The Prevalence and Development of Neck and Lower Back Pain and Associated Factors in Dentistry Students—A Long-Term Prospective Study
Abstract
:1. Introduction
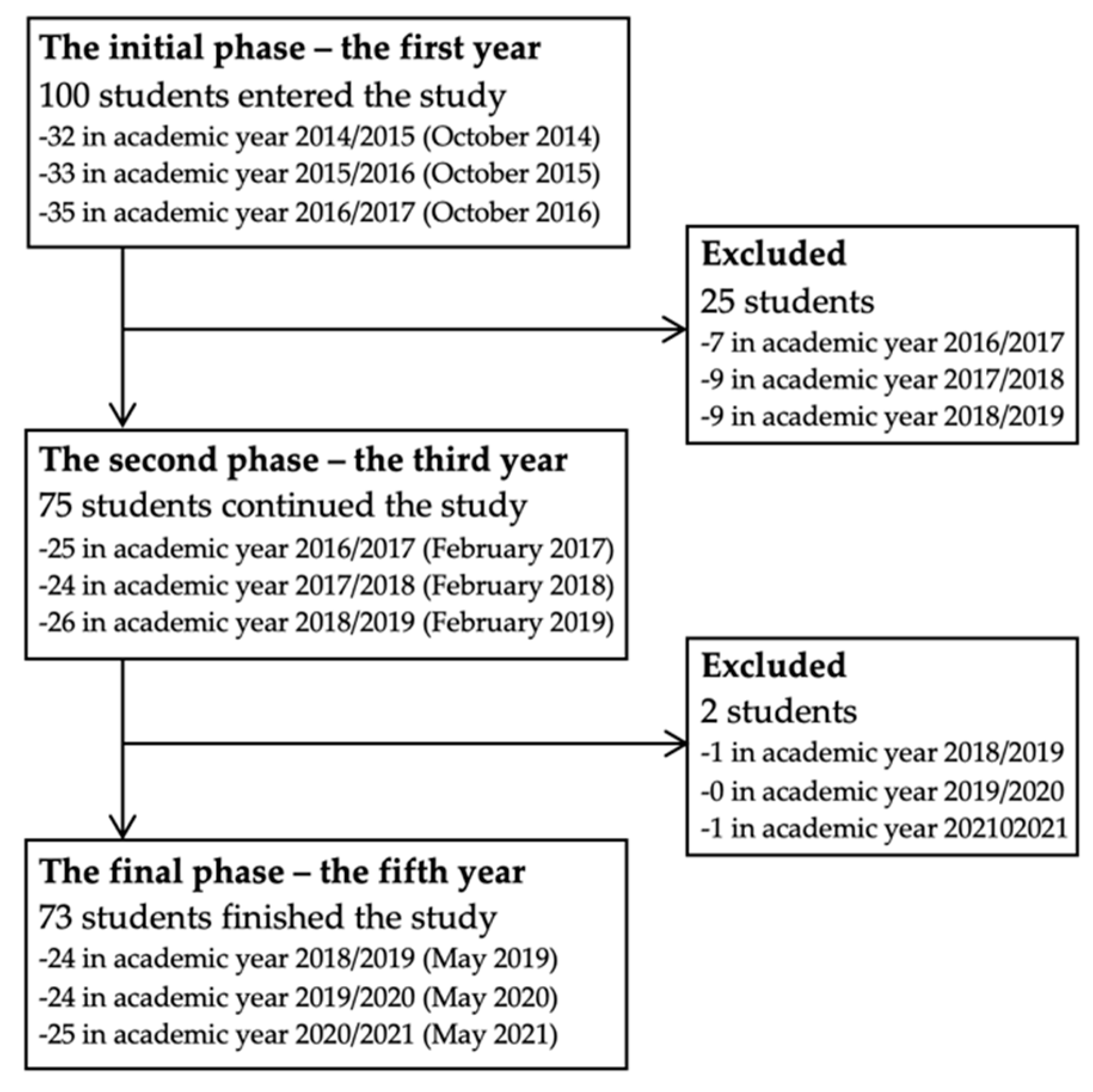
2. Materials and Methods
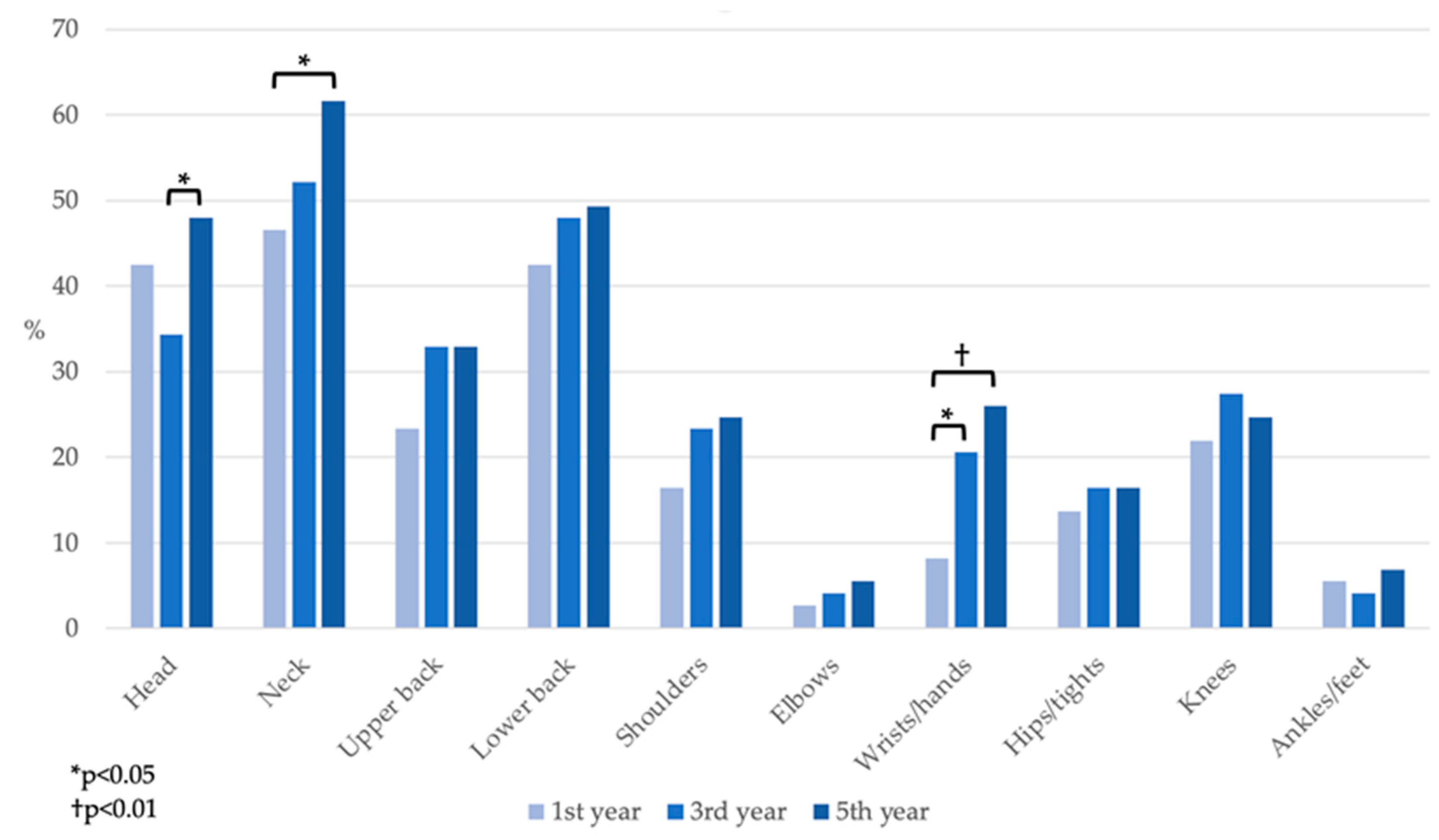
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Myers, H.L.; Myers, L.B. ‘It’s difficult being a dentist’: Stress and health in the general dental practitioner. Br. Dent. J. 2004, 197, 89–93, discussion 83; quiz 100–101. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Risi, A.; Prati, C. Musculoskeletal Disorders among Italian Dentists and Dental Hygienists. Int. J. Environ. Res. Public Health 2021, 18, 2705. [Google Scholar] [CrossRef] [PubMed]
- Aboalshamat, K.T. Nordic Assessment of Occupational Disorders among Dental Students and Dentists in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2020, 10, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Lietz, J.; Ulusoy, N.; Nienhaus, A. Prevention of Musculoskeletal Diseases and Pain among Dental Professionals through Ergonomic Interventions: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 3482. [Google Scholar] [CrossRef]
- Hayes, M.; Cockrell, D.; Smith, D.R. A systematic review of musculoskeletal disorders among dental professionals. Int. J. Dent. Hyg. 2009, 7, 159–165. [Google Scholar] [CrossRef]
- Hodacova, L.; Sustova, Z.; Cermakova, E.; Kapitan, M.; Smejkalova, J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind. Health 2015, 53, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Puriene, A.; Janulyte, V.; Musteikyte, M.; Bendinskaite, R. General health of dentists. Literature review. Stomatologija 2007, 9, 10–20. [Google Scholar]
- Czech Social Security Administration. Nemocenská Statistika. Sick-Leave Statistics. Available online: https://www.cssz.cz/web/cz/nemocenska-statistika#section_3 (accessed on 11 December 2021).
- Czech Statistical Office. Pracovní Neschopnost pro Nemoc a Úraz v České Republice. Available online: https://www.czso.cz/documents/10180/90577089/26000419p1.pdf/31ab8266-a4b3-4f8f-a5e5-edfc9cb4edd0?version=1.1 (accessed on 11 December 2021).
- Alzahem, A.M.; van der Molen, H.T.; Alaujan, A.H.; Schmidt, H.G.; Zamakhshary, M.H. Stress amongst dental students: A systematic review. Eur. J. Dent. Educ. 2011, 15, 8–18. [Google Scholar] [CrossRef]
- Nowak, J.; Erbe, C.; Hauck, I.; Groneberg, D.A.; Hermanns, I.; Ellegast, R.; Ditchen, D.; Ohlendorf, D. Motion analysis in the field of dentistry: A kinematic comparison of dentists and orthodontists. BMJ Open 2016, 6, e011559. [Google Scholar] [CrossRef] [Green Version]
- Ohlendorf, D.; Erbe, C.; Hauck, I.; Nowak, J.; Hermanns, I.; Ditchen, D.; Ellegast, R.; Groneberg, D.A. Kinematic analysis of work-related musculoskeletal loading of trunk among dentists in Germany. BMC Musculoskelet. Disord. 2016, 17, 427. [Google Scholar] [CrossRef] [Green Version]
- Ohlendorf, D.; Erbe, C.; Nowak, J.; Hauck, I.; Hermanns, I.; Ditchen, D.; Ellegast, R.; Groneberg, D.A. Constrained posture in dentistry—A kinematic analysis of dentists. BMC Musculoskelet. Disord. 2017, 18, 291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puriene, A.; Aleksejuniene, J.; Petrauskiene, J.; Balciuniene, I.; Janulyte, V. Self-reported occupational health issues among Lithuanian dentists. Ind. Health 2008, 46, 369–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sustová, Z.; Hodacová, L.; Kapitán, M. The prevalence of musculoskeletal disorders among dentists in the Czech Republic. Acta Med. (Hradec Kralove) 2013, 56, 150–156. [Google Scholar] [CrossRef] [Green Version]
- Valachi, B.; Valachi, K. Mechanisms leading to musculoskeletal disorders in dentistry. J. Am. Dent. Assoc. 2003, 134, 1344–1350. [Google Scholar] [CrossRef] [PubMed]
- Valachi, B.; Valachi, K. Preventing musculoskeletal disorders in clinical dentistry: Strategies to address the mechanisms leading to musculoskeletal disorders. J. Am. Dent. Assoc. 2003, 134, 1604–1612. [Google Scholar] [CrossRef] [Green Version]
- Vodanović, M.; Sović, S.; Galić, I. Occupational health problems among dentists in Croatia [Profesionalni zdravstveni problemi medu stomatolozima u Hrvatskoj]. Acta Stomatol. Croat. 2016, 50, 310–320. [Google Scholar] [CrossRef]
- Serota, K.S.; Andó, B.; Nagy, K.; Kovács, I. Revealing Distress and Perceived Stress among Dentists at the Outset of the COVID-19 Pandemic: A Cross-Sectional Factor Analytic Study. Int. J. Environ. Res. Public Health 2021, 18, 11813. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef]
- Valachi, B. Musculoskeletal health of the woman dentist: Distinctive interventions for a growing population. J. Calif. Dent. Assoc. 2008, 36, 127–132. [Google Scholar]
- Rising, D.W.; Bennett, B.C.; Hursh, K.; Plesh, O. Reports of body pain in a dental student population. J. Am. Dent. Assoc. 2005, 136, 81–86. [Google Scholar] [CrossRef]
- Thornton, L.J.; Barr, A.E.; Stuart-Buttle, C.; Gaughan, J.P.; Wilson, E.R.; Jackson, A.D.; Wyszynski, T.C.; Smarkola, C. Perceived musculoskeletal symptoms among dental students in the clinic work environment. Ergonomics 2008, 51, 573–586. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, M.V.; Soriano, E.P.; de França Caldas, A., Jr.; Campello, R.I.; de Miranda, H.F.; Cavalcanti, F.I. Work-related musculoskeletal disorders among Brazilian dental students. J. Dent. Educ. 2009, 73, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Caballero, A.J.; Gómez-Palencia, I.P.; Díaz-Cárdenas, S. Ergonomic factors that cause the presence of pain muscle in students of dentistry. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e906–e911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haas, Y.; Naser, A.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; Nienhaus, A.; et al. Prevalence of self-reported musculoskeletal disorders of the hand and associated conducted therapy approaches among dentists and dental assistants in Germany. PLoS ONE 2020, 15, e0241564. [Google Scholar] [CrossRef]
- Khan, S.A.; Chew, K.Y. Effect of working characteristics and taught ergonomics on the prevalence of musculoskeletal disorders amongst dental students. BMC Musculoskelet. Disord. 2013, 14, 118. [Google Scholar] [CrossRef] [Green Version]
- Ng, A.; Hayes, M.J.; Polster, A. Musculoskeletal Disorders and Working Posture among Dental and Oral Health Students. Healthcare 2016, 4, 13. [Google Scholar] [CrossRef] [Green Version]
- Rafie, F.; Zamani Jam, A.; Shahravan, A.; Raoof, M.; Eskandarizadeh, A. Prevalence of Upper Extremity Musculoskeletal Disorders in Dentists: Symptoms and Risk Factors. J. Environ. Public Health 2015, 2015, 517346. [Google Scholar] [CrossRef]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [Green Version]
- Morse, T.; Bruneau, H.; Dussetschleger, J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 2010, 35, 419–429. [Google Scholar] [CrossRef]
- Yi, J.; Hu, X.; Yan, B.; Zheng, W.; Li, Y.; Zhao, Z. High and specialty-related musculoskeletal disorders afflict dental professionals even since early training years. J. Appl. Oral Sci. 2013, 21, 376–382. [Google Scholar] [CrossRef]
- Harutunian, K.; Gargallo-Albiol, J.; Figueiredo, R.; Gay-Escoda, C. Ergonomics and musculoskeletal pain among postgraduate students and faculty members of the School of Dentistry of the University of Barcelona (Spain). A cross-sectional study. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e425–e429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapitán, M.; Hodačová, L.; Čermáková, E.; Machač, S.; Schmidt, J.; Pilbauerová, N. The Development of Musculoskeletal Disorders during Undergraduate Dentistry Studies-A Long-Term Prospective Study. Int. J. Environ. Res. Public Health 2021, 18, 7662. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Cross, M.J.; Hoy, D.G.; Sànchez-Riera, L.; Blyth, F.M.; Woolf, A.D.; March, L. Musculoskeletal Health Conditions Represent a Global Threat to Healthy Aging: A Report for the 2015 World Health Organization World Report on Ageing and Health. Gerontologist 2016, 56 (Suppl. S2), S243–S255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organisation. Protecting Workers’ Health. Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/protecting-workers’-health (accessed on 6 December 2021).
- Ísper Garbin, A.J.; Barreto Soares, G.; Moreira Arcieri, R.; Adas Saliba Garbin, C.; Siqueira, C.E. Musculoskeletal disorders and perception of working conditions: A survey of Brazilian dentists in São Paulo. Int. J. Occup. Med. Environ. Health 2017, 30, 367–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, R.L.; Carvalho, N.; Albuquerque, C.; Andrade, A.; Martins, C.; Campos, S.; Batista, S.; Dinis, A.I. Musculoskeletal disorders in adolescents: A study on prevalence and determining factors. Acta Paul. Enferm. 2020, 33, 1–8. [Google Scholar] [CrossRef] [Green Version]
| 1st Year | 3rd Year | 5th Year | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Mild | Moderate | Severe | No | Mild | Moderate | Severe | No | Mild | Moderate | Severe | |
| % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | |
| Head | 57.5 (42) | 28.8 (21) | 13.7 (10) | 0 (0) | 65.8 (48) | 26.0 (19) | 8.2 (6) | 0 (0) | 52.1 (38) | 34.2 (25) | 11.0 (8) | 2.7 (2) |
| Neck | 53.4 (39) | 32.9 (24) | 13.7 (10) | 0 (0) | 47.9 (35) | 41.1 (30) | 11.0 (8) | 0 (0) | 38.4 (28) | 41.1 (30) | 20.5 (15) | 0 (0) |
| Upper back | 76.7 (56) | 17.8 (13) | 5.5 (4) | 0 (0) | 67.1 (49) | 24.7 (18) | 8.2 (6) | 0 (0) | 67.1 (49) | 24.7 (18) | 6.8 (5) | 1.4 (1) |
| Lower back | 57.5 (42) | 38.4 (28) | 4.1 (3) | 0 (0) | 52.1 (38) | 39.7 (29) | 8.2 (6) | 0 (0) | 50.7 (37) | 38.4 (28) | 9.6 (7) | 1.4 (1) |
| Shoulders | 83.6 (61) | 12.3 (9) | 2.7 (2) | 1.4 (1) | 76.7 (56) | 16.4 (12) | 6.8 (5) | 0 (0) | 75.3 (55) | 20.5 (15) | 2.7 (2) | 1.4 (1) |
| Elbows | 97.3 (71) | 2.7 (2) | 0 (0) | 0 (0) | 95.9 (70) | 2.7 (2) | 1.4 (1) | 0 (0) | 94.5 (69) | 4.1 (3) | 1.4 (1) | 0 (0) |
| Wrists/hands | 91.8 (67) | 5.5 (4) | 1.4 (1) | 1.4 (1) | 79.5 (58) | 16.4 (12) | 4.1 (3) | 0 (0) | 74.0 (54) | 23.3 (17) | 1.4 (1) | 1.4 (1) |
| Hips/tights | 86.3 (63) | 11.0 (8) | 2.7 (2) | 0 (0) | 83.6 (61) | 12.3 (9) | 4.1 (3) | 0 (0) | 83.6 (61) | 12.3 (9) | 0 (0) | 4.1 (3) |
| Knees | 78.1 (57) | 15.1 (11) | 4.1 (3) | 2.7 (2) | 72.6 (53) | 23.3 (17) | 4.1 (3) | 0 (0) | 75.3 (55) | 19.2 (14) | 4.1 (3) | 1.4 (1) |
| Ankles/feet | 94.5 (69) | 4.1 (3) | 1.4 (1) | 0 (0) | 95.9 (70) | 2.7 (2) | 1.4 (1) | 0 (0) | 93.2 (68) | 5.5 (4) | 1.4 (1) | 0 (0) |
| 1st Year | 3rd Year | 5th Year | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Gender (men) | 1.12 (0.38, 3.27) | 0.83 | 2.03 (0.68, 6.02) | 0.2 | 2.57 (0.87, 7.62) | 0.087 |
| Age | 1.18 (0.76, 1.83) | 0.45 | 1.15 (0.77, 1.71) | 0.49 | 1.20 (0.77, 1.87) | 0.4 |
| Height | 1.00 (0.95, 1.06) | 0.98 | 0.97 (0.93, 1.04) | 0.63 | 0.98 (0.93, 1.04) | 0.53 |
| Height—men | 1.05 (0.93, 1.19) | 0.39 | 1.04 (0.92, 1.17) | 0.54 | 1.04 (0.93, 1.17) | 0.46 |
| Height—women | 0.98 (0.90, 1.08) | 0.69 | 1.00 (0.92, 1.10) | 0.92 | 1.01 (0.92, 1.11) | 0.86 |
| Actual weight—men | 1.04 (0.96, 1.12) | 0.35 | 1.04 (0.96, 1.12) | 0.34 | 1.04 (0.97, 1.13) | 0.25 |
| Actual weight—women | 1.00 (0.92, 1.09) | 0.94 | 1.02 (0.94, 1.10) | 0.61 | 1.02 (0.94, 1.10) | 0.71 |
| Weight increase | 0.71 (0.25, 2.04) | 0.73 | 1.14 (0.41, 3.19) | 0.94 | ||
| Weight decrease | 1.20 (0.32, 4.44) | 0.85 (0.17, 4.33) | ||||
| General disease | 1.64 (0.44, 6.18) | 0.46 | 0.57 (0.15, 2.15) | 0.4 | 1.85 (0.60, 5.67) | 0.28 |
| Chronic medication | 1.61 (0.55, 4.71) | 0.38 | 1.05 (0.35, 3.11) | 0.93 | 0.38 (0.11, 1.33) | 0.12 |
| Dominant hand (right) | 0.63 (0.13, 3.01) | 0.56 | 1.09 (0.21, 5.81) | 0.92 | 1.68 (0.31, 8.97) | 0.55 |
| Diseases of musculoskeletal system in blood relatives | 0.92 (0.37, 2.32) | 0.86 | 1.12 (0.43, 2.92) | 0.82 | 0.81 (0.31, 2.12) | 0.67 |
| Past disease or trauma of musculoskeletal system | 1.60 (0.33, 7.72) | 0.56 | 0.90 (0.28, 2.90) | 0.86 | 1.30 (0.35, 4.79) | 0.69 |
| Top-level sport | 2.29 (0.73, 7.17) | 0.15 | 5.89 (1.19, 29.17) | 0.013 | 9.82 (1.20, 80.37) | 0.0059 |
| Regular sporting activities | 2.28 (0.70, 7.40) | 0.16 | 1.10 (0.29, 4.18) | 0.89 | 0.19 (0.04, 0.92) | 0.018 |
| Awareness of MSDs among dentists | 1.17 (0.46, 2.93) | 0.74 | 1.48 (0.59, 3.73) | 0.4 | 0.88 (0.34, 2.25) | 0.78 |
| Considering the range of ergonomic education as sufficient | 1.11 (0.35, 3.55) | 0.86 | 0.67 (0.21, 2.19) | 0.5 | ||
| 1st Year | 3rd Year | 5th Year | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Gender (men) | 1.67 (0.55, 5.08) | 0.36 | 1.21 (0.41, 3.51) | 0.73 | 0.96 (0.33, 2.80) | 0.95 |
| Age | 1.02 (0.67, 1.55) | 0.92 | 1.37 (0.87, 2.16) | 0.14 | 2.29 (1.23, 4.29) | 0.0021 |
| Height | 0.97 (0.92, 1.02) | 0.26 | 0.96 (0.90, 1.01) | 0.13 | 1.00 (0.95, 1.05) | 0.97 |
| Height—men | 1.08 (0.94, 1.24) | 0.23 | 0.98 (0.87, 1.09) | 0.67 | 1.09 (0.96, 1.24) | 0.16 |
| Height—women | 0.92 (0.83, 1.01) | 0.074 | 0.92 (0.83, 1.01) | 0.068 | 0.95 (0.86, 1.06) | 0.22 |
| Actual weight—men | 1.09 (0.99, 1.20) | 0.047 | 0.99 (0.92, 1.06) | 0.8 | 1.01 (0.95, 1.09) | 0.7 |
| Actual weight—women | 0.98 (0.90, 1.06) | 0.6 | 0.95 (0.88, 1.03) | 0.2 | 0.92 (0.85, 1.00) | 0.045 |
| Weight increase | 0.60 (0.21, 1.76) | 0.23 | 0.68 (0.25, 1.84) | 0.7 | ||
| Weight decrease | 2.11 (0.54, 8.16) | 0.65 (0.13, 3.27) | ||||
| General disease | 1.35 (0.36, 5.09) | 0.65 | 0.73 (0.20, 2.65) | 0.63 | 0.70 (0.23, 2.14) | 0.53 |
| Chronic medication | 1.50 (0.51, 4.37) | 0.46 | 0.95 (0.32, 2.83) | 0.93 | 1.54 (0.44, 5.41) | 0.49 |
| Dominant hand (right) | 0.98 (0.20, 4.74) | 0.98 | 0.43 (0.07, 2.51) | 0.33 | 2.06 (0.35, 12.02) | 0.41 |
| Diseases of musculoskeletal system in blood relatives | 0.63 (0.25, 1.62) | 0.34 | 0.33 (0.12, 0.91) | 0.027 | 1.86 (0.72, 4.82) | 0.2 |
| Past disease or trauma of musculoskeletal system | 1.93 (0.40, 9.31) | 0.41 | 1.11 (0.35, 3.55) | 0.86 | 1.54 (0.44, 5.41) | 0.49 |
| Top-level sport | 4.07 (1.24, 13.36) | 0.016 | 0.48 (0.13, 1.78) | 0.26 | 1.83 (0.54, 6.24) | 0.33 |
| Regular sporting activities | 1.30 (0.42, 4.07) | 0.65 | 0.91 (0.24, 3.45) | 0.89 | 1.14 (0.37, 3.56) | 0.82 |
| Awareness of MSDs among dentists | 0.66 (0.26, 1.67) | 0.38 | 0.90 (0.30, 2.73) | 0.85 | 1.33 (0.44, 4.05) | 0.61 |
| Considering the range of ergonomic education as sufficient | 0.90 (0.28, 2.90) | 0.86 | 0.97 (0.32, 2.93) | 0.95 | ||
| 1st Year | 3rd Year | 5th Year | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Gender (men) | 1.33 (0.24, 7.27) | 0.74 | 2.74 (0.41, 18.14) | 0.28 | 6.98 (0.65, 74.40) | 0.08 |
| Age | 1.09 (0.66, 1.78) | 0.74 | 1.06 (0.65, 1.73) | 0.81 | 1.15 (0.68, 1.94) | 0.59 |
| Height | 0.99 (0.88, 1.10) | 0.81 | 0.92 (0.82, 1.04) | 0.18 | 0.95 (0.85, 1.08) | 0.45 |
| Actual weight | 1.01 (0.93, 1.10) | 0.75 | 1.08 (0.99, 1.18) | 0.073 | 1.07 (0.96, 1.19) | 0.21 |
| Weight increase | 0.58 (0.15, 2.18) | 0.67 | 1.71 (0.43, 6.74) | 0.73 | ||
| Weight decrease | 1.17 (0.26, 5.29) | 0.92 (0.10, 8.81) | ||||
| General disease | 3.26 (0.59, 18.06) | 0.16 | 0.26 (0.03, 2.08) | 0.19 | 1.23 (0.13, 11.62) | 0.86 |
| Chronic medication | 2.75 (0.64, 11.91) | 0.17 | 0.38 (0.07. 2.10) | 0.26 | 0.39 (0.03, 4.34) | 0.44 |
| Dominant hand (right) | 0.53 (0.08, 3.58) | 0.51 | 1.83 (0.20, 16.59) | 0.59 | 4.23 (0.30, 60.22) | 0.27 |
| Diseases of musculoskeletal system in blood relatives | 1.10 (0.38, 3.20) | 0.86 | 1.00 (0.30, 3.33) | 0.99 | 0.82 (0.24, 2.81) | 0.76 |
| Past disease or trauma of musculoskeletal system | 1.23 (0.20, 7.66) | 0.82 | 0.85 (0.20, 3.60) | 0.82 | 0.85 (0.12, 6.11) | 0.87 |
| Top-level sport | 2.44 (0.64, 9.33) | 0.19 | 11.93 (1.89, 75.26) | 0.0026 | 21.47 (1.84, 250.92) | 0.002 |
| Regular sporting activities | 2.75 (0.70, 10.85) | 0.14 | 0.85 (0.15, 4.84) | 0.85 | 0.14 (0.02, 0.89) | 0.018 |
| Awareness of MSDs among dentists | 0.99 (0.32, 3.06) | 0.99 | 1.72 (0.53, 5.66) | 0.37 | 1.12 (0.30, 4.13) | 0.87 |
| Considering the range of ergonomic education as sufficient | 1.50 (0.39, 5.84) | 0.56 | 0.81 (0.14, 4.67) | 0.81 | ||
| Whole model | 0.74 | 0.47 | 0.04996 | |||
| 1st Year | 3rd Year | 5th Year | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Gender (men) | 3.42 (0.40, 29.49) | 0.24 | 0.66 (0.10, 4.50) | 0.67 | 0.25 (0.04, 1.67) | 0.14 |
| Age | 0.87 (0.51, 1.46) | 0.59 | 1.45 (0.79, 2.67) | 0.19 | 2.16 (1.00, 4.65) | 0.015 |
| Height | 0.84 (0.73, 0.96) | 0.0068 | 0.95 (0.84, 1.07) | 0.38 | 1.03 (0.91, 1.17) | 0.64 |
| Actual weight | 1.13 (1.02, 1.25) | 0.0098 | 1.00 (0.91, 1.10) | 0.98 | 0.94 (0.85, 1.03) | 0.17 |
| Weight increase | 0.52 (0.13, 2.07) | 0.2 | 0.66 (0.18, 2.47) | 0.43 | ||
| Weight decrease | 2.84 (0.58, 13.94) | 0.27 (0.03, 2.29) | ||||
| General disease | 1.34 (0.23, 7.93) | 0.75 | 0.36 (0.05, 2.86) | 0.33 | 1.13 (0.14, 9.22) | 0.91 |
| Chronic medication | 1.39 (0.30, 6.35) | 0.67 | 0.31 (0.05, 1.81) | 0.18 | 1.14 (0.11, 12.04) | 0.92 |
| Dominant hand (right) | 0.78 (0.10, 6.17) | 0.81 | 0.18 (0.02, 1.95) | 0.14 | 4.70 (0.36, 61.79) | 0.22 |
| Diseases of musculoskeletal system in blood relatives | 0.53 (0.16, 1.69) | 0.28 | 0.29 (0.08, 0.96) | 0.037 | 1.97 (0.59, 6.60) | 0.27 |
| Past disease or trauma of musculoskeletal system | 1.07 (0.13, 8.62) | 0.95 | 1.12 (0.27, 4.61) | 0.88 | 1.46 (0.29, 7.33) | 0.65 |
| Top-level sport | 9.36 (1.88, 46.63) | 0.003 | 0.56 (0.11, 2.94) | 0.48 | 2.67 (0.51, 14.04) | 0.24 |
| Regular sporting activities | 1.06 (0.25, 4.47) | 0.93 | 2.22 (0.39, 12.75) | 0.37 | 0.76 (0.16, 3.52) | 0.72 |
| Awareness of MSDs among dentists | 0.72 (0.21, 2.51) | 0.6 | 1.29 (0.40, 4.16) | 0.68 | 3.91 (1.10, 13.88) | 0.028 |
| Considering the range of ergonomic education as sufficient | 0.62 (0.16, 2.42) | 0.49 | 0.85 (0.20, 3.56) | 0.83 | ||
| Whole model | 0.071 | 0.29 | 0.15 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hodačová, L.; Pilbauerová, N.; Čermáková, E.; Machač, S.; Schmidt, J.; Hodač, J.; Kapitán, M. The Prevalence and Development of Neck and Lower Back Pain and Associated Factors in Dentistry Students—A Long-Term Prospective Study. Int. J. Environ. Res. Public Health 2022, 19, 8539. https://doi.org/10.3390/ijerph19148539
Hodačová L, Pilbauerová N, Čermáková E, Machač S, Schmidt J, Hodač J, Kapitán M. The Prevalence and Development of Neck and Lower Back Pain and Associated Factors in Dentistry Students—A Long-Term Prospective Study. International Journal of Environmental Research and Public Health. 2022; 19(14):8539. https://doi.org/10.3390/ijerph19148539
Chicago/Turabian StyleHodačová, Lenka, Nela Pilbauerová, Eva Čermáková, Stanislav Machač, Jan Schmidt, Jan Hodač, and Martin Kapitán. 2022. "The Prevalence and Development of Neck and Lower Back Pain and Associated Factors in Dentistry Students—A Long-Term Prospective Study" International Journal of Environmental Research and Public Health 19, no. 14: 8539. https://doi.org/10.3390/ijerph19148539
APA StyleHodačová, L., Pilbauerová, N., Čermáková, E., Machač, S., Schmidt, J., Hodač, J., & Kapitán, M. (2022). The Prevalence and Development of Neck and Lower Back Pain and Associated Factors in Dentistry Students—A Long-Term Prospective Study. International Journal of Environmental Research and Public Health, 19(14), 8539. https://doi.org/10.3390/ijerph19148539










