Barriers and Supports in eHealth Implementation among People with Chronic Cardiovascular Ailments: Integrative Review
Abstract
1. Introduction
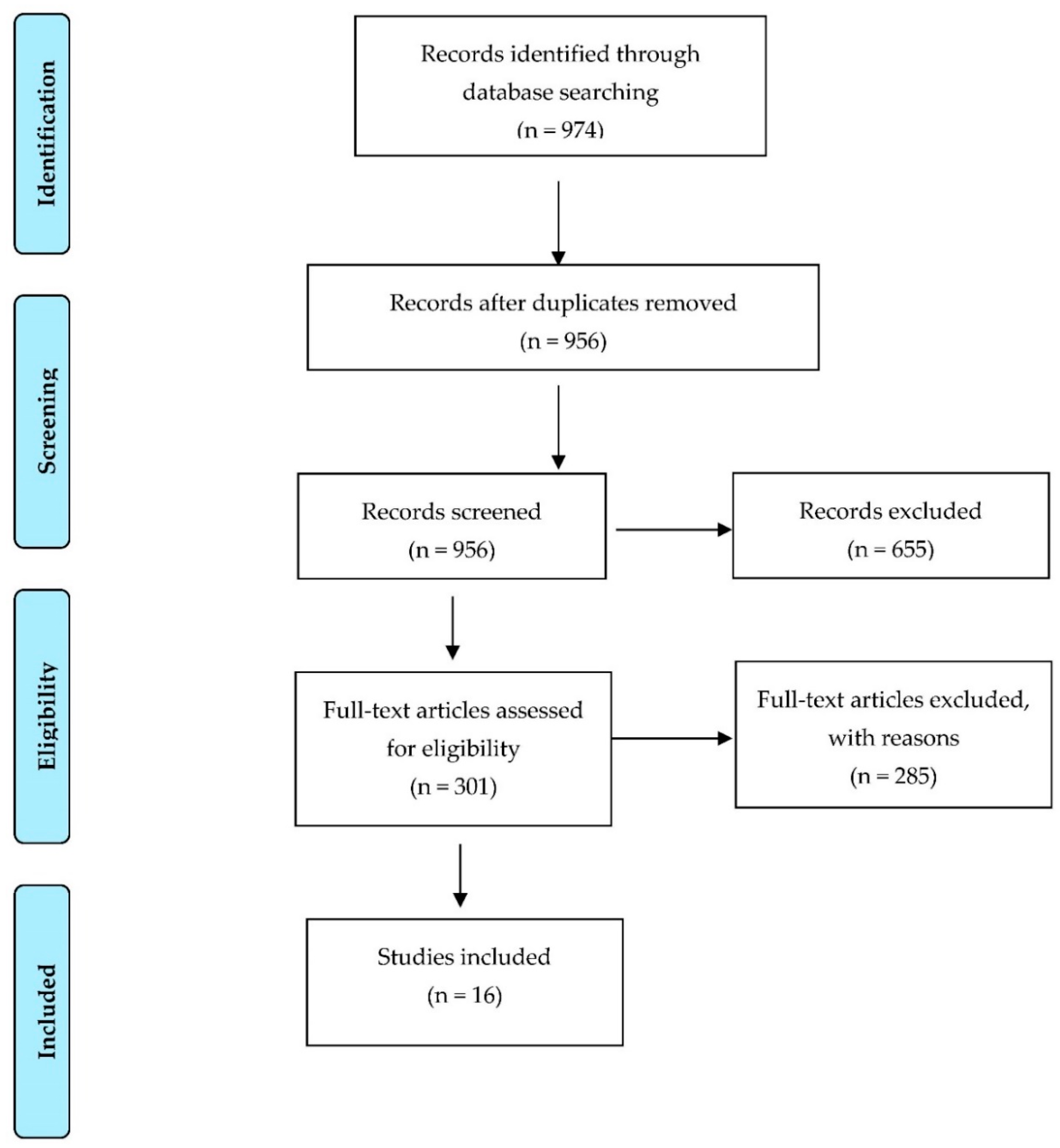
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO. Non Communicable Diseases Country Profiles; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Gallardo, A.; Franco, P.; Urtubey, X. Experiencia de pacientes con diabetes e hipertensión que participan en un programa de telemonitoreo. CES Med. 2019, 33, 31–41. [Google Scholar] [CrossRef]
- Boyne, J.J.J.; Vrijhoef, H.J.M. Implementing Telemonitoring in Heart Failure Care: Barriers from the Perspectives of Patients, Healthcare Professionals and Healthcare Organizations. Curr. Heart Fail. Rep. 2013, 10, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Dario, C.; Toffani, R.; Calcaterra, F.; Saccavini, C.; Stafylas, P.; Mancin, S.; Vio, E. Original Research Telemonitoring of Type 2 Diabetes Mellitus in Italy. Telemed. e-Health 2017, 23, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Chew, L.; Xin, X.; Yang, H.; Thumboo, J. An evaluation of the Virtual Monitoring Clinic, a novel nurse-led service for monitoring patients with stable rheumatoid arthritis. Int. J. Rheum. Dis. 2019, 22, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Nemanic, T.; Sarc, I.; Skrgat, S.; Flezar, M.; Cukjati, I.; Malovrh, M.M. Telemonitoring in asthma control: A randomized controlled trial. J. Asthma 2019, 56, 782–790. [Google Scholar] [CrossRef]
- Melo, M.d.C.B.; Santos, A.F.; Alves, H.J.; Queiroz, T.C.N.; Silva, N.L.C. Telemonitoring of Neonatal Intensive Care Units: Preliminary Experience in the State of Minas Gerais, Brazil. Am. J. Perinatol. 2019, 36, 393–398. [Google Scholar]
- Ware, P.; Dorai, M.; Ross, H.J.; A Cafazzo, J.; Laporte, A.; Boodoo, C.; Seto, E. Patient Adherence to a Mobile Phone–Based Heart Failure Telemonitoring Program: A Longitudinal Mixed-Methods Study. JMIR mHealth uHealth 2019, 7, e13259. [Google Scholar] [CrossRef]
- Lang, C.; Scheibe, M.; Voigt, K.; Hübsch, G.; Mocke, L.; Schmitt, J.; Bergmann, A.; Holthoff-Detto, V. Reasons for non-acceptance and non-use of a home telemonitoring application bymultimorbid patients aged 65 years and over. Z. Für Evidenz Fortbild. Und Qual. Im Gesundh. 2019, 141–142, 76–88. Available online: http://www.elsevier.com/locate/zefq (accessed on 2 June 2022). [CrossRef]
- Knibb, R.C.; Alviani, C.; Garriga-Baraut, T.; Mortz, C.G.; Vazquez-Ortiz, M.; Angier, E.; Blumchen, K.; Comberiati, P.; Duca, B.; DunnGalvin, A.; et al. The effectiveness of interventions to improve self-management for adolescents and young adults with allergic conditions: A systematic review. Allergy 2020, 75, 1881–1898. [Google Scholar] [CrossRef]
- Thabrew, H.; Stasiak, K.; Hetrick, S.E.; Wong, S.; Huss, J.H.; Merry, S.N. eHealth interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst. Rev. 2017, 2017, CD012489. [Google Scholar] [CrossRef]
- Jiménez-Muñoz, L.; Gutiérrez-Rojas, L.; Porras-Segovia, A.; Courtet, P.; Baca-García, E. Mobile applications for the management of chronic physical conditions: A systematic review. Intern. Med. J. 2022, 52, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Rezapour, A.; Hosseinijebeli, S.S.; Faradonbeh, S.B. Economic evaluation of E-health interventions compared with alternative treatments in older persons’ care: A systematic review. J. Educ. Health Promot. 2021, 10, 134. [Google Scholar] [PubMed]
- Ekeland, A.G.; Bowes, A.; Flottorp, S. Effectiveness of telemedicine: A systematic review of reviews. Int. J. Med. Inform. 2010, 79, 736–771. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Saaiq, M.; Ashraf, B. Modifying “Pico” Question into “Picos” Model for More Robust and Reproducible Presentation of the Methodology Employed in A Scientific Study. World J. Plast. Surg. 2017, 6, 390–392. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D. The PRISMA group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Pennsylvania State University Libraries. Levels of Evidence; The Pennsylvania State University: University Park, PA, USA, 2021; Available online: https://guides.libraries.psu.edu/c.php?g=319063&p=5221999 (accessed on 13 December 2020).
- Steinman, L.; Heang, G.; Van Pelt, M.; Haixia, N.; Rao, M.; LoGerfo, J.; Fitzpatrick, A. Enablers and Barriers to Chronic Disease Self-Management and Mobile Health Interventions for People Living with Diabetes and Hypertension in Cambodia: A Qualitative Study. JMIR mHealth uHealth 2020, 8, 13536. [Google Scholar] [CrossRef]
- Herrmann, M.; Boehme, P.; Hansen, A.; Jansson, K.; Rebacz, P.; Ehlers, J.P.; Mondritzki, T.; Truebel, H. Digital Competencies and Attitudes Toward Digital Adherence Solutions Among Elderly Patients Treated with Novel Anticoagulants: Qualitative Study. J. Med. Internet Res. 2020, 22, e13077. [Google Scholar] [CrossRef]
- Marsh, K.; Bush, R.; Connelly, C. Exploring perceptions and use of the patient portal by young adults with type 1 diabetes: A qualitative study. Health Inform. J. 2020, 26, 2586–2596. [Google Scholar] [CrossRef]
- Gjestsen, M.T.; Wiig, S.; Testad, I.; Mishina, K.; Anderson, K. Health Care Personnel’s Perspective on Potential Electronic Health Interventions to Prevent Hospitalizations for Older Persons Receiving Community Care: Qualitative Study. J. Med. Internet Res. 2020, 22, e12797. [Google Scholar] [CrossRef]
- Zigdom, A.; Zigdon, T.; Sender, D. Attitudes of Nurses Towards Searching Online for Medical Information for Personal Health Needs: Cross-Sectional Questionnaire Study. J. Med. Internet Res. 2020, 22, e16133. [Google Scholar] [CrossRef]
- Ernsting, C.; Mareike, L.; Dombrowski, S.; Voigt, J.; Kuhlmey, A.; Gellert, P. Associations of Health App Use and Perceived Effectiveness in People with Cardiovascular Diseases and Diabetes: Population-Based Survey. JMIR mHealth uHealth 2019, 7, e12179. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, B.; Bagala, M.; Creighton, A.; Leavey, T.; Nicholls, S.; Wood, C.; Longman, J.; Barker, J.; Pit, S. Mobile phone applications and their use in the self-management of Type 2 Diabetes Mellitus: A qualitative study among app users and non-app users. Diabetol. Metab. Syndr. 2019, 11, 84. [Google Scholar] [CrossRef] [PubMed]
- Mangin, D.; Parascandalo, J.; Khudoyarova, O.; Agarwal, G.; Bismah, V.; Orr, S. Multimorbidity, eHealth and implications for equity: A cross-sectional survey of patient perspectives on eHealth. BMJ Open. 2019, 9, e023731. [Google Scholar] [CrossRef] [PubMed]
- Milos, V.; Borgström, B.; Wolff, M.; Calling, S.; Gerward, S.; Sandberg, M. Having to learn this so late in our lives…’ Swedish elderly patients’ beliefs, experiences, attitudes and expectations of e-health in primary health care. Scand. J. Prim. Health Care. 2019, 37, 41–52. [Google Scholar]
- Diaz-Skeete, Y.; Giggins, O.M.; McQuaid, D.; Beaney, P. Enablers and obstacles to implementing remote monitoring technology in cardiac care: A report from an interactive workshop. Health Inform. J. 2019, 26, 2280–2288. [Google Scholar] [CrossRef]
- Rhoads, S.J.; Serrano, C.I.; Lynch, C.E.; Ounpraseuth, S.T.; Gauss, C.H.; Payakachat, N.; Lowery, C.L.; Eswaran, H. Exploring Implementation of m-Health Monitoring in Postpartum Women with Hypertension. Telemed. e-Health 2017, 23, 833–841. [Google Scholar] [CrossRef]
- Ernsting, C.; Dombrowski, S.; Oedekoven, M.; O´Sullivan, L.; Kanzler, M.; Kuhlmeyet, A.; Gellert, P. Using Smartphones and Health Apps to Change and Manage Health Behaviors: A Population-Based Survey. J. Med. Internet Res. 2017, 19, e6838. [Google Scholar] [CrossRef]
- Stangeland, S.; Karlsen, B.; Oord, E.R.; Graue, M.; Oftedal, B. Dropout From an eHealth Intervention for Adults with Type 2 Diabetes: A Qualitative Study. J. Med. Internet Res. 2017, 19, e7479. [Google Scholar]
- Ondiege, B.; Clarke, M. Investigating User Identification in Remote Patient Monitoring Devices. Bioengineering 2017, 4, 76. [Google Scholar] [CrossRef]
- Duplaga, M. Searching for a Role of Nursing Personnel in Developing Landscape of Ehealth: Factors Determining Attitudes toward Key Patient Empowering Applications. PLoS ONE 2016, 11, e0153173. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Granger, D.; Vandelanotte, C.; Duncan, M.J.; Alley, S.; Schoeppe, S.; Short, C.; Rebar, A. Is preference for mHealth intervention delivery platform associated with delivery platform familiarity? BMC Public Health 2016, 16, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Ortega, M. Dimensión formativa de la alfabetización tecnológica. TESI 2009, 10, 129–152. [Google Scholar] [CrossRef]
- Day, K.; Gu, Y. Influencing factors for adopting personal health record (PHR). Stud. Health Technol. Inform. 2012, 178, 39–44. [Google Scholar]
- González, M.; Herrera, O. Bioética y nuevas tecnologías: Telemedicina. Rev. Cubana Enfermer. 2007, 23, 1–12. [Google Scholar]
- Gorini, A.; Mazzocco, K.; Triberti, S.; Sebri, V.; Savioni, L.; Pravettoni, G. A P5 Approach to m-Health: Design Suggestions for Advanced Mobile Health Technology. Front. Psychol. 2018, 9, 2066. [Google Scholar] [CrossRef]
- Parker, S.; Prince, P.; Thomas, L. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: A systematic review and realist synthesis. BMJ Open 2018, 8, e019192. [Google Scholar] [CrossRef]
- Saner, H.; Velde, E. eHealth in cardiovascular medicine: A clinical update. Eur. J. Prev. Cardiol. 2016, 23, 5–12. [Google Scholar] [CrossRef]
- Van Gemert-Pijnen, J.E.; Nijland, N.; van Limburg, M.; Ossebaard, H.C.; Kelders, S.M.; Eysenbach, G.; Seydel, E.R. A holistic framework to improve the uptake and impact of eHealth technologies. J. Med. Internet Res. 2011, 13, e111. [Google Scholar] [CrossRef]
- Granja, C.; Janssen, W.; Johansen, M.A. Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature. J. Med. Internet Res. 2018, 20, e10235. [Google Scholar] [CrossRef]
- Jager, M.; Zeeuw, J.; Tullius, J.; Papa, R.; Giammarchi, C.; Whittal, A.; de Winter, A.F. Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies. Int. J. Environ. Res. Public Health 2019, 16, 4300. [Google Scholar] [CrossRef] [PubMed]
- González, P.; Morocho, V. Estrategias de sensibilización para la ejecución de proyectos de telesalud. Latin Am. J. Telehealth. 2010, 2, 302–317. [Google Scholar]
- Varsi, C.; Solberg, L.; Kristjansdottir, Ö.; Kelders, S.; Stenberg, U.; Zangi, H.; Børøsund, E.; Weiss, K.E.; Stubhaug, A.; Asbjørnsen, R.A.; et al. Implementation Strategies to Enhance the Implementation of eHealth Programs for Patients with Chronic Illnesses: Realist Systematic Review. J. Med. Internet Res. 2019, 21, 14255. [Google Scholar] [CrossRef] [PubMed]
- Parellada, E.; Bioque, M. Barriers to the Use of Long-Acting Injectable Antipsychotics in the Management of Schizophrenia. CNS Drugs 2016, 30, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Kaper, M.S.; Sixsmith, J.; Koot, J.A.; Meijering, L.B.; van Twillert, S.; Giammarchi, C.; Bevilacqua, R.; Barry, M.M.; Doyle, P.; Reijneveld, S.A.; et al. Developing and pilot testing a comprehensive health literacy communication training for health professionals in three European countries. Patient Educ. Couns. 2018, 101, 152–158. [Google Scholar] [CrossRef]
- Varsi, C.; Ekstedt, M.; Gammon, D.; Ruland, C.M. Using the consolidated framework for implementation research to identify barriers and facilitators for the implementation of an internet-based patient-provider communication service in five settings: A qualitative study. J. Med. Internet Res. 2015, 17, e262. [Google Scholar] [CrossRef]
- Samuels-Kalow, M.; Rhodes, K.; Uspal, J.; Reyes Smith, A.; Hardy, E.; Mollen, C. Unmet needs at the time of emergency department discharge. Acad. Emerg. Med. 2016, 23, 279–287. [Google Scholar] [CrossRef]
- Reiners, F.; Sturm, J. Sociodemographic Factors Influencing the Use of eHealth in People with Chronic Diseases. Int. J. Environ. Res. Public Health 2019, 16, 645. [Google Scholar] [CrossRef]
- Sandström, B.; Borglin, G.; Nilsson, R.; Willman, A. Promoting the Implementation of Evidence-Based Practice: A Literature Review Focusing on the Role of Nursing Leadership. Worldviews Evid. Based Nurs. 2011, 8, 212–223. [Google Scholar] [CrossRef]
- McKenna, V.; Sixsmith, J.; Barry, M. The relevance of context in understanding health literacy skills: Findings from a qualitative study. Health Expect. 2017, 20, 1049–1060. [Google Scholar] [CrossRef]
- Lambrinou, E.; Kyriakou, M.; Lakatamitou, I.; Angus, N.; Khatib, R.; Vellone, E. An integrative review on facilitators and barriers in delivering and managing injectable therapies in chronic conditions: A part of the ACNAP project ‘injectable medicines among patients with cardiovascular conditions’. Eur. J. Cardiovasc. Nurs. 2020, 19, 663–680. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Country | Objective | Study Design | Participants | Chronic Condition | eHealth Tool | Evidence Level |
|---|---|---|---|---|---|---|---|
| Steinman et al., 2020 [19]. | Cambodia | To understand facilitators and barriers to chronic disease management and the acceptability, appropriateness, and feasibility of mHealth to support chronic disease management and strengthen community-clinical linkages to existing services. | Qualitative exploratory study | 70 patients | ATH and DM2 | Text messages | Level 6 |
| Hermann et al., 2020 [20]. | Germany | Identifying factors supporting adhesion to digital focuses and wider patient acceptance. | Qualitative with grounded theory focus. | 20 patients with anticoagulant therapy, age > 65 years. | CVA and AMI | Telemonitoring via smartphone | Level 6 |
| Marsh et al., 2020 [21]. | USA | Exploring portal knowledge among emerging adult patients, with perceived barriers and aids. | Qualitative study | 27 emerging adults with Type 1 Diabetes Mellitus. | DM1 | Virtual health education platform. | Level 6 |
| Gjestsen et al., 2020 [22]. | Norway | Identify managers’ and professionals’ perspectives on eHealth intervention use. | Qualitative with case-study focus. | 17 health functionaries. | ----------- | Virtual health platform. | Level 6 |
| Zigdom et al., 2020 [23]. | Israel | Evaluate attitudes among general hospital nurses towards online medical information searching | Cross-sectional quantitative study. | 121 nurses at 3 general hospitals. | ----------- | Online database information search. | Level 6 |
| Ernsting et al., 2019 [24]. | Germany | Identify factors associated with chronic patients’ mobile health app use. | Quantitative study of secondary data analysis. | 1500 participants in a Web-based survey. | ATH, DM2, CVA, AMI | Pfizer Monitor mobile application | Level 6 |
| Jeffrey et al., 2019 [25]. | Australia | Evaluate experiences, barriers and aids to app use among people with Type 2 diabetes. | Qualitative | 30 people with DM2 diagnoses. | DM2 | Mobile health application. | Level 6 |
| Mangin et al., 2019 [26]. | Canada | Examine attitudes and online eHealth record use in patients with chronic cardiovascular disorders | Cross-sectional quantitative study. | 693 patients with primary care chronic cardiovascular conditions. | Chronic unspecified cardiovascular conditions. | Virtual health platform. | Level 6 |
| Milos et al., 2019 [27]. | Sweden | Exploring senior citizens’ attitudes and beliefs to better understand the factors influencing eHealth adhesion. | Qualitative study | 15 primary care left patients with chronic conditions | Nonspecified chronic cardiovascular conditions. | Mobile health application. | Level 6 |
| Díaz et al., 2019 [28]. | Ireland | Exploring barriers and aids to institutional-level eHealth technology adoption. | Summary of consensus at eHealth Innovations for Home and Community Care conference. | Doctors, research professors, policymakers and health service representatives. | ------------- | Cardiac telemonitoring. | Level 7 |
| Rhoads et al., 2017 [29] | USA | To identify the potential factors that influenced the use of m-health technology and adherence to the control of hypertension symptoms | Nonrandomized controlled study | 48 women | ATH | Telemonitoring of arterialpressure | Level 6 |
| Ernsting et al., 2017 [30]. | Germany | Exploring reach of smartphone and health app use and their use behavior in chronic patients. | Quantitative correlational study. | Survey of 4144 patients over 35 years old with chronic cardiovascular conditions. | Unspecified chronic conditions. | Mobile health app. | Level 6 |
| Stangeland et al., 2017 [31]. | Norway | Exploring experiences with a GSD-based eHealth intervention and understanding reasons for leaving it. | Qualitative study. | 12 adults with DM2 who left an eHealth intervention. | DM2 | Mobile health app. | Level 6 |
| Ondiege et al., 2017 [32]. | England | Exploring hypertension patients’ beliefs and worries about monitoring devices | Qualitative study | 20 cohabitating couples suffering from hypertension | ATH | Arterial pressure telemonitoring. | Level 6 |
| Duplaga et al., 2017 [33]. | USA | Evaluating skills, technology use and exploring opinions about the health area among nurses. | Quantitative cross-sectional study. | 628 nurses took a questionnaire to evaluate technology use in healthcare | ------------- | Virtual health platform. | Level 6 |
| Granger et al., 2016 [34]. | Australia | Determining whether greater smartphone-Tablet familiarity was associated with higher eHealth use, | Quantitative correlational study | 1865 participants with cardiovascular conditions who used technology. | Unspecified chronic conditions. | Mobile health app. | Level 6 |
| Article | Level | Barriers | Aids |
|---|---|---|---|
| Steinman et al., 2020 [19]. | Patient |
|
|
| Hermann M et al., 2020 [20]. | Patient |
|
|
| Marsh K et al., 2020 [21]. | Patient |
|
|
| Gjestsen M et al., 2020 [22]. | Healthcare Professional |
|
|
| Zigdom A et al., 2020 [23]. | Healthcare Professional |
|
|
| Ernsting C et al., 2019 [24]. | Patient |
|
|
| Jeffrey B et al., 2019 [25]. | Patient |
|
|
| Mangin D et al., 2019 [26]. | Patient |
|
|
| Milos V et al., 2019 [27]. | Patient |
|
|
| Díaz Y et al., 2019 [28]. | Institutional |
|
|
| Rhoads et al., 2017 [29]. | Patient |
|
|
| Ernsting C et al., 2017 [30]. | Patient |
|
|
| Stangeland S et al., 2017 [31]. | Patient |
|
|
| Ondiege B et al., 2017 [32]. | Patient |
|
|
| Duplaga M et al., 2017 [33]. | Healthcare professionals |
|
|
| Granger D et al., 2016 [34]. | Patient |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera, S.; Salazar, A.; Nazar, G. Barriers and Supports in eHealth Implementation among People with Chronic Cardiovascular Ailments: Integrative Review. Int. J. Environ. Res. Public Health 2022, 19, 8296. https://doi.org/10.3390/ijerph19148296
Herrera S, Salazar A, Nazar G. Barriers and Supports in eHealth Implementation among People with Chronic Cardiovascular Ailments: Integrative Review. International Journal of Environmental Research and Public Health. 2022; 19(14):8296. https://doi.org/10.3390/ijerph19148296
Chicago/Turabian StyleHerrera, Sophia, Alide Salazar, and Gabriela Nazar. 2022. "Barriers and Supports in eHealth Implementation among People with Chronic Cardiovascular Ailments: Integrative Review" International Journal of Environmental Research and Public Health 19, no. 14: 8296. https://doi.org/10.3390/ijerph19148296
APA StyleHerrera, S., Salazar, A., & Nazar, G. (2022). Barriers and Supports in eHealth Implementation among People with Chronic Cardiovascular Ailments: Integrative Review. International Journal of Environmental Research and Public Health, 19(14), 8296. https://doi.org/10.3390/ijerph19148296







