Eikemo, T.A. Informal care in Europe: Findings from the European Social Survey (2014) special module on the social determinants of health. Eur. J. Public Health 2017, 27 (Suppl. S1), 90–95. [Google Scholar] [CrossRef] [PubMed]
- Nasrabadi, A.N.; Sharif, S.P.; Allen, K.A.; Naghavi, N.; Nia, H.S.; Salisu, W.J.; Yaghoobzadeh, A. The role of socioeconomic status in the relationship between social support and burden among cancer caregivers. Eur. J. Cancer Prev. 2022, 31, 198–203. [Google Scholar] [CrossRef]
- Shrestha, D.; Rathi, S.; Grover, S.; Taneja, S.; Duseja, A.; Chawla, Y.K.; Dhiman, R.K. Factors affecting psychological burden on the informal caregiver of patients with cirrhosis: Looking beyond the patient. J. Clin. Exp. Hepatol. 2020, 10, 9–16. [Google Scholar] [CrossRef]
- Dauphinot, V.; Delphin-Combe, F.; Mouchoux, C.; Dorey, A.; Bathsavanis, A.; Makaroff, Z.; Rouch, I.; Krolak-Salmon, P. Risk factors of caregiver burden among patients with Alzheimer’s disease or related disorders: A cross-sectional study. J. Alzheimer’s Dis. 2015, 44, 907–916. [Google Scholar] [CrossRef] [Green Version]
- Kang, H.S.; Myung, W.; Na, D.L.; Kim, S.Y.; Lee, J.H.; Han, S.H.; Choi, S.H.; Kim, S.; Kim, S.; Kim, D.K. Factors associated with caregiver burden in patients with Alzheimer’s disease. Psychiatry Investig. 2014, 11, 152–159. [Google Scholar] [CrossRef] [Green Version]
- Grunfeld, E.; Coyle, D.; Whelan, T.; Clinch, J.; Reyno, L.; Earle, C.C.; Willan, A.; Viola, R.; Coristine, M.; Janz, T.; et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Can. Med. Assoc. J. 2004, 170, 1795–1801. [Google Scholar] [CrossRef] [Green Version]
- Jite, I.E.; Adetunji, A.A.; Folasire, A.M.; Akinyemi, J.O.; Bello, S. Caregiver burden and associated factors amongst carers of women with advanced breast cancer attending a radiation oncology clinic in Nigeria. Afr. J. Prim. Health Care Fam. Med. 2021, 13, a2812. [Google Scholar] [CrossRef]
- Seo, Y.J.; Park, H. Factors influencing caregiver burden in families of hospitalised patients with lung cancer. J. Clin. Nurs. 2019, 28, 1979–1989. [Google Scholar] [CrossRef] [PubMed]
- Ågren, S.; Evangelista, L.; Strömberg, A. Do partners of patients with chronic heart failure experience caregiver burden? Eur. J. Cardiovasc. Nurs. 2010, 9, 254–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pressler, S.J.; Gradus-Pizlo, I.; Chubinski, S.D.; Smith, G.; Wheeler, S.; Sloan, R.; Jung, M. Family caregivers of patients with heart failure: A longitudinal study. J. Cardiovasc. Nurs. 2013, 28, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Conde-Sala, J.L.; Turró-Garriga, O.; Calvo-Perxas, L.; Vilalta-Franch, J.; Lopez-Pousa, S.; Garre-Olmo, J. Three-year trajectories of caregiver burden in Alzheimer’s disease. J. Alzheimer’s Dis. 2014, 42, 623–633. [Google Scholar] [CrossRef] [Green Version]
- Berant, E.; Mikulincer, M.; Florian, V. The association of mothers’ attachment style and their psychological reactions to the diagnosis of infant’s congenital heart disease. J. Soc. Clin. Psychol. 2001, 20, 208–232. [Google Scholar] [CrossRef]
- Braun, M.; Mikulincer, M.; Rydall, A.; Walsh, A.; Rodin, G. Hidden morbidity in cancer: Spouse caregivers. J. Clin. Oncol. 2007, 25, 4829–4834. [Google Scholar] [CrossRef]
- Campbell, L.; Simpson, J.A.; Kashy, D.A.; Rholes, W.S. Attachment orientations, dependence, and behavior in a stressful situation: An application of the Actor-Partner Interdependence Model. J. Soc. Pers. Relatsh. 2001, 18, 821–843. [Google Scholar] [CrossRef]
- Kaitz, M.; Bar-Haim, Y.; Lehrer, M.; Grossman, E. Adult attachment style and interpersonal distance. Attach. Hum. Dev. 2004, 6, 285–304. [Google Scholar] [CrossRef]
- Pudelewicz, A.; Talarska, D.; Bączyk, G. Burden of caregivers of patients with Alzheimer’s disease. Scand. J. Caring Sci. 2019, 33, 336–341. [Google Scholar] [CrossRef]
- Gillath, O.; Karantzas, G.C.; Romano, D.; Karantzas, K.M. Attachment security priming: A meta-analysis. Personal. Soc. Psychol. Rev. 2022, 10888683211054592. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).