Difference between Minorities and Majorities in the Association between COVID-19-Related Stress and Psychological Distress: A Socio-Ecological Perspective and the Moderating Role of Parenthood
Abstract
1. Introduction
1.1. Socio-Ecological Perspective
1.2. The Palestinian Minority and the Jewish Majority
1.3. Parenthood and Distress
1.4. The Current Study
2. Materials and Methods
2.1. Participants and Data Collection
2.2. Measures
2.2.1. Demographic Information
2.2.2. COVID-19-Related Stress
2.2.3. Depression, Anxiety, and Stress Scale
2.3. Data Analysis
3. Results
3.1. Cohort Description
3.2. The Difference between the Palestinian Minority and the Jewish Majority Regarding the Levels of COVID-19-Related Stress and Psychological Distress Experienced during the Pandemic
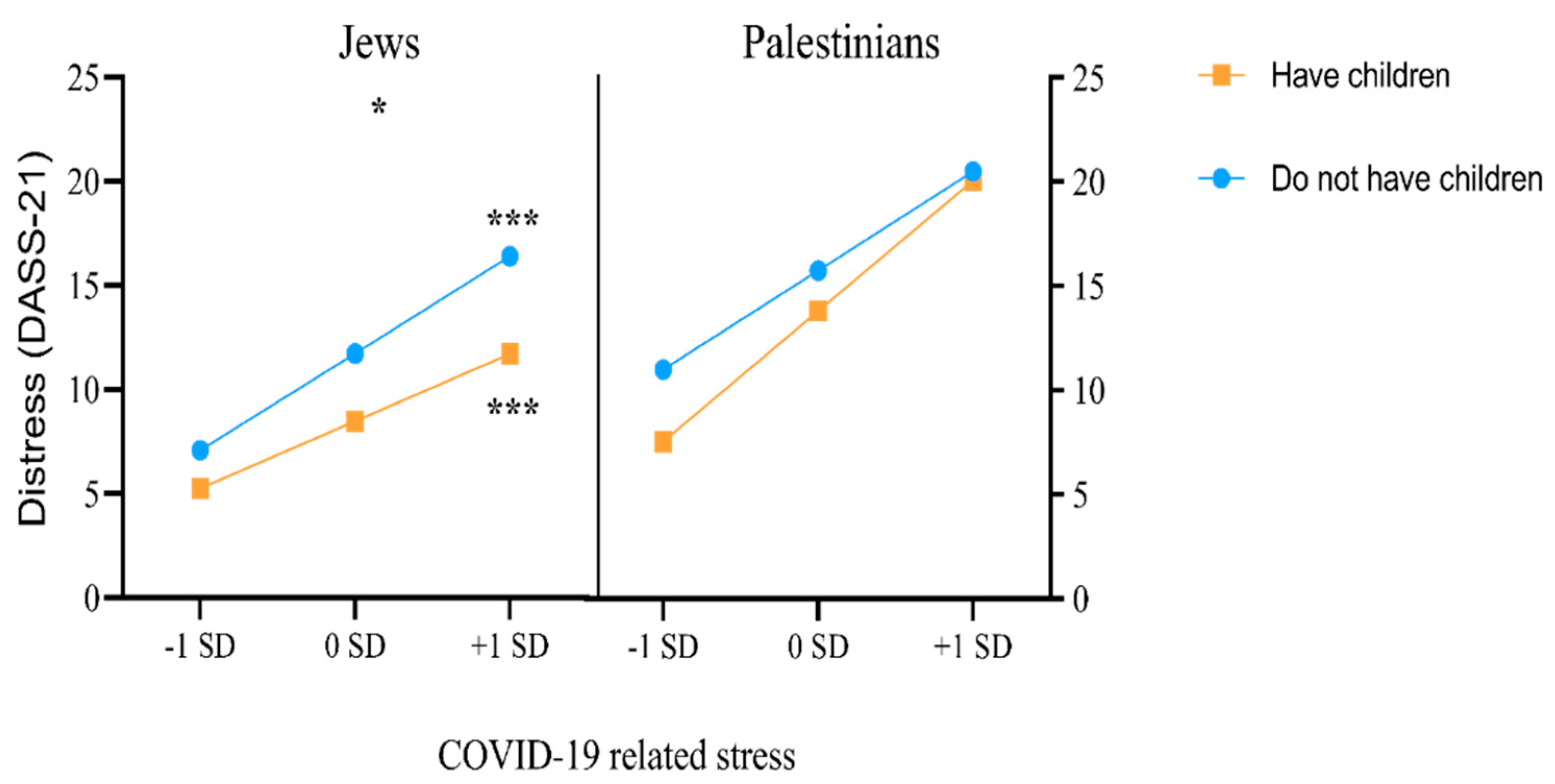
3.3. Parenthood as a Moderator of the Association between COVID-19-Related Stress and Psychological Distress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gori, A.; Topino, E. Across the COVID-19 waves: Assessing temporal fluctuations in perceived stress, post-traumatic symptoms, worry, anxiety and civic moral disengagement over one year of pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5651. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Alon-Tirosh, M.; Hadar-Shoval, D.; Asraf, K.; Tannous-Haddad, L.; Tzischinsky, O. The association between lifestyle changes and psychological distress during COVID-19 lockdown: The moderator effect of COVID-19 stressors. Int. J. Environ. Res. Public Health 2021, 18, 9695. [Google Scholar] [CrossRef]
- Ben-Ezra, M.; Sun, S.; Hou, W.K.; Goodwin, R. The association of being in quarantine and related COVID-19 recommended and non-recommended behaviors with psychological distress in Chinese population. J. Affect. Disord. 2020, 275, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Bonati, M.; Campi, R.; Segre, G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: A systematic review of the evidence. Epidemiol. Psychiatr. Sci. 2022, 31, E27. [Google Scholar] [CrossRef]
- Barzilay, R.; Moore, T.M.; Greenberg, D.M.; DiDomenico, G.E.; Brown, L.A.; White, L.K.; Gur, R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry 2020, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Best, L.A.; Law, M.A.; Roach, S.; Wilbiks, J.M.P. The psychological impact of COVID-19 in Canada: Effects of social isolation during the initial response. In, No Pagination Specified-No Pagination Specified. Can. Psychol. Psychol. Can. 2020, 62, 143–154. [Google Scholar] [CrossRef]
- Coiro, M.J.; Asraf, K.; Tzischinsky, O.; Hadar-Shoval, D.; Tannous-Haddad, L.; Wolfson, A.R. Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and U.S. adults. Sleep Health 2021, 7, 127–133. [Google Scholar] [CrossRef]
- Jin, Y.; Sun, T.; Zheng, P.; An, J. Mass quarantine and mental health during COVID-19: A meta-analysis. J. Affect. Disord. 2021, 295, 1335–1346. [Google Scholar] [CrossRef] [PubMed]
- Alegria, M.; Shrout, P.E.; Canino, G.; Alvarez, K.; Wang, Y.; Bird, H.; Duarte, C. The effect of minority status and social context on the development of depression and anxiety in Puerto Rican descent youth. World Psychiatry 2019, 18, 298–307. [Google Scholar] [CrossRef]
- Atkin, A.L.; Tran, A.G.T.T. The roles of ethnic identity and metastereotype awareness in the racial discrimination-psychological adjustment link for Asian Americans at predominantly White universities. Cult. Divers. Ethn. Minority Psychol. 2020, 26, 498–508. [Google Scholar] [CrossRef]
- Prapas, C.; Mavreas, V. The relationship between quality of life, psychological wellbeing, satisfaction with life and acculturation of immigrants in Greece. Cult. Med. Psychiatry 2019, 43, 77–92. [Google Scholar] [CrossRef]
- Iob, E.; Steptoe, A.; Fancourt, D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry 2020, 217, 543–546. [Google Scholar] [CrossRef]
- Guerrini, C.J.; Schneider, S.C.; Guzick, A.G.; Nwankwo, G.N.A.; Canfield, I.; Fedson, S.; Gutierrez, A.M.; Sheu, J.C.; Song, A.Y.; Villagran, A.M.; et al. Psychological distress among the U.S. general population during the COVID-19 pandemic. Front. Psychiatry 2021, 12, 810. [Google Scholar] [CrossRef]
- Kimhi, S.; Eshel, Y.; Marciano, H.; Adini, B. Distress and resilience in the days of COVID-19: Comparing two ethnicities. Int. J. Environ. Res. Public Health 2020, 17, 3956. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Mikocka-Walus, A.; Stokes, M.; Evans, S.; Olive, L.; Westrupp, E. Finding the power within and without: How can we strengthen resilience against symptoms of stress, anxiety, and depression in Australian parents during the COVID-19 pandemic? J. Psychosom. Res. 2021, 145, 110433. [Google Scholar] [CrossRef]
- Dwairy, M.A. Cross-Cultural Counseling: The Arab-Palestinian Case, 1st ed.; Routledge: London, UK, 1998. [Google Scholar] [CrossRef]
- Haj-Yahia, M. The Palestinian family in Israel: Its collectivist nature, structure, and implications for mental health interventions. In Mental Health and Palestinian Citizens in Israel; Haj-Yahia, M.M., Nakash, O., Levav, I., Eds.; Indiana University Press: Bloomington, IN, USA, 2019; pp. 97–120. [Google Scholar]
- Manna, A. The Nakba and its repercussions on Palestinian citizens in Israel. In Mental Health and Palestinian Citizens in Israel; Haj-Yahia, M.M., Nakash, O., Levav, I., Eds.; Indiana University Press: Bloomington, IN, USA, 2019; pp. 41–49. [Google Scholar]
- Smooha, S. The Arab minority in Israel: Radicalization or politicization? In Israel—State and Society, 1948–1988: Studies in Contemporary Jewry; Medding, P.Y., Ed.; Institute of Contemporary Jewry, Hebrew University of Jerusalem: Jerusalem, Israel; Oxford University Press: Oxford, UK, 1989; Volume 5, pp. 59–88. [Google Scholar]
- Ali, N. Palestinian citizens in Israel: A sociological portrait. In Mental Health and Palestinian Citizens in Israel; Haj-Yahia, M.M., Nakash, O., Levav, I., Eds.; Indiana University Press: Bloomington, IN, USA, 2019; pp. 70–96. [Google Scholar]
- Fuchs, A.; Blander, D.; Kremnitzer, M. Anti-democratic Legislation in the 18th Knesset (2009–2013). Israel Democracy Institute. 2015. Available online: https://www.idi.org.il/media/4058/anti_democratic_legislation.pdf (accessed on 20 July 2020). (In Hebrew).
- Ali-Saleh, O.; Bord, S.; Basis, F. Factors associated with decisions of Arab minority parents in Israel to vaccinate their children against COVID-19. Vaccines 2022, 10, 870. [Google Scholar] [CrossRef]
- Satran, C.; Ali Selah, O.; Mashiach-Aizenberg, M.; Bord, S. Stress and perceived discrimination among Israeli Arabs: The mediation role of threat and trust. Eur. J. Public Health 2021, 31 (Suppl. 3), ckab164-012. [Google Scholar] [CrossRef]
- Abu-Kaf, S.; Nakash, O.; Hayat, T.; Cohen, M. Emotional distress among the Bedouin Arab and Jewish elderly in Israel: The roles of gender, discrimination, and self-esteem. Psychiatry Res. 2020, 291, 113203. [Google Scholar] [CrossRef]
- Chernichovsky, D.; Bisharat, B.; Bowers, L.; Brill, A.; Sharony, C. The health of the Arab Israeli population. In State of the Nation Report; Taub Center for Social Policy Studies in Israel: Jerusalem, Israel, 2017; p. 325. [Google Scholar]
- Dan, O.; David, Y.M.; Abraham, M.; Souval, D. Differences in state anxiety responses to combat pictures between young adult Israeli Jews and Israeli Palestinian Arabs. Psychology 2015, 6, 1136–1143. [Google Scholar] [CrossRef][Green Version]
- Hadar-Shoval, D.; Asraf, K.; Tannous-Haddad, L.; Tzischinsky, O. Adjustment to the COVID-19 pandemic in Israel: Demographics, behavioral and psychological factors. Isr. J. Psychiatry Relat. Sci. 2021, 58, 4–13. [Google Scholar]
- Aruta, J.J.B.R. Socio-ecological determinants of distress in Filipino adults during COVID-19 crisis. Curr. Psychol. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.K.; Kushlev, K.; Lyubomirsky, S. The pains and pleasures of parenting: When, why, and how is parenthood associated with more or less well-being? Psychol. Bull. 2014, 140, 846–895. [Google Scholar] [CrossRef] [PubMed]
- O’leimat, A.S.; Alhussami, M.; Rayan, A. The correlates of psychological distress among parents of children with psychiatric disorders. J. Child Adolesc. Psychiatr. Nurs. 2019, 32, 24–32. [Google Scholar] [CrossRef]
- Carlo, G.; Crockett, L.J.; Streit, C.C.; Cardenas, R. Rural Latino/a youth and parents on the Northern Great Plains: Preliminary findings from the Latino Youth Care Project (LYCP). In Rural Ethnic Minority Youth and Families in the United States, Advancing Responsible Adolescent Development; Crockett, L.J., Carlo, G., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 165–183. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Davies, G.; Caputi, P.; Skarvelis, M.; Ronan, N. The depression anxiety and stress scales: Reference data from a large psychiatric outpatient sample. Aust. J. Psychol. 2015, 67, 97–104. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis; Guilford: New York, NY, USA, 2013. [Google Scholar]
- Gelkopf, M.; Solomon, Z.; Berger, R.; Bleich, A. The mental health impact of terrorism in Israel: A repeat cross-sectional study of Arabs and Jews. Acta Psychiatr. Scand. 2008, 117, 369–380. [Google Scholar] [CrossRef]
- Kimhi, S.; Dror, G.; Stern, S. Resilience among students from the majority and minority Group: The Israeli case. J. Psychol. Behav. Sci. 2017, 5, 37–46. [Google Scholar] [CrossRef]
- Chasson, M.; Taubman-Ben-Ari, O.; Abu-Sharkia, S. Jewish and Arab pregnant women’s psychological distress during the COVID-19 pandemic: The contribution of personal resources. Ethn. Health 2021, 26, 139–151. [Google Scholar] [CrossRef]
- Monache, K.; Milkie, M.A. Parenthood and well-being: A decade in review. J. Marriage Fam. 2020, 82, 198–223. [Google Scholar] [CrossRef]
| Demographic Measures | Full Sample N = 1943 |
|---|---|
| Ethnicity | Palestinian: 28.40% (n = 552) Jewish: 71.59% (n = 1391) |
| Age | M = 40.38, SD = 13.77 |
| Years of education | M = 14.63, SD = 2.50 |
| Gender | Female: 54.86% (n = 1066) Male: 45.13% (n = 877) |
| Residence | Urban: 75.14% (n = 1460) Rural: 24.85% (n = 483) |
| Impact of COVID-19 on employment status | Still working: 62.12% (n = 1207) Not working: 37.87% (n = 736) |
| Impact of COVID-19 on economic status | Income affected: 64.43% (n = 1252) Income not affected: 35.56% (n = 691) |
| Parenthood | Have children: 67.21% (n = 1306) Do not have children: 32.78% (n = 637) |
| Distress (DASS Total) | M = 11.53, SD = 12.53 |
| COVID-19-related stress | M = 32.72, SD = 8.16 |
| Predictor | B | t | CI |
|---|---|---|---|
| Constant | 15.34 | 17.85 *** | 13.71, 16.90 |
| COVID-19-related stress | 0.57 | 16.60 *** | 0.49, 0.66 |
| Parenthood (1 = having children) | −1.30 | −4.04 *** | −1.98, −0.56 |
| Ethnicity (1 = Palestinian) | 2.32 | 7.43 *** | 1.62, 3.01 |
| Age | −0.06 | −3.21 ** | −0.10, −0.03 |
| Gender (1 = female) | 0.33 | 1.36 | −0.14, 0.80 |
| Residence (1 = urban) | −0.35 | −1.26 | −0.95, 0.23 |
| Impact of COVID-19 on employment status (1 = not working) | 0.61 | 2.43 * | 0.11, 1.11 |
| Impact of COVID-19 on economic status (1 = income affected) | 0.59 | 2.33 * | 0.14, 1.05 |
| Parenthood × COVID-19-related stress | 0.002 | 0.08 | −0.08, 0.08 |
| Ethnicity × COVID-19-related stress | 0.09 | 2.83 ** | 0.01, 0.18 |
| Ethnicity × parenthood | 0.32 | 1.10 | −0.33, 1.02 |
| Ethnicity × parenthood × COVID-19-related stress | 0.09 | 2.65 ** | 0.005, 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tannous-Haddad, L.; Hadar-Shoval, D.; Alon-Tirosh, M.; Asraf, K.; Tzischinsky, O. Difference between Minorities and Majorities in the Association between COVID-19-Related Stress and Psychological Distress: A Socio-Ecological Perspective and the Moderating Role of Parenthood. Int. J. Environ. Res. Public Health 2022, 19, 8283. https://doi.org/10.3390/ijerph19148283
Tannous-Haddad L, Hadar-Shoval D, Alon-Tirosh M, Asraf K, Tzischinsky O. Difference between Minorities and Majorities in the Association between COVID-19-Related Stress and Psychological Distress: A Socio-Ecological Perspective and the Moderating Role of Parenthood. International Journal of Environmental Research and Public Health. 2022; 19(14):8283. https://doi.org/10.3390/ijerph19148283
Chicago/Turabian StyleTannous-Haddad, Lubna, Dorit Hadar-Shoval, Michal Alon-Tirosh, Kfir Asraf, and Orna Tzischinsky. 2022. "Difference between Minorities and Majorities in the Association between COVID-19-Related Stress and Psychological Distress: A Socio-Ecological Perspective and the Moderating Role of Parenthood" International Journal of Environmental Research and Public Health 19, no. 14: 8283. https://doi.org/10.3390/ijerph19148283
APA StyleTannous-Haddad, L., Hadar-Shoval, D., Alon-Tirosh, M., Asraf, K., & Tzischinsky, O. (2022). Difference between Minorities and Majorities in the Association between COVID-19-Related Stress and Psychological Distress: A Socio-Ecological Perspective and the Moderating Role of Parenthood. International Journal of Environmental Research and Public Health, 19(14), 8283. https://doi.org/10.3390/ijerph19148283







