Behavioral Patterns of Supply and Demand Sides of Health Services for the Elderly in Sustainable Digital Transformation: A Mixed Methods Study
Abstract
:1. Introduction
2. Literature Review
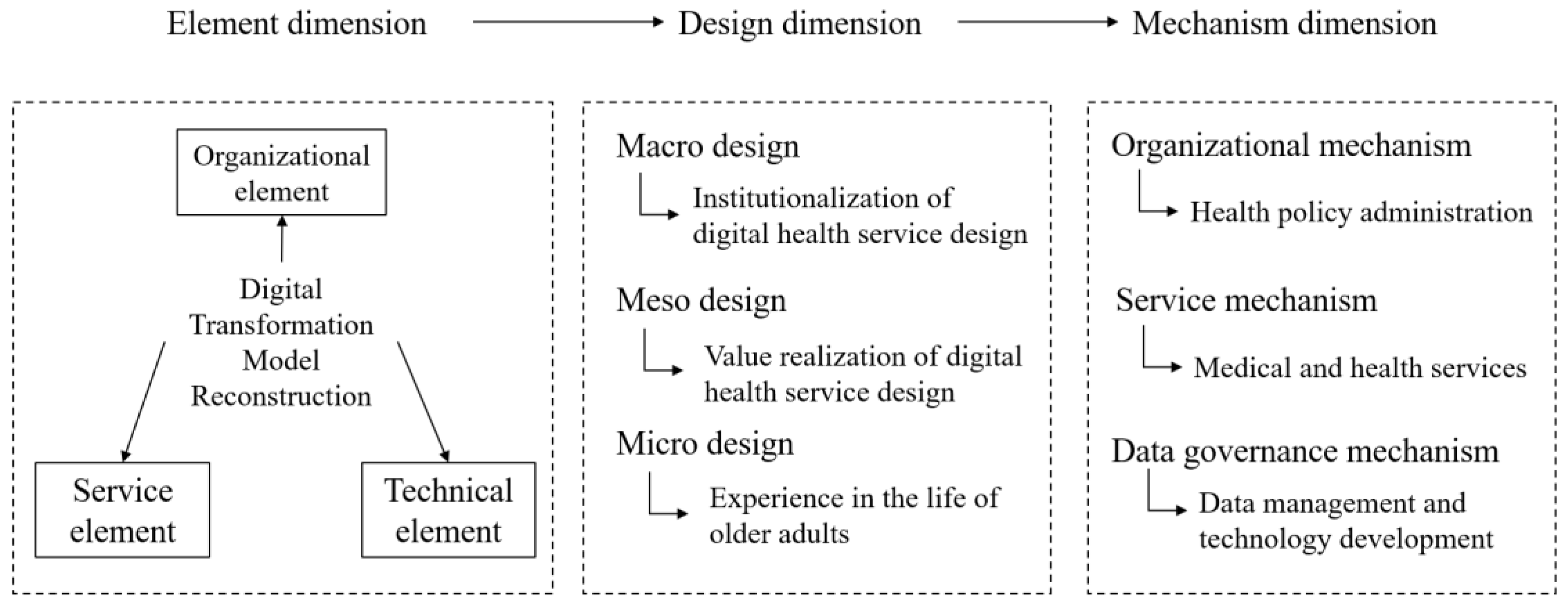
2.1. The Elements of Digital Transformation on Public Services
2.2. The Experience and Service Design Path for the Elderly
2.3. The Operational Mechanism of Digital Transformation in Health Services
3. Materials and Methods
3.1. Participants
3.2. Research Method
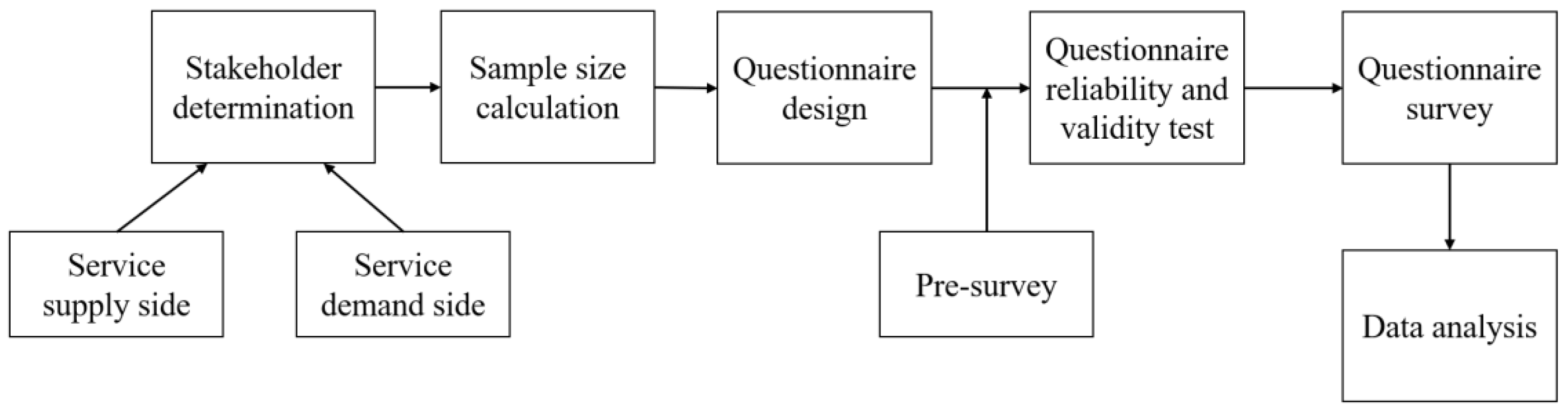
3.3. Quantitative Research Process
3.3.1. Participant Selection
3.3.2. Data Collection Procedures
- Socio-demographic characteristics: including gender, age, living conditions, educational background, and health self-assessment of participants. Self-rated health ranged from 1 (very unhealthy) to 5 (very healthy).
- Perception of digital transformation: it included the perception of organizations, services, and technologies under digital transformation. The items were: Your perception of the transformation of digital services in the organization; Your perception of digital health service projects; Your perception of technology in digital health services.
- Identity of digital transformation: including the identity of the organizations, services, and technologies under digital transformation. The items were: Do you think digital transformation in the organization is effective; Do you think digital transformation in health services is effective; Do you think the application of digital technology is effective.
- Satisfaction with digital transformation: it included satisfaction with organizations, services, and technologies under digital transformation. The items were: You are satisfied with the transformation of digital services in the organization; You are satisfied with the health services in digital transformation; You are satisfied with the application of technology in digital transformation.
3.3.3. Statistical Analysis
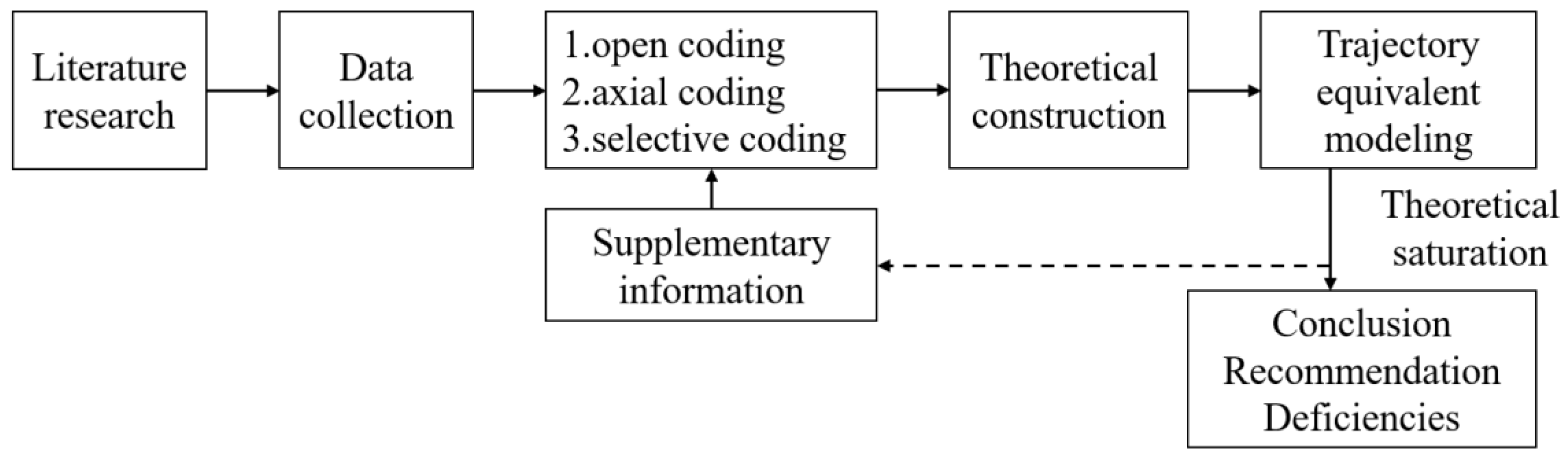
3.4. Qualitative Research Process
3.4.1. Participant Selection
3.4.2. Data Collection Procedures
3.4.3. Data Analysis
- (1)
- Data organization
- (2)
- Data extraction
- (3)
- Data categorization
- (4)
- Grounded theory approach
4. Results
4.1. Participants
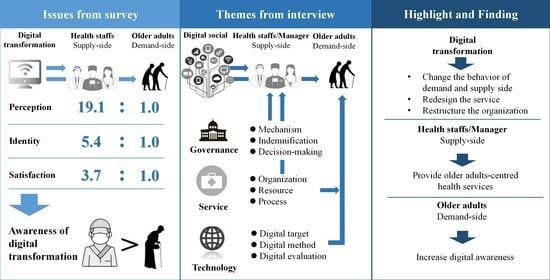
4.2. Differences in Perception, Identity, and Satisfaction under Digital Transformation
4.3. Correlation Analyses of Perception, Identity, and Satisfaction
4.4. Influencing Factors in Perception, Identity, and Satisfaction
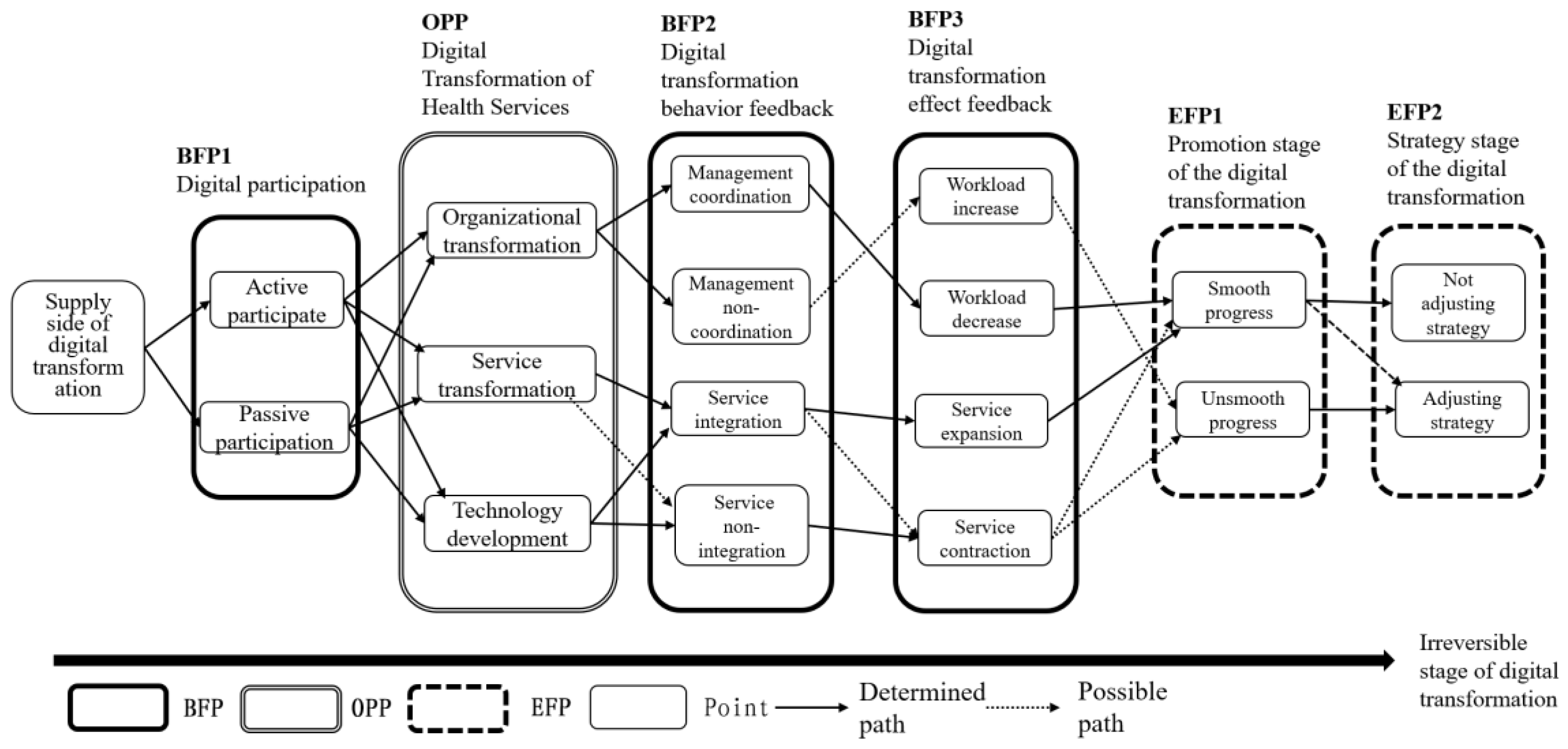
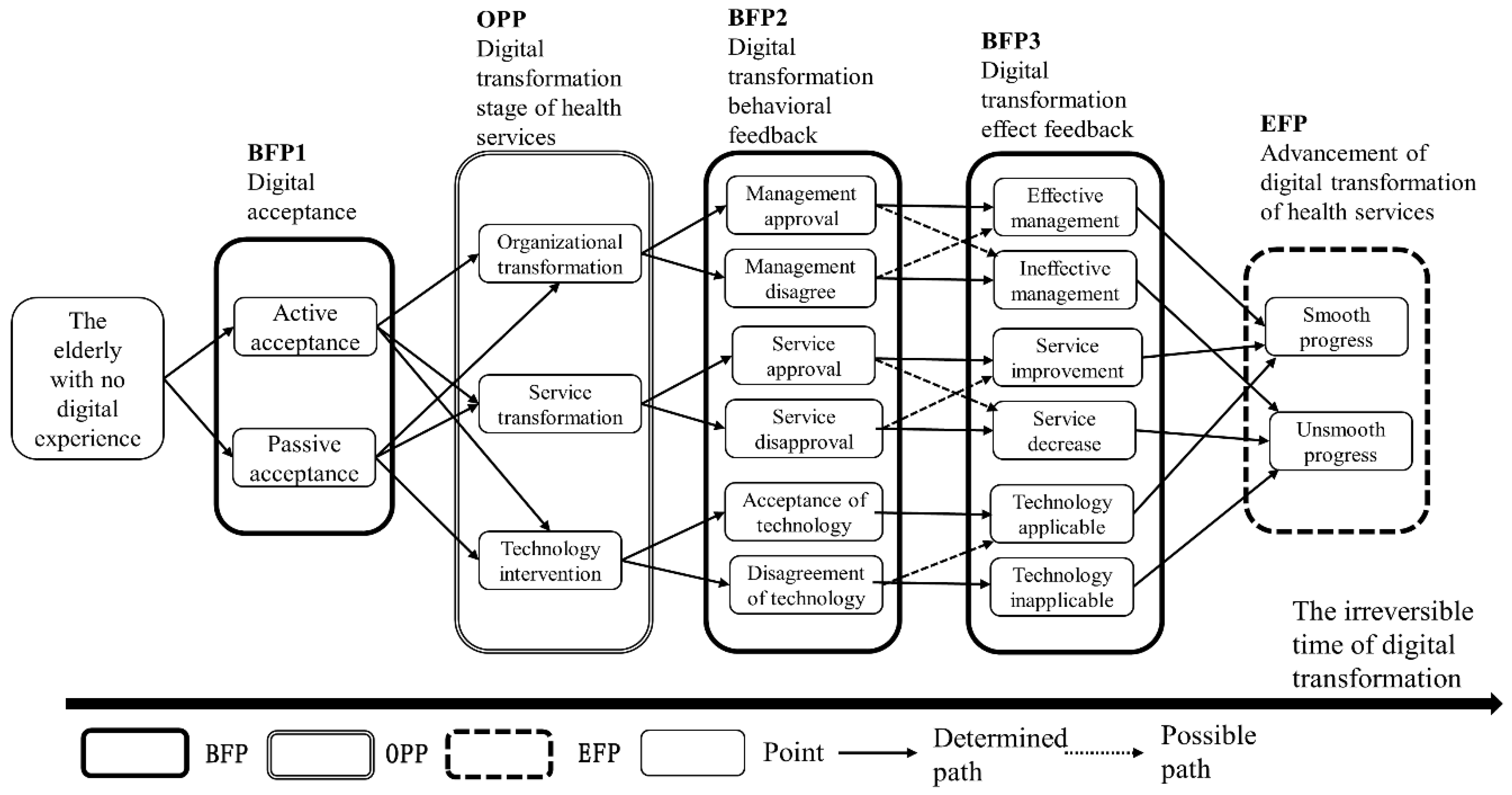
4.5. Qualitative Time Series Analysis
4.6. Open Coding
4.7. Axial Coding
4.8. Selective Coding
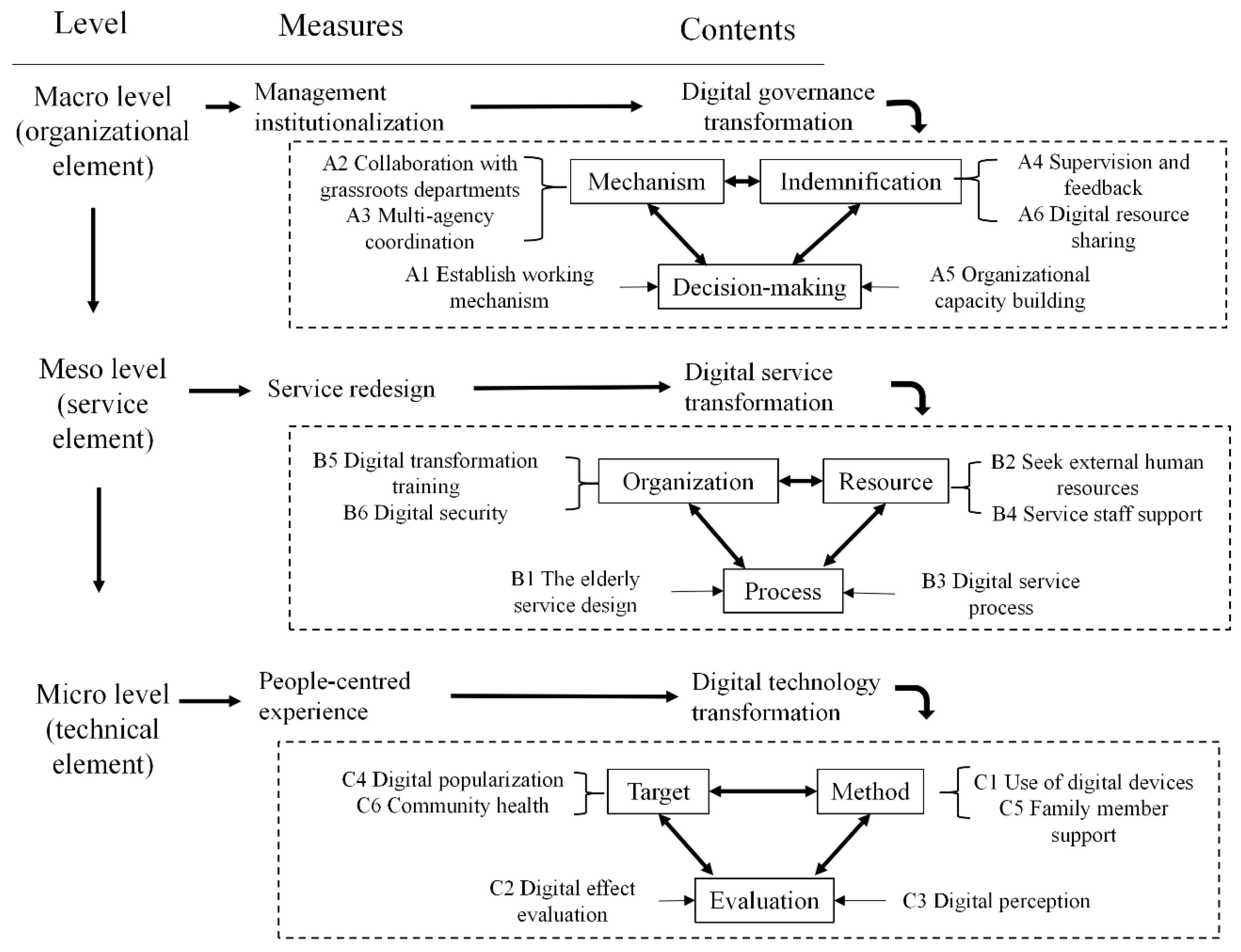
4.9. Digital Transformation Model
5. Discussion
5.1. Digital Governance Transformation
5.2. Digital Service Transformation
5.3. Digital Technology Transformation
- Form an institutionalized decision-making process for management, consolidate the premise and foundation of digital transformation from the organization and security content, and realize governance transformation by relying on the establishment of working mechanisms and organizational capacity building.
- Focus on service redesign, recruit volunteers to help consolidate human resources, and realize the service transformation of aging-appropriate design on the process side.
- Assess the possible effects of the integration of digital technology on the elderly population and obtain feedback to achieve technological transformation through digital device use and family member support.
- Digital transformation should consider irreversible time changes, and it is necessary to track behavioral and effect feedback in the process to design more effective strategies.
5.4. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, J.C.; Henfridsson, O.; Liu, M.J.; Newell, S. Growing on Steroids: Rapidly Scaling the User Base of Digital Ventures Through Digital Innovation. MIS Q. 2017, 41, 301–314. [Google Scholar] [CrossRef]
- Chatfield, A.T.; Reddick, C.G. A framework for Internet of Things-enabled smart government: A case of IoT cybersecurity policies and use cases in U.S. federal government. Gov. Inf. Q. 2019, 36, 346–357. [Google Scholar] [CrossRef]
- Janowski, T. Digital government evolution: From transformation to contextualization. Gov. Inf. Q. 2015, 32, 221–236. [Google Scholar] [CrossRef]
- Lee, J.; Kim, B.J.; Park, S.; Park, S.; Oh, K. Proposing a value-based digital government model: Toward broadening sustainability and public participation. Sustainability 2018, 10, 3078. [Google Scholar] [CrossRef] [Green Version]
- Iyamu, I.; Xu, A.X.; Gómez-Ramírez, O.; Ablona, A.; Chang, H.J.; Mckee, G.; Gilbert, M. Defining Digital Public Health and the Role of Digitization, Digitalization, and Digital Transformation: Scoping Review. JMIR Public Health Surveill. 2021, 7, e30399. [Google Scholar] [CrossRef]
- Wilson, J.; Herron, D.; Nachev, P.; McNally, N.; Williams, B.; Rees, G. The Value of Data: Applying a Public Value Model to the English National Health Service. J. Med. Internet Res. 2020, 22, e15816. [Google Scholar] [CrossRef]
- Fu, L.; Teng, T.; Wang, Y.; He, L. Data Analysis Model Design of Health Service Monitoring System for China’s Elderly Population: The Proposal of the F-W Model Based on the Collaborative Governance Theory of Healthy Aging. Healthcare 2020, 9, 9. [Google Scholar] [CrossRef]
- Andersson, C.; Hallin, A.; Ivory, C. Unpacking the digitalisation of public services: Configuring work during automation in local government. Gov. Inf. Q. 2022, 39, 101662. [Google Scholar] [CrossRef]
- Tomičić Pupek, K.; Pihir, I.; Tomičić Furjan, M. Smart city initiatives in the context of digital transformation–scope, services and technologies. Manag. J. Contemp. Manag. Issues 2019, 24, 39–54. [Google Scholar]
- Henni, S.H.; Maurud, S.; Fuglerud, K.S.; Moen, A. The experiences, needs and barriers of people with impairments related to usability and accessibility of digital health solutions, levels of involvement in the design process and strategies for participatory and universal design: A scoping review. BMC Public Health 2022, 22, 35. [Google Scholar] [CrossRef]
- Aabel, B.; Abeywarna, D. Digital Cross-Channel Usability Heuristics: Improving the Digital Health Experience. J. Usability Stud 2018, 13, 52–72. [Google Scholar]
- Poli, A.; Kelfve, S.; Motel-Klingebiel, A. A research tool for measuring non-participation of older people in research on digital health. BMC Public Health 2019, 19, 1487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cresci, M.K.; Jarosz, P. Bridging the Digital Divide for urban seniors: Community partnership. Geriatr. Nurs. 2010, 31, 455–463. [Google Scholar] [CrossRef]
- Zhang, T.; Liu, J.; Liu, C. Changes in Perceived Accessibility to Healthcare from the Elderly between 2005 and 2014 in China: An Oaxaca-Blinder Decomposition Analysis. Int. J. Environ. Res. Public Health 2019, 16, 3824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, G.; Connolly, R. Mobile health technology adoption across generations: Narrowing the digital divide. Inf. Syst. J. 2018, 28, 995–1019. [Google Scholar] [CrossRef]
- Xie, L.; Yang, H.; Lin, X.; Ti, S.; Wu, Y.; Zhang, S.; Zhang, S.; Zhou, W. Does the Internet Use Improve the Mental Health of Chinese Older Adults? Front. Public Health 2021, 9, 673368. [Google Scholar] [CrossRef]
- He, T.; Huang, C.; Li, M.; Zhou, Y.; Li, S. Social participation of the elderly in China: The roles of conventional media, digital access and social media engagement. Telemat. Inform. 2020, 48, 101347. [Google Scholar] [CrossRef]
- Diener, J.; Rayling, S.; Bezold, J.; Krell-Roesch, J.; Woll, A.; Wunsch, K. Effectiveness and Acceptability of e- and m-Health Interventions to Promote Physical Activity and Prevent Falls in Nursing Homes-A Systematic Review. Front. Physiol. 2022, 13, 894397. [Google Scholar] [CrossRef]
- Auster-Gussman, L.A.; Lockwood, K.G.; Graham, S.A.; Pitter, V.; Branch, O.H. Engagement in Digital Health App-Based Prevention Programs Is Associated With Weight Loss Among Adults Age 65. Front. Digit. Health 2022, 4, 886783. [Google Scholar] [CrossRef]
- Wang, Y.; Song, Y.; Zhu, Y.; Ji, H.; Wang, A. Association of eHealth Literacy with Health Promotion Behaviors of Community-Dwelling Older People: The Chain Mediating Role of Self-Efficacy and Self-Care Ability. Int. J. Environ. Res. Public Health 2022, 19, 6092. [Google Scholar] [CrossRef]
- Kusumota, L.; Diniz, M.; Ribeiro, R.M.; Silva, I.; Figueira, A.; Rodrigues, F.R.; Rodrigues, R. Impact of digital social media on the perception of loneliness and social isolation in older adults. Impacto de mídias sociais digitais na percepção de solidão e no isolamento social em idosos. Rev. Lat.—Am. De Enferm. 2022, 30, e3573. [Google Scholar]
- Mohlman, J.; Tsang, W.; Magee, S.A.; Dalokay, L.; Basch, C. Which Variant of Anxiety Is Associated with Smartphone Expertise in Community Dwelling Older Adults? Clin. Gerontol. 2022, 45, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Low, S.; Sakhardande, P.G.; Lai, Y.F.; Long, A.; Kaur-Gill, S. Attitudes and Perceptions Toward Healthcare Technology Adoption Among Older Adults in Singapore: A Qualitative Study. Front. Public Health 2021, 9, 588590. [Google Scholar] [CrossRef] [PubMed]
- Matt, C.; Hess, T.; Benlian, A. Digital transformation strategies. Bus. Inf. Syst. Eng. 2015, 57, 339–343. [Google Scholar] [CrossRef]
- Alvarenga, A.; Matos, F.; Godina, R.; CO Matias, J. Digital transformation and knowledge management in the public sector. Sustainability 2020, 12, 5824. [Google Scholar] [CrossRef]
- Shi, Y.; Ma, D.; Zhang, J.; Chen, B. In the digital age: A systematic literature review of the e-health literacy and influencing factors among Chinese older adults. Z. Fur Gesundh. 2021, 1–9. [Google Scholar] [CrossRef]
- Shpigelman, C.N.; Tal, A.; Zisman-Ilani, Y. Digital Community Inclusion of Individuals with Serious Mental Illness: A National Survey to Map Digital Technology Use and Community Participation Patterns in the Digital Era. JMIR Ment. Health 2021, 8, e28123. [Google Scholar] [CrossRef]
- Lefler, L.L.; Rhoads, S.J.; Harris, M.; Funderburg, A.E.; Lubin, S.A.; Martel, I.D.; Faulkner, J.L.; Rooker, J.L.; Bell, D.K.; Marshall, H.; et al. Evaluating the Use of Mobile Health Technology in Older Adults with Heart Failure: Mixed-Methods Study. JMIR Aging 2018, 1, e12178. [Google Scholar] [CrossRef]
- Lv, Q.; Jiang, Y.; Qi, J.; Zhang, Y.; Zhang, X.; Fang, L.; Tu, L.; Yang, M.; Liao, Z.; Zhao, M.; et al. Using Mobile Apps for Health Management: A New Health Care Mode in China. JMIR Mhealth Uhealth 2019, 7, e10299. [Google Scholar] [CrossRef]
- Jones, L.S.; Russell, A.J.; Collis, E.; Brosnan, M.J. To What Extent Can Digitally-Mediated Team Communication in Children’s Physical Health and Mental Health Services Bring about Improved Outcomes? A Systematic Review. Child Psychiatry Hum. Dev. 2021, 1–18. [Google Scholar] [CrossRef]
- Nouri, S.S.; Adler-Milstein, J.; Thao, C.; Acharya, P.; Barr-Walker, J.; Sarkar, U.; Lyles, C. Patient characteristics associated with objective measures of digital health tool use in the United States: A literature review. J. Am. Med. Inform. Assoc. 2020, 27, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.; Stevenson, F.; Dack, C.; Pal, K.; May, C.; Michie, S.; Barnard, M.; Murray, E. Developing an implementation strategy for a digital health intervention: An example in routine healthcare. BMC Health Serv. Res. 2018, 18, 794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Luca, V.; Lazic, V.; Birov, S.; Piesche, K.; Beyhan, O.; Pengo, M.F.; Melgara, M.; Sherman, M.H.; Lilja, M.; Balenovic, A.; et al. Digitally Enabled Health Service for the Integrated Management of Hypertension: A Participatory User-Centred Design Process. Int. J. Environ. Res. Public Health 2021, 18, 12442. [Google Scholar] [CrossRef]
- Nigussie, Z.Y.; Zemicheal, N.F.; Tiruneh, G.T.; Bayou, Y.T.; Teklu, G.A.; Kibret, E.S.; Eifler, K.; Hodsdon, S.E.; Altaye, D.E.; Rosenblum, L.; et al. Using mHealth to Improve Timeliness and Quality of Maternal and Newborn Health in the Primary Health Care System in Ethiopia. Glob. Health Sci. Pract. 2021, 9, 668–681. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Segura, M.; Dugarte-Peña, G.; Amescua, A.; Medina-Domínguez, F.; López-Almansa, E.; Reyes, E.B. Smart occupational health and safety for a digital era and its place in smart and sustainable cities. Math. Biosci. Eng. MBE 2021, 18, 8831–8856. [Google Scholar] [CrossRef]
- Stickdorn, M.; Hormess, M.E.; Lawrence, A.; Schneider, J. This Is Service Design Doing: Applying Service Design Thinking in the Real World, 1st ed.; O’Reilly Media, Inc.: Sebastopol, CA, USA, 2018; pp. 124–144. [Google Scholar]
- Jacobson, P.D.; Neumann, P.J. A framework to measure the value of public health services. Health Serv. Res. 2009, 44, 1880–1896. [Google Scholar] [CrossRef] [Green Version]
- Cheng, H.; Lyu, K.; Li, J.; Shiu, H. Bridging the Digital Divide for Rural Older Adults by Family Intergenerational Learning: A Classroom Case in a Rural Primary School in China. Int. J. Environ. Res. Public Health 2021, 19, 371. [Google Scholar] [CrossRef]
- Tam, E.; Boas, P.; Ruaro, F.; Flesch, J.; Wu, J.; Thomas, A.; Li, J.; Lopes, F. Feasibility and Adoption of a Focused Digital Wellness Program in Older Adults. Geriatrics 2021, 6, 54. [Google Scholar] [CrossRef]
- Greer, C.R.; Lusch, R.F.; Vargo, S.L. A service perspective. Key managerial insights from service-dominant (S-D) logic. Organ. Dyn. 2016, 45, 28–38. [Google Scholar] [CrossRef]
- Roe, L.; Galvin, M. Providing inclusive, person-centred care for LGBT+ older adults: A discussion on health and social care design and delivery. J. Nurs. Manag. 2021, 29, 104–108. [Google Scholar] [CrossRef]
- Pérès, K.; Ouvrard, C.; Koleck, M.; Rascle, N.; Dartigues, J.F.; Bergua, V.; Amieva, H. Living in rural area: A protective factor for a negative experience of the lockdown and the COVID-19 crisis in the oldest old population? Int. J. Geriatr. Psychiatry 2021, 36, 1950–1958. [Google Scholar] [CrossRef]
- Walsh, L.; Hyett, N.; Juniper, N.; Li, C.; Rodier, S.; Hill, S. The use of social media as a tool for stakeholder engagement in health service design and quality improvement: A scoping review. Digit. Health 2021, 7, 2055207621996870. [Google Scholar] [CrossRef] [PubMed]
- Barbosa Neves, B.; Franz, R.; Judges, R.; Beermann, C.; Baecker, R. Can Digital Technology Enhance Social Connectedness Among Older Adults? A Feasibility Study. J. Appl. Gerontol. Off. J. South. Gerontol. Soc. 2019, 38, 49–72. [Google Scholar] [CrossRef] [PubMed]
- Castillo de Mesa, J.; Gómez Jacinto, L. Facebook groups as social intervention tools for improving digital skills. Soc. Work. Educ. 2020, 39, 71–84. [Google Scholar] [CrossRef]
- Lu, P.; Shelley, M.; Kong, D. Unmet Community Service Needs and Life Satisfaction Among Chinese Older Adults: A Longitudinal Study. Soc. Work. Public Health 2021, 36, 665–676. [Google Scholar] [CrossRef]
- Barnett, A.; Kelly, J.T.; Wright, C.; Campbell, K.L. Technology-supported models of nutrition care: Perspectives of health service providers. Digit. Health 2022, 8, 20552076221104670. [Google Scholar] [CrossRef]
- Gan, D.; McGillivray, L.; Larsen, M.E.; Christensen, H.; Torok, M. Technology-supported strategies for promoting user engagement with digital mental health interventions: A systematic review. Digit. Health 2022, 8, 20552076221098268. [Google Scholar] [CrossRef]
- Herbert, M.S.; Dochat, C.; Wooldridge, J.S.; Materna, K.; Blanco, B.H.; Tynan, M.; Lee, M.W.; Gasperi, M.; Camodeca, A.; Harris, D.; et al. Technology-supported Acceptance and Commitment Therapy for chronic health conditions: A systematic review and meta-analysis. Behav. Res. Ther. 2022, 148, 103995. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.K.; Bernhardt, J.M.; Dodd, V.; Vollrath, M.W. The digital health divide: Evaluating online health information access and use among older adults. Health Educ. Behav. 2015, 42, 202–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willem, A.; Gemmel, P. Do governance choices matter in health care networks? An exploratory configuration study of health care networks. BMC Health Serv. Res. 2013, 13, 229. [Google Scholar] [CrossRef] [Green Version]
- Krueger, P.M.; Dovel, K.; Denney, J.T. Democracy and self-rated health across 67 countries: A multilevel analysis. Soc. Sci. Med. 2015, 143, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubbio, I.; Bruccoleri, M.; Pietrosi, A.; Ragonese, B. Digital health technology enhances resilient behaviour: Evidence from the ward. Int. J. Oper. Prod. Manag. 2020, 40, 34–67. [Google Scholar] [CrossRef]
- Halminen, O.; Chen, A.; Tenhunen, H.; Lillrank, P. Demonstrating the value of digital health: Guidance on contextual evidence gathering for companies in different stages of maturity. Health Serv. Manag. Res. 2021, 34, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Kayser, L.; Nøhr, C.; Bertelsen, P.S.; Botin, L.; Villumsen, S.; Showell, C.; Turner, P. Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions. Informatics 2018, 5, 41. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Zhang, L.; Wei, M. How Does Smart Healthcare Service Affect Resident Health in the Digital Age? Empirical Evidence From 105 Cities of China. Front. Public Health 2022, 9, 833687. [Google Scholar] [CrossRef]
- Hackett, C.; Brennan, K.; Fowler, H.S.; Leaver, C. Valuing citizen access to digital health services: Applied value-based outcomes in the Canadian context and tools for modernizing health systems. J. Med. Internet Res. 2019, 21, e12277. [Google Scholar] [CrossRef]
- Grossoehme, D.H. Overview of qualitative research. J. Health Care Chaplain. 2014, 20, 109–122. [Google Scholar] [CrossRef]
- Sato, T.; Hidaka, T.; Fukuda, M. Depicting the Dynamics of Living the Life: The Trajectory Equifinality Model, 1st ed.; Valsiner, J., Molenaar, P., Lyra, M., Chaudhary, N., Eds.; Dynamic Process Methodology in the Social and Developmental Sciences; Springer: New York, NY, USA, 2009; pp. 112–150. [Google Scholar]
- Evans, L.; Evans, J.; Pagliari, C.; Källander, K. Exploring the Equity Impact of Current Digital Health Design Practices: Protocol for a Scoping Review. JMIR Res. Protoc. 2022, 11, e34013. [Google Scholar] [CrossRef]
- Huang, B.; Yu, J. Leading Digital Technologies for Coproduction: The Case of “Visit Once” Administrative Service Reform in Zhejiang Province, China. J. Chin. Political Sci. 2019, 24, 513–532. [Google Scholar] [CrossRef]
- Song, Y.; Qian, C.; Pickard, S. Age-Related Digital Divide during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2021, 18, 11285. [Google Scholar] [CrossRef]
- Hong, Y.A.; Zhou, Z.; Fang, Y.; Shi, L. The Digital Divide and Health Disparities in China: Evidence from a National Survey and Policy Implications. J. Med. Internet Res. 2017, 19, e317. [Google Scholar] [CrossRef]
- Kim, S.; Yao, W.; Du, X. Exploring Older Adults’ Adoption and Use of a Tablet Computer During COVID-19: Longitudinal Qualitative Study. JMIR Aging 2022, 5, e32957. [Google Scholar] [CrossRef]
- Han, S.; Nam, S.I. Creating supportive environments and enhancing personal perception to bridge the digital divide among older adults. Educ. Gerontol. 2021, 47, 339–352. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, Z.; Li, X.; Xiaoming, T.; Zhou, Y.; Zhang, X. Factors affecting ICT use in health communication among the older population in Jiangsu, China. Libri 2019, 69, 41–53. [Google Scholar] [CrossRef]
- Andersen, K.N.; Nielsen, J.A.; Kim, S. Use, cost, and digital divide in online public health care: Lessons from Denmark. Transform. Gov. People Process Policy 2019, 13, 197–211. [Google Scholar] [CrossRef]
- Olu, O.; Muneene, D.; Bataringaya, J.E.; Nahimana, M.-R.; Ba, H.; Turgeon, Y.; Karamagi, H.C.; Dovlo, D. How Can Digital Health Technologies Contribute to Sustainable Attainment of Universal Health Coverage in Africa? A Perspective. Front. Public Health 2019, 7, 341. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Zhou, X. Impacts of the internet on perceptions of governance at the community level: The case of Jiangqiao Township in Shanghai, China. Public Adm. Policy Asia-Pac. J. 2021, 24, 165–181. [Google Scholar] [CrossRef]
- Yang, Y. Towards a New Digital Era: Observing Local E-Government Services Adoption in a Chinese Municipality. Future Internet 2017, 9, 53. [Google Scholar] [CrossRef] [Green Version]
- Locsin, R.C.; Soriano, G.P.; Juntasopeepun, P.; Kunaviktikul, W.; Evangelista, L.S. Social transformation and social isolation of older adults: Digital technologies, nursing, healthcare. Collegian 2021, 28, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Castleton, A. Older Adults, Tablets, and Ambivalence: A Grounded Theory Study of a One-Tablet-Per Older Person, Public Program in Uruguay. J. Aging Soc. Policy 2022, 1–22. [Google Scholar] [CrossRef]
- Wang, L.; Wang, Z.; Ma, Q.; Fang, G.; Yang, J. The development and reform of public health in China from 1949 to 2019. Glob. Health 2019, 15, 45. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Zheng, X.; Chen, Z.; Dai, S.; Xu, J.; Ye, H.; Zhang, Z.; Ge, F.; Lei, J. The experience and challenges of healthcare-reform-driven medical consortia and Regional Health Information Technologies in China: A longitudinal study. Int. J. Med. Inform. 2019, 131, 103954. [Google Scholar] [CrossRef] [PubMed]
- Orozco, F.; Guaygua, S.; López Villacis, D.H.; Muñoz, F.; Urquía, M.L. Vinculación de datos administrativos y su utilidad en salud pública: El caso de Ecuador [Administrative data linkage and its usefulness in public health: The case of EcuadorVinculação de dados administrativos e sua utilização em saúde pública: O caso do Equador]. Pan Am. J. Public Health 2021, 45, e9. [Google Scholar]
- Sharma, A.; Harrington, R.A.; McClellan, M.B.; Turakhia, M.P.; Eapen, Z.J.; Steinhubl, S.; Mault, J.R.; Majmudar, M.D.; Roessig, L.; Chandross, K.J.; et al. Using Digital Health Technology to Better Generate Evidence and Deliver Evidence-Based Care. J. Am. Coll. Cardiol. 2018, 71, 2680–2690. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.G.; Croskerry, P.; Petrie, D.A. Cognitive bias in health leaders. Healthc. Manag. Forum 2017, 30, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Keen, J. Digital health care: Cementing centralisation? Health Inform. J. 2014, 20, 168–175. [Google Scholar] [CrossRef]
- Feroz, A.S.; Khoja, A.; Saleem, S. Equipping community health workers with digital tools for pandemic response in LMICs. Arch. Public Health 2021, 79, 1. [Google Scholar] [CrossRef]
- Schütz, N.; Saner, H.; Botros, A.; Buluschek, P.; Urwyler, P.; Müri, R.M.; Nef, T. Wearable Based Calibration of Contactless In-home Motion Sensors for Physical Activity Monitoring in Community-Dwelling Older Adults. Front. Digit. Health 2021, 2, 566595. [Google Scholar] [CrossRef]
- Fredriksen, E.; Thygesen, E.; Moe, C.E.; Martinez, S. Digitalisation of municipal healthcare collaboration with volunteers: A case study applying normalization process theory. BMC Health Serv. Res. 2021, 21, 410. [Google Scholar] [CrossRef]
- Fregnan, E.; Ivaldi, S.; Scaratti, G. HRM 4.0 and New Managerial Competences Profile: The COMAU Case. Front. Psychol. 2020, 11, 578251. [Google Scholar] [CrossRef]
- Cristiano, A.; Musteata, S.; De Silvestri, S.; Bellandi, V.; Ceravolo, P.; Cesari, M.; Azzolino, D.; Sanna, A.; Trojaniello, D. Older Adults’ and Clinicians’ Perspectives on a Smart Health Platform for the Aging Population: Design and Evaluation Study. JMIR Aging 2022, 5, e29623. [Google Scholar] [CrossRef] [PubMed]
- Seifert, A.; Charness, N. Digital transformation of everyday lives of older Swiss adults: Use of and attitudes toward current and future digital services. Eur. J. Ageing 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Portz, J.D.; Ford, K.L.; Doyon, K.; Bekelman, D.B.; Boxer, R.S.; Kutner, J.S.; Czaja, S.; Bull, S. Using Grounded Theory to Inform the Human-Centered Design of Digital Health in Geriatric Palliative Care. J. Pain Symptom Manag. 2020, 60, 1181–1192.e1. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, V. The Big Picture on the “AI Turn” for Digital Health: The Internet of Things and Cyber-Physical Systems. Omics A J. Integr. Biol. 2019, 23, 308–311. [Google Scholar] [CrossRef] [Green Version]
- van der Vaart, R.; van Driel, D.; Pronk, K.; Paulussen, S.; Te Boekhorst, S.; Rosmalen, J.; Evers, A. The Role of Age, Education, and Digital Health Literacy in the Usability of Internet-Based Cognitive Behavioral Therapy for Chronic Pain: Mixed Methods Study. JMIR Form. Res. 2019, 3, e12883. [Google Scholar] [CrossRef]
- Sorkin, D.H.; Janio, E.A.; Eikey, E.V.; Schneider, M.; Davis, K.; Schueller, S.M.; Stadnick, N.A.; Zheng, K.; Neary, M.; Safani, D.; et al. Rise in Use of Digital Mental Health Tools and Technologies in the United States During the COVID-19 Pandemic: Survey Study. J. Med. Internet Res. 2021, 23, e26994. [Google Scholar] [CrossRef]
- Mahajan, S.; Lu, Y.; Spatz, E.S.; Nasir, K.; Krumholz, H.M. Trends and Predictors of Use of Digital Health Technology in the United States. Am. J. Med. 2021, 134, 129–134. [Google Scholar] [CrossRef]
- Arai, S.; Fukase, Y.; Okii, A.; Suzukamo, Y.; Suga, T. Selection process for botulinum toxin injections in patients with chronic-stage hemiplegic stroke: A qualitative study. BMC Med. Inform. Decis. Mak. 2019, 19, 280. [Google Scholar] [CrossRef]
- Seifert, A.; Schelling, H.R. Old and offline? Findings on the use of the Internet by people aged 65 years and older in Switzerland. Z. Fur Gerontol. Und Geriatr. 2016, 49, 619–625. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.K.; Choi, M. Older adults’ willingness to share their personal and health information when adopting healthcare technology and services. Int. J. Med. Inform. 2019, 126, 86–94. [Google Scholar] [CrossRef]
- Baik, D.; Willems, E. Use of Digital Health Technology for Seeking Health Information Among Older Family Caregivers. Stud. Health Technol. Inform. 2022, 290, 997–999. [Google Scholar] [PubMed]
| Item | 1 | 2 | 3 |
|---|---|---|---|
| Perception of organization | 0.706 | ||
| Perception of service | 0.682 | ||
| Perception of technology | 0.677 | ||
| Identity of organization | 0.676 | ||
| Identity of service | 0.663 | ||
| Identity of technology | 0.641 | ||
| Satisfaction of organization | 0.586 | ||
| Satisfaction of service | 0.570 | ||
| Satisfaction of technology | 0.522 |
| Items | Perception | p | Identity | p | Satisfaction | p |
|---|---|---|---|---|---|---|
| Supply or demand side | <0.01 | <0.01 | <0.01 | |||
| Supply side | 3.8 ± 0.4 | 3.7 ± 0.4 | 3.7 ± 0.4 | |||
| Demand side | 3.1 ± 0.4 | 3.3 ± 0.5 | 3.4 ± 0.4 | |||
| Gender | 0.58 | 0.26 | 0.64 | |||
| Male | 3.5 ± 0.5 | 3.5 ± 0.6 | 3.5 ± 0.5 | |||
| Female | 3.4 ± 0.5 | 3.5 ± 0.5 | 3.4 ± 0.5 | |||
| Age | <0.01 | <0.01 | <0.01 | |||
| <40 | 4.0 ± 0.2 | 3.8 ± 0.3 | 3.8 ± 0.3 | |||
| 40–59 | 3.7 ± 0.4 | 3.6 ± 0.4 | 3.5 ± 0.6 | |||
| ≥60 | 3.2 ± 0.4 | 3.3 ± 0.5 | 3.4 ± 0.5 | |||
| Residence | 0.04 | 0.62 | 0.05 | |||
| Living with partner | 3.4 ± 0.5 | 3.5 ± 0.4 | 3.5 ± 0.4 | |||
| Living with children | 3.7 ± 0.5 | 3.6 ± 0.5 | 3.7 ± 0.4 | |||
| Living alone | 3.2 ± 0.4 | 3.4 ± 0.5 | 3.2 ± 0.4 | |||
| Education | <0.01 | 0.01 | 0.02 | |||
| Primary and below | 3.3 ± 0.4 | 3.4 ± 0.5 | 3.3 ± 0.4 | |||
| Junior | 3.2 ± 0.3 | 3.3 ± 0.4 | 3.4 ± 0.5 | |||
| High | 3.3 ± 0.5 | 3.4 ± 0.6 | 3.4 ± 0.5 | |||
| University and above | 3.8 ± 0.4 | 3.7 ± 0.4 | 3.7 ± 0.4 | |||
| Self-rated health | 0.13 | <0.01 | 0.03 | |||
| Healthy | 3.2 ± 0.5 | 3.3 ± 0.6 | 3.4 ± 0.4 | |||
| Unhealthy | 3.5 ± 0.5 | 3.6 ± 0.5 | 3.5 ± 0.5 |
| Supply Side | Demand Side | ||||||
|---|---|---|---|---|---|---|---|
| Perception | Identity | Satisfaction | Perception | Identity | Satisfaction | ||
| Perception | 1 | Perception | 1 | ||||
| Identity | 0.24 | 1 | Identity | 0.69 ** | 1 | ||
| Satisfaction | 0.48 ** | 0.37 ** | 1 | Satisfaction | 0.64 ** | 0.56 ** | 1 |
| Perception OR (95%CI) | p | Identity OR (95%CI) | p | Satisfaction OR (95%CI) | p | |
|---|---|---|---|---|---|---|
| Supply or demand side | ||||||
| Supply side | 1 | 1 | 1 | |||
| Demand side | 19.1 (8.7–45.1) | <0.01 | 5.4 (2.6–10.9) | <0.01 | 3.7 (1.8–7.2) | <0.01 |
| Age | ||||||
| ≥60 | 1 | 1 | 1 | |||
| 40–59 | 10.4 (4.2–25.1) | <0.01 | 3.9 (1.7–8.9) | <0.01 | 1.9 (0.8–4.2) | 0.09 |
| <40 | 116 (14.7–909.5) | <0.01 | 8.6 (3.0–24.7) | <0.01 | 11.2 (3.6–34.9) | <0.01 |
| Residence | ||||||
| Living alone | 1 | 1 | 1 | |||
| Living with partner | 3.2 (0.3–30.2) | 0.08 | 1.6 (0.2–10.2) | 0.06 | 3.7 (0.4–34.1) | 0.24 |
| Living with children | 8.8 (0.7–99.2) | 0.29 | 2.5 (0.3–19.5) | 0.38 | 12 (1.1–141.3) | 0.04 |
| Education | ||||||
| Primary and below | 1 | 1 | 1 | |||
| Junior | 0.4 (0.1–1.5) | 0.85 | 0.6 (0.2–1.7) | 0.36 | 1.2 (0.4–3.7) | 0.66 |
| High | 0.9 (0.3–2.5) | 0.19 | 0.8 (0.3–2.2) | 0.74 | 1.1 (0.4–2.9) | 0.88 |
| University and above | 8.2 (2.9–22.8) | <0.01 | 3.1 (1.2–7.9) | 0.02 | 4.1 (1.5–10.6) | <0.01 |
| Self-rated health | ||||||
| Healthy | 1 | 1 | 1 | |||
| Unhealthy | 3.9 (1.7–8.8) | <0.01 | 2.3 (1.1–4.7) | 0.02 | 0.6 (0.3–1.2) | 0.15 |
| No. | Job | Gender | Age | Working Years |
|---|---|---|---|---|
| 1 | Community manager | Female | 40 | 10 |
| 2 | Community manager | Female | 28 | 5 |
| 3 | Community manager | Female | 55 | 36 |
| 4 | Community manager | Female | 42 | 14 |
| 5 | Community manager | Male | 30 | 6 |
| 6 | Family doctor | Male | 45 | 18 |
| 7 | Family doctor | Female | 40 | 16 |
| 8 | Family doctor | Male | 36 | 8 |
| 9 | Family doctor | Female | 52 | 26 |
| 10 | Family doctor | Female | 47 | 23 |
| 11 | Service personnel | Male | 44 | 6 |
| 12 | Service personnel | Female | 32 | 2 |
| 13 | Service personnel | Female | 56 | 6 |
| 14 | Volunteer | Female | 56 | 6 |
| 15 | Volunteer | Female | 55 | 5 |
| 16 | Volunteer | Female | 50 | 2 |
| 17 | IT developer | Male | 27 | 5 |
| 18 | IT developer | Male | 34 | 8 |
| 19 | IT developer | Male | 30 | 6 |
| 20 | IT developer | Male | 30 | 5 |
| No. | Gender | Age | Years of Residence | Utilization of Digital Health Services |
|---|---|---|---|---|
| 1 | Male | 62 | 22 | Telehealth, Electronic health monitoring |
| 2 | Female | 63 | 14 | Online health consultation |
| 3 | Male | 82 | 34 | Wearable devices, Online health consultation |
| 4 | Female | 71 | 28 | Telehealth |
| 5 | Female | 72 | 22 | Telehealth, Wearable devices |
| 6 | Female | 73 | 28 | Online health consultation |
| 7 | Female | 62 | 6 | Online health consultation |
| 8 | Male | 82 | 32 | Telehealth |
| 9 | Male | 77 | 24 | Medication reminder, Online health education |
| 10 | Female | 72 | 25 | Online health consultation |
| 11 | Female | 78 | 15 | Wearable devices, Electronic health monitoring |
| 12 | Female | 67 | 26 | Online health education |
| 13 | Male | 81 | 13 | Telehealth |
| 14 | Male | 80 | 17 | Online health consultation |
| 15 | Male | 67 | 22 | Wearable devices, Online health education |
| 16 | Female | 63 | 10 | Online psychological consultation |
| 17 | Female | 65 | 9 | Telehealth |
| 18 | Male | 63 | 20 | Online health consultation, Medication reminder |
| 19 | Male | 75 | 12 | Online health education |
| 20 | Female | 81 | 32 | Online health education |
| 21 | Male | 81 | 27 | Online health consultation |
| 22 | Female | 65 | 11 | Telehealth, Wearable devices |
| 23 | Female | 76 | 25 | Online health consultation |
| 24 | Female | 72 | 22 | Online health consultation |
| Categories | Concepts |
|---|---|
| Establish working mechanism | Establish digital teams, clarify project division, establish an information reporting system, regular meetings, establish project teams, select young managers, establish an analysis system, determine work procedures. |
| Collaboration with grassroots departments | Multi-community collaboration, community meeting room sharing, building management cooperation, service experience sharing, unified security management, service group notification, vaccination records. |
| Multi-agency coordination | Two-way referral service, appointment registration, nurse communication, the elderly health service coordination, family doctor team, welfare supplies on behalf of others, drug distribution, the elderly housekeeping services. |
| Supervision and feedback | Set up feedback mailbox, work progress report, confirm partner authority, information release review, service effect evaluation, service content feedback, leadership reception day. |
| Organizational capacity building | Digital discussion meeting, organizational communication meeting, digital thinking, brainstorming, project discussion, Dingding App daily report, WeChat App operation, expert consultation. |
| Digital resource sharing | Data sharing, data backup, data traceability, community information registration, SMS reminder, service record synchronization, information covering the whole community. |
| The elderly service design | Enlarge fonts, slow down processes, amplify notification sounds, health and wellness knowledge, free health lectures, traditional Chinese medicine services, regular telephone calls. |
| Seek external human resources | Volunteer participation, college students caring for the elderly, provision of sphygmomanometer, public welfare promotion, business preferential services. |
| Digital service process | Use mobile phones throughout the process, paperless, telemedicine, Dingding video, QR code service, electronic health code, electronic medical insurance card, smart registration, electronic health record. |
| Service staff support | Guidance for appointment registration, medical reminder, department guidance, electronic signboard, electronic questionnaire, electronic equipment guidance. |
| Digital transformation training | Digital training, development of new digital functions, daily Dingding report, entry of electronic information records, mobile phone training for the elderly. |
| Digital security | Risk control, personal information privacy, information collection protocol, electronic police, infrared smoke sensor, focus on key groups, prevention of telecommunication fraud. |
| Use of digital devices | Use of registration APP, use of self-service registration machines, wearing of smart wristbands, electronic test list printer, electronic triage, electronic hospital guidance. |
| Digital effect evaluation | Decreased medical satisfaction, decreased medical time, increased risk, difficulty with electronic use, insufficient health reminders. |
| Digital perception | Willing to go to a community health service center, unwilling to go to a general hospital, weak experience, not suitable for the elderly, complex digital operations. |
| Digital popularization | Door-to-door support from social workers, distribution of mobile phones for the elderly, telephone notification for the elderly, registration to receive gifts. |
| Family member support | Electronic family network, family member early warning notice, family member teaching, family member accompanying medical treatment. |
| Community health | Chronic diseases, traditional Chinese medicine, vaccination, epidemic prevention and control, first aid measures, AED first aid. |
| Main Categories | Subcategories | Concept Explanation |
|---|---|---|
| A. Institutionalization of digital health service transformation | A1 Establish working mechanism | Establishing a working mechanism is the guarantee of digital transformation |
| A2 Collaboration with grassroots departments | Collaboration between grassroots departments is the internal consensus of digital transformation | |
| A3 Multi-agency coordination | Multi-agency coordination is the premise to meet the diverse health needs of the elderly | |
| A4 Supervision and feedback | Monitoring and feedback ensure that the organization’s risks can be controlled | |
| A5 Organizational capacity building | Organizational capacity building is the internal driving force for digital transformation | |
| A6 Digital resource sharing | Digital resource sharing is the data foundation for digital transformation | |
| B. Digital health service transformation service redesign | B1 The elderly service design | Age-friendly service design is the goal of digital transformation |
| B2 Seek external human resources | External resources can expand digital transformation resources | |
| B3 Digital service process | Digital service process is a direct manifestation of digital transformation | |
| B4 Service staff support | Service personnel promote humanistic care under digital transformation | |
| B5 Digital transformation training | Digital transformation training enhances digital capabilities at different stages | |
| B6 Digital security | Digital security is the premise of digital transformation | |
| C. Digital health service transformation experience evaluation | C1 Use of digital devices | Digital device usage is an enabling tool for digital transformation |
| C2 Digital effect evaluation | Digital effect evaluation reflects the recognition of the elderly | |
| C3 Digital perception | Digital perception experience is the source of service optimization | |
| C4 Digital popularization | Digital popularization can expand the value of digital transformation | |
| C5 Family member support | Family member support is a family requirement for the elderly to embrace digital | |
| C6 Community health | Community health is final result of digital transformation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, S.; Ni, Z.; Ogihara, A.; Wang, X. Behavioral Patterns of Supply and Demand Sides of Health Services for the Elderly in Sustainable Digital Transformation: A Mixed Methods Study. Int. J. Environ. Res. Public Health 2022, 19, 8221. https://doi.org/10.3390/ijerph19138221
Zhou S, Ni Z, Ogihara A, Wang X. Behavioral Patterns of Supply and Demand Sides of Health Services for the Elderly in Sustainable Digital Transformation: A Mixed Methods Study. International Journal of Environmental Research and Public Health. 2022; 19(13):8221. https://doi.org/10.3390/ijerph19138221
Chicago/Turabian StyleZhou, Siyu, Ziling Ni, Atsushi Ogihara, and Xiaohe Wang. 2022. "Behavioral Patterns of Supply and Demand Sides of Health Services for the Elderly in Sustainable Digital Transformation: A Mixed Methods Study" International Journal of Environmental Research and Public Health 19, no. 13: 8221. https://doi.org/10.3390/ijerph19138221
APA StyleZhou, S., Ni, Z., Ogihara, A., & Wang, X. (2022). Behavioral Patterns of Supply and Demand Sides of Health Services for the Elderly in Sustainable Digital Transformation: A Mixed Methods Study. International Journal of Environmental Research and Public Health, 19(13), 8221. https://doi.org/10.3390/ijerph19138221