Exploring the Role of Provider–Patient Communication in Women’s Sexual Health and Pre-Exposure Prophylaxis Care in the Primary Care Settings in New York State of the United States
Abstract
:1. Introduction
2. Materials and Methods
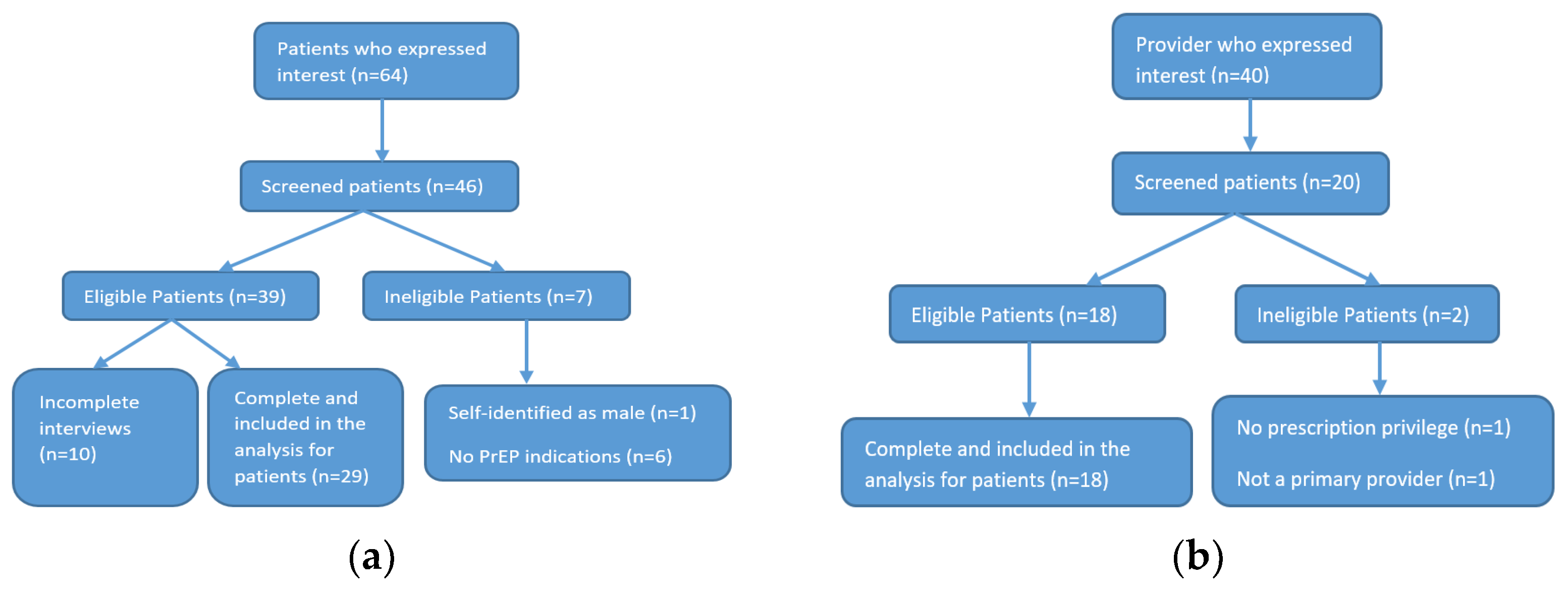
2.1. Participants’ Recruitment and Screening
2.2. Sample Size, Data Collection and Data Analysis
3. Results
3.1. Participants’ Characteristics
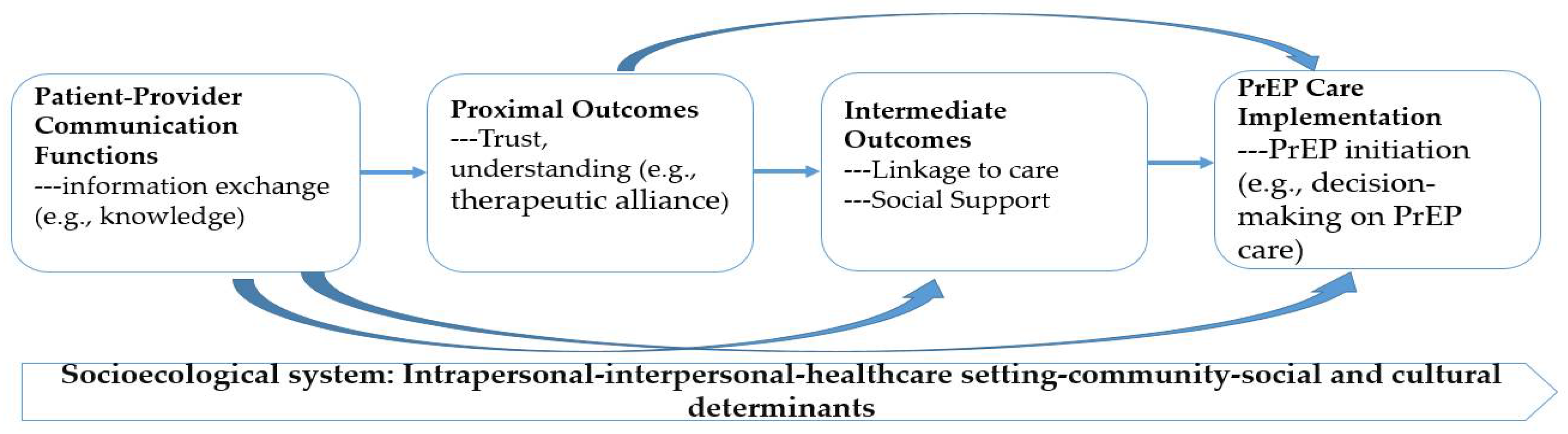
3.2. Key Findings Based upon the Framework
3.2.1. The Status of PrEP Care Implementation in the Primary Care Settings
Pathway via Patient Knowledge (i.e., PrEP Awareness and Perceived Risks) and Linkage to Care
“I would say um, I had a little less than moderate (risk of HIV infection), not super light…but, um, I’m—I don’t use drugs, and I’m not using it to contact those people who use drugs. I tend to have, um, other casual, sexual partners, I do not use condoms, and I just assume that the other person is safe, even though I don’t truly have everything condom using. I just assume that the person is safe enough for me to not use it. But it’s not based on any proof, or it’s not like I check specific for HIV negative. Yeah. It’s just a judgement on my part. I don’t know if their HIV—status is negative.”(women#22, 22 years)
“In my old practice, we had PrEP navigators that would actually kind of help on the back end of getting, um, you know, the PrEP app filled out, and any sort of, um, drug assistance programs that the patients might qualify for. But, that’s just not a resource that I have in my current practice. a lot of times if I am running into cost barriers, um, I do, um, end up just referring patients to a local practice that I know is much more capable of navigating that. it’s just a lot easier when you can kind of have all of that information right at the time of the visit.”(PCP#14, 38 years, female, family medicine)
“I think there is a misconception that only men who have sex with men should consider being on PrEP…it’s important when I talk to patients about it that, um, patients recognize that anyone is at risk for HIV who has any sexual activity. I pretty much talk about safe sex practices with all my patients regularly, not just at their health visits, but at many other visits as well… I don’t think I get immediate negative reactions from patients when I bring it up… I try to normalize the reaction by saying, you know, a lot of the messaging regarding PrEP has been to certain groups of people who we think might be more at risk for contracting HIV, but we know the risk of contracting HIV lies in anyone who has unprotected sex, which is why I bring it up with all my patients who are having unprotected sex.”(PCP#38, 29 years, female, family medicine)
Pathway through Establishing the Therapeutic Alliance and Facilitating Decision Making on PrEP Care
“PrEP is a fantastic harm reduction strategy. Um, and as a HIV provider, um, I find it incredibly useful for, um, patients who, um, potentially have partners, uh, who are sero-discordant, um, or in sero-discordant relationships to protect the partner. people who maybe, um, engaged in a little bit riskier behavior. Um, so that we can, uh, keep them healthy. Yes, there are some possible risks with it, but overall, in a young, healthy individual, um, the benefits of it often significantly outweigh the risks.”(PCP#14, 38 years, female, family medicine)
“…he (my PCP) was the one that discussed (PrEP)… At that time, he (my HIV-positive husband) wasn’t doin’ too well, so he (my PCP) was like, ‘Well, he doesn’t like usin’ condoms. You know, you have to use protection.’ He (my PCP) told me about Truvada. And it upset my stomach a little bit when I first, ‘, started usin’ it, you know, but then, after a while, I felt better about takin’ it…No, it wasn’t embarrassing, no…but he (my PCP) was like, you know, ‘You need to take care of yourself. You know, you need to take care of him too. If you’re not using condoms, this is the best thing I could give you, but, also, use condoms.’ and he (my PCP) gave me a pamphlet and stuff like that for me to read while I was sitting there, and then he explained it to me even more. And I decided right there and then, ‘Okay, fine. I will take it (PrEP)’, cause he (my PCP) was very open about it. You know, like I said, if it came different, I probably would’ve felt uncomfortable.”(women#20, 51 years)
3.2.2. Sexual Wellness and Sexual Health Exploration in the Primary Care Settings
“I had a new patient visit, um, a couple of days ago that, um—it was actually kinda easy because I asked—um, the patient had mentioned that he had a perianal strep infection. And so, um, you know, that was awkward for him, and-and it was a new patient visit, so I think that made it a little bit more awkward for him. And, um, that just kinda segued us into the discussion about sexual health, and I asked him, you know, “Have you heard of PrEP?” And he had been on it on the past. Um, asked him, you know, was he interested in restarting in it because he doesn’t have—he didn’t have a PCP. He was establishing PCP with me, and so he was-he was interested in restarting it., kind of an easy, um, discussion.”(PCP#15, 28 years, male, family medicine)
“I never heard of it (PrEP) except for in ads about HIV. And I thought it was more for people who have HIV or for people who were very greatly at risk. So I didn’t really put myself into those categories. And, um, I was—but, yeah. I feel like I have heard of PrEP, like on T.V. I don’t feel uncomfortable or anything. I would do something like that if it was something I felt was beneficial for me. I mean, I guess it would just be them either bringing it up or bringing up, like—like, if they said, like, ‘Have you ever heard of PrEP?’ Or like if they say something like, ‘It seems you’re at risk for HIV.’ at that point, I would probably go, ‘Is there anything I can do about it?’ Or “What is PrEP?” Like, I guess those would be the two things that would make me to think about it.”(women#32, 21 years)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- HIV.gov. The Global HIV/AIDS Epidemic. 2021. Available online: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics (accessed on 20 April 2022).
- CDC. Estimated HIV Incidence and Prevalence in the United States 2015–2019; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2021; Volume 26.
- Baeten, J.M.; Donnell, D.; Ndase, P.; Mugo, N.R.; Campbell, J.D.; Wangisi, J.; Tappero, J.W.; Bukusi, E.A.; Cohen, C.R.; Katabira, E.; et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 2012, 367, 399–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delaugerre, C.; Antoni, G.; Mahjoub, N.; Pialoux, G.; Cua, E.; Pasquet, A.; Hall, N.; Tremblay, C.; Cotte, L.; Capitant, C.; et al. Assessment of HIV Screening Tests for Use in Preexposure Prophylaxis Programs. J. Infect. Dis. 2017, 216, 382–386. [Google Scholar] [CrossRef] [PubMed]
- McCormack, S.; Dunn, D.T.; Desai, M.; Dolling, D.I.; Gafos, M.; Gilson, R.; Sullivan, A.K.; Clarke, A.; Reeves, I.; Schembri, G.; et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): Effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet 2016, 387, 53–60. [Google Scholar] [CrossRef] [Green Version]
- Molina, J.M.; Charreau, I.; Spire, B.; Cotte, L.; Chas, J.; Capitant, C.; Tremblay, C.; Rojas-Castro, D.; Cua, E.; Pasquet, A.; et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: An observational cohort study. Lancet HIV 2017, 4, E402–E410. [Google Scholar] [CrossRef] [Green Version]
- Morton, J.F.; Celum, C.; Njoroge, J.; Nakyanzi, A.; Wakhungu, I.; Tindimwebwa, E.; Ongachi, S.; Sedah, E.; Okwero, E.; Ngure, K.; et al. Counseling Framework for HIV-Serodiscordant Couples on the Integrated Use of Antiretroviral Therapy and Pre-exposure Prophylaxis for HIV Prevention. J. Acquir. Immune Defic. Syndr. 2017, 74 (Suppl. S1), S15–S22. [Google Scholar] [CrossRef] [Green Version]
- Bailey, J.L.; Molino, S.T.; Vega, A.D.; Badowski, M. A Review of HIV Pre-Exposure Prophylaxis: The Female Perspective. Infect. Dis. Ther. 2017, 6, 363–382. [Google Scholar] [CrossRef] [Green Version]
- Gilead. HIV Prevention with Your Patients’ Tomorrow in Mind. 2019. Available online: https://www.descovyhcp.com/about-descovy-for-prep?utm_medium=cpc&utm_campaign=71700000058222423&utm_content=Truvada_KW&utm_term=%2BTruvada&utm_source=google&gclid=CjwKCAiAqqTuBRBAEiwA7B66hdFmxPyRlcCossE6dhjoVk0DZEJ2UmdumCKMwrvnZ31-PpCvoSYNbxoCVMgQAvD_BwE&gclsrc=aw.ds (accessed on 12 November 2019).
- USPSTF. Draft Recommendation Statement: Prevention of Human Immunodeficiency Virus (HIV) Infection: Pre-Exposure Prophylaxis. U.S. 2018. Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis (accessed on 30 April 2019).
- Haberer, J.E.; Bangsberg, D.R.; Baeten, J.M.; Curran, K.; Koechlin, F.; Amico, K.R.; Anderson, P.; Mugo, N.; Venter, F.; Goicochea, P.; et al. Defining success with HIV pre-exposure prophylaxis: A prevention-effective adherence paradigm. AIDS 2015, 29, 1277–1285. [Google Scholar] [CrossRef]
- Smith, D.K.; Van Handel, M.; Wolitski, R.J.; Stryker, J.E.; Hall, H.I.; Prejean, J.; Koenig, L.J.; Valleroy, L.A. Vital Signs: Estimated Percentages and Numbers of Adults with Indications for Preexposure Prophylaxis to Prevent HIV Acquisition—United States, 2015. J. Miss. State Med. Assoc. 2015, 56, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Siegler, A.J.; Mehta, C.C.; Mouhanna, F.; Giler, R.M.; Castel, A.; Pembleton, E.; Jaggi, C.; Jones, J.; Kramer, M.R.; McGuinness, P.; et al. Policy- and county-level associations with HIV pre-exposure prophylaxis use, the United States, 2018. Ann. Epidemiol. 2020, 45, 24–31.e23. [Google Scholar] [CrossRef]
- Kamitani, E.; Johnson, W.D.; Wichser, M.E.; Adegbite, A.H.; Mullins, M.M.; Sipe, T.A. Growth in Proportion and Disparities of HIV PrEP Use Among Key Populations Identified in the United States National Goals: Systematic Review and Meta-analysis of Published Surveys. J. Acquir. Immune Defic. Syndr. 2020, 84, 379–386. [Google Scholar] [CrossRef]
- AIDSVu. State-level PrEP Utilization Data Now Available from AIDSVu. 2020. Available online: https://www.hiv.gov/blog/state-level-prep-utilization-data-now-available-aidsvu (accessed on 10 September 2020).
- CDC. HIV and Women; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Alexander, K.A.; Coleman, C.L.; Deatrick, J.A.; Jemmott, L.S. Moving beyond safe sex to women-controlled safe sex: A concept analysis. J. Adv. Nurs. 2012, 68, 1858–1869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaler, A. The female condom in North America: Selling the technology of ‘empowerment. J. Gend. Stud. 2004, 13, 139–152. [Google Scholar] [CrossRef]
- Higgins, J.A.; Hoffman, S.; Dworkin, S.L. Rethinking gender, heterosexual men, and women’s vulnerability to HIV/AIDS. Am. J. Public Health 2010, 100, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Bekker, L.G.; Johnson, L.; Cowan, F.; Overs, C.; Besada, D.; Hillier, S.; Cates, W., Jr. Combination HIV prevention for female sex workers: What is the evidence? Lancet 2015, 385, 72–87. [Google Scholar] [CrossRef]
- Hanscom, B.; Janes, H.E.; Guarino, P.D.; Huang, Y.; Brown, E.R.; Chen, Y.Q.; Hammer, S.M.; Gilbert, P.B.; Donnell, D.J. Brief Report: Preventing HIV-1 Infection in Women Using Oral Preexposure Prophylaxis: A Meta-analysis of Current Evidence. J. Acquir. Immune Defic. Syndr. 2016, 73, 606–608. [Google Scholar] [CrossRef] [Green Version]
- Headley, J.; Lemons, A.; Corneli, A.; Agot, K.; Ahmed, K.; Wang, M.; Odhiambo, J.; Skhosana, J.; Tharaldson, J.; Van Damme, L.; et al. The sexual risk context among the FEM-PrEP study population in Bondo, Kenya and Pretoria, South Africa. PLoS ONE 2014, 9, e106410. [Google Scholar] [CrossRef] [Green Version]
- Luecke, E.H.; Cheng, H.; Woeber, K.; Nakyanzi, T.; Mudekunye-Mahaka, I.C.; van der Straten, A. Stated product formulation preferences for HIV pre-exposure prophylaxis among women in the VOICE-D (MTN-003D) study. J. Int. AIDS Soc. 2016, 19, 20875. [Google Scholar] [CrossRef]
- Grant, R.M.; Lama, J.R.; Anderson, P.L.; McMahan, V.; Liu, A.Y.; Vargas, L.; Goicochea, P.; Casapia, M.; Guanira-Carranza, J.V.; Ramirez-Cardich, M.E.; et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 2010, 363, 2587–2599. [Google Scholar] [CrossRef] [Green Version]
- Liu, A.Y.; Cohen, S.E.; Vittinghoff, E.; Anderson, P.L.; Doblecki-Lewis, S.; Bacon, O.; Chege, W.; Postle, B.S.; Matheson, T.; Amico, K.R.; et al. Preexposure Prophylaxis for HIV Infection Integrated With Municipal- and Community-Based Sexual Health Services. JAMA Intern. Med. 2016, 176, 75–84. [Google Scholar] [CrossRef] [Green Version]
- Yun, K.; Xu, J.J.; Zhang, J.; Li, J.M.; Hu, Q.H.; Chu, Z.X.; Jiang, Y.J.; Geng, W.Q.; Shang, H.; Wang, N. Female and younger subjects have lower adherence in PrEP trials: A meta-analysis with implications for the uptake of PrEP service to prevent HIV. Sex. Transm. Infect. 2017, 94, 163–168. [Google Scholar] [CrossRef] [Green Version]
- Cairns, G.; McCormack, S.; Molina, J.M. The European preexposure prophylaxis revolution. Curr. Opin. HIV AIDS 2016, 11, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Nunn, A.S.; Brinkley-Rubinstein, L.; Oldenburg, C.E.; Mayer, K.H.; Mimiaga, M.; Patel, R.; Chan, P.A. Defining the HIV pre-exposure prophylaxis care continuum. AIDS 2017, 31, 731–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, C.; McMahon, J.; Fiscella, K.; Przybyla, S.; Braksmajer, A.; LeBlanc, N.; Liu, Y. HIV pre-exposure prophylaxis implementation cascade among health care professionals in the United States: Implications from a systematic review and meta-analysis. AIDS Patient Care STDs 2019, 33, 507–527. [Google Scholar] [CrossRef] [PubMed]
- Przybyla, S.; LaValley, S.; St Vil, N. Health Care Provider Perspectives on Pre-exposure Prophylaxis: A Qualitative Study. J. Assoc. Nurses AIDS Care JANAC 2019, 30, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; McMahon, J.; LeBlanc, N.; Braksmajer, A.; Crean, H.; Alcena-Stiner, D. Poor communication and mistrust with health care provides among urban-dwelling HIV positive men of color. AIDS Patient Care STDs, 2019; in press. [Google Scholar]
- Brindley, P.G.; Smith, K.E.; Cardinal, P.; LeBlanc, F. Improving medical communication with patients and families: Skills for a complex (and multilingual) clinical world. Can. Respir. J. 2014, 21, 89–91. [Google Scholar] [CrossRef]
- Street, R.L., Jr.; Makoul, G.; Arora, N.K.; Epstein, R.M. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ. Couns. 2009, 74, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Griffin, S.J.; Kinmonth, A.L.; Veltman, M.W.; Gillard, S.; Grant, J.; Stewart, M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: A systematic review of trials. Ann. Fam. Med. 2004, 2, 595–608. [Google Scholar] [CrossRef] [Green Version]
- Ashton, C.M.; Haidet, P.; Paterniti, D.A.; Collins, T.C.; Gordon, H.S.; O’Malley, K.; Petersen, L.A.; Sharf, B.F.; Suarez-Almazor, M.E.; Wray, N.P.; et al. Racial and ethnic disparities in the use of health services: Bias, preferences, or poor communication? J. Gen. Intern. Med. 2003, 18, 146–152. [Google Scholar] [CrossRef] [Green Version]
- Viswanath, K.; Kreuter, M.W. Health disparities, communication inequalities, and eHealth. Am. J. Prev. Med. 2007, 32, S131–S133. [Google Scholar] [CrossRef] [Green Version]
- Wilson, K.; Bleasdale, J.; Przybyla, S.M. Provider-Patient Communication on Pre-Exposure Prophylaxis (Prep) for HIV Prevention: An Exploration of Healthcare Provider Challenges. Health Commun. 2021, 36, 1677–1686. [Google Scholar] [CrossRef]
- CDC. US Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: Clinical Providers’ Supplement; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018.
- CDC. Prescribe HIV Prevention. 2018. Available online: https://npin.cdc.gov/publication/prescribe-hiv-prevention (accessed on 2 September 2021).
- Townsend, K. How many interviews are enough? Do qualitative interviews in building energy consumption research produce reliable knowledge? J. Build. Eng. 2015, 1, 2–12. [Google Scholar] [CrossRef]
- Sandelowski, M. Sample size in qualitative research. Res. Nurs. Health 1995, 18, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 2018, 18, 148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual. Health Res. 2015, 26, 1753–1760. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. What can “thematic analysis” offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well-Being 2014, 9, 26152. [Google Scholar] [CrossRef] [Green Version]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Srivastava, P.; Hopwood, N. A Practical Iterative Framework for Qualitative Data Analysis. Int. J. Qual. Methods 2009, 8, 76–84. [Google Scholar] [CrossRef] [Green Version]
- de Haes, H.; Teunissen, S. Communication in palliative care: A review of recent literature. Curr. Opin. Oncol. 2005, 17, 345–350. [Google Scholar] [CrossRef] [Green Version]
- Putnam, S.M.; Stiles, W.B.; Jacob, M.C.; James, S.A. Patient exposition and physician explanation in initial medical interviews and outcomes of clinic visits. Med. Care 1985, 23, 74–83. [Google Scholar] [CrossRef]
- Smets, E.; van Zwieten, M.; Michie, S. Comparing genetic counseling with non-genetic health care interactions: Two of a kind? Patient Educ. Couns. 2007, 68, 225–234. [Google Scholar] [CrossRef]
- Kelley, C.F.; Kahle, E.; Siegler, A.; Sanchez, T.; Del Rio, C.; Sullivan, P.S.; Rosenberg, E.S. Applying a PrEP Continuum of Care for Men Who Have Sex With Men in Atlanta, Georgia. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015, 61, 1590–1597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makoul, G.; Clayman, M.L.; Lynch, E.B.; Thompson, J.A. Four concepts of health in America: Results of national surveys. J. Health Commun. 2009, 14, 3–14. [Google Scholar] [CrossRef]
- Charles, C.; Gafni, A.; Whelan, T. Decision-making in the physician-patient encounter: Revisiting the shared treatment decision-making model. Soc. Sci. Med. 1999, 49, 651–661. [Google Scholar] [CrossRef]
- Fuertes, J.N.; Mislowack, A.; Bennett, J.; Paul, L.; Gilbert, T.C.; Fontan, G.; Boylan, L.S. The physician-patient working alliance. Patient Educ. Couns. 2007, 66, 29–36. [Google Scholar] [CrossRef]
- Visser, A.; Rehman, S.; Makoul, G. Patient education and counseling. Editorial. Patient Educ. Couns. 2008, 72, 357–358. [Google Scholar] [CrossRef] [PubMed]
- Aidoo-Frimpong, G.; Wilson, K.; Przybyla, S. Factors influencing pre-exposure prophylaxis uptake among current users: A qualitative study. J. HIV/AIDS Soc. Serv. 2020, 19, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. CMAJ Can. Med. Assoc. J. J. De L’association Med. Can. 1995, 152, 1423–1433. [Google Scholar]
- Bharel, M.; Lin, W.C.; Zhang, J.; O’Connell, E.; Taube, R.; Clark, R.E. Health care utilization patterns of homeless individuals in Boston: Preparing for Medicaid expansion under the Affordable Care Act. Am. J. Public Health 2013, 103 (Suppl. S2), S311–S317. [Google Scholar] [CrossRef]
- Zhang, C.; Przybylek, S.; Braksmajer, A.; Liu, Y. An Integrated Conceptual Framework of Behavioral Intervention Technologies to Promote Healthcare Utilization Among Socially-Marginalized Populations in the United States. J. Nurs. Stud. Patient Care, 2022; in press. [Google Scholar]
- Epstein, R.M.; Alper, B.S.; Quill, T.E. Communicating evidence for participatory decision making. JAMA 2004, 291, 2359–2366. [Google Scholar] [CrossRef]
- Hunt, L.M.; Castañeda, H.; KB, D.E.V. Do notions of risk inform patient choice? Lessons from a study of prenatal genetic counseling. Med. Anthropol. 2006, 25, 193–219. [Google Scholar] [CrossRef]
- Lipkus, I.M. Numeric, verbal, and visual formats of conveying health risks: Suggested best practices and future recommendations. Med. Decis. Mak. Int. J. Soc. Med. Decis. Mak. 2007, 27, 696–713. [Google Scholar] [CrossRef] [PubMed]
- Meyer, D.; Leventhal, H.; Gutmann, M. Common-sense models of illness: The example of hypertension. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 1985, 4, 115–135. [Google Scholar] [CrossRef]
- Cahill, S.; Taylor, S.W.; Elsesser, S.A.; Mena, L.; Hickson, D.; Mayer, K.H. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care 2017, 29, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.T.; Bussell, J.; Dutta, S.; Davis, K.; Strong, S.; Mathew, S. Medication Adherence: Truth and Consequences. Am. J. Med. Sci. 2016, 351, 387–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rose, A.; Peters, N.; Shea, J.A.; Armstrong, K. Development and testing of the health care system distrust scale. J. Gen. Intern. Med. 2004, 19, 57–63. [Google Scholar] [CrossRef] [Green Version]
- Calabrese, S.K.; Krakower, D.S.; Mayer, K.H. Integrating HIV Preexposure Prophylaxis (PrEP) Into Routine Preventive Health Care to Avoid Exacerbating Disparities. Am. J. Public Health 2017, 107, 1883–1889. [Google Scholar] [CrossRef]
- Smith, D.K.; Chang, M.H.; Duffus, W.A.; Okoye, S.; Weissman, S. Missed Opportunities to Prescribe Preexposure Prophylaxis in South Carolina, 2013–2016. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019, 68, 37–42. [Google Scholar] [CrossRef] [Green Version]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2008, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- CDC. HIV in the Southern United States; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019.
- Tekeste, M.; Hull, S.; Dovidio, J.F.; Safon, C.B.; Blackstock, O.; Taggart, T.; Kershaw, T.S.; Kaplan, C.; Caldwell, A.; Lane, S.B.; et al. Differences in Medical Mistrust Between Black and White Women: Implications for Patient-Provider Communication About PrEP. AIDS Behav. 2019, 23, 1737–1748. [Google Scholar] [CrossRef]
| Primary Care Providers (n = 18) | PrEP-Eligible Women (n = 29) | ||
|---|---|---|---|
| Age (mean, * SD; range) | 42.4 (SD = 12.9; 28–68) | Age (mean, * SD; range) | 38.1 (SD = 15.1; 20–61) |
| Year of Practice (mean, * SD; range) | 9.0 (SD = 10.9; 1–40) | ||
| Gender (n, %) | Number of sex partnership (mean, * SD; range) | 1.6 (SD = 1.1; 0–5) | |
| Male | 4 (30.7%) | ||
| Female | 13 (72.2%) | Sex without condoms (n, %) | 23 (79.3%) |
| Others | 1 (5.6%) | ||
| Race/Ethnicity (n, %) | Living with HIV positive partners (n, %) | 6 (20.7%) | |
| White | 17 (94.4%) | ||
| Black | 1 (5.6%) | Reported sexually transmitted infections in the past 6 months (n, %) | 2 (6.9%) |
| Practice Places (n, %) | |||
| Hospital-based | 13 (72.2%) | Ever used substances (e.g., alcohol, cocaine, or other drugs) (n, %) | 5 (17.2%) |
| Federally qualified health center | 3 (16.7%) | ||
| Group practice | 3 (16.7%) | Ever injected drugs (n, %) | 7 (24.1%) |
| Kaiser Permanente | 2 (11.1%) | ||
| Primary Specialty (n, %) | Ever had HIV testing (n, %) | 20 (69.0%) | |
| Family Medicine | 10 (55.6%) | ||
| Primary care | 7 (38.9%) | Ever used PrEP (n, %) | 3 (10.3%) |
| Internal Medicine | 3 (16.7%) | ||
| Infectious Disease | 2 (11.1%) | ||
| Adolescent Health | 1 (5.6%) | ||
| Thematic Domains | Specific Pathways |
|---|---|
| 3.2.1 Provider–patient communication and PrEP care implementation | Via Patient knowledge (i.e., informational exchange) |
| Via Therapeutic alliance (i.e., proximal outcomes) | |
| Via Linkage to care (i.e., intermediate outcomes) | |
| Via Decision making on PrEP care (PrEP implementation) | |
| 3.2.2 Discussion paradox | Initiation of the PrEP care |
| Sexual wellness exploration |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Fiscella, K.; Liu, Y. Exploring the Role of Provider–Patient Communication in Women’s Sexual Health and Pre-Exposure Prophylaxis Care in the Primary Care Settings in New York State of the United States. Int. J. Environ. Res. Public Health 2022, 19, 8084. https://doi.org/10.3390/ijerph19138084
Zhang C, Fiscella K, Liu Y. Exploring the Role of Provider–Patient Communication in Women’s Sexual Health and Pre-Exposure Prophylaxis Care in the Primary Care Settings in New York State of the United States. International Journal of Environmental Research and Public Health. 2022; 19(13):8084. https://doi.org/10.3390/ijerph19138084
Chicago/Turabian StyleZhang, Chen, Kevin Fiscella, and Yu Liu. 2022. "Exploring the Role of Provider–Patient Communication in Women’s Sexual Health and Pre-Exposure Prophylaxis Care in the Primary Care Settings in New York State of the United States" International Journal of Environmental Research and Public Health 19, no. 13: 8084. https://doi.org/10.3390/ijerph19138084
APA StyleZhang, C., Fiscella, K., & Liu, Y. (2022). Exploring the Role of Provider–Patient Communication in Women’s Sexual Health and Pre-Exposure Prophylaxis Care in the Primary Care Settings in New York State of the United States. International Journal of Environmental Research and Public Health, 19(13), 8084. https://doi.org/10.3390/ijerph19138084








