Engaging Public Health Critical Race Praxis in Local Social Determinants of Health Research: The Youth Health Equity and Action Research Training Program in Portland, OR—yHEARTPDX
Abstract
:1. Introduction
2. yHEARTPDX: Conceptual Roots and Theoretical Groundings
3. yHEARTPDX Vol.I: Youth Participatory Research on Local Social Determinants of Health
3.1. yHEARTPDX Overview
- Create opportunities for youth to influence local public health practice and policy
- Assess community SDH through democratized community health assessment processes
- Provide training opportunities for youth to gain public health skills for future educational opportunities
- Pilot a curriculum for training local youth on health equity, SDH, and participatory research
- Guide youth through a participatory research project to identify and map local SDH concerns
- Use youth research data to generate a series of research and creative arts products that can be used to inform and guide LHD and city planning practices/strategies related to SDH
3.2. yHEARTPDX Training + Research Process
| yHEARTPDX Participatory Research Method | Description |
|---|---|
| Photovoice | A participatory action research method designed to facilitate the empowerment of youth and adults through photography [61,62]. Participants used photography to visually document their daily/weekly experiences (and perceptions thereof) of place-based SDH. The visual representations they generated provided the focus for group discussions and documentation of stories and themes examining/uncovering their lived local SDH experiences in NE Portland. Participants used their smartphones for this method. Activities for this method included 1 training session covering method conceptual roots and ethical concerns, 3 photo review sessions, and 3 participatory photo analysis sessions. For these analysis sessions, youth were trained to complete their own qualitative coding and theming analysis using a process similar to that detailed in Petteway and colleagues [63]. |
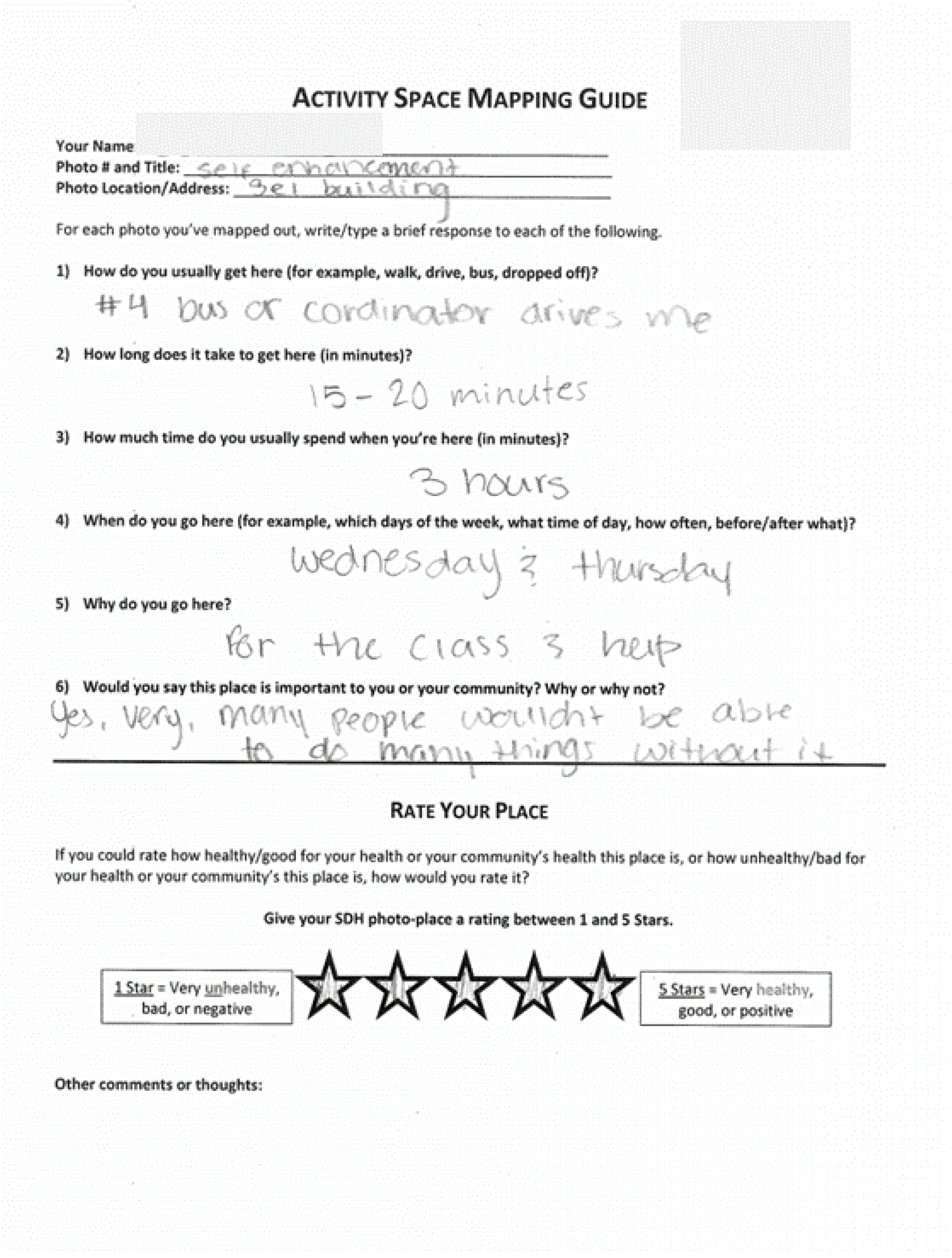
| Activity SpaceMapping | A process by which a participants’ daily activity locations and patterns are mapped out [64,65,66]. In this project, we used a participatory approach. Participants documented their daily activity spaces in a two-fold process. First, they used web-based maps to indicate locations of photovoice photos and other important daily places not captured via Photovoice. Second, they completed Activity Space Mapping worksheets for each photovoice photo location. These worksheets included a series of short descriptive questions and a “Rate Your Place” activity for youth to assign a star-rating to each place (see Figure 2 below). Activities for this method included 1 training session and 1 mapping session. |
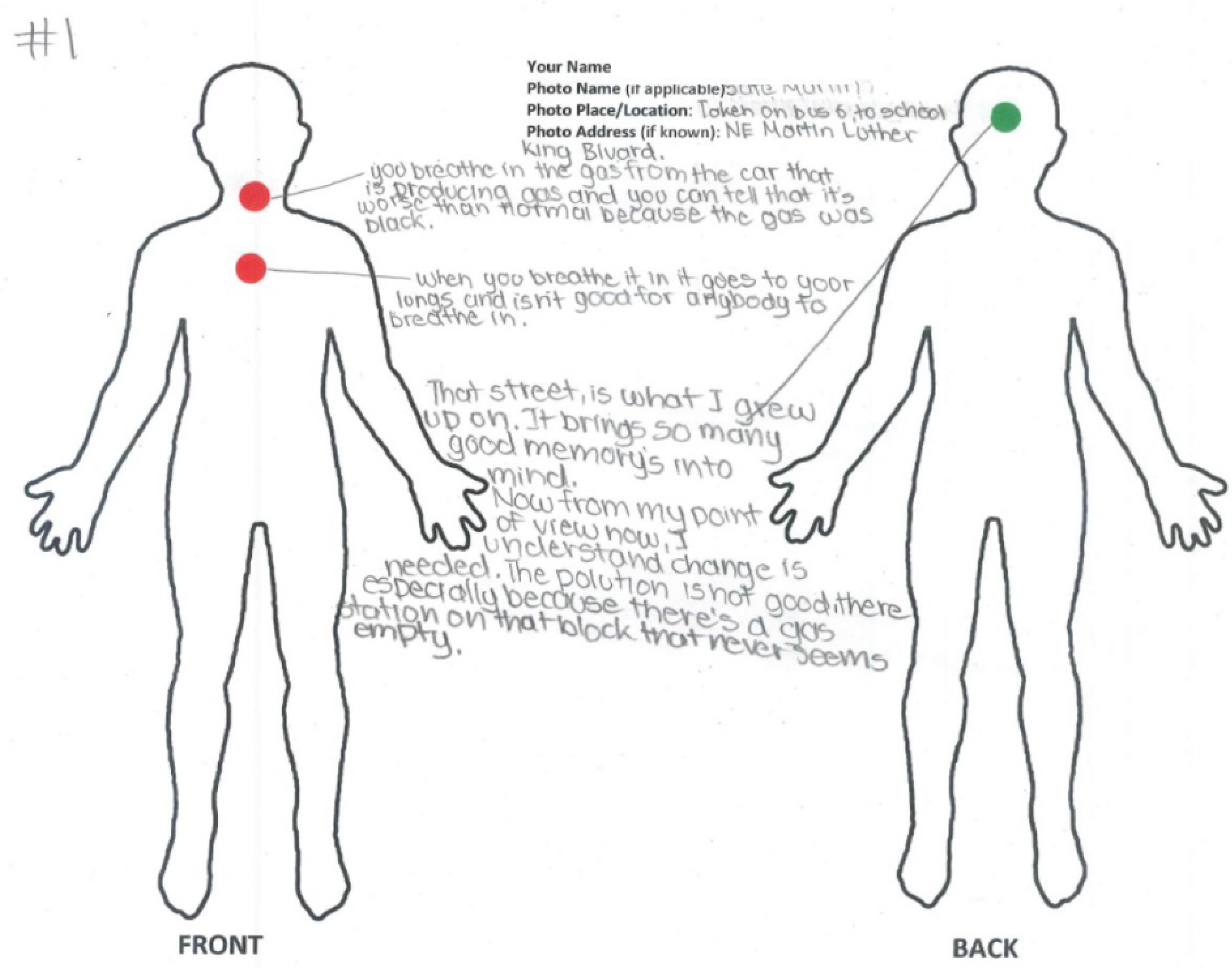
| X-ray Mapping | A cognitive mapping method to understand how participants perceive their daily experiences with place-based SDH and how those experiences affect their bodies/health [29,67]. Essentially, a participatory method to capture subjective notions of embodiment. Participants used “X-ray Map” worksheets containing a basic body outline with ventral and dorsal representation on the front side of the paper and were instructed to locate their perceived place-embodiment effects for each SDH photovoice location (see Figure 3 below). They used color-coded stickers, with green representing a perceived positive body effect, red representing a negative effect, and yellow representing both a positive and negative effect. Participants used the back of their X-ray Map worksheets (and often the front) to write a brief description/narrative explaining their SDH place-embodiment representations. Activities for this method included 1 training session covering notions of embodiment, allostatic load, and weathering, as well as method details, and 1 mapping session. |
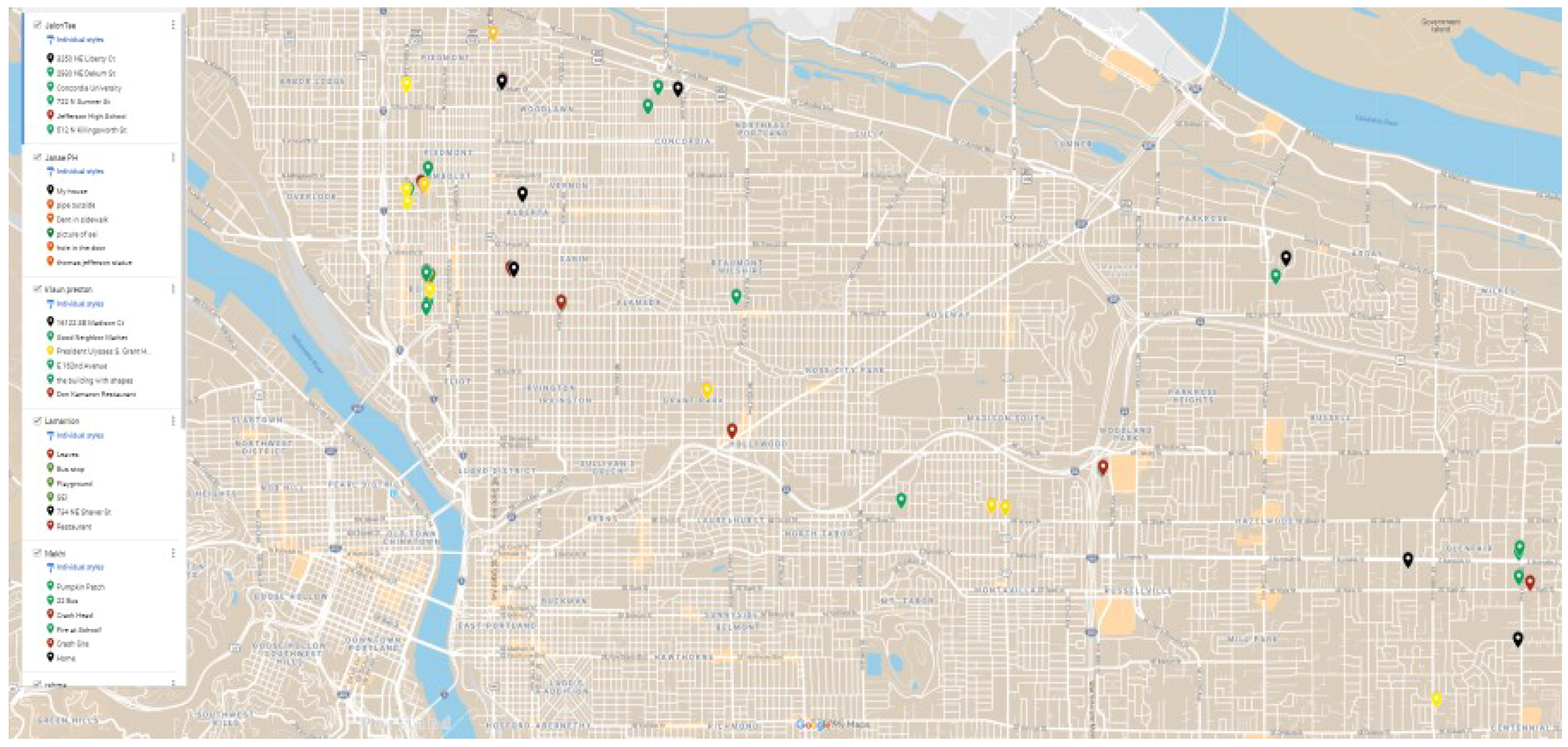
| Participatory GIS | A method by which participants actively define and spatially locate places and share power in creating mapped realities [68,69]. Here, participants integrated Photovoice, Activity Space Mapping, and X-ray Mapping findings for the creation of web-based maps with photos and narratives embedded into each SDH location they identified. Activities for this method included 2 mapping sessions. |
3.3. Illustrative Examples of yHEARTPDX Vol.1 Research
3.3.1. Photovoice
3.3.2. Activity Space Mapping
3.3.3. X-ray Mapping
3.3.4. Participatory GIS
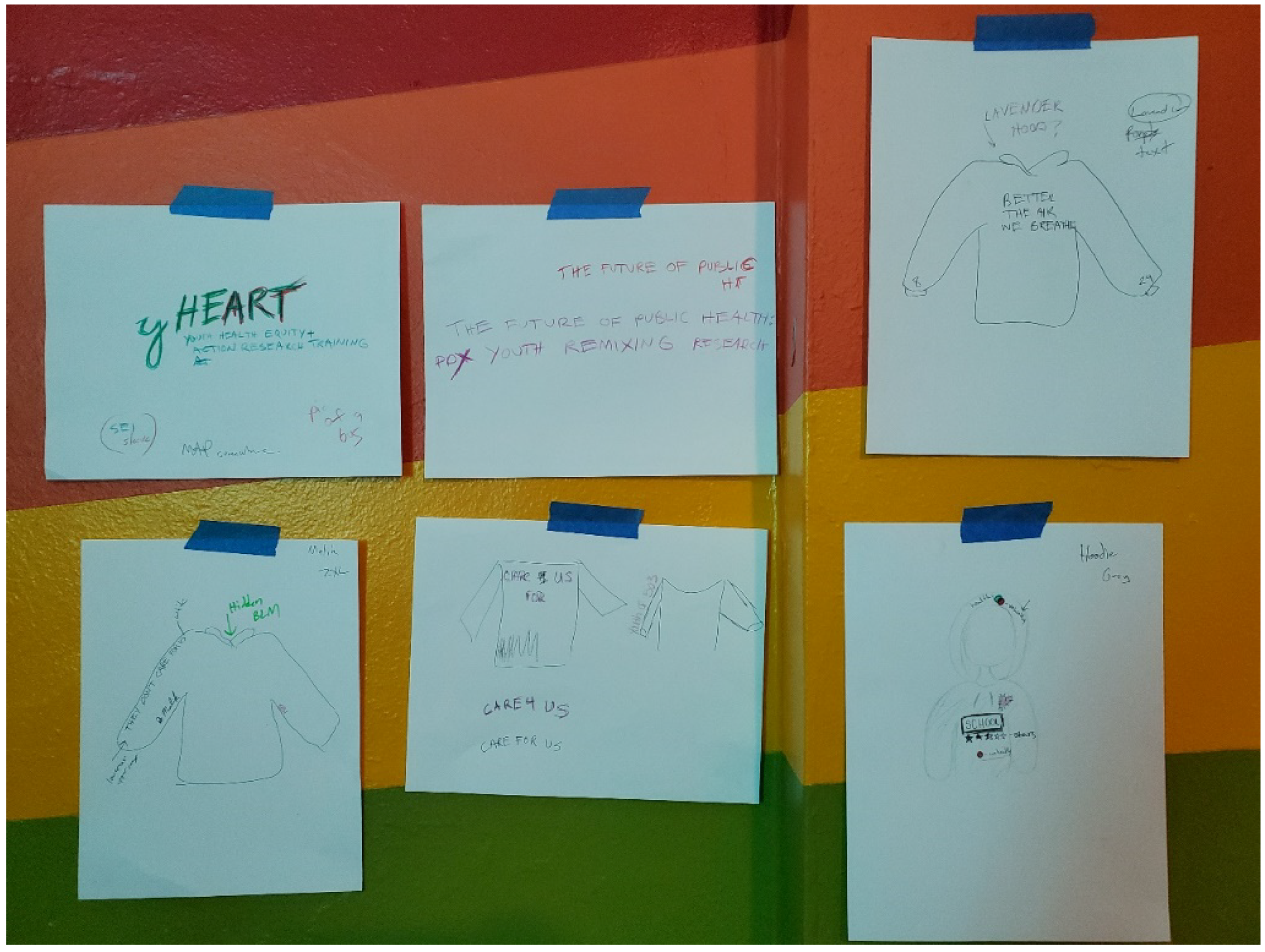
3.4. Creative Arts Products and Dissemination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural Racism and Health Inequities in the USA: Evidence and Interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Gee, G.C.; Ford, C.L. Structural Racism and Health Inequities. Bois Rev. Soc. Sci. Res. Race 2011, 8, 115–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gee, G.C.; Payne-Sturges, D.C. Environmental Health Disparities: A Framework Integrating Psychosocial and Environmental Concepts. Environ. Health Perspect. 2004, 112, 1645–1653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Homan, P.A.; Brown, T.H. Sick and Tired of Being Excluded: Structural Racism in Disenfranchisement as a Threat to Population Health Equity. Health Aff. 2022, 41, 219–227. [Google Scholar] [CrossRef]
- Jacoby, S.F.; Dong, B.; Beard, J.H.; Wiebe, D.J.; Morrison, C.N. The Enduring Impact of Historical and Structural Racism on Urban Violence in Philadelphia. Soc. Sci. Med. 2018, 199, 87–95. [Google Scholar] [CrossRef]
- King, C.J.; Buckley, B.O.; Maheshwari, R.; Griffith, D.M. Race, Place, and Structural Racism: A Review of Health and History in Washington, D.C. Health Aff. 2022, 41, 273–280. [Google Scholar] [CrossRef]
- Viruell-Fuentes, E.A.; Miranda, P.Y.; Abdulrahim, S. More than Culture: Structural Racism, Intersectionality Theory, and Immigrant Health. Soc. Sci. Med. 2012, 75, 2099–2106. [Google Scholar] [CrossRef]
- Williams, D.R.; Collins, C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Rep. 2001, 116, 404. [Google Scholar] [CrossRef]
- Yearby, R.; Clark, B.; Figueroa, J.F. Structural Racism in Historical and Modern US Health Care Policy. Health Aff. 2022, 41, 187–194. [Google Scholar] [CrossRef]
- Goodman, M.S.; Plepys, C.M.; Bather, J.R.; Kelliher, R.M. Racial/Ethnic Diversity in Academic Public Health: 20-Year Update. Public Health Rep. 2019, 135, 74–81. [Google Scholar] [CrossRef] [Green Version]
- McFarling, U. STAT. 12 April 2021. Available online: https://www.statnews.com/2021/04/12/lack-of-diversity-at-premier-medical-journals-jama-nejm/ (accessed on 30 April 2022).
- NIH CSR Data & Evaluations. Available online: https://public.csr.nih.gov/AboutCSR/Evaluations#SRO_demographics (accessed on 3 December 2021).
- Salazar, J.W.; Claytor, J.D.; Habib, A.R.; Guduguntla, V.; Redberg, R.F. Gender, Race, Ethnicity, and Sexual Orientation of Editors at Leading Medical and Scientific Journals: A Cross-Sectional Survey. JAMA Intern. Med. 2021, 181, 1248–1251. [Google Scholar] [CrossRef] [PubMed]
- Petteway, R.J. On Epidemiology as Racial-Capitalist (Re)Colonization and Epistemic Violence. Crit. Public Health 2022, forthcoming. [Google Scholar]
- Petteway, R.J. Something Something Something by Race, 2021. Int. J. Epidemiol. 2022, dyac010. [Google Scholar] [CrossRef]
- Adkins-Jackson, P.B.; Chantarat, T.; Bailey, Z.D.; Ponce, N.A. Measuring Structural Racism: A Guide for Epidemiologists and Other Health Researchers. Am. J. Epidemiol. 2021, 191, 539–547. [Google Scholar] [CrossRef]
- Alang, S.; Hardeman, R.; Karbeah, J.; Akosionu, O.; McGuire, C.; Abdi, H.; McAlpine, D. White Supremacy and the Core Functions of Public Health. Am. J. Public Health 2021, 111, 815–819. [Google Scholar] [CrossRef]
- Hardeman, R.R.; Homan, P.A.; Chantarat, T.; Davis, B.A.; Brown, T.H. Improving the Measurement of Structural Racism to Achieve Antiracist Health Policy. Health Aff. 2022, 41, 179–186. [Google Scholar] [CrossRef]
- Lett, E.; Adekunle, D.; McMurray, P.; Asabor, E.N.; Irie, W.; Simon, M.A.; Hardeman, R.; McLemore, M.R. Health Equity Tourism: Ravaging the Justice Landscape. J. Med. Syst. 2022, 46, 17. [Google Scholar] [CrossRef]
- Ford, C.L.; Airhihenbuwa, C.O. Critical Race Theory, Race Equity, and Public Health: Toward Antiracism Praxis. Am. J. Public Health 2010, 100, S30–S35. [Google Scholar] [CrossRef]
- Petteway, R.; Mujahid, M.; Allen, A.; Morello-Frosch, R. Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century. Int. J. Environ. Res. Public Health 2019, 16, 3983. [Google Scholar] [CrossRef] [Green Version]
- Balazs, C.L.; Morello-Frosch, R. The Three Rs: How Community-Based Participatory Research Strengthens the Rigor, Relevance, and Reach of Science. Environ. Justice 2013, 6, 9–16. [Google Scholar] [CrossRef] [Green Version]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of Community-Based Research: Assessing Partnership Approaches to Improve Public Health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minkler, M. Linking Science and Policy through Community-Based Participatory Research to Study and Address Health Disparities. Am. J. Public Health 2010, 100, S81–S87. [Google Scholar] [CrossRef]
- Wallerstein, N.B.; Yen, I.H.; Syme, S.L. Integration of Social Epidemiology and Community-Engaged Interventions to Improve Health Equity. Am. J. Public Health 2011, 101, 822–830. [Google Scholar] [CrossRef]
- Wallerstein, N.; Duran, B. The Theoretical, Historical, and Practice Roots of CBPR. In Community-Based Participatory Research for Health: Advancing Social and Health Equity; Wallerstein, N., Duran, B., Oetzel, J., Minkler, M., Eds.; Jossey-Bass: New York, NY, USA, 2017. [Google Scholar]
- Krieger, N. Theories for Social Epidemiology in the 21st Century: An Ecosocial Perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N. Embodiment: A Conceptual Glossary for Epidemiology. J. Epidemiol. Community Health 2005, 59, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Petteway, R.; Mujahid, M.; Allen, A. Understanding Embodiment in Place-Health Research: Approaches, Limitations, and Opportunities. J. Urban Health 2019, 96, 289–299. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J. Social Conditions as Fundamental Causes of Disease. J. Health Soc. Behav. 1995, 35, 80. [Google Scholar] [CrossRef] [Green Version]
- Phelan, J.C.; Link, B.G.; Diez-Roux, A.; Kawachi, I.; Levin, B. “Fundamental Causes” of Social Inequalities in Mortality: A Test of the Theory. J. Health Soc. Behav. 2004, 45, 265–285. [Google Scholar] [CrossRef]
- Beckfield, J.; Krieger, N. Epi + Demos + Cracy: Linking Political Systems and Priorities to the Magnitude of Health Inequities--Evidence, Gaps, and a Research Agenda. Epidemiol. Rev. 2009, 31, 152–177. [Google Scholar] [CrossRef] [Green Version]
- Navarro, V.; Borrell, C.; Benach, J.; Muntaner, C.; Quiroga, A.; Rodríguez-Sanz, M.; Vergés, N.; Gumá, J.; Pasarín, M.I. The Importance of the Political and the Social in Explaining Mortality Differentials among the Countries of the OECD, 1950–1998. Int. J. Health Serv. 2003, 33, 419–494. [Google Scholar] [CrossRef]
- Bambra, C. The Political Economy of the United States and the People’s Health. Am. J. Public Health 2019, 109, 833–834. [Google Scholar] [CrossRef] [PubMed]
- Phelan, J.C.; Link, B.G. Is Racism a Fundamental Cause of Inequalities in Health? Annu. Rev. Sociol. 2015, 41, 311–330. [Google Scholar] [CrossRef]
- Jones, M.R.; Diez-Roux, A.V.; Hajat, A.; Kershaw, K.N.; O’Neill, M.S.; Guallar, E.; Post, W.S.; Kaufman, J.D.; Navas-Acien, A. Race/Ethnicity, Residential Segregation, and Exposure to Ambient Air Pollution: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Public Health 2014, 104, 2130–2137. [Google Scholar] [CrossRef] [PubMed]
- Morello-Frosch, R.; Jesdale, B.M. Separate and Unequal: Residential Segregation and Estimated Cancer Risks Associated with Ambient Air Toxics in U.S. Metropolitan Areas. Environ. Health Perspect. 2006, 114, 386–393. [Google Scholar] [CrossRef] [Green Version]
- Morello-Frosch, R.; Shenassa, E.D. The Environmental “Riskscape” and Social Inequality: Implications for Explaining Maternal and Child Health Disparities. Environ. Health Perspect. 2006, 114, 1150–1153. [Google Scholar] [CrossRef]
- Wilson, S.; Hutson, M.; Mujahid, M. How Planning and Zoning Contribute to Inequitable Development, Neighborhood Health, and Environmental Injustice. Environ. Justice 2008, 1, 211–216. [Google Scholar] [CrossRef] [Green Version]
- Wilson, S.; Aber, A.; Wright, L.; Ravichandran, V. A Review of Community-Engaged Research Approaches Used to Achieve Environmental Justice and Eliminate Disparities. In The Routledge Handbook of Environmental Justice; Routledge: London, UK, 2017; ISBN 978-1-315-67898-6. [Google Scholar]
- Bowleg, L. The Problem with the Phrase Women and Minorities: Intersectionality—An Important Theoretical Framework for Public Health. Am. J. Public Health 2012, 102, 1267–1273. [Google Scholar] [CrossRef]
- Gee, G.C.; Walsemann, K.M.; Brondolo, E. A Life Course Perspective on How Racism May Be Related to Health Inequities. Am. J. Public Health 2012, 102, 967–974. [Google Scholar] [CrossRef]
- Hertzman, C. Putting the Concept of Biological Embedding in Historical Perspective. Proc. Natl. Acad. Sci. USA 2012, 109, 17160–17167. [Google Scholar] [CrossRef] [Green Version]
- Loi, M.; Del Savio, L.; Stupka, E. Social Epigenetics and Equality of Opportunity. Public Health Ethics 2013, 6, 142–153. [Google Scholar] [CrossRef] [Green Version]
- Seeman, T.; Epel, E.; Gruenewald, T.; Karlamangla, A.; McEwen, B.S. Socio-Economic Differentials in Peripheral Biology: Cumulative Allostatic Load: SES Peripheral Biology. Ann. N. Y. Acad. Sci. 2010, 1186, 223–239. [Google Scholar] [CrossRef] [PubMed]
- Diamond, L. Liberation Technology. J. Democr. 2010, 21, 69–83. [Google Scholar] [CrossRef]
- Pfister, D.S.; Godana, G.D. Deliberation Technology. J. Public Deliberation 2012, 8, 7. [Google Scholar]
- D’Ignazio, C.; Warren, J.; Blair, D. The Role of Small Data for Governance in the 21st Century. In Governança Digital; Universidade Federal Rio Grande do Sul: Porto Alegre, Brazil, 2014; pp. 115–129. [Google Scholar]
- Macintyre, S.; Ellaway, A.; Cummins, S. Place Effects on Health: How Can We Conceptualise, Operationalise and Measure Them? Soc. Sci. Med. 2002, 55, 125–139. [Google Scholar] [CrossRef]
- Cummins, S.; Curtis, S.; Diez-Roux, A.V.; Macintyre, S. Understanding and Representing ‘Place’ in Health Research: A Relational Approach. Soc. Sci. Med. 2007, 65, 1825–1838. [Google Scholar] [CrossRef] [PubMed]
- Matthews, S.A. Spatial Polygamy and the Heterogeneity of Place: Studying People and Place via Egocentric Methods. In Communities, Neighborhoods, and Health; Burton, L.M., Matthews, S.A., Leung, M., Kemp, S.P., Takeuchi, D.T., Eds.; Springer: New York, NY, USA, 2011; pp. 35–55. ISBN 978-1-4419-7481-5. [Google Scholar]
- Freire, P. Pedagogy of the Oppressed, 30th anniversary ed.; Continuum: New York, NY, USA, 2000; ISBN 978-0-8264-1276-8. [Google Scholar]
- Haraway, D. Situated Knowledges: The Science Question in Feminism and the Privilege of Partial Perspective. Fem. Stud. 1988, 14, 575–599. [Google Scholar] [CrossRef]
- Smith, P.L.T. Decolonizing Methodologies: Research and Indigenous Peoples; Zed Books Ltd.: London, UK, 2013; ISBN 978-1-84813-953-4. [Google Scholar]
- Chinn, P.W.U. Decolonizing Methodologies and Indigenous Knowledge: The Role of Culture, Place and Personal Experience in Professional Development. J. Res. Sci. Teach. 2007, 44, 1247–1268. [Google Scholar] [CrossRef]
- Hooks, B. Feminist Theory: From Margin to Center; Pluto Press: London, UK, 2000; ISBN 978-0-7453-1663-5. [Google Scholar]
- Hooks, B. Yearning: Race, Gender, and Cultural Politics; Routledge: New York, NY, USA, 2015. [Google Scholar]
- Ford, C.L.; Airhihenbuwa, C.O. The Public Health Critical Race Methodology: Praxis for Antiracism Research. Soc. Sci. Med. 2010, 71, 1390–1398. [Google Scholar] [CrossRef] [PubMed]
- RWJF County Health Rankings. Available online: https://www.countyhealthrankings.org/explore-health-rankings (accessed on 30 July 2020).
- CDC 500 Cities Project: Local Data for Better Health. Available online: https://www.cdc.gov/500cities/index.htm (accessed on 30 July 2020).
- Catalani, C.; Minkler, M. Photovoice: A Review of the Literature in Health and Public Health. Health Educ. Behav. 2010, 37, 424–451. [Google Scholar] [CrossRef]
- Wang, C.; Burris, M.A. Photovoice: Concept, Methodology, and Use for Participatory Needs Assessment. Health Educ. Behav. Off. Publ. Soc. Public Health Educ. 1997, 24, 369–387. [Google Scholar] [CrossRef] [Green Version]
- Petteway, R.J. Intergenerational Photovoice Perspectives of Place and Health in Public Housing: Participatory Coding, Theming, and Mapping in/of the “Structure Struggle”. Health Place 2019, 60, 102229. [Google Scholar] [CrossRef] [PubMed]
- Cagney, K.A.; York Cornwell, E.; Goldman, A.W.; Cai, L. Urban Mobility and Activity Space. Annu. Rev. Sociol. 2020, 46, 623–648. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.; Pebley, A.R. Redefining Neighborhoods Using Common Destinations: Social Characteristics of Activity Spaces and Home Census Tracts Compared. Demography 2014, 51, 727–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perchoux, C.; Chaix, B.; Cummins, S.; Kestens, Y. Conceptualization and Measurement of Environmental Exposure in Epidemiology: Accounting for Activity Space Related to Daily Mobility. Health Place 2013, 21, 86–93. [Google Scholar] [CrossRef]
- Ruglis, J. Mapping the Biopolitics of School Dropout and Youth Resistance. Int. J. Qual. Stud. Educ. 2011, 24, 627–637. [Google Scholar] [CrossRef]
- Dunn, C.E. Participatory GIS—A People’s GIS? Prog. Hum. Geogr. 2007, 31, 616–637. [Google Scholar] [CrossRef]
- Elwood, S. Critical Issues in Participatory GIS: Deconstructions, Reconstructions, and New Research Directions. Trans. GIS 2006, 10, 693–708. [Google Scholar] [CrossRef]
- Petteway, R.; Gonzalez, L. (Chillin’ Out) “Maxing”: YPAR Perspectives on Embodiment and Transportation Equity in Portland, or. In Proceedings of the 148th Meeting of the American Public Health Association, Minneapolis, MN, USA, 27 October 2020; American Public Health Association: Washington, DC, USA, 2020. [Google Scholar]
- Burch, S.R. Perspectives on Racism: Reflections on Our Collective Moral Responsibility When Leveraging Arts and Culture for Health Promotion. Health Promot. Pract. 2021, 22, 12S–16S. [Google Scholar] [CrossRef]
- Griffith, D.M.; Semlow, A.R. Art, Anti-Racism and Health Equity: “Don’t Ask Me Why, Ask Me How”! Ethn. Dis. 2020, 30, 373–380. [Google Scholar] [CrossRef]
- Jackson, M.R. Addressing Inequity through Public Health, Community Development, Arts, and Culture: Confluence of Fields and the Opportunity to Reframe, Retool, and Repair. Health Promot. Pract. 2021, 22, 141S–146S. [Google Scholar] [CrossRef]
- Petteway, R.J. Poetry as Praxis + “Illumination”: Toward an Epistemically Just Health Promotion for Resistance, Healing, and (Re)Imagination. Health Promot. Pract. 2021, 22, 20S–26S. [Google Scholar] [CrossRef] [PubMed]
- Dill, L.J. Poetic Justice: Engaging in Participatory Narrative Analysis to Find Solace in the “Killer Corridor”. Am. J. Community Psychol. 2015, 55, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Delgado, R. Storytelling for Oppositionists and Others: A Plea for Narrative. Mich. Law Rev. 1989, 87, 2411–2441. [Google Scholar] [CrossRef] [Green Version]
- Solórzano, D.G.; Yosso, T.J. Critical Race Methodology: Counter-Storytelling as an Analytical Framework for Education Research. Qual. Inq. 2002, 8, 23–44. [Google Scholar] [CrossRef]

| yHEARTPDX Training Module | Description |
|---|---|
| Public Health 101 | Introduced youth to public health systems and processes in both practice and academic/research contexts. Discussed core aspects of public health laws and regulations, including basic structure of public health powers across legislative, judicial (e.g., case law), and executive branches (e.g., administrative law) of federal, state, and local government. Example discussion topics included aspects of public health law, policy, and practice related to inspections, nuisance abatement, health monitoring and surveillance, quarantine, and environmental regulation. Discussed role of governmental (e.g., CDC, EPA) and non-governmental public health organizations (e.g., NACCHO). Provided a basic overview of core public health subfields of Epidemiology, Health Education/Health Promotion, Environmental Health, Health Systems and Policy, and Biostatistics. |
| Epidemiology 101 | Explored historical foundations and evolution of epidemiology, including core elements of modern practice, goals, and tools/approaches. Introduced youth to various areas of epidemiology, including Infections Disease, Chronic Disease, Behavioral, Environmental, and Injury. Discussed the roles, responsibilities, and functions of epidemiology in LHDs. Covered basic definitions for key terms (e.g., “incidence”, “prevalence”, “exposures”, “outcomes”). This session made use of local epidemiology data (e.g., mortality data) to discuss aspects of local health surveillance and monitoring. |
| SDH + Social Epi 101 | Developed youth knowledge and understanding of SDH and introduced socioecological models and health equity frameworks. This session made use of local SDH and health data and maps to discuss the impact and role of SDH locally. Discussed basic foundations of social epidemiology (in contrast to traditional epidemiology), including political economy, ecosocial theory, and the notion of embodiment. Highlighted role of structural forms of oppression and exclusion (e.g., racism, class inequality, sexism) in shaping health. Highlighted the “place” and health subfield as an area important for addressing SDH. |
| Health Equity 101 | Introduced conceptual foundations and frameworks related to health equity and social justice within public health, and presented basic definitions for critical concepts (e.g., “disparities” vs. “inequities”, health in all policies). Highlighted the role of SDH and population-focused approaches to public health. |
| Public Health Research + Research Ethics 101 | Introduced youth to basic elements of public health research, research methods (e.g., quantitative, qualitative, mixed), functions/roles of public health research (e.g., community assessment, accountability, implications for policy), and goals (e.g., addressing health inequities). Additionally, discussed historical foundations and considerations related to research ethics (e.g., Belmont Report, Tuskegee “study”), specifically in relation to human subjects research and research involving vulnerable populations. |
| CBPR + YPAR 101 | Introduced core principles of CBPR and YPAR and provided an overview of the potential benefits of participatory research in comparison to traditional research. Highlighted importance of power relations and building community capacity. Additionally, introduced critical concepts of decolonizing research and methods, as well as feminist and Black feminist notions of situated knowledge(s) and centering the margins. Session also covered Freire’s notion of critical consciousness, Gramsci’s notion of “organic intellectual”, and general discussion of popular epidemiology, citizen science, and co-production of knowledge. |
| Place, Placemaking, & Health 101 | Developed youth knowledge and understanding of the significance of “place” in shaping health, including notions and mechanisms of “placemaking”. This included introduction to historic and current forces that shape neighborhood built, natural, and social environments, including discussion of core racialized placemaking processes as follows: Indian Removal Act of 1830, Homestead Act of 1862, Oregon Donation Lands Claim Act of 1850, redlining, racially restrictive covenants, the GI Bill, Federal Highway Act of 1956, Gentrification, Serial Forced Displacement, Blockbusting, and exclusionary zoning. This session also discussed general aspects of city planning, land use, and community development. Session was connected to local/regional social determinants of health, making use of local health data and maps to discuss the impact of placemaking processes on SDH locally. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petteway, R.J.; González, L.A. Engaging Public Health Critical Race Praxis in Local Social Determinants of Health Research: The Youth Health Equity and Action Research Training Program in Portland, OR—yHEARTPDX. Int. J. Environ. Res. Public Health 2022, 19, 8187. https://doi.org/10.3390/ijerph19138187
Petteway RJ, González LA. Engaging Public Health Critical Race Praxis in Local Social Determinants of Health Research: The Youth Health Equity and Action Research Training Program in Portland, OR—yHEARTPDX. International Journal of Environmental Research and Public Health. 2022; 19(13):8187. https://doi.org/10.3390/ijerph19138187
Chicago/Turabian StylePetteway, Ryan J., and Lourdes A. González. 2022. "Engaging Public Health Critical Race Praxis in Local Social Determinants of Health Research: The Youth Health Equity and Action Research Training Program in Portland, OR—yHEARTPDX" International Journal of Environmental Research and Public Health 19, no. 13: 8187. https://doi.org/10.3390/ijerph19138187
APA StylePetteway, R. J., & González, L. A. (2022). Engaging Public Health Critical Race Praxis in Local Social Determinants of Health Research: The Youth Health Equity and Action Research Training Program in Portland, OR—yHEARTPDX. International Journal of Environmental Research and Public Health, 19(13), 8187. https://doi.org/10.3390/ijerph19138187






