Hospital Restraints: Safe or Dangerous? A Case of Hospital Death Due to Asphyxia from the Use of Mechanical Restraints
Abstract
:1. Introduction
2. Materials and Methods
3. Case Report
4. Results
4.1. Medical-Record Investigation
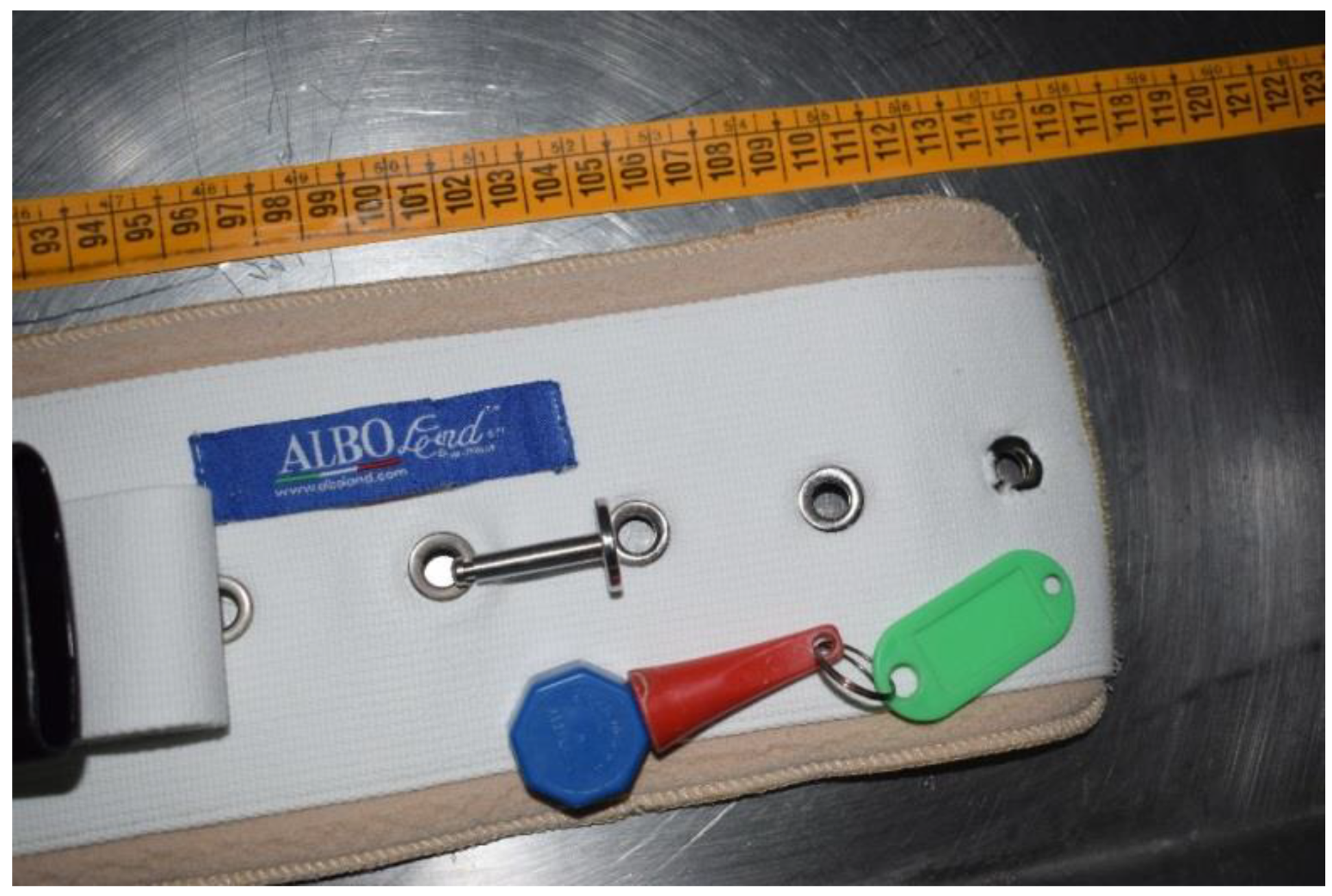
4.2. Crime-Scene Investigation
4.3. Autopsy and Histopathological Findings
5. Discussion
6. Conclusions
- -
- Provide health personnel with periodic information on the appropriate use of restraints;
- -
- Improve operator–patient relationships so that the healthcare staff can personally supervise patients;
- -
- Increase the use of devices that allow video surveillance;
- -
- Apply safety devices for opening and closing doors;
- -
- Apply protective bars to windows to reduce the risk of precipitation;
- -
- Apply rails to beds to prevent falls;
- -
- Use safety devices in buildings and in their surrounding environments;
- -
- Eliminate all objects that could be used by patients as weapons to harm themselves or others (pointed objects, blunt or sharp objects, curtains, carpets).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delmonte, C.; Capelozzi, V.L. Morphologic determinants of asphyxia in lungs: A semiquantitative study in forensic autopsies. Am. J. Forensic Med. Pathol. 2001, 22, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Strömmer, E.M.F.; Leith, W.; Zeegers, M.P.; Freeman, M.D. The role of restraint in fatal excited delirium: A research synthesis and pooled analysis. Forensic Sci. Med. Pathol. 2020, 165, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Achir Yani Syuhaimie Hamid, M.; Catharina Daulima, N.H. The experience of restraint-use among patients with violent behaviors in mental health hospital. Enferm. Clin. 2018, 28 (Suppl. 1), 295–299, (In English and Spanish). [Google Scholar] [CrossRef] [PubMed]
- De Vries, O.J.; Ligthart, G.J.; Nikolaus, T. European Academy of Medicine of Ageing-Course III. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, M922–M923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamers, J.P.; Huizing, A.R. Why do we use physical restraints in the elderly? Z Gerontol. Geriatr. 2005, 38, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Capezuti, E.; Strumpf, N.E.; Evans, L.K.; Grisso, J.A.; Maislin, G. The relationship between physical restraint removal and falls and injuries among nursing home residents. J. Gerontol. A Biol. Sci. Med. Sci. 1998, 53, M47–M52. [Google Scholar] [CrossRef] [Green Version]
- Capezuti, E.; Maislin, G.; Strumpf, N.; Evans, L.K. Side rail use and bed-related fall outcomes among nursing home residents. J. Am. Geriatr. Soc. 2002, 50, 90–96. [Google Scholar] [CrossRef]
- Evans, D.; Wood, J.; Lambert, L.; Fitzgerald, M. Physical Restraint in Acute and Residential Care: A Systematic Review Number 22; Joanna Briggs Institute for Evidence Based Nursing & Midwifery: Adelaide, Australia, 2002. [Google Scholar]
- Demir, A. Nurses’ use of physical restraints in four Turkish hospitals. J. Nurs. Scholarsh. 2007, 39, 38–45. [Google Scholar] [CrossRef]
- Myers, H.; Nikoletti, S.; Hill, A. Nurses’ use of restraints and their attitudes toward restraint use and the elderly in an acute care setting. Nurs. Health Sci. 2001, 3, 29–34. [Google Scholar] [CrossRef]
- Goethals, S.; Dierckx de Casterlé, B.; Gastmans, C. Nurses’ decision-making process in cases of physical restraint in acute elderly care: A qualitative study. Int. J. Nurs. Stud. 2013, 50, 603–612. [Google Scholar] [CrossRef]
- Brown, E.A. Systematic review of the effects of prison segregation. Aggress. Violent Behav. 2020, 52, 101389. [Google Scholar] [CrossRef]
- Grassi, S.; Mandarelli, G.; Polacco, M.; Vetrugno, G.; Spagnolo, A.G.; De-Giorgio, F. Suicide of isolated inmates suffering from psychiatric disorders: When a preventive measure becomes punitive. Int. J. Legal. Med. 2018, 132, 1225–1230. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.; Aboud, A.; Smith, T. Using the stress–vulnerability model to better understand suicide in prison populations. Psychiatry Psychol. Law 2022, 1–35. [Google Scholar] [CrossRef]
- Cramer, R.J.; Kaniuka, A.R.; Peiper, L.J. The core competency model for corrections: An education program for managing self-directed violence in correctional institutions. Psychol. Serv. 2022. [Google Scholar] [CrossRef] [PubMed]
- Testoni, I.; Marrella, F.; Biancalani, G.; Cottone, P.; Alemanno, F.; Mamo, D.; Grassi, L. The Value of Dignity in Prison: A Qualitative Study with Life Convicts. Behav. Sci. 2020, 10, 95. [Google Scholar] [CrossRef]
- Koczy, P.; Becker, C.; Rapp, K.; Klie, T.; Beische, D.; Büchele, G.; Kleiner, A.; Guerra, V.; Rissmann, U.; Kurrle, S.; et al. Effectiveness of a Multifactorial Intervention to Reduce Physical Restraint in Nursing Home Resents. J. Am. Soc. Geriatr. 2011, 59, 333–339. [Google Scholar] [CrossRef]
- Castle, N.G.; Fogel, B.; Mor, V. Risk factors for physical restraint use in nursing homes: Pre- and post-implementation of the Nursing Home Reform Act. Gerontologist 1997, 37, 737–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharifi, A.; Arsalani, N.; Fallahi-Khoshknab, M.; Mohammadi-Shahbolaghi, F.; Ebadi, A. Iranian nurses’ perceptions about using physical restraint for hospitalized elderly people: A cross-sectional descriptive-correlational study. BMC Geriatr. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Cordasco, F.; Scalise, C.; Sacco, M.A.; Bonetta, C.F.; Zibetti, A.; Cacciatore, G.; Caputo, F.; Ricci, P.; Aquila, I. The silent deaths of the elderly in long-term care facilities during the COVID-19 pandemic: The role of forensic pathology. Med. Leg. J. 2020, 88, 66–68. [Google Scholar] [CrossRef]
- NICE (National Institute for Health and Care Excellence). Violence and aggression: Short-Term Management in Mental Health, Health and Community Settings. Available online: https://www.nice.org.uk/guidance/ng10 (accessed on 12 June 2022).
- Southcott, J.; Howard, A.; Collins, E. Control and restraint training in acute mental health care. Nurs. Stand. 2002, 16, 33–36. [Google Scholar] [CrossRef]
- Raveesh, B.N.; Lepping, P. Restraint guidelines for mental health services in India. Indian J. Psychiatry 2019, 61 (Suppl. 4), S698–S705. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scalise, C.; Cordasco, F.; Sacco, M.A.; Aquila, V.R.; Ricci, P.; Aquila, I. Hospital Restraints: Safe or Dangerous? A Case of Hospital Death Due to Asphyxia from the Use of Mechanical Restraints. Int. J. Environ. Res. Public Health 2022, 19, 8432. https://doi.org/10.3390/ijerph19148432
Scalise C, Cordasco F, Sacco MA, Aquila VR, Ricci P, Aquila I. Hospital Restraints: Safe or Dangerous? A Case of Hospital Death Due to Asphyxia from the Use of Mechanical Restraints. International Journal of Environmental Research and Public Health. 2022; 19(14):8432. https://doi.org/10.3390/ijerph19148432
Chicago/Turabian StyleScalise, Carmen, Fabrizio Cordasco, Matteo Antonio Sacco, Valerio Riccardo Aquila, Pietrantonio Ricci, and Isabella Aquila. 2022. "Hospital Restraints: Safe or Dangerous? A Case of Hospital Death Due to Asphyxia from the Use of Mechanical Restraints" International Journal of Environmental Research and Public Health 19, no. 14: 8432. https://doi.org/10.3390/ijerph19148432
APA StyleScalise, C., Cordasco, F., Sacco, M. A., Aquila, V. R., Ricci, P., & Aquila, I. (2022). Hospital Restraints: Safe or Dangerous? A Case of Hospital Death Due to Asphyxia from the Use of Mechanical Restraints. International Journal of Environmental Research and Public Health, 19(14), 8432. https://doi.org/10.3390/ijerph19148432







