Cross-Cultural Adaptation and Validation of the Fear of COVID-19 Scale for Chinese University Students: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participant Characteristics
2.2. Ethical Considerations
2.3. Measures
2.3.1. Fear of COVID-19 Scale (FCV-19S)
2.3.2. Patient Health Questionnaire 9 (PHQ-9)
2.3.3. Generalized Anxiety Disorder Questionnaire (GAD-7)
2.4. Statistics Analysis
2.4.1. Reliability
2.4.2. Validity
3. Results
3.1. Item Analysis
3.2. Reliability Analysis
3.3. Validity Analysis
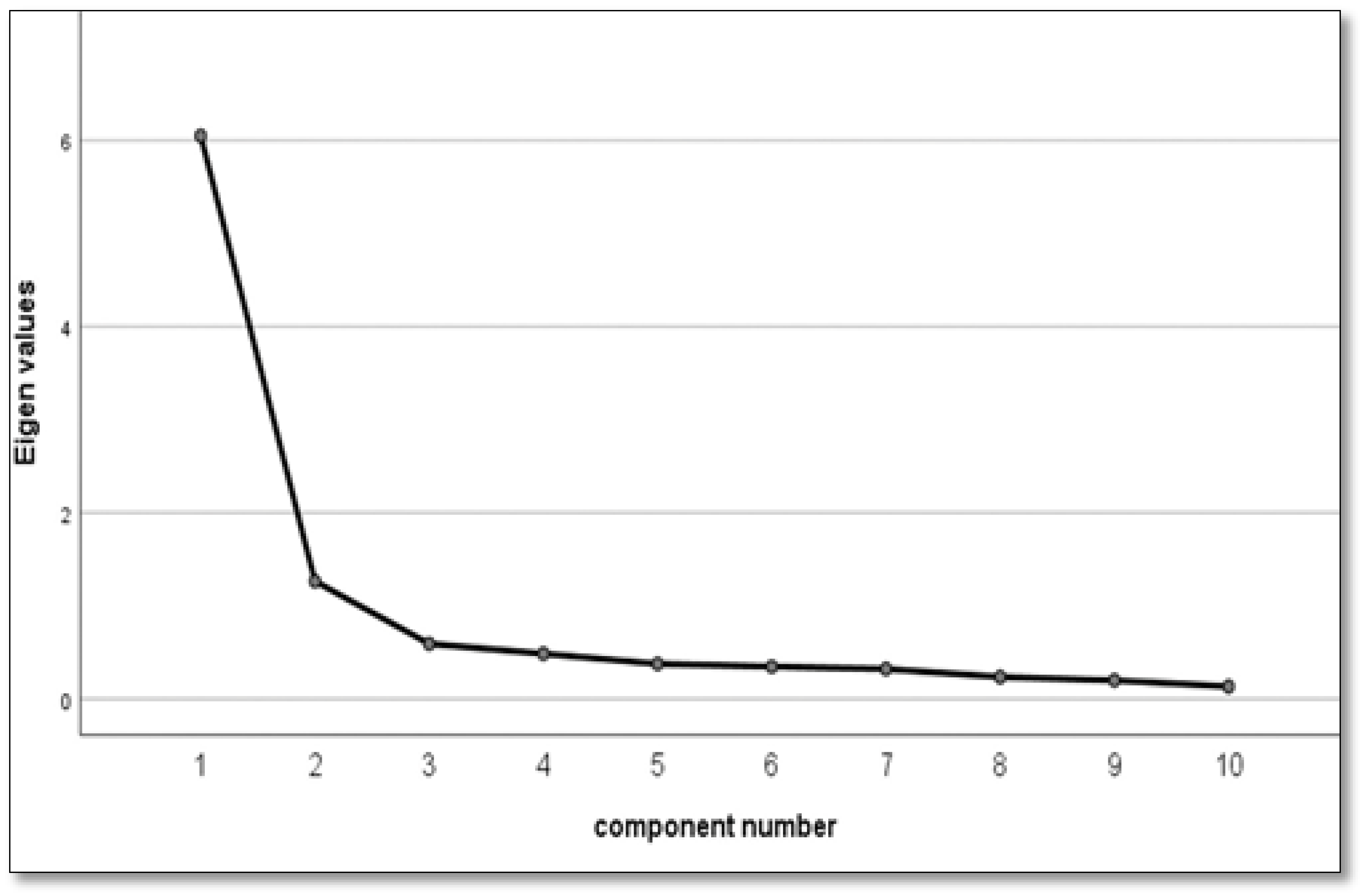
3.3.1. Exploratory Factor Analysis (EFA)
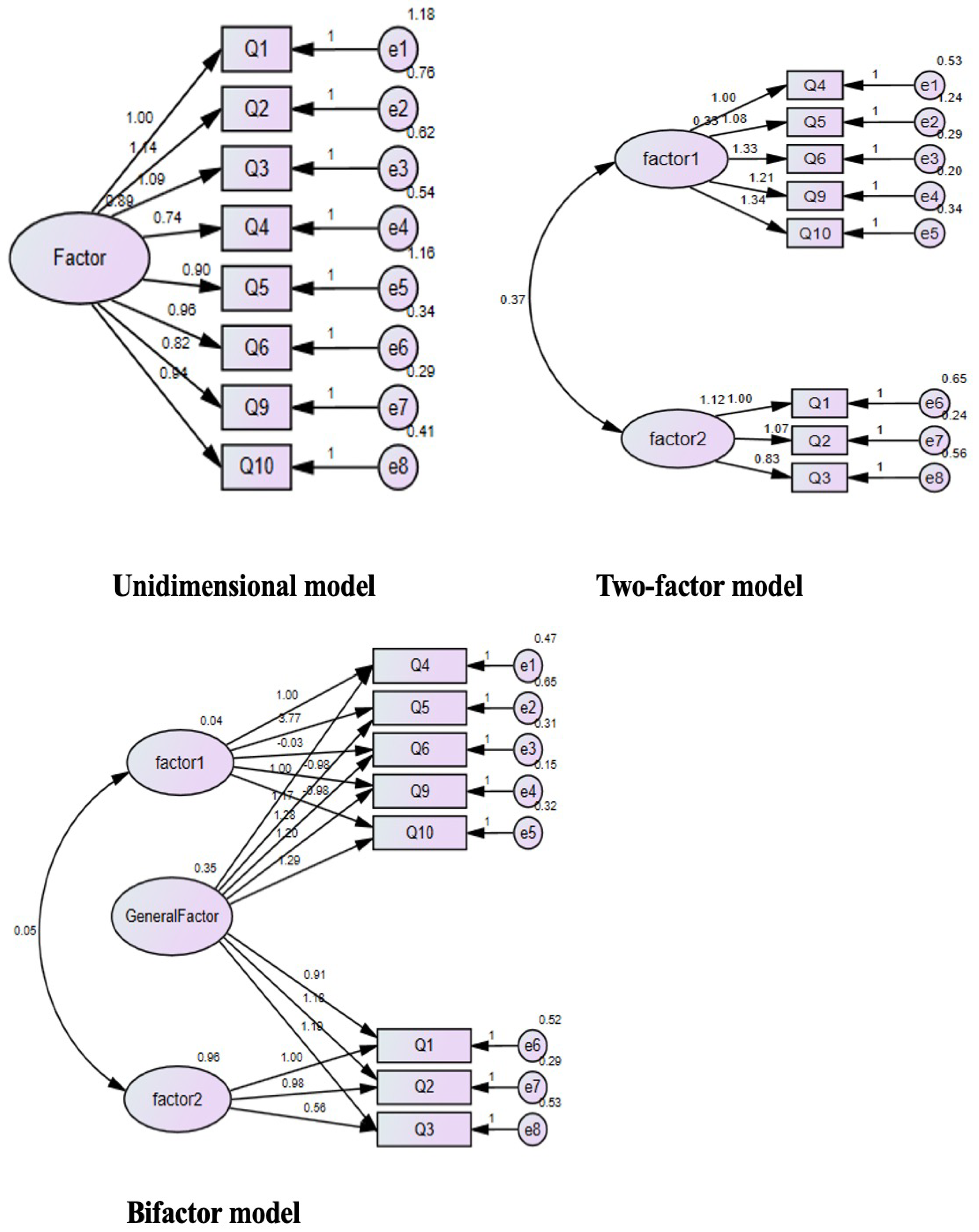
3.3.2. Confirmatory Factor Analysis (CFA)
3.3.3. Convergent Validity
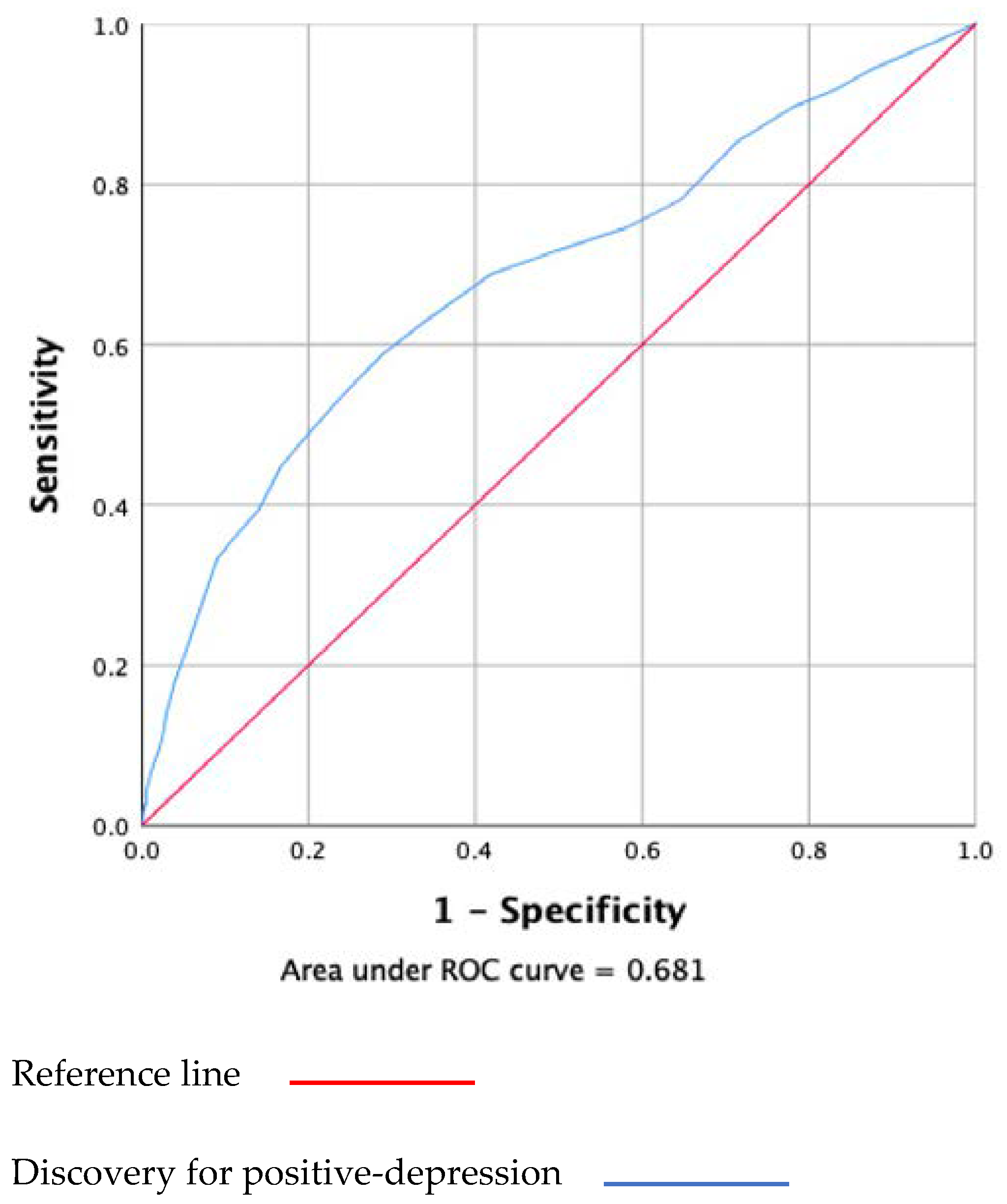
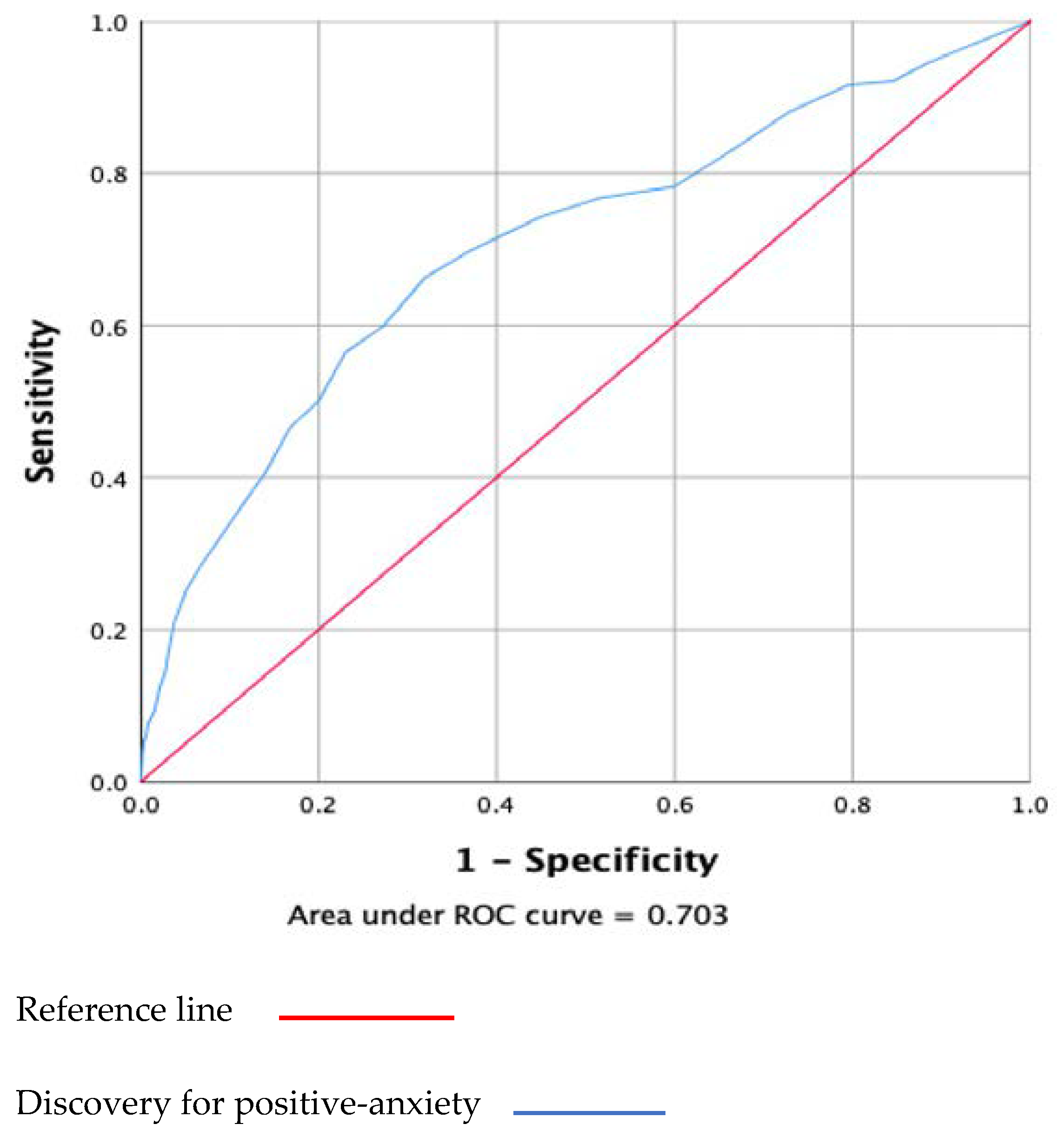
3.3.4. Diagnostic Accuracy and Criterion Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Items | Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree |
| I am most afraid of coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
| It makes me uncomfortable to think about coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
| I worry a lot about coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
| Coronavirus-19 is almost always terminal. | 1 | 2 | 3 | 4 | 5 |
| Coronavirus-19 is an unpredictable disease. | 1 | 2 | 3 | 4 | 5 |
| My hands become clammy when I think about coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
| I cannot sleep because I’m worrying about getting coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
| My heart races or palpitates when I think about getting coronavirus-19. | 1 | 2 | 3 | 4 | 5 |
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; McHugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health-The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef]
- Das, S. Mental Health and Psychosocial Aspects of COVID-19 in India: The Challenges and Responses. J. Health Manag. 2020, 22, 197–205. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef]
- Nikopoulou, V.A.; Holeva, V.; Parlapani, E.; Karamouzi, P.; Voitsidis, P.; Porfyri, G.N.; Blekas, A.; Papigkioti, K.; Patsiala, S.; Diakogiannis, I. Mental Health Screening for COVID-19: A Proposed Cutoff Score for the Greek Version of the Fear of COVID-19 Scale (FCV-19S). Int. J. Ment. Health Addict. 2020, 20, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Liang, Y.; Yin, X.; Zhou, X.; Gao, R. The Factor Structure and Rasch Analysis of the Fear of COVID-19 Scale (FCV-19S) Among Chinese Students. Front. Psychol. 2021, 12, 678979. [Google Scholar] [CrossRef]
- Tzur Bitan, D.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef]
- Moreta-Herrera, R.; Lopez-Calle, C.; Caycho-Rodriguez, T.; Cabezas Guerra, C.; Gallegos, M.; Cervigni, M.; Martino, P.; Bares, I.; Calandra, M. Is it possible to find a bifactor structure in the Fear of COVID-19 Scale (FCV-19S)? Psychometric evidence in an Ecuadorian sample. Death Stud. 2021. [Google Scholar] [CrossRef] [PubMed]
- Chi, X.; Chen, S.; Chen, Y.; Chen, D.; Yu, Q.; Guo, T.; Cao, Q.; Zheng, X.; Huang, S.; Hossain, M.M.; et al. Psychometric Evaluation of the Fear of COVID-19 Scale Among Chinese Population. Int. J. Ment. Health Addict. 2021, 20, 1273–1288. [Google Scholar] [CrossRef] [PubMed]
- Reznik, A.; Gritsenko, V.; Konstantinov, V.; Khamenka, N.; Isralowitz, R. COVID-19 Fear in Eastern Europe: Validation of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 19, 1903–1908. [Google Scholar] [CrossRef] [PubMed]
- Conti, A.; Clari, M.; Arese, S.; Bandini, B.; Cavallaro, L.; Mozzone, S.; Vellone, E.; Frigerio, S.; Campagna, S. Validation and psychometric evaluation of the Italian version of the Spinal Cord Injury Secondary Conditions Scale. Spinal Cord 2020, 58, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Alyami, M.; Henning, M.; Krgeloh, C.U. Psychometric Evaluation of the Arabic Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 19, 2219–2232. [Google Scholar] [CrossRef]
- Ransing, R.; Ramalho, R.; Orsolini, L.; Adiukwu, F.; Gonzalez-Diaz, J.M.; Larnaout, A.; Pinto da Costa, M.; Grandinetti, P.; Bytyci, D.G.; Shalbafan, M.; et al. Can COVID-19 related mental health issues be measured? Brain Behav. Immun. 2020, 88, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Pakpour, A.H.; Griffiths, M.D.; Chang, K.C.; Chen, Y.P.; Kuo, Y.J.; Lin, C.Y. Assessing the fear of COVID-19 among different populations: A response to Ransing et al. (2020). Brain Behav. Immun. 2020, 89, 524–525. [Google Scholar] [CrossRef]
- Pan, X.; Ojcius, D.M.; Gao, T. Lessons learned from the 2019-nCoV epidemic on prevention of future infectious diseases. Microbes Infect. 2020, 22, 86–91. [Google Scholar] [CrossRef]
- Deng, S.Q.; Peng, H.J. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J. Clin. Med. 2020, 9, 575. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatr. 2020, 33, 100213. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lv, S.; Liu, L.; Chen, R.; Chen, J.; Liang, S.; Tang, S.; Zhao, J. COVID-19 in Guangdong: Immediate Perceptions and Psychological Impact on 304, 167 College Students. Front. Psychol. 2020, 11, 2024. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Cheng, Z.; Yue, X.G.; McAleer, M. Risk Management of COVID-19 by Universities in China. J. Risk Financ. Manag. 2020, 13, 36. [Google Scholar] [CrossRef]
- Han, T.; Ma, W.; Gong, H.; Hu, Y.; Zhang, Y.; Zhang, C.; Yao, Z.; Fan, Y.; Zheng, Y.; Wang, C. Investigation and analysis of negative emotion among university students during home quarantine of COVID-19. J. Xi’an Jiaotong Univ. (Med. Sci.) 2020, 41, 1–11. [Google Scholar]
- Zhao, B.; Kong, F.; Aung, M.N.; Yuasa, M.; Nam, E.W. Novel Coronavirus (COVID-19) Knowledge, Precaution Practice, and Associated Depression Symptoms among University Students in Korea, China, and Japan. Environ. Res. Public Health 2020, 17, 6671. [Google Scholar] [CrossRef]
- Chang, J.; Yuan, Y.; Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 2020, 40, 171–176. [Google Scholar]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open. 2020, 3, e2025591. [Google Scholar] [CrossRef]
- The Chinese People’s Health Commission. A Notification on Intervention of Emergency Psychological Crisis during the Prevention and Control of New Coronavirus Pneumonia (in Chinese). Available online: http://www.gov.cn/xinwen/2020-01/27/content_5472433.htm (accessed on 27 January 2020).
- The Ministry of Education of the People’s Republic of China. A Notification on Several Matters Related to Teachers’ Affairs during the Prevention and Control of New Coronavirus Pneumonia. Available online: http://www.gov.cn:8080/zhengce/zhengceku/2020-02/14/content_5478554.htm (accessed on 2 February 2020).
- Price, B. A First Course in Factor Analysis. Technometrics 1993, 35, 453. [Google Scholar] [CrossRef]
- Kroenke, K.S.R.L.; Williams, J. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Kroenke, K.S.R.L.; Williams, J.; Janet, B.W. Lowe, Bernd. A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar]
- Pa, N.A.N.; Tapsir, R. Analysis of Instruments Measuring Values of Mathematics Education. Procedia-Soc. Behav. Sci. 2013, 90, 449–457. [Google Scholar] [CrossRef][Green Version]
- Santos, J. Cronbach’s Alpha: A Tool for Assessing the Reliability of Scales. J. Ext. 1999, 37, 1–5. [Google Scholar]
- Markus, K.A. Principles and Practice of Structural Equation Modeling by Rex B. Kline. Struct. Equ. Modeling: A Multidiscip. J. 2012, 19, 509–512. [Google Scholar] [CrossRef]
- Bagozzi, R. Evaluating structural equation models with unobservable variables and measurement error: A comment. J. Market. Res. 1981, 18, 375–381. [Google Scholar] [CrossRef]
- Drasgow, F.E. Fitting Polytomous Item Response Theory Models to Multiple-Choice Tests. Appl. Psychol. Meas. 1995, 19, 143–166. [Google Scholar] [CrossRef]
- McDonald, R.P.; Ho, M. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Tay, L.; Drasgow, F. Adjusting the Adjusted χ2/df Ratio Statistic for Dichotomous Item Response Theory Analyses. Educ. Psychol. Meas. 2011, 72, 510–528. [Google Scholar] [CrossRef]
- Khamis, H. Measures of Association: How to Choose? J. Diagn. Med. Sonogr. 2008, 24, 155–162. [Google Scholar] [CrossRef]
- Kaiser, H. A second-generation little jiffy. Psychometrika 1970, 35, 401–415. [Google Scholar] [CrossRef]
- Martínez-Lorca, M.; Martínez-Lorca, A.; Criado-Lvarez, J.J. The Fear of COVID-19 Scale: Validation in Spanish university students. Psychiatry Res. 2020, 293, 113350. [Google Scholar] [CrossRef] [PubMed]
- Masuyama, A.; Shinkawa, H.; Kubo, T. Validation and Psychometric Properties of the Japanese Version of the Fear of COVID-19 Scale Among Adolescents. Int. J. Ment. Health Addict. 2020, 20, 389–397. [Google Scholar] [CrossRef]
- Yang, Z.H.; Wang, B.; Ma, Q.; Wang, L.; Lin, Y.X.; Yan, H.F.; Fan, Z.X.; Chen, H.J.; Ge, Z.; Zhu, F.; et al. Potential Mechanisms of Action of Chinese Patent Medicines for COVID-19: A Review. Front. Pharmacol. 2021, 12, 668407. [Google Scholar] [CrossRef]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Alivernini, F.; Manganelli, S.; Girelli, L.; Cozzolino, M.; Lucidi, F.; Cavicchiolo, E. Physical Distancing Behavior: The Role of Emotions, Personality, Motivations, and Moral Decision-Making. J. Pediatric Psychol. 2021, 46, 15–26. [Google Scholar] [CrossRef]
- Cavicchiolo, E.; Manganelli, S.; Girelli, L.; Cozzolino, M.; Lucidi, F.; Alivernini, F. Adolescents at a distance: The importance of socio-cognitive factors in preventive behavior during the COVID-19 pandemic. Eur. J. Health Psychol. 2021, 28, 161–170. [Google Scholar] [CrossRef]
- Kolifarhood, G.; Aghaali, M.; Mozafar Saadati, H.; Taherpour, N.; Rahimi, S.; Izadi, N.; Hashemi Nazari, S.S. Epidemiological and clinical aspects of COVID-19: A narrative review. Arch. Acad. Emerg. Med. 2020, 8, e41. [Google Scholar]
- Wen, Z.; Kit-Tai, H.; Herber, W. Marsh. Structural equation model testing: Cutoff criteria for goodness of fit indices and chi-square test. Acta Psychol. Sin. 2004, 36, 186–194. [Google Scholar]
- Hu, L.T.; Bentler, P.M.; Hu, L.T.; Bentler, P.M. Fit Indices in Covariance Structure Modeling: Sensitivity to under Parameterized Model Misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Marsh, H.W.; Hau, K.T.; Wen, Z. In Search of Golden Rules: Comment on Hypothesis-Testing Approaches to Setting Cutoff Values for Fit Indexes and Dangers in Overgeneralizing Hu and Bentler’s (1999) Findings. Struct. Equ. Modeling Multidiscip. J. 2004, 11, 320–341. [Google Scholar] [CrossRef]
- Haktanir, A.; Seki, T.; Dilmac, B. Adaptation and evaluation of Turkish version of the fear of COVID-19 Scale. Death Stud. 2020, 46, 719–727. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± Standard Deviation or n (%) | |
|---|---|---|
| Age (years old) | 19 ± 1.29 | |
| 17–19 | 1075 (46.1) | |
| 20–22 | 1198 (51.3) | |
| 23–29 | 61 (2.6) | |
| University | ||
| key university | 965 (41.3) | |
| common university | 1369 (58.7) | |
| Gender | ||
| Male | 1275 (54.6) | |
| female | 1059 (45.4) | |
| PHQ-9 | 4.88 ± 4.82 | |
| Negative-depression | 1850 (79.3) | |
| Positive-depression | 484 (20.7) | |
| GAD-7 | 3.31 ± 3.98 | |
| Negative-anxiety | 2132 (91.3) | |
| Positive-anxiety | 202 (8.7) | |
| C-FV-19S | 16.04 ± 6.12 (8–50) |
| The C-FCV-19S Items | Mean (SD) | Skewness | Kurtosis | Correlation | p-Value |
|---|---|---|---|---|---|
| 1. I am most afraid of corona virus-19. | 3.02 (1.33) | −0.037 | −1.134 | 0.678 | <0.001 |
| 2. It makes me uncomfortable to think about coronavirus-19. | 2.61 (1.24) | 0.314 | −0.888 | 0.783 | <0.001 |
| 3. I worry a lot about coronavirus-19. | 2.30 (1.15) | 0.577 | −0.500 | 0.771 | <0.001 |
| 4. Coronavirus-19 is almost always terminal. | 1.61 (0.93) | 1.503 | 1.671 | 0.64 | <0.001 |
| 5. Coronavirus-19 is an unpredictable disease. | 2.36 (1.28) | 0.551 | −0.786 | 0.636 | <0.001 |
| 6. My hands become clammy when I think about coronavirus-19. | 1.60 (0.936) | 1.646 | 2.274 | 0.772 | <0.001 |
| 7. I am afraid of losing my life because of coronavirus-19. | 2.15 (1.30) | 0.858 | −0.424 | 0.747 | <0.001 |
| 8. When watching news and stories about coronavirus-19 on social media, I become nervous or anxious. | 2.28 (1.18) | 0.562 | −0.680 | 0.765 | <0.001 |
| 9. I cannot sleep because I’m worrying about getting coronavirus-19. | 1.46 (0.83) | 1.895 | 3.225 | 0.715 | <0.001 |
| 10. My heart races or palpitates when I think about getting coronavirus-19. | 1.60 (0.97) | 1.660 | 2.116 | 0.741 | <0.001 |
| Items | Factor 1 | Factor 2 |
|---|---|---|
| Q9. I cannot sleep because I’m worrying about getting coronavirus-19. | 0.893 | 0.209 |
| Q10. My heart races or palpitates when I think about getting coronavirus-19. | 0.861 | 0.255 |
| Q6. My hands become clammy when I think about coronavirus-19. | 0.851 | 0.314 |
| Q 4. Coronavirus-19 is almost always terminal. | 0.82 | 0.169 |
| Q5. Coronavirus-19 is an unpredictable disease. | 0.584 | 0.402 |
| Q7. I am afraid of losing my life because of coronavirus-19. | 0.575 | 0.544 |
| Q8. When watching news and stories about coronavirus-19 on social media, I become nervous or anxious. | 0.571 | 0.578 |
| Q1. I am most afraid of corona virus-19. | 0.076 | 0.904 |
| Q2. It makes me uncomfortable to think about coronavirus-19. | 0.288 | 0.869 |
| Q3. I worry a lot about coronavirus-19. | 0.452 | 0.698 |
| Eigen values | 6.05 | 1.263 |
| Variance contribution rate | 60.5 | 12.63 |
| Cumulative variance contribution rate (%) | 60.5 | 73.14 |
| χ2 (df.) | χ2/df | RMSEA | SRMR | GFI | CFI | TLI | NFI | RFI | IFI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Threshold value | ≤5.0 | ≤0.08 | ≤0.08 | >0.09 | >0.09 | >0.09 | >0.09 | >0.09 | >0.09 | |
| Model 1 | 1239.172 (20) *** | 61.95 | 0.229 | 0.1002 | 0.754 | 0.747 | 0.646 | 0.744 | 0.642 | 0.748 |
| Model 2 | 450.63 (19) *** | 23.68 | 0.14 | 0.0774 | 0.907 | 0.936 | 0.906 | 0.934 | 0.902 | 0.936 |
| Model 3 | 68.055 (11) *** | 6.18 | 0.067 | 0.028 | 0.986 | 0.988 | 0.970 | 0.986 | 0.964 | 0.988 |
| Without Fear COVID-19 | With-Fear COVID-19 | F/χ2 | p-Value | ||
|---|---|---|---|---|---|
| n = 1518 | n = 682 | ||||
| Anxiety | 2.51 ± 3.38 | 4.80 ± 4.56 | 189.562 | <0.001 | |
| without | 1450 (68) | 682 (32) | 95.737 | <0.001 | |
| with | 68 (33.7) | 134 (66.3) | |||
| Depression | 3.98 ± 4.17 | 6.56 ± 5.45 | 163.798 | <0.001 | |
| without | 1318 (71.2) | 532 (28.8) | 151.045 | <0.001 | |
| with | 200 (41.3) | 284 (58.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, W.; Li, P.; Huang, Y.; Yang, X.; Mu, W.; Jing, W.; Ma, X.; Zhang, X. Cross-Cultural Adaptation and Validation of the Fear of COVID-19 Scale for Chinese University Students: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 8624. https://doi.org/10.3390/ijerph19148624
Yang W, Li P, Huang Y, Yang X, Mu W, Jing W, Ma X, Zhang X. Cross-Cultural Adaptation and Validation of the Fear of COVID-19 Scale for Chinese University Students: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(14):8624. https://doi.org/10.3390/ijerph19148624
Chicago/Turabian StyleYang, Wanqiu, Peng Li, Yubo Huang, Xiao Yang, Wei Mu, Wangwei Jing, Xiaohong Ma, and Xiangyang Zhang. 2022. "Cross-Cultural Adaptation and Validation of the Fear of COVID-19 Scale for Chinese University Students: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 14: 8624. https://doi.org/10.3390/ijerph19148624
APA StyleYang, W., Li, P., Huang, Y., Yang, X., Mu, W., Jing, W., Ma, X., & Zhang, X. (2022). Cross-Cultural Adaptation and Validation of the Fear of COVID-19 Scale for Chinese University Students: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(14), 8624. https://doi.org/10.3390/ijerph19148624






