Effects of the COVID-19 Restrictions on Eating Behaviour and Eating Disorder Symptomology in Female Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
- Clinical sample
- 19 patients with AN;
- 20 patients with depression.
- Online sample
- 45 adolescents with a self-reported psychiatric disorder (SRPD);
- 138 typically developing control participants.
2.2. Survey Procedures and Questions
2.3. Data Analysis and Statistics
3. Results
3.1. Participant Characteristics
3.2. Quality of Life
3.3. Changes of CIES Factors
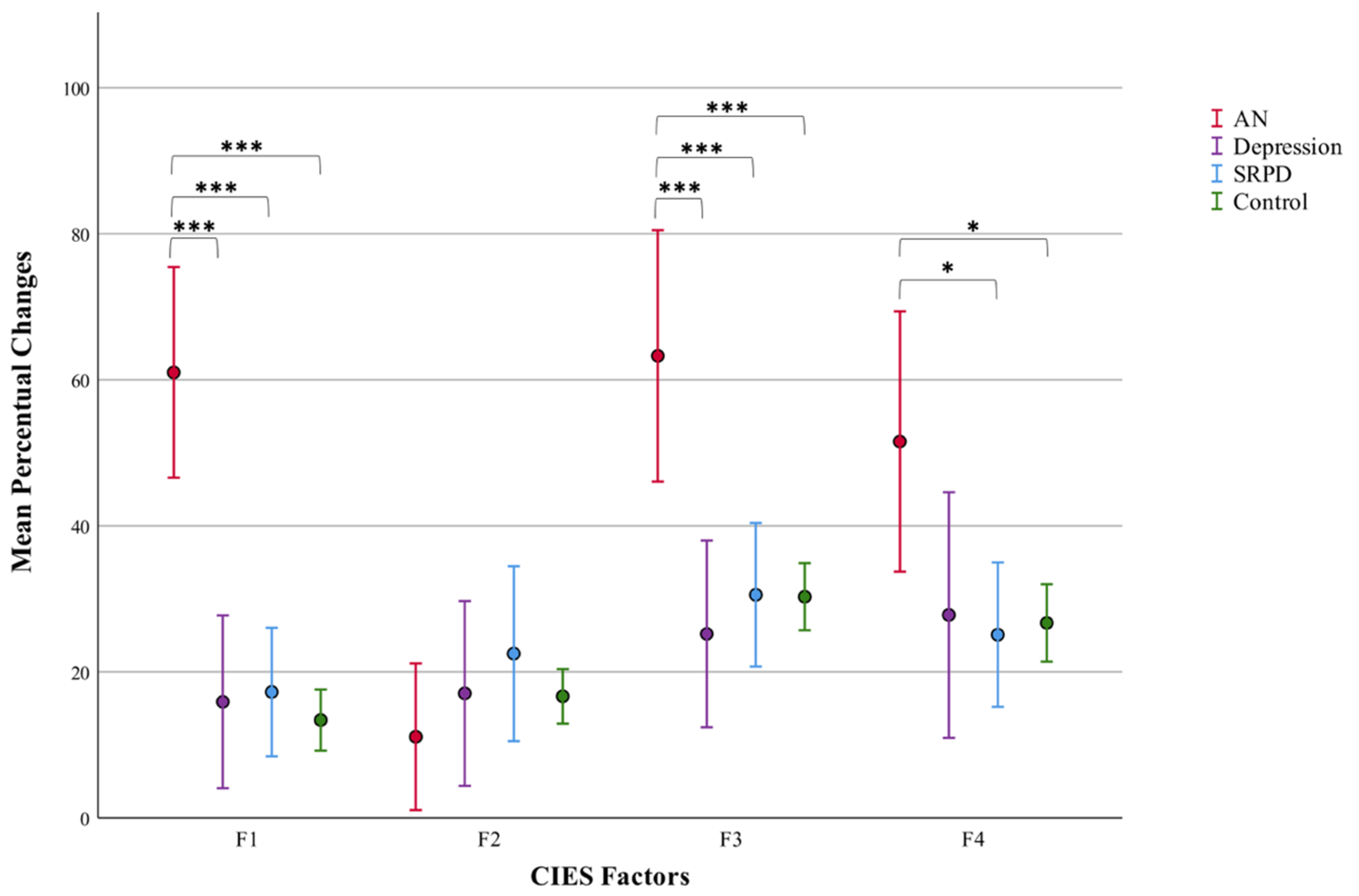
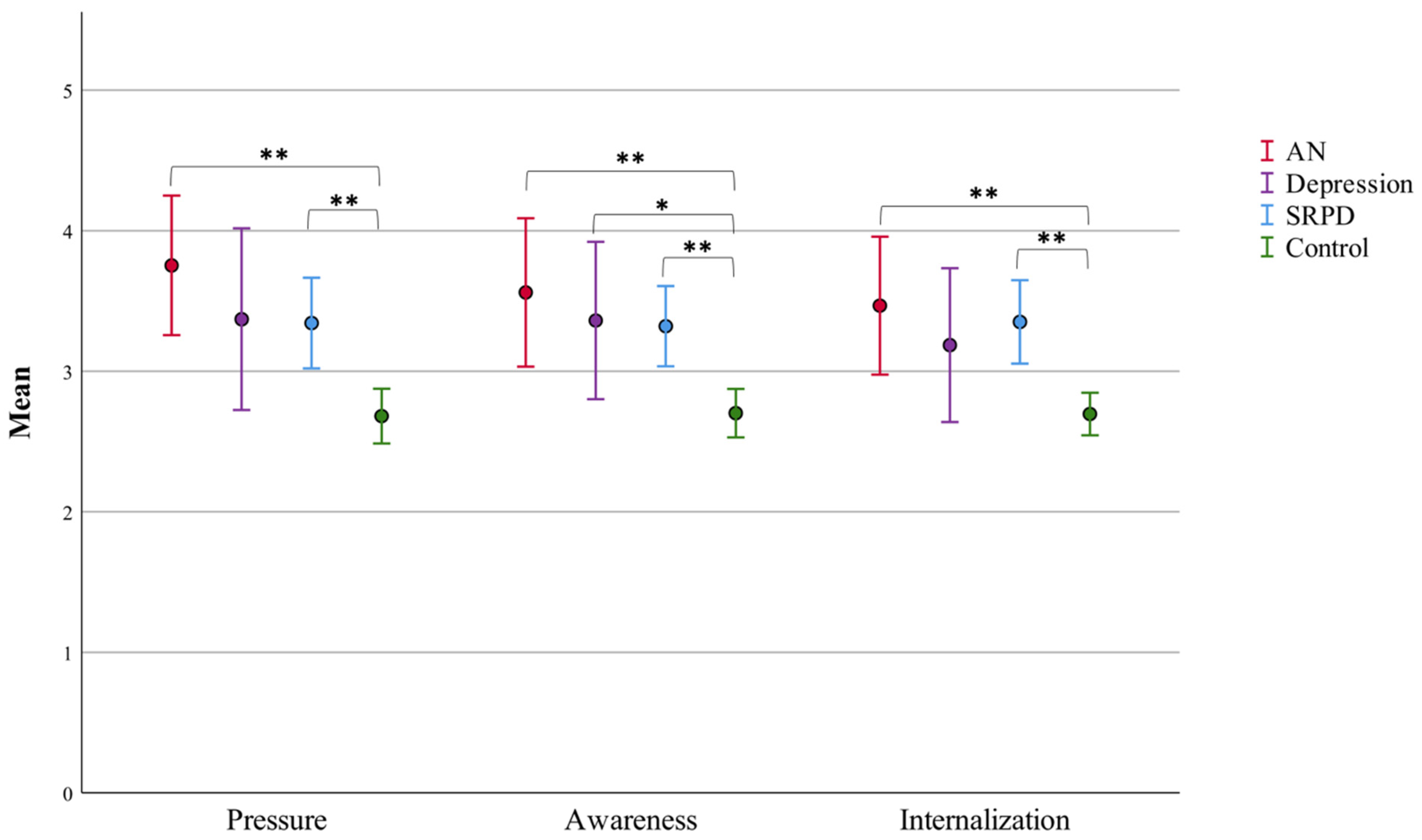
3.4. Social Media Use
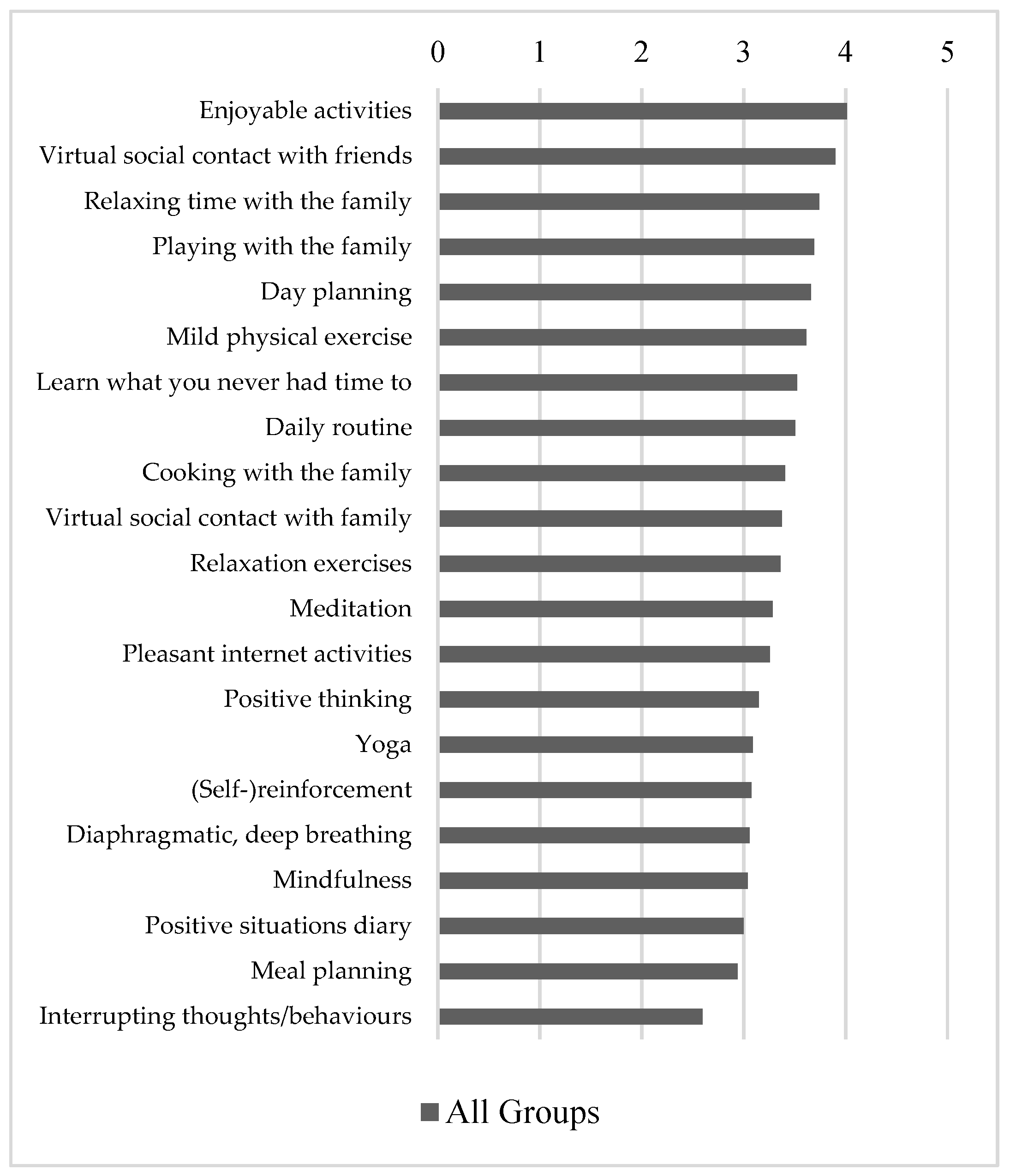
3.5. Use and Helpfulness of Coping Strategies during COVID-19 Restrictions
3.6. Qualitative Analysis: Personal Experiences and Coping Strategies
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schuck, K.; Munsch, S.; Schneider, S. Body image perceptions and symptoms of disturbed eating behavior among children and adolescents in Germany. Child Adolesc. Psychiatry Ment. Health 2018, 12, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravens-Sieberer, U.; Kaman, A.; Otto, C.; Adedeji, A.; Devine, J.; Erhart, M.; Napp, A.K.; Becker, M.; Blanck-Stellmacher, U.; Löffler, C.; et al. Mental Health and Quality of Life in Children and Adolescents During the COVID-19 Pandemic-Results of the Copsy Study. Dtsch. Ärzteblatt Int. 2020, 117, 828–829. [Google Scholar]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Otto, C.; Devine, J.; Löffler, C.; Hurrelmann, K.; Bullinger, M.; Barkmann, C.; Siegel, N.A.; et al. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. Eur. Child Adolesc. Psychiatry 2021, 30, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Otto, C.; Kriston, L.; Rothenberger, A.; Döpfner, M.; Herpertz-Dahlmann, B.; Barkmann, C.; Schön, G.; Hölling, H.; Schulte-Markwort, M.; et al. The longitudinal BELLA study: Design, methods and first results on the course of mental health problems. Eur. Child Adolesc. Psychiatry 2015, 24, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Bignardi, G.; Dalmaijer, E.S.; Anwyl-Irvine, A.L.; Smith, T.A.; Siugzdaite, R.; Uh, S.; Astle, D.E. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch. Dis. Child. 2020, 106, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Waite, P.; Pearcey, S.; Shum, A.; Raw, J.A.; Patalay, P.; Creswell, C. How did the mental health symptoms of children and adolescents change over early lockdown during the COVID-19 pandemic in the UK? JCPP Adv. 2021, 1, e12009. [Google Scholar] [CrossRef]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Thorisdottir, I.E.; Asgeirsdottir, B.B.; Kristjansson, A.L.; Valdimarsdottir, H.B.; Tolgyes, E.M.J.; Sigfusson, J.; Allegrante, J.P.; Sigfusdottir, I.D.; Halldorsdottir, T. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: A longitudinal, population-based study. Lancet Psychiatry 2021, 8, 663–672. [Google Scholar] [CrossRef]
- Koenig, J.; Kohls, E.; Moessner, M.; Lustig, S.; Bauer, S.; Becker, K.; Thomasius, R.; Eschenbeck, H.; Diestelkamp, S.; Gillé, V.; et al. The impact of COVID-19 related lockdown measures on self-reported psychopathology and health-related quality of life in German adolescents. Eur. Child Adolesc. Psychiatry 2021, 30, 1–10. [Google Scholar] [CrossRef]
- Schlegl, S.; Maier, J.; Meule, A.; Voderholzer, U. Eating disorders in times of the COVID-19 pandemic—Results from an online survey of patients with anorexia nervosa. Int. J. Eat. Disord. 2020, 53, 1791–1800. [Google Scholar] [CrossRef]
- Matthews, A.; Kramer, R.A.; Peterson, C.M.; Mitan, L. Higher admission and rapid readmission rates among medically hospitalized youth with anorexia nervosa/atypical anorexia nervosa during COVID-19. Eat. Behav. 2021, 43, 101573. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.A.; Hartman-Munick, S.M.; Kells, M.R.; Milliren, C.E.; Slater, W.A.; Woods, E.R.; Forman, S.F.; Richmond, T.K. The Impact of the COVID-19 Pandemic on the Number of Adolescents/Young Adults Seeking Eating Disorder-Related Care. J. Adolesc. Health 2021, 69, 660–663. [Google Scholar] [CrossRef]
- Spettigue, W.; Obeid, N.; Erbach, M.; Feder, S.; Finner, N.; Harrison, M.E.; Isserlin, L.; Robinson, A.; Norris, M.L. The impact of COVID-19 on adolescents with eating disorders: A cohort study. J. Eat. Disord. 2021, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Springall, G.; Cheung, M.; Sawyer, S.M.; Yeo, M. Impact of the coronavirus pandemic on anorexia nervosa and atypical anorexia nervosa presentations to an Australian tertiary paediatric hospital. J. Paediatr. Child Health 2021, 58, 491–496. [Google Scholar] [CrossRef]
- Goldberg, L.; Ziv, A.; Vardi, Y.; Hadas, S.; Zuabi, T.; Yeshareem, L.; Gur, T.; Steinling, S.; Scheuerman, O.; Levinsky, Y. The effect of COVID-19 pandemic on hospitalizations and disease characteristics of adolescents with anorexia nervosa. Eur. J. Pediatr. 2022, 181, 1767–1771. [Google Scholar] [CrossRef]
- Ayton, A.; Viljoen, D.; Ryan, S.; Ibrahim, A.; Ford, D. Risk, demand, capacity and outcomes in adult specialist eating disorder services in South-East of England before and since COVID-19. BJPsych Bull. 2021, 46, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.J.; Stephan, A.; Menkes, D.B. The impact of COVID-19 on eating disorder referrals and admissions in Waikato, New Zealand. J. Eat. Disord. 2021, 9, 105. [Google Scholar] [CrossRef] [PubMed]
- Vitagliano, J.A.; Jhe, G.; Milliren, C.E.; Lin, J.A.; Spigel, R.; Freizinger, M.; Woods, E.R.; Forman, S.F.; Richmond, T.K. COVID-19 and eating disorder and mental health concerns in patients with eating disorders. J. Eat. Disord. 2021, 9, 1–8. [Google Scholar] [CrossRef]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Billieux, J.; Griffiths, M.D.; Kuss, D.J.; Demetrovics, Z.; Mazzoni, E.; Pallesen, S. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychol. Addict. Behav. 2016, 30, 252–262. [Google Scholar] [CrossRef] [Green Version]
- Cohen, R.; Newton-John, T.; Slater, A. The relationship between Facebook and Instagram appearance-focused activities and body image concerns in young women. Body Image 2017, 23, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Fardouly, J.; Vartanian, L.R. Social Media and Body Image Concerns: Current Research and Future Directions. Curr. Opin. Psychol. 2016, 9, 1–5. [Google Scholar] [CrossRef]
- Sherlock, M.; Wagstaff, D.L. Exploring the relationship between frequency of Instagram use, exposure to idealized images, and psychological well-being in women. Psychol. Popul. Media 2019, 8, 482–490. [Google Scholar] [CrossRef]
- Liu, D.; Baumeister, R.F. Social networking online and personality of self-worth: A meta-analysis. J. Res. Pers. 2016, 64, 79–89. [Google Scholar] [CrossRef]
- Woods, H.C.; Scott, H. #Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J. Adolesc. 2016, 51, 41–49. [Google Scholar] [CrossRef] [Green Version]
- Sidani, J.E.; Shensa, A.; Hoffman, B.; Hanmer, J.; Primack, B.A. The Association between Social Media Use and Eating Concerns among US Young Adults. J. Acad. Nutr. Diet. 2016, 116, 1465–1472. [Google Scholar] [CrossRef] [Green Version]
- Vall-Roqué, H.; Andrés, A.; Saldaña, C. The impact of COVID-19 lockdown on social network sites use, body image disturbances and self-esteem among adolescent and young women. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 110, 110293. [Google Scholar] [CrossRef]
- Vuillier, L.; May, L.; Greville-Harris, M.; Surman, R.; Moseley, R.L. The impact of the COVID-19 pandemic on individuals with eating disorders: The role of emotion regulation and exploration of online treatment experiences. J. Eat. Disord. 2021, 9, 1–18. [Google Scholar] [CrossRef]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and implications for eating disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- Wilksch, S.M.; Wade, T.D. Examination of the Sociocultural Attitudes Towards Appearance Questionnaire-3 in a mixed-gender young-adolescent sample. Psychol. Assess. 2012, 24, 352–364. [Google Scholar] [CrossRef] [Green Version]
- Knauss, C.; Paxton, S.; Alsaker, F.D. Validation of the German version of the Sociocultural Attitudes Towards Appearance Questionnaire (SATAQ-G). Body Image 2009, 6, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Schlottbohm, E.; Tagay, S. Is psychotherapy able to increase quality of life in individuals with eating disorders? Psychother. Psychosom. Med. Psychol. 2015, 65, 163–170. [Google Scholar] [PubMed]
- Brown, M.; Robinson, L.; Campione, G.C.; Wuensch, K.; Hildebrandt, T.; Micali, N. Intolerance of Uncertainty in Eating Disorders: A Systematic Review and Meta-Analysis. Eur. Eat. Disord. Rev. 2017, 25, 329–343. [Google Scholar] [CrossRef]
- Mahoney, A.E.J.; McEvoy, P. A Transdiagnostic Examination of Intolerance of Uncertainty Across Anxiety and Depressive Disorders. Cogn. Behav. Ther. 2012, 41, 212–222. [Google Scholar] [CrossRef]
- Frank, G.K.; Roblek, T.; Bs, M.E.S.; Jappe, L.M.; Rollin, M.D.; Hagman, J.; Pryor, T. Heightened fear of uncertainty in anorexia and bulimia nervosa. Int. J. Eat. Disord. 2011, 45, 227–232. [Google Scholar] [CrossRef] [Green Version]
- McLean, S.A.; Wertheim, E.H.; Masters, J.; Paxton, S. A pilot evaluation of a social media literacy intervention to reduce risk factors for eating disorders. Int. J. Eat. Disord. 2017, 50, 847–851. [Google Scholar] [CrossRef]
- Hards, E.; Loades, M.E.; Higson-Sweeney, N.; Shafran, R.; Serafimova, T.; Brigden, A.; Reynolds, S.; Crawley, E.; Chatburn, E.; Linney, C.; et al. Loneliness and mental health in children and adolescents with pre-existing mental health problems: A rapid systematic review. Br. J. Clin. Psychol. 2021, 61, 313–334. [Google Scholar] [CrossRef]
- Starick, E.; Montemarano, V.; Cassin, S.E. Coping during COVID-19: The Impact of Cognitive Appraisal on Problem Orientation, Coping Behaviors, Body Image, and Perceptions of Eating Behaviors and Physical Activity during the Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11305. [Google Scholar] [CrossRef]
- Miniati, M.; Marzetti, F.; Palagini, L.; Marazziti, D.; Orrù, G.; Conversano, C.; Gemignani, A. Eating Disorders Spectrum During the COVID Pandemic: A Systematic Review. Front. Psychol. 2021, 12, 663376. [Google Scholar] [CrossRef]
- Konstantakopoulos, G.; Tchanturia, K.; Surguladze, S.A.; David, A.S. Insight in eating disorders: Clinical and cognitive correlates. Psychol. Med. 2011, 41, 1951–1961. [Google Scholar] [CrossRef]
- Lock, J. An Update on Evidence-Based Psychosocial Treatments for Eating Disorders in Children and Adolescents. J. Clin. Child Adolesc. Psychol. 2014, 44, 707–721. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, A.; Hoek, H.W.; Schmidt, R. Evidence-based clinical guidelines for eating disorders: International comparison. Curr. Opin. Psychiatry 2017, 30, 423–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, K.E.; Byrne, C.E.; Crosby, R.D.; Le Grange, D. Utilizing Telehealth to deliver family-based treatment for adolescent anorexia nervosa. Int. J. Eat. Disord. 2017, 50, 1235–1238. [Google Scholar] [CrossRef] [PubMed]
- Backhaus, A.; Agha, Z.; Maglione, M.L.; Repp, A.; Ross, B.; Zuest, D.; Rice-Thorp, N.M.; Lohr, J.; Thorp, S.R. Videoconferencing psychotherapy: A systematic review. Psychol. Serv. 2012, 9, 111–131. [Google Scholar] [CrossRef]
- Berryhill, M.B.; Culmer, N.; Williams, N.; Halli-Tierney, A.; Betancourt, A.; Roberts, H.; King, M. Videoconferencing Psychotherapy and Depression: A Systematic Review. Telemed. e-Health 2019, 25, 435–446. [Google Scholar] [CrossRef]
- Hilty, D.M.; Ferrer, D.C.; Parish, M.B.; Johnston, B.; Callahan, E.J.; Yellowlees, P.M. The Effectiveness of Telemental Health: A 2013 Review. Telemed. e-Health 2013, 19, 444–454. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Tabatabaei, M.; Tavakol, K.; Naghipour, M.; Moghbeli, F. Telemental Health Care, an Effective Alternative to Conventional Mental Care: A Systematic Review. Acta Inform. Medica 2017, 25, 240–246. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Wykes, T. Opportunities From the Coronavirus Disease 2019 Pandemic for Transforming Psychiatric Care With Telehealth. JAMA Psychiatry 2020, 77, 1205. [Google Scholar] [CrossRef]
- Wind, T.R.; Rijkeboer, M.; Andersson, G.; Riper, H. The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet Interv. 2020, 20, 100317. [Google Scholar] [CrossRef]
- Bruining, H.; Bartels, M.; Polderman, T.J.; Popma, A. COVID-19 and child and adolescent psychiatry: An unexpected blessing for part of our population? Eur. Child Adolesc. Psychiatry 2020, 30, 1139–1140. [Google Scholar] [CrossRef] [PubMed]
| All Groups (N = 222) | AN (N = 19) | Depression (N = 20) | SRPD (N = 45) | Control (N = 138) | |
|---|---|---|---|---|---|
| Age (years) | |||||
| Mean (SD) | 15.53 (1.92) | 14.60 (1.31) | 15.60 (1.28) | 16.28 (1.89) | 15.40 (2.00) |
| Range | 11.2–18.9 | 12.5–17.6 | 13.5–17.9 | 12.3–18.7 | 11.2–18.9 |
| BMI (kg/m2) | |||||
| Mean (SD) | 19.89 (3.51) | 16.91 (1.88) | 21.05 (3.23) | 21.02 (4.69) | 19.76 (3.01) |
| Range | 12.74–39.18 | 12.74–19.82 | 16.51–30.76 | 14.5–39.18 | 14.06–31.57 |
| Strongly Agree % | Agree % | Undecided % | Disagree % | Strongly Disagree % | Cannot Say % | |
|---|---|---|---|---|---|---|
| All groups | 14.0% | 33.8% | 11.7% | 18.0% | 15.2% | 7.2% |
| AN | 15.8% | 52.6% | 10.6% | 5.3% | 5.3% | 10.5% |
| Depression | 35.0% | 35.0% | 10.0% | 5.0% | 10.0% | 5.0% |
| SRPD | 20.0% | 33.3% | 20.0% | 13.3% | 8.9% | 4.4% |
| Control | 8.7% | 31.2% | 9.4% | 23.2% | 19.6% | 8.0% |
| Personal Experiences | |
| Negative thoughts and mood | “Ultimately, the entire lockdown was a development stage that felt like hell though, especially because one is constantly confronted with oneself.” (SRPD) “It’s very hard not to think negatively in this time [of lockdown].” (Control) “Unfortunately, I fell into a big hole again once the school had started again (…) I didn’t manage to get out of bed anymore or to motivate myself for anything.” (SRPD) |
| Problems at home with family | “(…) the isolation in the same house with the same people was just exhausting.” (Control) “a hard test for our family life” (Control) |
| Struggles with body image and weight (weight loss, weight gain) | “I ate a lot and also gained weight and am very discontent with that now. Because of social media I don’t know if I want to learn to accept myself or lose weight. I’m indecisive what would make me happier.” (Control) “I lost over 10 kg in one year. I was a little bigger before but definitely more carefree and more confident than I am now. I miss my old self. Since the gyms have opened up again, I go there until I must grant myself a rest day. I love exercising, it’s not compulsive in that sense, rather the constant thought about what I’m going to eat today.” (SRPD) |
| Lack of social contacts | “practically sat at home all day” (Control) |
| Positive experiences | “The lockdown was good for me, because going to school is very hard for me. (…) I started becoming more confident and worked on myself, which caused me to feel much better.” (SRPD) “All in all, I experienced many good things and took more time for things. I was more motivated, and I think that the lockdown was good for me.” (Control) |
| Strategies | |
| Time with family and friends | “It also helped me a lot to talk to my friends on the phone.” (Control) “I especially used the time to do more with my family, particularly my siblings.” (SRPD) |
| Working out | “When I was bored, I tried not to eat anything, but to work out.” (Control) “By exercising regularly, I added variety into my everyday life.” (SRPD) |
| Time spent outdoors in nature and/or with animals | “walks in nature” (AN) “walks with my dog” (AN) “Contact with animals helped me a lot.” (Control) |
| Hobbies and interests | “tried new hobbies” (SRPD) “watching movies and TV-shows, playing violent computer games” (Depression) |
| Positive thinking, relaxation exercises | “My number one coping strategy was self-reflection, trauma processing, inner child-healing” (SRPD) “breathing exercises” (Control) “One should always think positive even when the body changes” (SRPD) “Always try to think positive, but that doesn’t help much with body insecurities.” (Control) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muth, L.; Leven, K.-H.; Moll, G.; Kratz, O.; Horndasch, S. Effects of the COVID-19 Restrictions on Eating Behaviour and Eating Disorder Symptomology in Female Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 8480. https://doi.org/10.3390/ijerph19148480
Muth L, Leven K-H, Moll G, Kratz O, Horndasch S. Effects of the COVID-19 Restrictions on Eating Behaviour and Eating Disorder Symptomology in Female Adolescents. International Journal of Environmental Research and Public Health. 2022; 19(14):8480. https://doi.org/10.3390/ijerph19148480
Chicago/Turabian StyleMuth, Lois, Karl-Heinz Leven, Gunther Moll, Oliver Kratz, and Stefanie Horndasch. 2022. "Effects of the COVID-19 Restrictions on Eating Behaviour and Eating Disorder Symptomology in Female Adolescents" International Journal of Environmental Research and Public Health 19, no. 14: 8480. https://doi.org/10.3390/ijerph19148480
APA StyleMuth, L., Leven, K.-H., Moll, G., Kratz, O., & Horndasch, S. (2022). Effects of the COVID-19 Restrictions on Eating Behaviour and Eating Disorder Symptomology in Female Adolescents. International Journal of Environmental Research and Public Health, 19(14), 8480. https://doi.org/10.3390/ijerph19148480






