Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report
Abstract
:1. Introduction
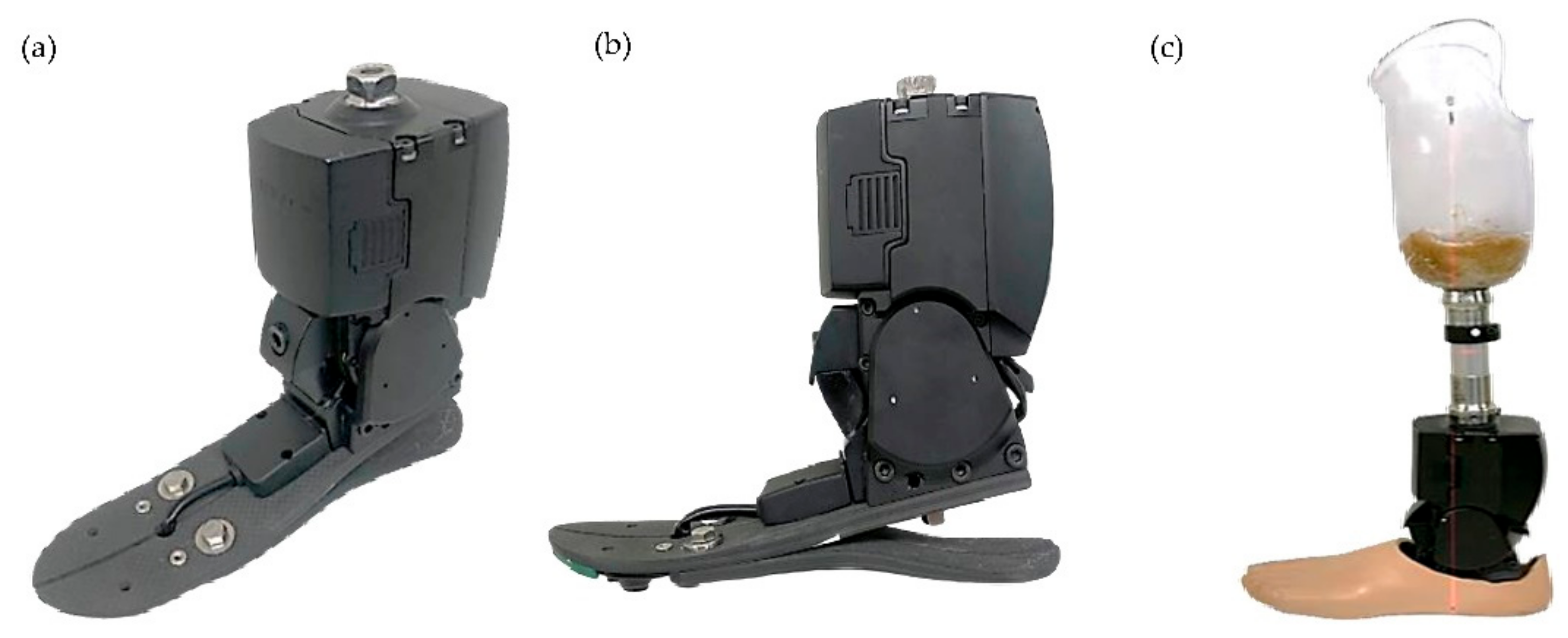
2. Materials and Methods
2.1. History
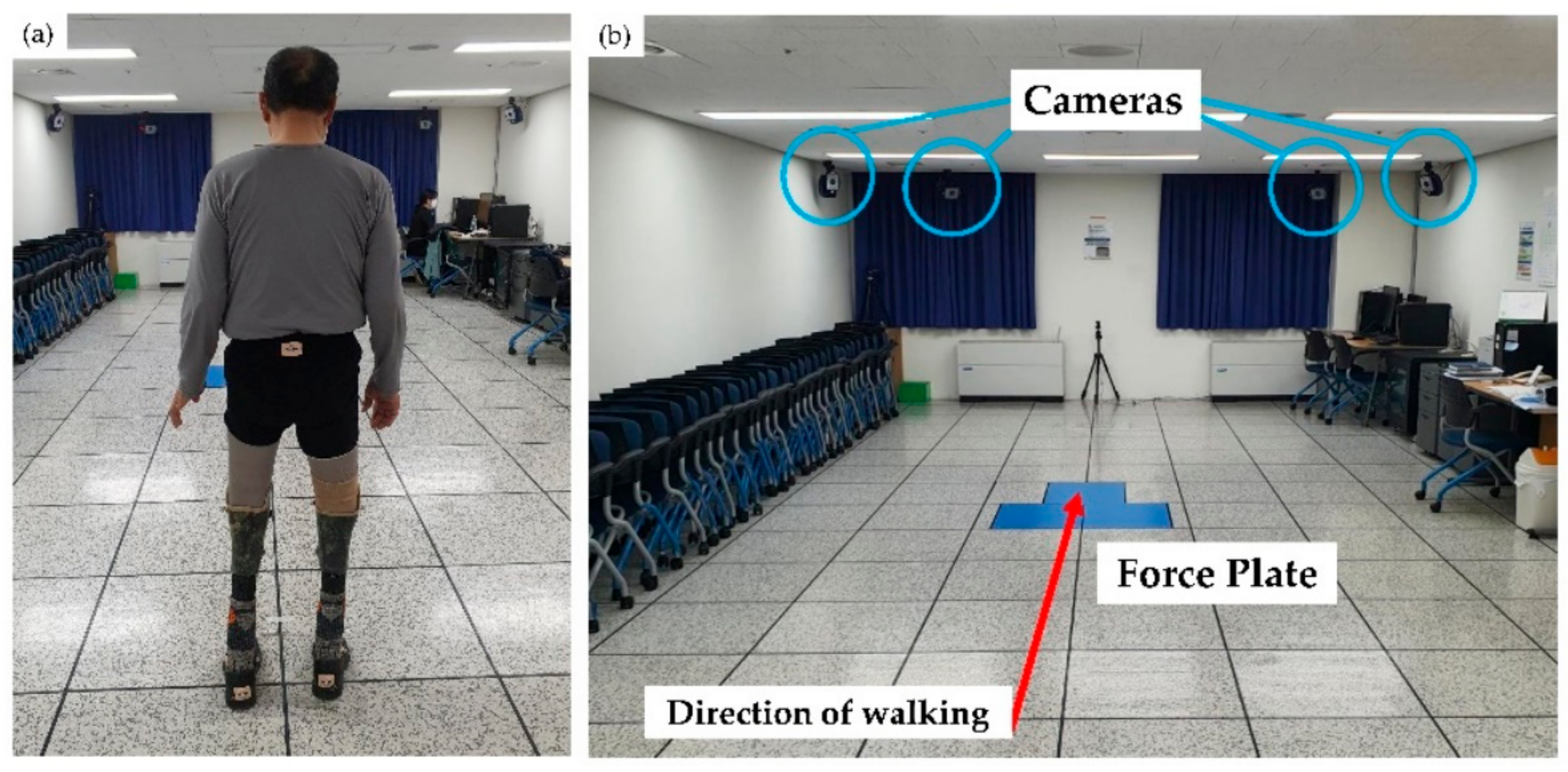
2.2. Methods
3. Results
3.1. Spatiotemporal Parameters
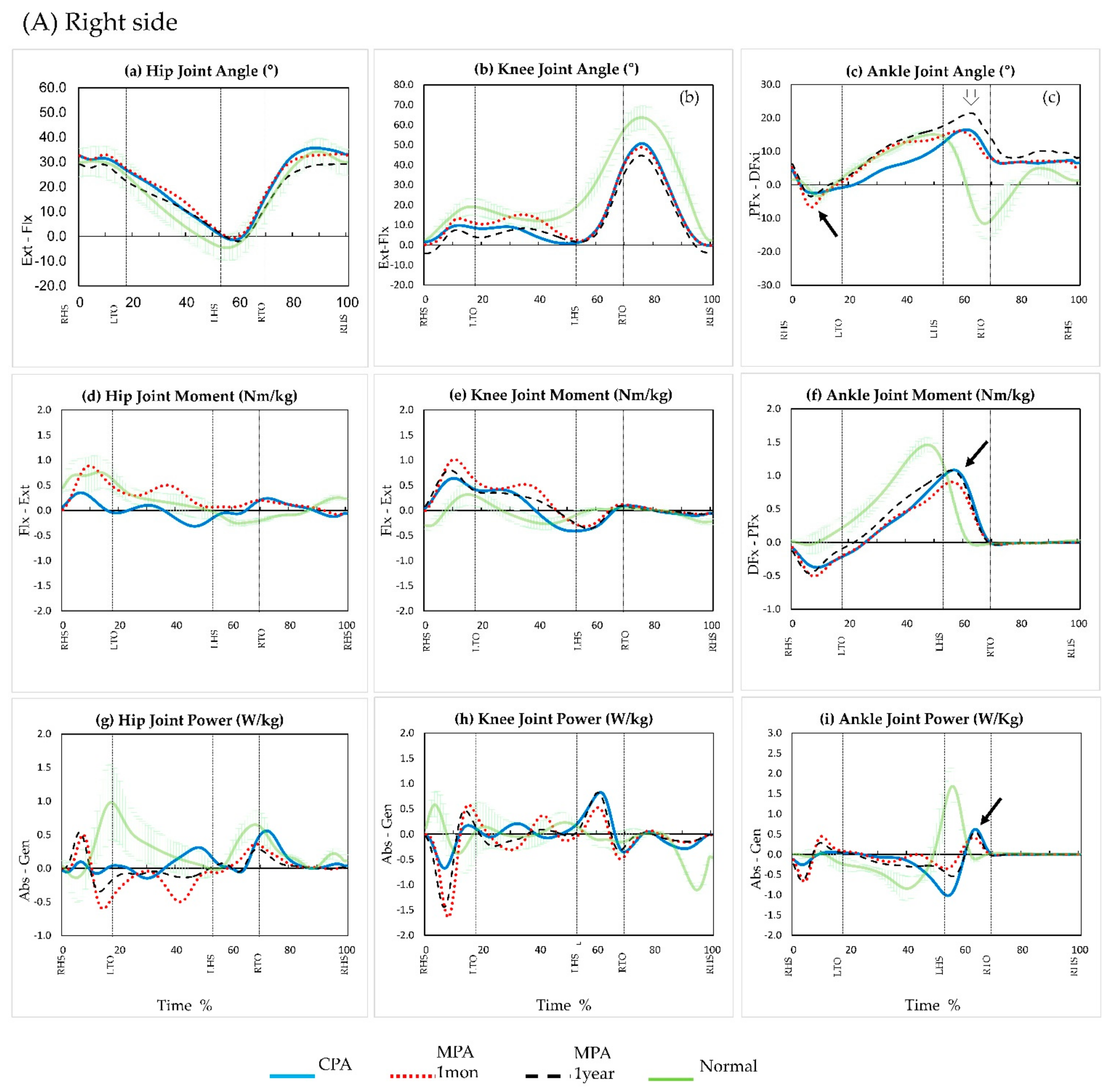
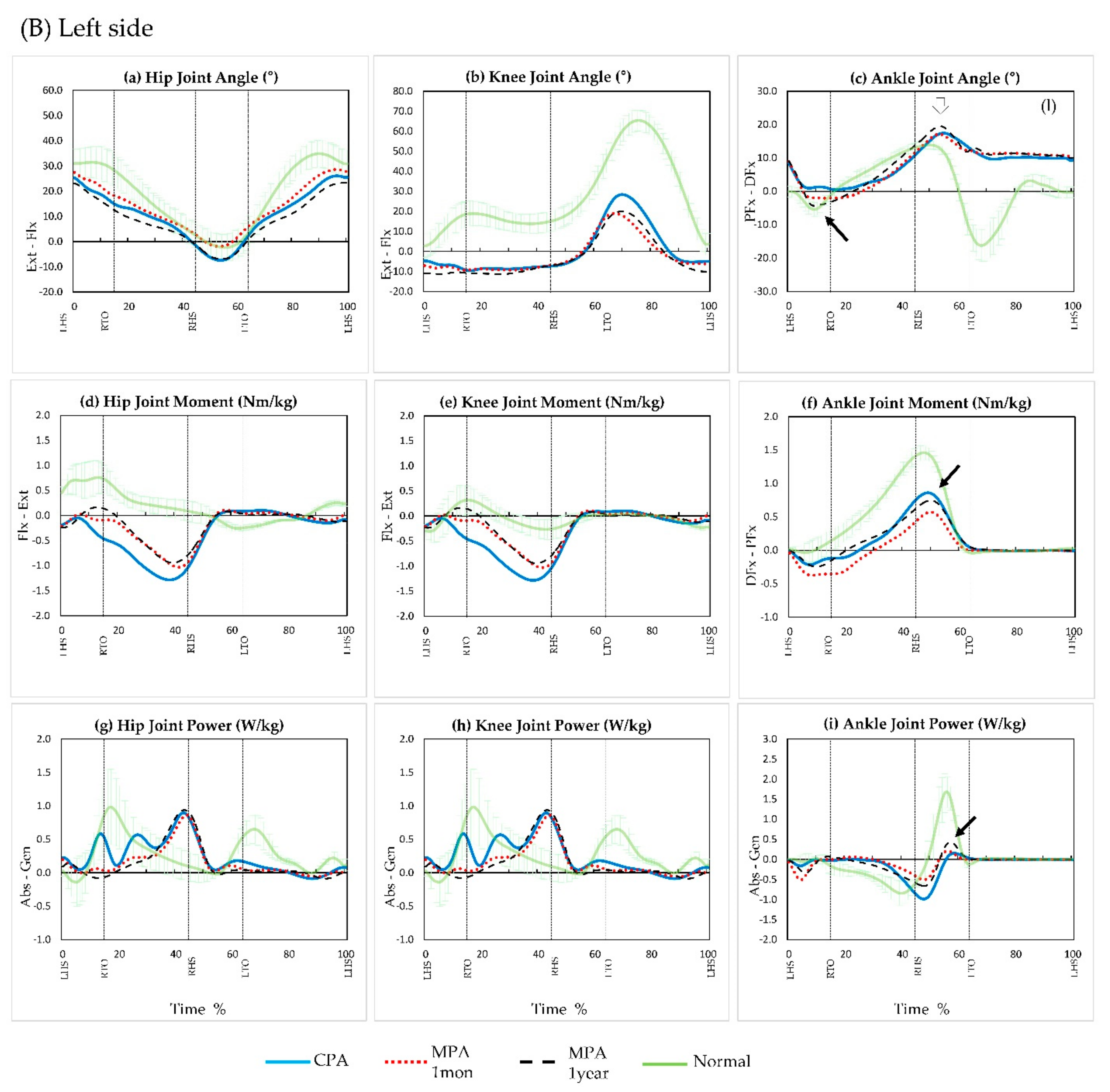
3.2. Kinematic Parameters
3.3. Kinetic Parameters
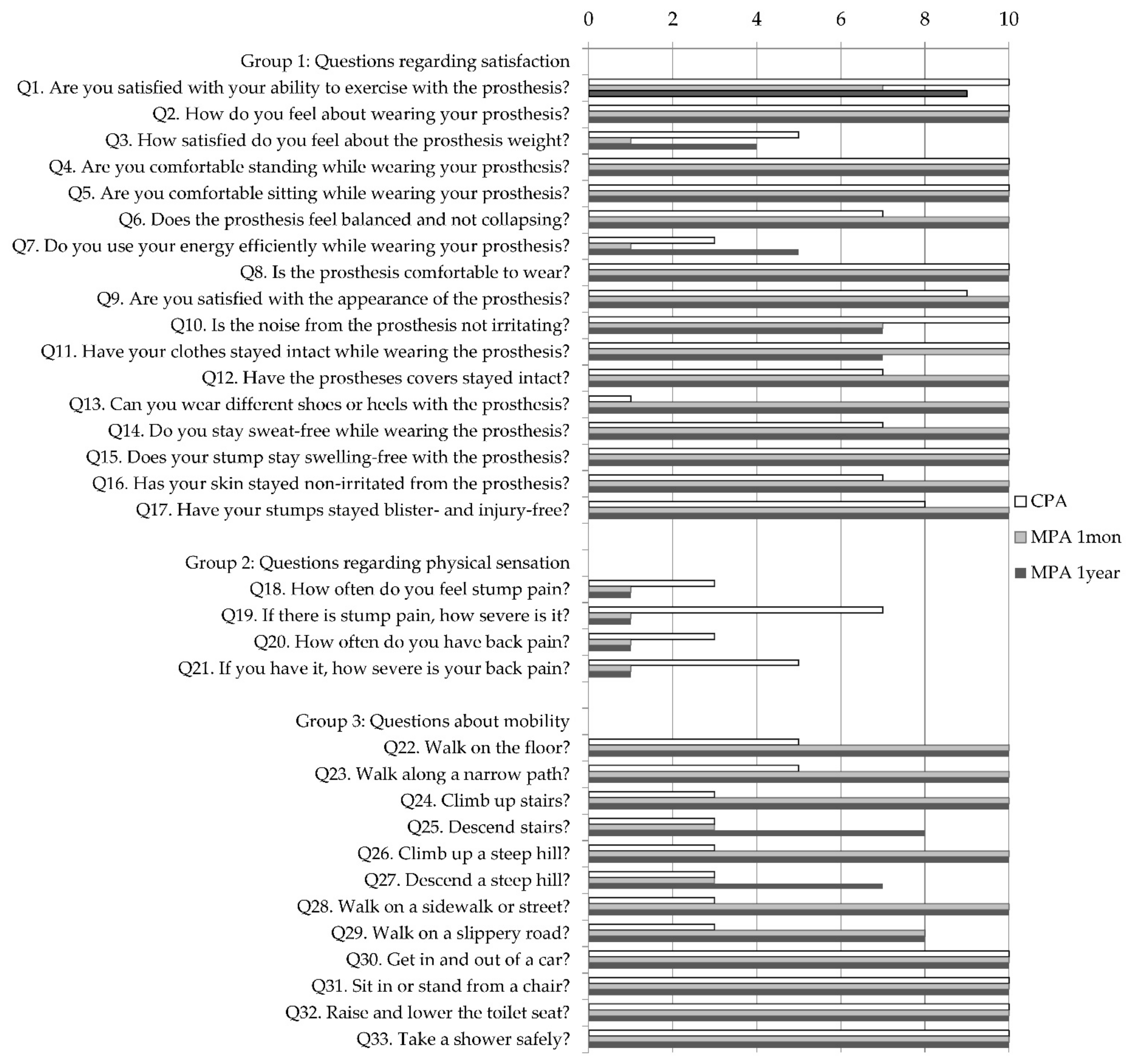
3.4. Questionnaire
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Braddom, R.L. Physical Medicine and Rehabilitation, 4th ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2010. [Google Scholar]
- Shinha, R.; Van Den Heuvel, W.J.A. A systematic literature review of quality of life in lower limb amputees. Disabil. Rehabil. 2011, 33, 883–899. [Google Scholar] [CrossRef] [PubMed]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J. Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. South Med. J. 2002, 95, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Varma, P.; Stineman, M.G.; Dilingham, T.R. Epidemiology of limb loss. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef]
- Hughes, W.; Goodall, R.; Salciccioli, J.D.; Marshall, D.C.; Davies, A.H.; Shalhoub, J. Editor’s Choice—Trends in Lower Extremity Amputation Incidence in European Union 15+ Countries 1990-2017. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Esquenazi, A.; DiGiacomo, R. Rehabiliattion after amputation. J. Am. Podiatr. Med. Assoc. 2001, 91, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Kanata, Y.; Ito, T.; Yoshida, T.; Koyama, T.; Mikami, Y.; Domen, K. Prosthetic walking after bilateral transfemoral amputation in a patient with dilated cardiomyopathy: A case report. Prosthet. Orthot. Int. 2022, 46, 195–198. [Google Scholar] [CrossRef]
- Mohanty, R.K.; Kumar, J.P.; Rout, S.; Das, S.P. Successful prosthetic rehabilitation and gait analysis of individual with bilateral transtibial amputation: A case study with comparison to able-bodied gait. J. Orthop. Trauma Rehabil. 2020, 27, 93–100. [Google Scholar] [CrossRef]
- Agrawal, V.; Gailey, R.S.; Gaunaurd, I.A.; O’Toole, C.; Finnieston, A.; Tolchin, R. Comparison of four different categories of prosthetic feet during ramp ambulation in unilateral transtibial amputees. Prosthet. Orthot. Int. 2015, 39, 380–390. [Google Scholar] [CrossRef]
- Vickers, D.R.; Palk, C.; McIntosh, A.S.; Beatty, K.T. Elderly unilateral transtibial amputee gait on an inclined walkway: A biomechanical analysis. Gait Posture 2008, 27, 518–529. [Google Scholar] [CrossRef]
- Ko, C.Y.; Shin, H.J.; Ryu, J.C.; Kim, K.S. State-of-the-art in microprocessor controlled prostheses for the lower limb amputees. J. Korean Soc. Prosthet. Orthot. 2016, 10, 1–8. [Google Scholar]
- Versluys, R.; Beyl, P.; Van Damme, M.; Desomer, A.; Van Ham, R.; Lefeber, D. Prosthetic feet: State-of-the-art review and the importance of mimicking human ankle–foot biomechanics. Disabil. Rehabil. Assist. Technol. 2009, 4, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Sagawa, Y., Jr.; Turcot, K.; Armand, S.; Thevenon, A.; Vuillerme, N.; Watelain, E. Biomechanics and physiological parame-ters during gait in lower-limb amputees: A systematic review. Gait Posture 2011, 33, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Webster, J.B.; Murphy, D.P. Atlas of Orthoses and Assistive Devices, 5th ed.; Elsevier: Philadelphia, PA, USA, 2019; pp. 69–95. [Google Scholar]
- Agrawal, V.; Gailey, R.S.; Gaunaurd, I.A.; O’Toole, C.; Finnieston, A.A. Comparison between microprocessor-controlled ankle/foot and conventional prosthetic feet during stair negotiation in people with unilateral transtibial amputation. J. Rehabil. Res. Dev. 2013, 50, 941–950. [Google Scholar] [CrossRef]
- Sinitski, E.H.; Hansen, A.H.; Wilken, J.M. Biomechanics of the ankle–foot system during stair ambulation: Implications for design of advanced ankle–foot prostheses. J. Biomech. 2012, 45, 588–594. [Google Scholar] [CrossRef]
- Au, S.K.; Herr, H.; Weber, J.; Martinez-Villalpando, E.C. Powered ankle-foot prosthesis for the improvement of amputee ambulation. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 3020–3026. [Google Scholar]
- Ferris, A.E.; Aldridge, J.M.; Rábago, C.A.; Wilken, J.M. Evaluation of a powered ankle-foot prosthetic system during walking. Arch. Phys. Med. Rehabil. 2012, 93, 1911–1918. [Google Scholar] [CrossRef]
- Thomas-Pohl, M.; Villa, C.; Davot, J.; Bonnet, X.; Facione, J.; Lapeyre, E.; Bascou, J.; Pillet, H. Microprocessor prosthetic ankles: Comparative biomechanical evaluation of people with transtibial traumatic amputation during standing on level ground and slope. Disabil. Rehabil. Assist. Technol. 2021, 16, 17–26. [Google Scholar] [CrossRef]
- Hafner, B.J.; Willingham, L.L.; Buell, N.C.; Allyn, K.J.; Smith, D.G. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch. Phys. Med. Rehabil. 2007, 88, 207–217. [Google Scholar] [CrossRef]
- Collins, T.D.; Ghoussayni, S.N.; Ewins, D.J.; Kent, J.A. A six degrees-of-freedom marker set for gait analysis: Repeatability and comparison with a modified Helen Hayes set. Gait Posture 2009, 30, 173–180. [Google Scholar] [CrossRef]
- Park, S.H.; Yoon, S.H. Validity Evaluation of an Inertial Measurement Unit (IMU) in Gait Analysis Using Statistical Parametric Mapping (SPM). Sensors 2021, 21, 3667. [Google Scholar] [CrossRef]
- Lenzi, T.; Cempini, M.; Newkirk, J.; Hargrove, L.J.; Kuiken, T.A. A lightweight robotic ankle prosthesis with non-backdrivable cam-based transmission. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1142–1147. [Google Scholar]
- Seong, W.S.; Kim, J.H.; Jung, D.H. Development and validity verification of Korean-Prosthesis Evaluation Questionnaire (KPEQ) for amputee’s use of prosthesis. J. Spec. Educ. Rehabil. Sci. 2017, 56, 293–330. [Google Scholar] [CrossRef]
- Su, P.; Gard, S.A.; Lipschutz, R.D.; Kuiken, T.A. Gait characteristics of persons with bilateral transtibial amputations. J. Rehabil. Res. Dev. 2007, 44, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Gitter, A.; Czerniecki, J.; Meinders, M. Effect of prosthetic mass on swing phase work during above knee amputee ambulation. Am. J. Phys. Med. Rehabil. 1997, 76, 114–121. [Google Scholar] [CrossRef]
- Sadeghi, H.; Allard, P.; Duhaime, P. Muscle power compensatory mechanisms in below-knee amputee gait. Am. J. Phys. Med. Rehabil. 2001, 80, 25–32. [Google Scholar] [CrossRef]
- Perry, J.; Burnfield, J.M. Gait Analysis: Normal and Pathological Function, 2nd ed.; Slack Incorporated: Pomona, CA, USA, 2010. [Google Scholar]
- Martin, J.; Pollock, A.; Hettinger, J. Microprocessor Lower Limb Prosthetics: Review of Current State of the Art. J. Prosthet. Orthot. 2010, 22, 183–193. [Google Scholar] [CrossRef]
- Xiu, H.; Han, Y.; Wang, X.; Zhang, Y.; Liang, W.; Wei, G.; Ren, L.; Ren, L. Design, development, and clinical validation of a two degrees of freedom compliant ankle-foot prosthesis based on a 4-4r parallel mechanism. Mech. Mach. Theory. 2022, 172, 104818. [Google Scholar] [CrossRef]
- Au, S.K.; Weber, J.; Herr, H. Biomechanical Design of a Powered Ankle-Foot Prosthesis. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 298–303. [Google Scholar]

| CPA | MPA (1 Mon) | MPA (1 Year) | ||||
|---|---|---|---|---|---|---|
| Right (n = 8) | Left (n = 8) | Right (n = 11) | Left (n = 11) | Right (n = 9) | Left (n = 9) | |
| Spatiotemporal parameters | ||||||
| Forward velocity (cm/s) | 63.27 ± 3.62 | 64.36 ± 2.60 | 57.56 ± 4.40 | 57.05 ± 4.77 | 57.95 ± 6.74 | 58.97 ± 7.00 |
| Cadence (step/min) | 85.07 ± 1.92 | 85.83 ± 1.80 | 78.79 ± 3.18 | 79.11 ± 3.55 | 81.19 ± 3.14 | 82.13 ± 4.22 |
| Step length (cm) | 45.72 ± 3.17 | 43.91 ± 3.30 | 41.71 ± 3.61 | 44.96 ± 2.56 | 44.21 ± 5.04 | 41.25 ± 3.42 |
| Stride length (cm) | 89.96 ± 6.21 | 90.37 ± 4.7 | 86.09 ± 5.75 | 86.71 ± 6.98 | 84.71 ± 7.64 | 86.03 ± 7.52 |
| Step width (cm) | 28.31 ± 1.03 | 28.08 ± 0.99 | 26.93 ± 1.64 | |||
| Stance time (%cycle) | 70.58 ± 1.51 | 68.13 ± 2.45 | 69.95 ± 1.80 | 62.09 ± 1.76 | 70 ± 1.87 | 63.77 ± 1.78 |
| Swing time (%cycle) | 29.42 ± 1.51 | 31.87 ± 2.45 | 30.05 ± 1.80 | 37.91 ± 1.76 | 30 ± 1.87 | 36.23 ± 1.78 |
| Initial double support time (%cycle) | 21.43 ± 1.45 | 16.81 ± 0.91 | 16.83 ± 1.51 | 15.26 ± 1.59 | 16.78 ± 1.64 | 14.75 ± 1.24 |
| Total double support time (%cycle) | 38.71 ± 2.39 | 32.04 ± 3.42 | 33.77 ± 2.53 | |||
| Single support time (%cycle) | 31.87 ± 2.45 | 29.42 ± 1.51 | 37.91 ± 1.76 | 30.05 ± 1.80 | 36.23 ± 1.78 | 30 ± 1.87 |
| Single:Double support time ratio | 31.87:38.71 | 29.42:38.71 | 37.91:32.04 | 30.05:32.04 | 36.23:33.77 | 30.00:33.77 |
| Kinematic parameters | ||||||
| Maximal hip flexion angle (°) | 35.76 ± 1.08 | 26.50 ± 0.87 | 34.03 ± 1.03 | 28.94 ± 1.04 | 30.22 ± 2.16 | 23.86 ± 1.39 |
| Knee flexion angle in stance phase (°) | 10.82 ± 2.50 | - | 15.62 ± 4.06 | - | 9.62 ± 4.46 | - |
| Ankle plantarflexion peak angle at loading response (°) | −2.52 ± 0.56 | 0.48 ± 0.40 | −6.97 ± 0.93 | −2.41 ± 0.49 | −3.96 ± 0.94 | −4.61 ± 0.62 |
| Ankle dorsiflexion peak angle in late stance phase (°) | 16.67 ± 0.92 | 17.63 ± 0.69 | 16.33 ± 0.89 | 17.45 ± 1.58 | 21.84 ± 1.03 | 19.80 ± 1.28 |
| Ankle ROM in stance phase (°) | 19.19 ± 0.93 | 17.15 ± 0.72 | 23.30 ± 1.11 | 19.86 ± 1.51 | 25.79 ± 1.73 | 24.41 ± 1.69 |
| Kinetic parameters | ||||||
| Peak ankle plantarflexion moment in late stance phase (Nm/kg) | 1.09 ± 0.12 | 0.90 ± 0.08 | 0.91 ± 0.09 | 0.58 ± 0.17 | 1.08 ± 0.07 | 0.78 ± 0.13 |
| Peak positive ankle power (W/kg) | 0.67 ± 0.12 | 0.21 ± 0.05 | 0.45 ± 0.10 | 0.25 ± 0.21 | 0.60 ± 0.16 | 0.47 ± 0.23 |
| Symmetry ratios1 | ||||||
| Step length ratio | 1.04 | 0.93 | 1.07 | |||
| Early stance ratio | 1.27 | 1.10 | 1.14 | |||
| Late stance ratio | 0.79 | 0.91 | 0.89 | |||
| Ankle ROM ratio | 1.12 | 1.17 | 1.06 | |||
| Hip flexion ratio | 1.35 | 1.18 | 1.27 | |||
| Ankle plantarflexion moment | 1.21 | 1.56 | 1.40 | |||
| Ankle plantarflexion power | 3.21 | 1.83 | 1.27 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, J.H.; Yang, H.S.; Choi, P.-h.; Ahn, E.J.; Sim, W.S.; Ahn, D.Y.; Kim, J.Y.; Lee, S.B.N.; Jo, M.; Cho, M.H. Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report. Int. J. Environ. Res. Public Health 2022, 19, 8279. https://doi.org/10.3390/ijerph19148279
Jeon JH, Yang HS, Choi P-h, Ahn EJ, Sim WS, Ahn DY, Kim JY, Lee SBN, Jo M, Cho MH. Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report. International Journal of Environmental Research and Public Health. 2022; 19(14):8279. https://doi.org/10.3390/ijerph19148279
Chicago/Turabian StyleJeon, Jong Hu, Hee Seung Yang, Pyoung-hwa Choi, Eui Jin Ahn, Woo Sob Sim, Dong Young Ahn, Jin Yang Kim, Seul Bin Na Lee, Min Jo, and Min Hee Cho. 2022. "Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report" International Journal of Environmental Research and Public Health 19, no. 14: 8279. https://doi.org/10.3390/ijerph19148279
APA StyleJeon, J. H., Yang, H. S., Choi, P.-h., Ahn, E. J., Sim, W. S., Ahn, D. Y., Kim, J. Y., Lee, S. B. N., Jo, M., & Cho, M. H. (2022). Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report. International Journal of Environmental Research and Public Health, 19(14), 8279. https://doi.org/10.3390/ijerph19148279






