The Role of Digital Technology in Curbing COVID-19
Abstract
:1. Introduction
Digital Health Solutions
- Which digital technologies have been used during the COVID-19 pandemic to mitigate the transmission of the virus?
- To what extent have digital technology applications helped to mitigate the spread of COVID-19?
- Which facilitators and barriers have contributed to the usability of digital technologies during the COVID-19 pandemic?
2. Methods
3. Results
3.1. Which Digital Technologies Have Been Used during COVID-19 to Mitigate the Transmission of the Virus?
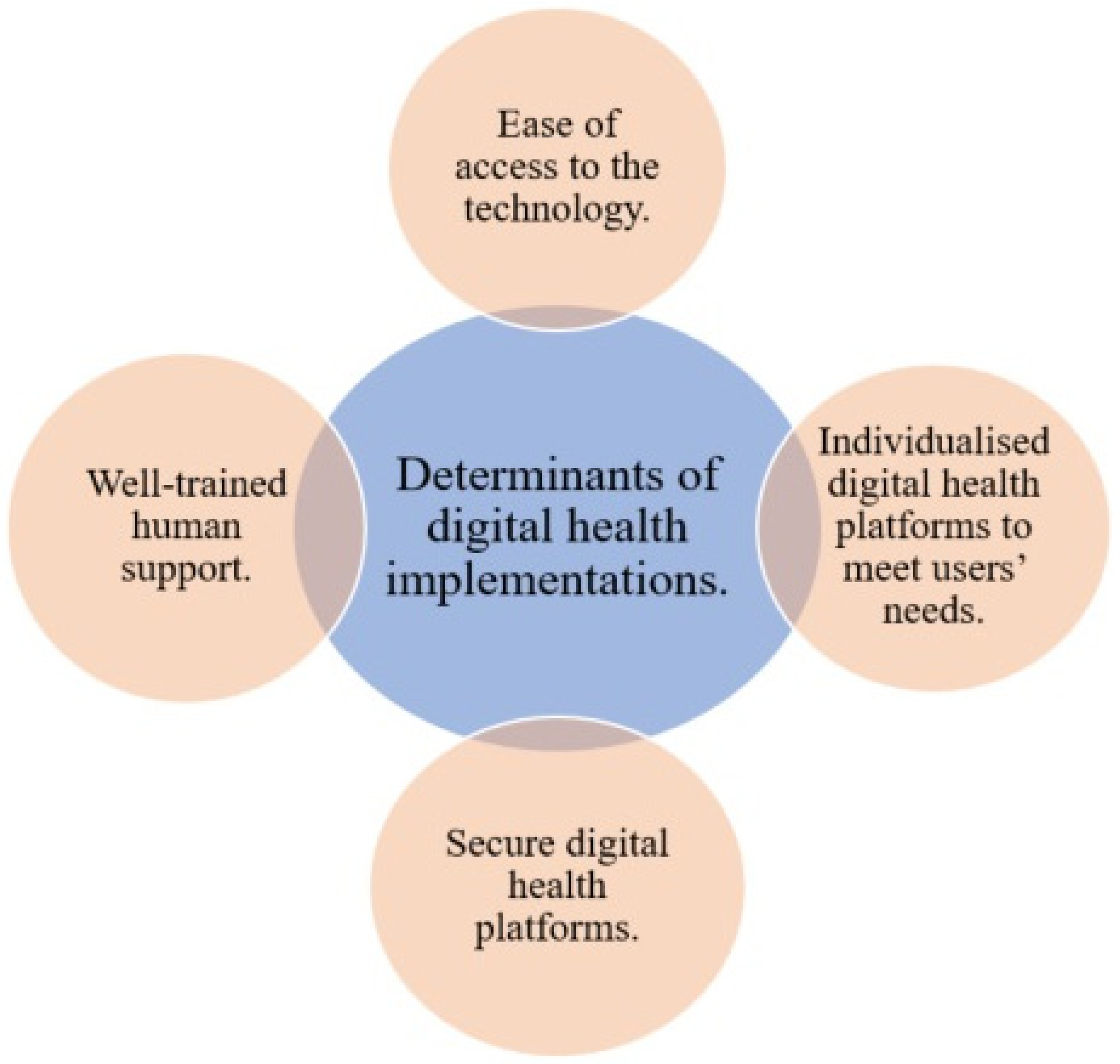
3.2. Determinants of Digital Health during COVID-19
3.3. To What Extent Have Digital Technology Applications Helped to Mitigate the Spread of COVID-19?
3.3.1. Telehealth Has Helped to Follow Up and Treat People with Chronic Diseases
3.3.2. Tele-Education to Support Professional Training
3.3.3. Virtual Intensive Care Unit
3.3.4. Virtual Reality Helps in the Management of Pain and Physical Therapy
3.3.5. Tele-Pharmacy Services
3.3.6. Artificial Intelligence Helps in Decision Making
3.3.7. Machine Learning Has Helped in Predictions, Expectations, and Planning
3.4. What Are the Facilitators and Barriers That Contribute to the Usability of Digital Technologies during the COVID-19 Pandemic?
3.4.1. Government Support
3.4.2. Technology and Computer Literacy
3.4.3. Faster Vaccine Development
3.4.4. Access Real-Time Data
3.4.5. Cost-Effectiveness
3.4.6. Barriers
3.4.7. Healthcare Systems Complexity
3.4.8. Lack of Financial Support
3.4.9. Absent of the Guidelines
4. Limitations
5. Conclusions and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pan, L.; Mu, M.; Yang, P.; Sun, Y.; Wang, R.; Yan, J.; Li, P.; Hu, B.; Wang, J.; Hu, C. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Jebril, N. World Health Organization declared a pandemic public health menace: A systematic review of the coronavirus disease 2019 “COVID-19”. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Gostin, L.O.; Wiley, L.F. Governmental public health powers during the COVID-19 pandemic: Stay-at-home orders, business closures, and travel restrictions. JAMA 2020, 323, 2137–2138. [Google Scholar] [CrossRef]
- Alghamdi, S.M.; Alsulayyim, A.S.; Alqahtani, J.S.; Aldhahir, A.M. Digital Health platforms in Saudi Arabia: Determinants from the COVID-19 pandemic experience. Healthcare 2021, 8, 1517. [Google Scholar] [CrossRef]
- Lone, S.A.; Ahmad, A. COVID-19 pandemic—An African perspective. Emerg. Microbes Infect. 2020, 9, 1300–1308. [Google Scholar] [CrossRef]
- Shrestha, N.; Shad, M.Y.; Ulvi, O.; Khan, M.H.; Karamehic-Muratovic, A.; Nguyen, U.-S.D.; Baghbanzadeh, M.; Wardrup, R.; Aghamohammadi, N.; Cervantes, D. The impact of COVID-19 on globalization. One Health 2020, 11, 100180. [Google Scholar] [CrossRef]
- Watts, G. COVID-19 and the digital divide in the UK. Lancet Digit. Health 2020, 2, e395–e396. [Google Scholar] [CrossRef]
- Barlow, J. Managing Innovation in Healthcare; World Scientific Publishing Company: London, UK, 2016. [Google Scholar] [CrossRef]
- Alghamdi, S.M.; Alqahtani, J.S.; Aldhahir, A.M. Current status of telehealth in Saudi Arabia during COVID-19. J. Fam. Community Med. 2020, 27, 208. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Imran, A.; Posokhova, I.; Qureshi, H.N.; Masood, U.; Riaz, M.S.; Ali, K.; John, C.N.; Hussain, M.I.; Nabeel, M. AI4COVID-19: AI enabled preliminary diagnosis for COVID-19 from cough samples via an app. Inform. Med. Unlocked 2020, 20, 100378. [Google Scholar] [CrossRef]
- Jnr, B.A. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J. Med. Syst. 2020, 44, 1–9. [Google Scholar]
- Mohamed Ibrahim, O.; Ibrahim, R.M.; Abdel-Qader, D.H.; Al Meslamani, A.Z.; Al Mazrouei, N. Evaluation of telepharmacy services in light of COVID-19. Telemed. e-Health 2020, 27, 649–656. [Google Scholar] [CrossRef]
- Olayiwola, J.N.; Magaña, C.; Harmon, A.; Nair, S.; Esposito, E.; Harsh, C.; Forrest, L.A.; Wexler, R. Telehealth as a bright spot of the COVID-19 pandemic: Recommendations from the virtual frontlines (“Frontweb”). JMIR Public Health Surveill. 2020, 6, e19045. [Google Scholar] [CrossRef]
- Sasangohar, F.; Dhala, A.; Zheng, F.; Ahmadi, N.; Kash, B.; Masud, F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: An interview study and sentiment analysis. BMJ Qual. Saf. 2020, 67, 274–302. [Google Scholar] [CrossRef]
- Sharma, D.; Bhaskar, S. Addressing the COVID-19 burden on medical education and training: The role of telemedicine and tele-education during and beyond the pandemic. Front. Public Health 2020, 8, 838. [Google Scholar] [CrossRef]
- Singh, R.P.; Javaid, M.; Kataria, R.; Tyagi, M.; Haleem, A.; Suman, R. Significant applications of virtual reality for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 661–664. [Google Scholar] [CrossRef]
- Wang, C.J.; Ng, C.Y.; Brook, R.H. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA 2020, 323, 1341–1342. [Google Scholar] [CrossRef]
- Whitelaw, S.; Mamas, M.A.; Topol, E.; Van Spall, H.G. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit. Health 2020, 2, E435–E440. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef] [Green Version]
- Adeniyi, E.A.; Awotunde, J.B.; Ogundokun, R.O.; Kolawole, P.O.; Abiodun, M.K.; Adeniyi, A.A. Mobile health application and COVID-19: Opportunities and challenges. J. Crit. Rev. 2020, 7, 3481–3488. [Google Scholar]
- Adiukwu, F.; Orsolini, L.; Bytyçi, D.G.; El Hayek, S.; Gonzalez-Diaz, J.M.; Larnaout, A.; Grandinetti, P.; Nofal, M.; Pereira-Sanchez, V.; Da Costa, M.P. COVID-19 mental health care toolkit: An international collaborative effort by Early Career Psychiatrists section. Gen. Psychiatry 2020, 33, e100270. [Google Scholar] [CrossRef] [PubMed]
- ALOmari, M.O.; Jenkins, J. Exploring the Attitudes of Patients towards using the Seha Application (Telehealth) in Saudi Arabia during the Coronavirus Epidemic. ABC J. Adv. Res. 2021, 10, 9–22. [Google Scholar] [CrossRef]
- Babalola, D.; Anayo, M.; Itoya, D.A. Telehealth during COVID-19: Why Sub-Saharan Africa is yet to log-in to virtual healthcare? AIMS Med. Sci. 2021, 8, 46–55. [Google Scholar] [CrossRef]
- Anglemyer, A.; Moore, T.H.; Parker, L.; Chambers, T.; Grady, A.; Chiu, K.; Parry, M.; Wilczynska, M.; Flemyng, E.; Bero, L. Digital contact tracing technologies in epidemics: A rapid review. Cochrane Database Syst. Rev. 2020, 8, CD013699. [Google Scholar]
- Blandford, A.; Wesson, J.; Amalberti, R.; AlHazme, R.; Allwihan, R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob. Health 2020, 8, e1364–e1365. [Google Scholar] [CrossRef]
- WHO World Health Organization: Coronavirus Disease (COVID-19): Weekly Epidemiological Update. Available online: https://www.who.int/ (accessed on 3 June 2022).
- Liu, J. Deployment of IT in China’s Fight against the COVID-19 Pandemic; ITN: London, UK, 2020. [Google Scholar]
- Buoite Stella, A.; Manganotti, P.; Furlanis, G.; Accardo, A.; Ajčević, M. Return to school in the COVID-19 era: Considerations for temperature measurement. J. Med. Eng. Technol. 2020, 44, 468–471. [Google Scholar] [CrossRef]
- Jorfi, M.; Luo, N.M.; Hazra, A.; Herisson, F.; Miller, G.; Toombs, J.A.; Walt, D.R.; Bonato, P.; Ahmad, R. Diagnostic technology for COVID-19: Comparative evaluation of antigen and serology-based SARS-CoV-2 immunoassays, and contact tracing solutions for potential use as at-home products. medRxiv 2020. [Google Scholar] [CrossRef]
- Imai, N.; Dorigatti, I.; Cori, A.; Riley, S.; Ferguson, N. Estimating the Potential Ttal Number of Novel Coronavirus Cases in Wuhan City, China. Available online: https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-01-17-COVID19-Report-1.pdf (accessed on 2 June 2022).
- Thompson, H.; Mousa, A.; Dighe, A.; Fu, H.; Arnedo-Pena, A.; Barrett, P.; Bellido-Blasco, J.; Bi, Q.; Caputi, A.; Chaw, L. Report 38: SARS-CoV-2 setting-specific transmission rates: A systematic review and meta-analysis. Imp. Coll. Lond. 2020, 10, 84270. [Google Scholar]
- Hassounah, M.; Raheel, H.; Alhefzi, M. Digital response during the COVID-19 pandemic in Saudi Arabia. J. Med. Internet Res. 2020, 22, e19338. [Google Scholar] [CrossRef]
- Wymant, C.; Ferretti, L.; Tsallis, D.; Charalambides, M.; Abeler-Dörner, L.; Bonsall, D.; Hinch, R.; Kendall, M.; Milsom, L.; Ayres, M. The epidemiological impact of the NHS COVID-19 App. Nature 2021, 594, 408–412. [Google Scholar] [CrossRef]
- Alanzi, T. A review of mobile applications available in the app and google play stores used during the COVID-19 outbreak. J. Multidiscip. Healthc. 2021, 14, 45. [Google Scholar] [CrossRef]
- Panchal, M.; Singh, S.; Rodriguez-Villegas, E. Analysis of the Factors Affecting the Adoption and Compliance of the NHS COVID-19 Mobile Application. medRxiv 2021. [Google Scholar] [CrossRef]
- Assiri, A.; Al-Tawfiq, J.A.; Alkhalifa, M.; Al Duhailan, H.; Al Qahtani, S.; Dawas, R.A.; El Seoudi, A.A.; Alomran, N.; Omar, O.A.; Alotaibi, N. Launching COVID-19 vaccination in Saudi Arabia: Lessons learned, and the way forward. Travel Med. Infect. Dis. 2021, 43, 102119. [Google Scholar] [CrossRef]
- Mihalj, M.; Carrel, T.; Gregoric, I.D.; Andereggen, L.; Zinn, P.O.; Doll, D.; Stueber, F.; Gabriel, R.A.; Urman, R.D.; Luedi, M.M. Telemedicine for preoperative assessment during a COVID-19 pandemic: Recommendations for clinical care. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 345–351. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Alharbi, A.; Alzuwaed, J.; Qasem, H. Evaluation of e-health (Seha) application: A cross-sectional study in Saudi Arabia. BMC Med. Inform. Decis. Mak. 2021, 21, 103. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alqahtani, J.S.; Althobiani, M.A.; Alghamdi, S.M.; Alanazi, A.F.; Alnaim, N.; Alqarni, A.A.; Alwafi, H. Current Knowledge, Satisfaction, and Use of E-Health Mobile Application (Seha) Among the General Population of Saudi Arabia: A Cross-Sectional Study. J. Multidiscip. Healthc. 2022, 15, 667. [Google Scholar] [CrossRef]
- Kodali, P.B.; Hense, S.; Kopparty, S.; Kalapala, G.R.; Haloi, B. How Indians responded to the Arogya Setu app? Indian J. Public Health 2020, 64, 228. [Google Scholar]
- Zamberg, I.; Manzano, S.; Posfay-Barbe, K.; Windisch, O.; Agoritsas, T.; Schiffer, E. A mobile health platform to disseminate validated institutional measurements during the COVID-19 outbreak: Utilization-focused evaluation study. JMIR Public Health Surveill. 2020, 6, e18668. [Google Scholar] [CrossRef]
- Timmers, T.; Janssen, L.; Stohr, J.; Murk, J.; Berrevoets, M. Using eHealth to support COVID-19 education, self-assessment, and symptom monitoring in the Netherlands: Observational study. JMIR mHealth uHealth 2020, 8, e19822. [Google Scholar] [CrossRef] [PubMed]
- Menni, C.; Valdes, A.M.; Freidin, M.B.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Ganesh, S.; Varsavsky, T.; Cardoso, M.J.; Moustafa, J.S.E.-S. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. 2020, 26, 1037–1040. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, S.M.; Rajah, A.M.A.; Aldabayan, Y.S.; Aldhahir, A.M.; Alqahtani, J.S.; Alzahrani, A.A. Chronic Obstructive Pulmonary Disease Patients’ Acceptance in E-Health Clinical Trials. Int. J. Environ. Res. Public Health 2021, 18, 5230. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.J.; Pak, S.S.; Keller, D.R.; Barnes, D.E. Evaluation of pragmatic telehealth physical therapy implementation during the COVID-19 pandemic. Phys. Ther. 2021, 101, pzaa193. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.H.d.S.; Faustino, L.R.; Oliveira Sobrinho, M.S.d.; Silva, F.B.F. Distance Learning in continued medical training during the pandemic: Feasibility and perceptions. Rev. Bras. Educ. Méd. 2021, 45, e044. [Google Scholar] [CrossRef]
- Schwarz, M.; Scherrer, A.; Hohmann, C.; Heiberg, J.; Brugger, A.; Nuñez-Jimenez, A. COVID-19 and the academy: It is time for going digital. Energy Res. Soc. Sci. 2020, 68, 101684. [Google Scholar] [CrossRef]
- Rose, L.; Yu, L.; Casey, J.; Cook, A.; Metaxa, V.; Pattison, N.; Rafferty, A.M.; Ramsay, P.; Saha, S.; Xyrichis, A. Communication and virtual visiting for families of patients in intensive care during COVID-19: A UK national survey. Ann. Am. Thorac. Soc. 2021, 18, 1685–1692. [Google Scholar] [CrossRef]
- Wong, T.Y.; Bandello, F. Academic ophthalmology during and after the COVID-19 pandemic. Ophthalmology 2020, 127, e51–e52. [Google Scholar] [CrossRef]
- Smits, M.; Staal, J.B.; Van Goor, H. Could Virtual Reality play a role in the rehabilitation after COVID-19 infection? BMJ Open Sport Exerc. Med. 2020, 6, e000943. [Google Scholar] [CrossRef]
- Garcia, L.M.; Birckhead, B.J.; Krishnamurthy, P.; Sackman, J.; Mackey, I.G.; Louis, R.G.; Salmasi, V.; Maddox, T.; Darnall, B.D. An 8-Week Self-Administered at-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J. Med. Internet Res. 2021, 23, e26292. [Google Scholar] [CrossRef]
- Torous, J.; Myrick, K.J.; Rauseo-Ricupero, N.; Firth, J. Digital mental health and COVID-19: Using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment. Health 2020, 7, e18848. [Google Scholar] [CrossRef]
- Chen, Z.-J.; Liang, W.-T.; Liu, Q.; He, R.; Chen, Q.-C.; Li, Q.-F.; Zhang, Y.; Du, X.-D.; Pan, Y.; Liu, S. Use of a Remote Oncology Pharmacy Service Platform for Patients with Cancer during the COVID-19 Pandemic: Implementation and User Acceptance Evaluation. J. Med. Internet Res. 2021, 23, e24619. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 337–339. [Google Scholar] [CrossRef] [PubMed]
- Rahmatizadeh, S.; Valizadeh-Haghi, S.; Dabbagh, A. The role of artificial intelligence in management of critical COVID-19 patients. J. Cell. Mol. Anesth. 2020, 5, 16–22. [Google Scholar]
- Rasheed, J.; Jamil, A.; Hameed, A.A.; Aftab, U.; Aftab, J.; Shah, S.A.; Draheim, D. A survey on artificial intelligence approaches in supporting frontline workers and decision makers for COVID-19 pandemic. Chaos Solitons Fractals 2020, 141, 110337. [Google Scholar] [CrossRef]
- Bachtiger, P.; Peters, N.S.; Walsh, S.L. Machine learning for COVID-19—Asking the right questions. Lancet Digit. Health 2020, 2, e391–e392. [Google Scholar] [CrossRef]
- Kushwaha, S.; Bahl, S.; Bagha, A.K.; Parmar, K.S.; Javaid, M.; Haleem, A.; Singh, R.P. Significant applications of machine learning for COVID-19 pandemic. J. Ind. Integr. Manag. 2020, 5, 453–479. [Google Scholar] [CrossRef]
- Kaxiras, E.; Neofotistos, G.; Angelaki, E. The first 100 days: Modeling the evolution of the COVID-19 pandemic. Chaos Solitons Fractals 2020, 138, 110114. [Google Scholar] [CrossRef]
- Komies, S.; Aldhahir, A.M.; Almehmadi, M.; Alghamdi, S.M.; Alqarni, A.; Oyelade, T.; Alqahtani, J.S. COVID-19 Outcomes in Saudi Arabia and the UK: A Tale of Two Kingdoms. medRxiv 2020. [Google Scholar] [CrossRef]
- Iwendi, C.; Bashir, A.K.; Peshkar, A.; Sujatha, R.; Chatterjee, J.M.; Pasupuleti, S.; Mishra, R.; Pillai, S.; Jo, O. COVID-19 patient health prediction using boosted random forest algorithm. Front. Public Health 2020, 8, 357. [Google Scholar] [CrossRef]
- Tan, C.M.; Owuamalam, C.K.; Ng, P.K. Stay at home, protect the NHS and save lives! Confidence in government moderates the negative effects of staying at home on mental health. Personal. Individ. Differ. 2021, 179, 110948. [Google Scholar] [CrossRef]
- Andreadakis, Z.; Kumar, A.; Román, R.G.; Tollefsen, S.; Saville, M.; Mayhew, S. The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020, 19, 305–306. [Google Scholar]
- Abbasi, J. COVID-19 and mRNA vaccines—First large test for a new approach. JAMA 2020, 324, 1125–1127. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. COVID-19: Moderna vaccine is nearly 95% effective, trial involving high risk and elderly people shows. BMJ Br. Med. J. 2020, 371, m4471. [Google Scholar] [CrossRef]
- Knoll, M.D.; Wonodi, C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet 2021, 397, 72–74. [Google Scholar] [CrossRef]
- Wang, R.; Chen, J.; Gao, K.; Wei, G.-W. Vaccine-escape and fast-growing mutations in the United Kingdom, the United States, Singapore, Spain, India, and other COVID-19-devastated countries. Genomics 2021, 113, 2158–2170. [Google Scholar] [CrossRef]
- Yen, Y.-F.; Tsai, Y.-F.; Su, V.Y.-F.; Chan, S.-Y.; Yu, W.-R.; Ho, H.; Hou, C.-M.; Chen, C.-C.; Woung, L.-C.; Huang, S.-J. Use and cost-effectiveness of a telehealth service at a centralized COVID-19 quarantine center in Taiwan: Cohort study. J. Med. Internet Res. 2020, 22, e22703. [Google Scholar] [CrossRef]
- Baggett, T.P.; Scott, J.A.; Le, M.H.; Shebl, F.M.; Panella, C.; Losina, E.; Flanagan, C.; Gaeta, J.M.; Neilan, A.; Hyle, E.P. Clinical outcomes, costs, and cost-effectiveness of strategies for adults experiencing sheltered homelessness during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2028195. [Google Scholar] [CrossRef]
- Dosaj, A.; Thiyagarajan, D.; Ter Haar, C.; Cheng, J.; George, J.; Wheatley, C.; Ramanathan, A. Rapid implementation of telehealth services during the COVID-19 pandemic. Telemed. e-Health 2021, 27, 116–120. [Google Scholar] [CrossRef]
- Fagherazzi, G.; Goetzinger, C.; Rashid, M.A.; Aguayo, G.A.; Huiart, L. Digital health strategies to fight COVID-19 worldwide: Challenges, recommendations, and a call for papers. J. Med. Internet Res. 2020, 22, e19284. [Google Scholar] [CrossRef]
- Car, J.; Koh, G.C.-H.; Foong, P.S.; Wang, C.J. Video consultations in primary and specialist care during the COVID-19 pandemic and beyond. BMJ 2020, 371, m3945. [Google Scholar] [CrossRef]
- Silsand, L.; Severinsen, G.-H.; Berntsen, G. Preservation of Person-Centered Care Through Videoconferencing for Patient Follow-up During the COVID-19 Pandemic: Case Study of a Multidisciplinary Care Team. JMIR Form. Res. 2021, 5, e25220. [Google Scholar] [CrossRef]
- Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Dorodchi, M.; Valero, M.; Arabnia, H.R. Internet of Things for current COVID-19 and future pandemics: An exploratory study. J. Healthc. Inform. Res. 2020, 4, 325–364. [Google Scholar] [CrossRef]
| App Name | Objective | Target Providers/Patients | Location |
|---|---|---|---|
| Seha | Daily symptoms, online appointments, and health records | Patients, doctors, and healthcare providers | Saudi Arabia [41,42]. |
| Arogya Setu | Daily symptoms and real-time data | Patients | India [43]. |
| HeadToToe | Education and coronavirus-related information and practice | Healthcare providers | Switzerland [44]. |
| Elisabeth Twee Steden Behandelwijer | Daily symptoms, self-assessment, and coronavirus-related information | Policymakers, healthcare providers, and patients | The Netherlands [45]. |
| NHS COVID-19 | Daily symptoms, controlling social distance, test results, and data sharing | Policymakers, healthcare providers, and patients | United Kingdom [46]. |
| Field | Distributions/Uses |
|---|---|
| Doctor training | Support the training of doctors regarding the COVID-19 virus [52]. |
| Pulmonary rehabilitation | Speed up the recovery rate of COVID-19 patients [53]. |
| Physiotherapy | Virtual reality helps physiotherapists to handle cases of rehabilitation therapy more effectively [18]. |
| Managing chronic pain | Support COVID-19 patients with chronic pain to achieve relief [54]. |
| Mental rehabilitation/support | Support people suffering from mental issues, depression, and anxiety [55]. |
| Psychological support | Support patients who are socially isolated, or who have phobias, fear, and any other psychological illnesses [55]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alghamdi, N.S.; Alghamdi, S.M. The Role of Digital Technology in Curbing COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 8287. https://doi.org/10.3390/ijerph19148287
Alghamdi NS, Alghamdi SM. The Role of Digital Technology in Curbing COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(14):8287. https://doi.org/10.3390/ijerph19148287
Chicago/Turabian StyleAlghamdi, Noha S., and Saeed M. Alghamdi. 2022. "The Role of Digital Technology in Curbing COVID-19" International Journal of Environmental Research and Public Health 19, no. 14: 8287. https://doi.org/10.3390/ijerph19148287
APA StyleAlghamdi, N. S., & Alghamdi, S. M. (2022). The Role of Digital Technology in Curbing COVID-19. International Journal of Environmental Research and Public Health, 19(14), 8287. https://doi.org/10.3390/ijerph19148287







