Metabolic and Obesity Phenotype Trajectories in Taiwanese Medical Personnel
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Population
2.2. Measurements Metabolic Health, Overweight and Obesity
2.2.1. Metabolic and Obesity Phenotypes
2.2.2. Working Hours and Health Behavior Characteristics
2.3. Statistical Analysis
3. Results
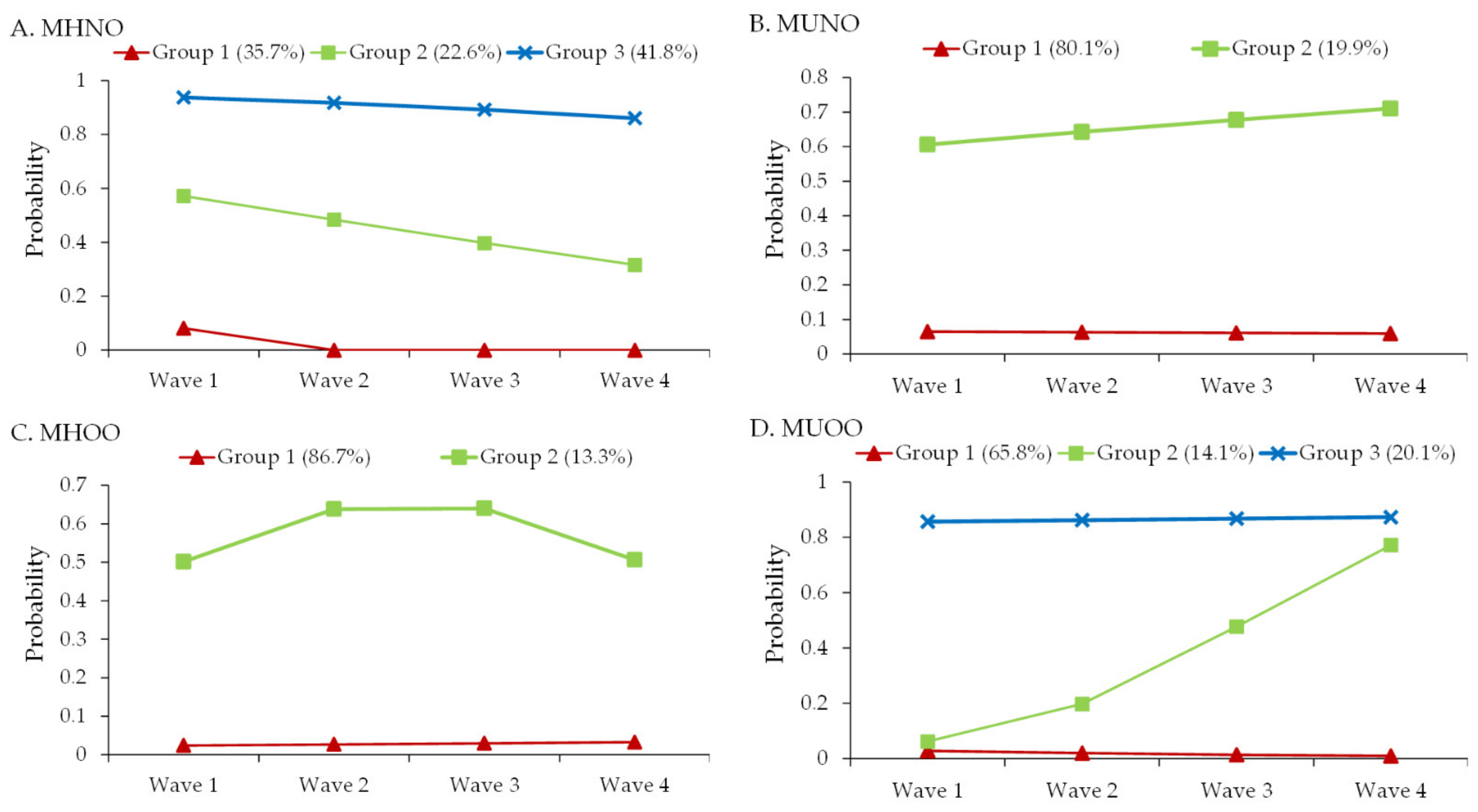
3.1. Latent Classes of the Developmental Trajectories for the Metabolic and Obesity Phenotypes
3.2. Factors Associated with the Latent Classes of Developmental Trajectories for Each Phenotype
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Total (n = 3264) | MHNO (n = 1484) | MUNO (n = 595) | MHOO (n = 401) | MUOO (n = 784) | p Value |
|---|---|---|---|---|---|---|
| Age (years) | 34.5 ± 8.8 | 32.7 ± 7.8 | 35.2 ± 9.7 a | 34.8 ± 8.4 a | 37.2 ± 9.2 abc | <0.001 |
| Age (years) | <0.001 | |||||
| 20–40 | 2634 (80.7) | 1284 (86.5) | 463 (77.8) a | 319 (79.6) a | 568 (72.4) ac | |
| ≥40 | 630 (19.3) | 200 (13.5) | 132 (22.2) a | 82 (20.4) a | 216 (27.6) ac | |
| Male | 737 (22.6) | 136 (9.2) | 177 (29.7) a | 92 (22.9) a | 332 (42.3) abc | <0.001 |
| Body mass index (kg/m2) | 23.3 ± 4.0 | 20.7 ± 1.9 | 21.3 ± 1.9 a | 26.3 ± 2.3 ab | 28.1 ± 3.6 abc | <0.001 |
| Alcohol consumption | 887 (27.2) | 370 (24.9) | 161 (27.1) | 117 (29.2) | 239 (30.5) a | 0.030 |
| Working hours/week | 45.6 ± 11.4 | 44.9 ± 10.8 | 45.9 ± 11.8 | 46.2 ± 11.9 | 46.3 ± 11.8 a | 0.016 |
| Working hours/week | 0.023 | |||||
| ≤40 | 1858 (56.9) | 872 (58.8) | 338 (56.8) | 211 (52.6) | 437 (55.7) | |
| 41–49 | 674 (20.6) | 317 (21.4) | 114 (19.2) | 95 (23.7) | 148 (18.9) | |
| ≥50 | 732 (22.4) | 295 (19.9) | 143 (24.0) | 95 (23.7) | 199 (25.4) a | |
| Profession type | <0.001 | |||||
| Nurse | 1681 (51.5) | 879 (59.2) | 269 (45.2) a | 216 (53.9) b | 317 (40.4) ac | |
| Physician | 656 (20.1) | 239 (16.1) | 132 (22.2) a | 82 (20.4) | 203 (25.9) a | |
| Other medical staff | 358 (11.0) | 151 (10.2) | 85 (14.3) a | 39 (9.7) | 83 (10.6) | |
| Administrative staff | 569 (17.4) | 215 (14.5) | 109 (18.3) | 64 (16.0) | 181 (3.1) ac |
| Reference Group: MHNO | ||||||
|---|---|---|---|---|---|---|
| MUNO | MHOO | MUOO | ||||
| Variable | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value |
| Age (years) | ||||||
| 20–40 | Reference | Reference | Reference | |||
| ≥40 | 1.93 (1.50–2.48) | <0.001 | 1.72 (1.28–2.29) | <0.001 | 2.80 (2.22–3.52) | <0.001 |
| Male | 5.19 (3.81–7.06) | <0.001 | 3.63 (2.53–5.21) | <0.001 | 10.50 (7.85–14.04) | <0.001 |
| Alcohol consumption | 0.94 (0.75–1.18) | 0.600 | 1.12 (0.87–1.44) | 0.395 | 1.01 (0.82–1.25) | 0.931 |
| Working hours/week | ||||||
| ≤40 | Reference | Reference | Reference | |||
| 41–49 | 0.97 (0.75–1.25) | 0.814 | 1.24 (0.94–1.64) | 0.130 | 0.98 (0.77–1.25) | 0.864 |
| ≥50 | 1.03 (0.77–1.38) | 0.843 | 1.14 (0.81–1.59) | 0.457 | 0.96 (0.72–1.27) | 0.761 |
| Profession type | ||||||
| Nurse | Reference | Reference | Reference | |||
| Physician | 0.73 (0.51–1.05) | 0.090 | 0.68 (0.45–1.03) | 0.068 | 0.59 (0.42–0.84) | 0.003 |
| Other medical staff | 1.35 (0.98–1.84) | 0.064 | 0.86 (0.58–1.28) | 0.470 | 0.85 (0.61–1.18) | 0.329 |
| Administrative staff | 1.29 (0.97–1.71) | 0.078 | 1.06 (0.76–1.47) | 0.744 | 1.45 (1.12–1.88) | 0.005 |
References
- Niazi, E.; Saraei, M.; Aminian, O.; Izadi, N. Frequency of metabolic syndrome and its associated factors in health care workers. Diabetes Metab. Syndr. 2019, 13, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Rossa, C.E.; Caramori, P.R.; Manfroi, W.C. Metabolic syndrome in workers in a university hospital. Rev. Port. Cardiol. 2012, 31, 629–636. [Google Scholar]
- Sharma, S.V.; Upadhyaya, M.; Karhade, M.; Baun, W.B.; Perkison, W.B.; Pompeii, L.A.; Brown, H.S.; Hoelscher, D.M. Are Hospital Workers Healthy: A study of cardiometabolic, behavioral, and psychosocial factors associated with obesity among hospital workers. J. Occup. Environ. Med. 2016, 58, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.G.; Wills, J.; Mahoney, C.; Hoyle, L.; Kelly, M.; Atherton, I.M. Obesity prevalence among healthcare professionals in England: A cross-sectional study using the Health Survey for England. BMJ Open 2017, 7, e018498. [Google Scholar] [CrossRef]
- Yeh, W.C.; Chuang, H.H.; Lu, M.C.; Tzeng, I.S.; Chen, J.Y. Prevalence of metabolic syndrome among employees of a Taiwanese hospital varies according to profession. Medicine 2018, 97, e11664. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Eckel, N.; Li, Y.; Kuxhaus, O.; Stefan, N.; Hu, F.B.; Schulze, M.B. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018, 6, 714–724. [Google Scholar] [CrossRef]
- Gao, M.; Lv, J.; Yu, C.; Guo, Y.; Bian, Z.; Yang, R.; Du, H.; Yang, L.; Chen, Y.; Li, Z.; et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: A cohort study. PLoS Med. 2020, 17, e1003351. [Google Scholar] [CrossRef]
- Pega, F.; Náfrádi, B.; Momen, N.C.; Ujita, Y.; Streicher, K.N.; Prüss-Üstün, A.M.; Group, T.A.; Descatha, A.; Driscoll, T.; Fischer, F.M.; et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO JoInt. Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 154, 106595. [Google Scholar]
- Bannai, A.; Tamakoshi, A. The association between long working hours and health: A systematic review of epidemiological evidence. Scand. J. Work Environ. Health 2014, 40, 5–18. [Google Scholar] [CrossRef]
- Rogers, A.E.; Hwang, W.T.; Scott, L.D.; Aiken, L.H.; Dinges, D.F. The working hours of hospital staff nurses and patient safety. Health Aff. 2004, 23, 202–212. [Google Scholar] [CrossRef]
- Chou, L.P.; Li, C.Y.; Hu, S.C. Job stress and burnout in hospital employees: Comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open 2014, 4, e004185. [Google Scholar] [CrossRef]
- WHO Expert Consultation. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Genuth, S.; Alberti, K.G.M.M.; Bennett, P.; Buse, J.; Defronzo, R.; Kahn, R.; Kitzmiller, J.; Knowler, W.C.; Lebovitz, H.; Lernmark, A.; et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003, 26, 3160–3167. [Google Scholar]
- Janghorbani, M.; Salamat, M.R.; Amini, M.; Aminorroaya, A. Risk of diabetes according to the metabolic health status and degree of obesity. Diabetes Metab. Syndr. 2017, 11 (Suppl. 1), S439–S444. [Google Scholar] [CrossRef]
- Chu, N.F. Prevalence of obesity in Taiwan. Obes. Rev. 2005, 6, 271–274. [Google Scholar] [CrossRef]
- Andruff, H.; Carraro, N.; Thompson, A.; Gaudreau, P.; Louvet, B. Latent class growth modelling: A tutorial. Tutor. Quant. Methods Psychol. 2009, 5, 11–24. [Google Scholar] [CrossRef]
- Jones, B.L.; Nagin, D.S.; Roeder, K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol. Methods Res. 2001, 29, 374–393. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The epidemiology of obesity: A big picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Kabat, G.C.; Wu, W.Y.; Bea, J.W.; Chen, C.; Qi, L.; Stefanick, M.L.; Chlebowski, R.T.; Lane, D.S.; Wactawski-Wende, J.; Wassertheil-Smoller, S.; et al. Metabolic phenotypes of obesity: Frequency, correlates and change over time in a cohort of postmenopausal women. Int. J. Obes. 2017, 41, 170–177. [Google Scholar] [CrossRef]
- Pan, W.H.; Flegal, K.M.; Chang, H.Y.; Yeh, W.T.; Yeh, C.J.; Lee, W.C. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: Implications for definitions of overweight and obesity for Asians. Am. J. Clin. Nutr. 2004, 79, 31–39. [Google Scholar] [CrossRef]
- Wang, Y.-W. 2017 Annual Report of Health Promotion Administration; Health Promotion Administration, Ministry of Health and Welfare: Taipei, Taiwan, 2018.
- Blüher, M. Metabolically healthy obesity. Endocr. Rev. 2020, 41, 405–420. [Google Scholar] [CrossRef]
- Stefan, N.; Häring, H.U.; Hu, F.B.; Schulze, M.B. Metabolically healthy obesity: Epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 2013, 1, 152–162. [Google Scholar] [CrossRef]
- Stefan, N. Metabolically healthy and unhealthy normal weight and obesity. Endocrinol. Metab. 2020, 35, 487–493. [Google Scholar] [CrossRef]
- Smith, G.I.; Mittendorfer, B.; Klein, S. Metabolically healthy obesity: Facts and fantasies. J. Clin. Investig. 2019, 129, 3978–3989. [Google Scholar] [CrossRef]
- Klitgaard, H.B.; Kilbak, J.H.; Nozawa, E.A.; Seidel, A.V.; Magkos, F. Physiological and lifestyle traits of metabolic dysfunction in the absence of obesity. Curr. Diabetes Rep. 2020, 20, 17. [Google Scholar] [CrossRef]
- Lin, C.C.; Liu, C.S.; Lai, M.M.; Li, C.I.; Chen, C.C.; Chang, P.C.; Lin, W.Y.; Lee, Y.D.; Lin, T.; Li, T.C. Metabolic syndrome in a Taiwanese metropolitan adult population. BMC Public Health 2007, 7, 239. [Google Scholar] [CrossRef]
- Vishram, J.K.; Borglykke, A.; Andreasen, A.H.; Jeppesen, J.; Ibsen, H.; Jørgensen, T.; Palmieri, L.; Giampaoli, S.; Donfrancesco, C.; Kee, F.; et al. Impact of age and gender on the prevalence and prognostic importance of the metabolic syndrome and its components in Europeans. The MORGAM Prospective Cohort Project. PLoS ONE 2014, 9, e107294. [Google Scholar] [CrossRef]
- Sidorenkov, O.; Nilssen, O.; Brenn, T.; Martiushov, S.; Arkhipovsky, V.L.; Grjibovski, A.M. Prevalence of the metabolic syndrome and its components in Northwest Russia: The Arkhangelsk study. BMC Public Health 2010, 10, 23. [Google Scholar] [CrossRef]
- Park, H.S.; Lee, S.Y.; Kim, S.M.; Han, J.H.; Kim, D.J. Prevalence of the metabolic syndrome among Korean adults according to the criteria of the International Diabetes Federation. Diabetes Care 2006, 29, 933–934. [Google Scholar] [CrossRef][Green Version]
- Novak, M.; Björck, L.; Welin, L.; Welin, C.; Manhem, K.; Rosengren, A. Gender differences in the prevalence of metabolic syndrome in 50-year-old Swedish men and women with hypertension born in 1953. J. Hum. Hypertens. 2013, 27, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.L.; Hsu, M.Y.; Hu, C.C.; Tantoh, D.M.; Lu, W.Y.; Nfor, O.N.; Liaw, Y.P. Association of age and sex with metabolic syndrome in taiwanese adults. Int. J. Gen. Med. 2021, 14, 1403–1411. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.A.; Chey, T.; Merom, D.; Bauman, A.E. Occupational risk of overweight and obesity: An analysis of the Australian Health Survey. J. Occup. Med. Toxicol 2010, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.K.; Charles, L.E.; Bang, K.M.; Ma, C.C.; Andrew, M.E.; Violanti, J.M.; Burchfiel, C.M. Prevalence of obesity by occupation among US workers: The National Health Interview Survey 2004–2011. J. Occup. Env. Med. 2014, 56, 516–528. [Google Scholar] [CrossRef]
- Eum, M.J.; Jung, H.S. Association between occupational characteristics and overweight and obesity among Working Korean Women: The 2010–2015 Korea national health and nutrition examination survey. Int. J. Environ. Res. Public Health 2020, 17, 51585. [Google Scholar] [CrossRef]
- Van Zon, S.K.; Amick, B.C., III; de Jong, T.; Brouwer, S.; Bültmann, U. Occupational distribution of metabolic syndrome prevalence and incidence differs by sex and is not explained by age and health behavior: Results from 75,000 Dutch workers from 40 occupational groups. BMJ Open Diabetes Res. Care 2020, 8, e001436. [Google Scholar] [CrossRef]
- Virtanen, M.; Kivimäki, M. Long working hours and risk of cardiovascular disease. Curr. Cardiol. Rep. 2018, 20, 123. [Google Scholar] [CrossRef]
- Kobayashi, T.; Suzuki, E.; Takao, S. Long working hours and metabolic syndrome among Japanese men: A cross-sectional study. BMC Public Health 2012, 12, 395. [Google Scholar] [CrossRef]
- Itani, O.; Kaneita, Y.; Ikeda, M.; Kondo, S.; Murata, A.; Ohida, T. Associations of work hours and actual availability of weekly rest days with cardiovascular risk factors. J. Occup. Health 2013, 55, 11–20. [Google Scholar] [CrossRef]
- Yu, J. Relationship between long working hours and metabolic syndrome among Korean workers. Asian Nurs. Res. 2017, 11, 36–41. [Google Scholar] [CrossRef]
- Pimenta, A.M.; Bes-Rastrollo, M.; Sayon-Orea, C.; Gea, A.; Aguinaga-Ontoso, E.; Lopez-Iracheta, R.; Martinez-Gonzalez, M.A. Working hours and incidence of metabolic syndrome and its components in a Mediterranean cohort: The SUN project. Eur. J. Public Health 2015, 25, 683–688. [Google Scholar] [CrossRef]
- Ochiai, Y.; Takahashi, M.; Matsuo, T.; Sasaki, T.; Fukasawa, K.; Araki, T.; Tsuchiya, M.; Otsuka, Y. Objective and subjective working hours and their roles on workers’ health among Japanese employees. Ind. Health 2020, 58, 265–275. [Google Scholar] [CrossRef]
- Chowdhury, R.; Shah, D.; Payal, A.R. Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods—A Review. Indian J. Occup. Environ. Med. 2017, 21, 2–8. [Google Scholar] [CrossRef]
| Descriptive Statistics | Logistic Model, Reference: Group 3 | ||||||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | |||
| Variable | (n = 417) | (n = 264) | (n = 488) | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value |
| Age (years) | 38.2 ± 8.9 | 35.6 ± 9.2 | 33.0 ± 8.6 | ||||
| Age (years) | |||||||
| 20–40 | 200 (48.0) | 153 (58.0) | 340 (69.7) | Reference | Reference | ||
| ≥40 | 217 (52.0) | 111 (42.0) | 148 (30.3) | 2.39 (1.75–3.27) | <0.001 | 1.61 (1.15–2.27) | 0.006 |
| Male sex | 122 (29.3) | 41 (15.5) | 20 (4.1) | 12.24 (6.47–23.15) | <0.001 | 5.90 (2.92–11.94) | <0.001 |
| Alcohol consumption | 387 (92.8) | 251 (95.1) | 431 (88.3) | 1.36 (0.81–2.30) | 0.244 | 2.31 (1.22–4.39) | 0.010 |
| Working hours/week | 48.4 ± 12.0 | 45.7 ± 8.1 | 45.6 ± 8.8 | ||||
| Working hours/week | |||||||
| ≤40 | 161 (38.6) | 107 (40.5) | 212 (43.4) | Reference | Reference | ||
| 41–49 | 109 (26.1) | 83 (31.4) | 143 (29.3) | 1.00 (0.71–1.42) | 0.986 | 1.11 (0.77–1.60) | 0.578 |
| ≥50 | 147 (35.3) | 74 (28.0) | 133 (27.3) | 1.09 (0.76–1.55) | 0.647 | 0.91 (0.61–1.36) | 0.652 |
| Profession type | |||||||
| Nurse | 202 (48.4) | 166 (62.9) | 338 (69.3) | Reference | Reference | ||
| Physician | 72 (17.3) | 30 (11.4) | 34 (7.0) | 0.70 (0.37–1.35) | 0.291 | 0.69 (0.34–1.41) | 0.311 |
| Other medical staff | 54 (12.9) | 30 (11.4) | 41 (8.4) | 1.20 (0.74–1.95) | 0.460 | 1.03 (0.61–1.76) | 0.905 |
| Administrative staff | 89 (21.3) | 38 (14.4) | 75 (15.4) | 1.06 (0.71–1.57) | 0.787 | 0.72 (0.46–1.14) | 0.166 |
| Variable | Descriptive Statistics | Logistic Model, Reference: Group 1 | ||
|---|---|---|---|---|
| Group 1 (n = 936) | Group 2 (n = 233) | Adjusted OR (95% CI) | p-Value | |
| Age (years) | 34.7 ± 8.9 | 38.5 ± 9.4 | ||
| Age (years) | ||||
| 20–40 | 588 (62.8) | 105 (45.1) | Reference | |
| ≥40 | 348 (37.2) | 128 (54.9) | 1.80 (1.31–2.47) | <0.001 |
| Male sex | 136 (14.5) | 47 (20.2) | 1.66 (1.02–2.68) | 0.040 |
| Alcohol consumption | 845 (90.3) | 224 (96.1) | 2.04 (1.00–4.18) | 0.051 |
| Working hours/week | 46.9 ± 10.4 | 45.7 ± 7.8 | ||
| Working hours/week | ||||
| ≤40 | 378 (40.4) | 102 (43.8) | Reference | |
| 41–49 | 271 (29.0) | 64 (27.5) | 0.84 (0.59–1.21) | 0.358 |
| ≥50 | 287 (30.7) | 67 (28.8) | 0.83 (0.57–1.21) | 0.332 |
| Profession type | ||||
| Nurse | 584 (62.4) | 122 (52.4) | Reference | |
| Physician | 112 (12.0) | 24 (10.3) | 0.76 (0.40–1.43) | 0.391 |
| Other medical staff | 89 (9.5) | 36 (15.5) | 1.38 (0.87–2.20) | 0.171 |
| Administrative staff | 151 (16.1) | 51 (21.9) | 1.16 (0.78–1.74) | 0.460 |
| Variable | Descriptive Statistics | Logistic Model, Reference: Group 1 | ||
|---|---|---|---|---|
| Group 1 (n = 1014) | Group 2 (n = 155) | Adjusted OR (95% CI) | p-Value | |
| Age (years) | 35.6 ± 9.2 | 34.5 ± 8.5 | ||
| Age (years) | ||||
| 20–40 | 592 (58.4) | 101 (65.2) | Reference | |
| ≥40 | 422 (41.6) | 54 (34.8) | 0.71 (0.48–1.04) | 0.078 |
| Male sex | 159 (15.7) | 24 (15.5) | 1.06 (0.58–1.95) | 0.850 |
| Alcohol consumption | 927 (91.4) | 142 (91.6) | 1.15 (0.62–2.15) | 0.661 |
| Working hours/weeks | 46.4 ± 9.6 | 47.9 ± 11.9 | ||
| Working hours/weeks | ||||
| ≤40 | 422 (41.6) | 58(37.4) | Reference | |
| 41–49 | 287 (28.3) | 48 (31.0) | 1.25 (0.82–1.89) | 0.300 |
| ≥50 | 305 (30.1) | 49 (31.6) | 1.27 (0.82–1.97) | 0.289 |
| Profession type | ||||
| Nurse | 610 (60.2) | 96 (61.9) | Reference | |
| Physician | 118 (11.6) | 18 (11.6) | 0.85 (0.41–1.77) | 0.670 |
| Other medical staff | 106 (10.5) | 19 (12.3) | 1.25 (0.71–2.19) | 0.441 |
| Administrative staff | 180 (17.8) | 22 (14.2) | 0.87 (0.52–1.46) | 0.593 |
| Descriptive Statistics | Logistic Model, Reference: Group 1 | ||||||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 2 | Group 3 | |||
| Variable | (n = 769) | (n = 165) | (n = 235) | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value |
| Age (years) | 34.5 ± 9.1 | 35.2 ± 8.4 | 38.8 ± 8.9 | ||||
| Age (years) | |||||||
| 20–40 | 480 (62.4) | 107 (64.8) | 106 (45.1) | Reference | Reference | ||
| ≥40 | 289 (37.6) | 58 (35.2) | 129 (54.9) | 0.82 (0.56–1.21) | 0.314 | 2.07 (1.48–2.89) | <0.001 |
| Male sex | 68 (8.8) | 39 (23.6) | 76 (32.3) | 3.35 (1.89–5.93) | <0.001 | 5.42 (3.26–9.02) | <0.001 |
| Alcohol consumption | 696 (90.5) | 155 (93.9) | 218 (92.8) | 1.74 (0.86–3.51) | 0.122 | 1.14 (0.63–2.08) | 0.663 |
| Working hours/week | 45.7 ± 8.5 | 46.9 ± 11.3 | 49.5 ± 12.5 | ||||
| Working hours/week | |||||||
| ≤40 | 329 (42.8) | 68 (41.2) | 83 (35.3) | Reference | Reference | ||
| 41–49 | 224 (29.1) | 52 (31.5) | 59 (25.1) | 1.17 (0.78–1.77) | 0.440 | 1.07 (0.72–1.58) | 0.741 |
| ≥50 | 216 (28.1) | 45 (27.3) | 93 (39.6) | 0.92 (0.58–1.45) | 0.723 | 1.30 (0.88–1.91) | 0.188 |
| Profession type | |||||||
| Nurse | 498 (64.8) | 90 (54.5) | 118 (50.2) | Reference | Reference | ||
| Physician | 64 (8.3) | 25 (15.2) | 47 (20.0) | 0.97 (0.48–1.98) | 0.943 | 0.83 (0.44–1.56) | 0.561 |
| Other medical staff | 78 (10.1) | 25 (15.2) | 22 (9.4) | 1.42 (0.83–2.45) | 0.205 | 0.65 (0.36–1.14) | 0.133 |
| Administrative staff | 129 (16.8) | 25 (15.2) | 48 (20.4) | 0.90 (0.54–1.52) | 0.697 | 0.87 (0.56–1.35) | 0.544 |
| Metabolic and Obesity Phenotype/Latent Classes | BMI at Wave 1 | BMI at Wave 4 | Change (95% CI) | p-Value |
|---|---|---|---|---|
| MHNO | ||||
| Group 1 | 26.4 ± 3.9 | 27.3 ± 3.9 | 0.90 (0.68, 1.11) | <0.001 |
| Group 2 | 21.9 ± 2.3 | 23.3 ± 2.5 | 1.39 (1.12, 1.66) | <0.001 |
| Group 3 | 20.3 ± 2.0 | 21.1 ± 2.0 | 0.81 (0.68, 0.95) | <0.001 |
| MUNO | ||||
| Group 1 | 23.2 ± 4.2 | 24.2 ± 4.3 | 1.01 (0.88, 1.14) | <0.001 |
| Group 2 | 21.3 ± 1.9 | 22.1 ± 1.8 | 0.83 (0.63, 1.03) | <0.001 |
| MHOO | ||||
| Group 1 | 22.4 ± 4.0 | 23.3 ± 3.9 | 0.90 (0.78, 1.02) | <0.001 |
| Group 2 | 25.6 ± 2.5 | 27.1 ± 2.6 | 1.45 (1.09, 1.81) | <0.001 |
| MUOO | ||||
| Group 1 | 21.0 ± 2.4 | 21.7 ± 2.4 | 0.78 (0.66, 0.89) | <0.001 |
| Group 2 | 24.1 ± 2.4 | 26.6 ± 2.5 | 2.42 (2.11, 2.74) | <0.001 |
| Group 3 | 28.1 ± 3.8 | 28.7 ± 3.7 | 0.60 (0.27, 0.94) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, H.-Y.; Chang, J.-H.; Chang, Y.-F.; Wu, C.-H.; Yang, Y.-C. Metabolic and Obesity Phenotype Trajectories in Taiwanese Medical Personnel. Int. J. Environ. Res. Public Health 2022, 19, 8184. https://doi.org/10.3390/ijerph19138184
Chang H-Y, Chang J-H, Chang Y-F, Wu C-H, Yang Y-C. Metabolic and Obesity Phenotype Trajectories in Taiwanese Medical Personnel. International Journal of Environmental Research and Public Health. 2022; 19(13):8184. https://doi.org/10.3390/ijerph19138184
Chicago/Turabian StyleChang, Hsin-Yun, Jer-Hao Chang, Yin-Fan Chang, Chih-Hsing Wu, and Yi-Ching Yang. 2022. "Metabolic and Obesity Phenotype Trajectories in Taiwanese Medical Personnel" International Journal of Environmental Research and Public Health 19, no. 13: 8184. https://doi.org/10.3390/ijerph19138184
APA StyleChang, H.-Y., Chang, J.-H., Chang, Y.-F., Wu, C.-H., & Yang, Y.-C. (2022). Metabolic and Obesity Phenotype Trajectories in Taiwanese Medical Personnel. International Journal of Environmental Research and Public Health, 19(13), 8184. https://doi.org/10.3390/ijerph19138184






