Managing Minds at Work: Development of a Digital Line Manager Training Program
Abstract
:1. Introduction
2. Methods
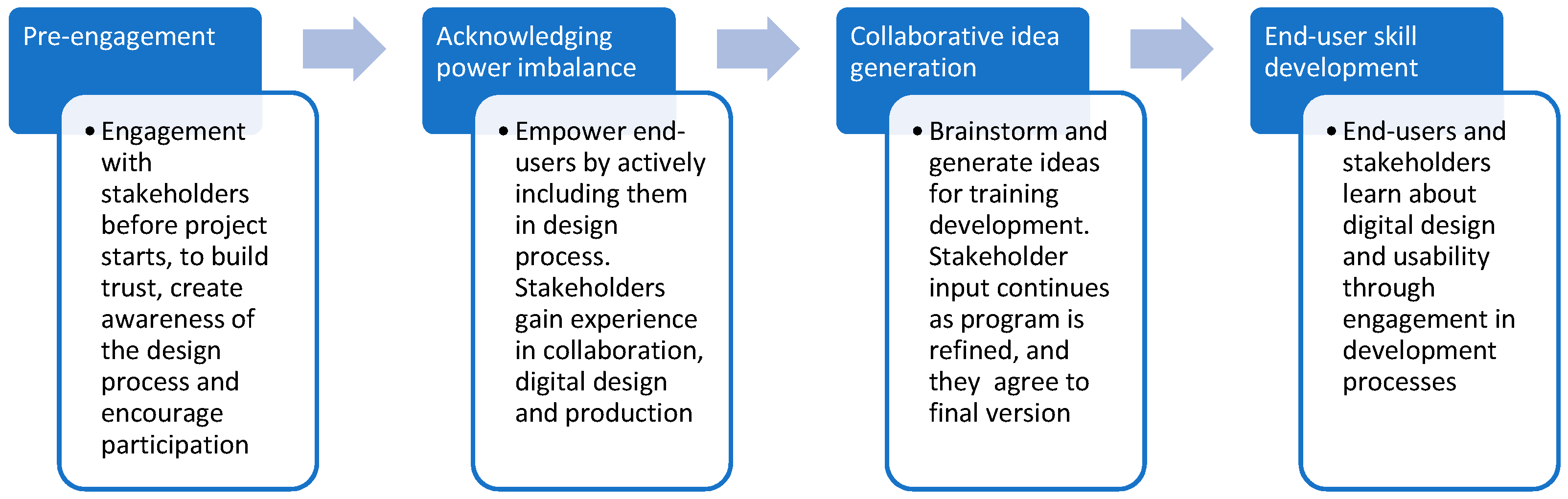
2.1. Design
2.2. Procedure
- Order of modules and materials.
- Frequency and timing of module delivery.
- Content revisions (additions/removals).
- Targeting of information (e.g., specific/generic).
- What are the barriers that could prevent line managers from accessing/engaging in the training?
- What are the facilitators that could support line managers in completing the training?
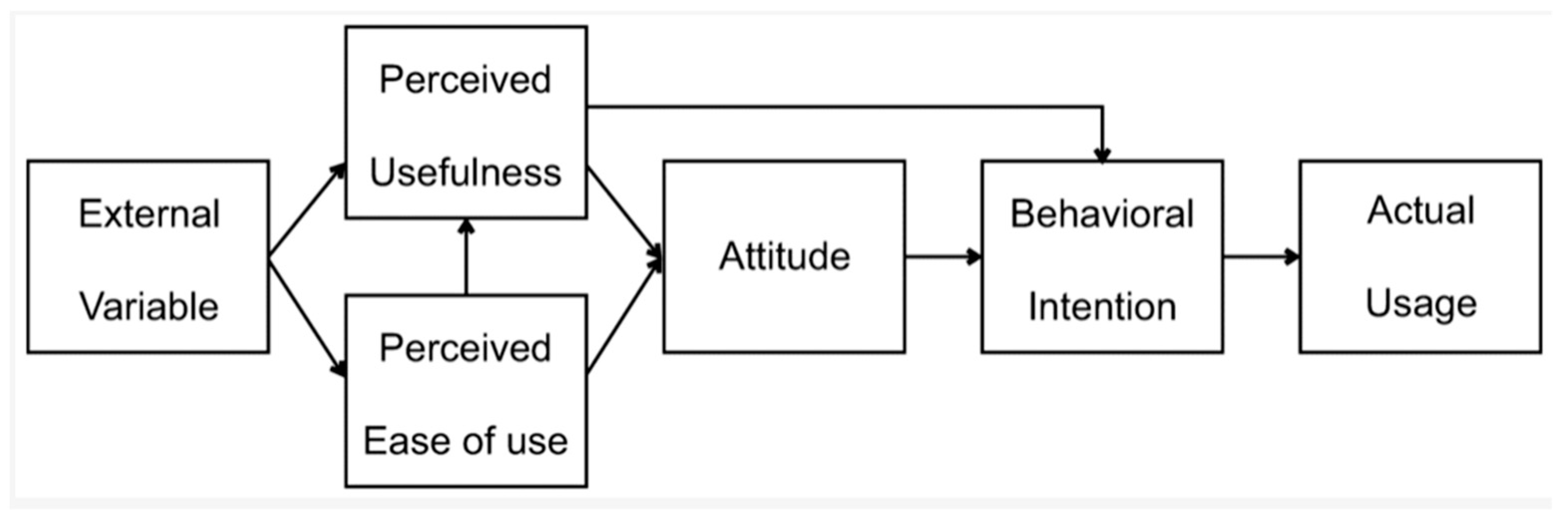
2.3. Usability and Pilot Testing
3. Results
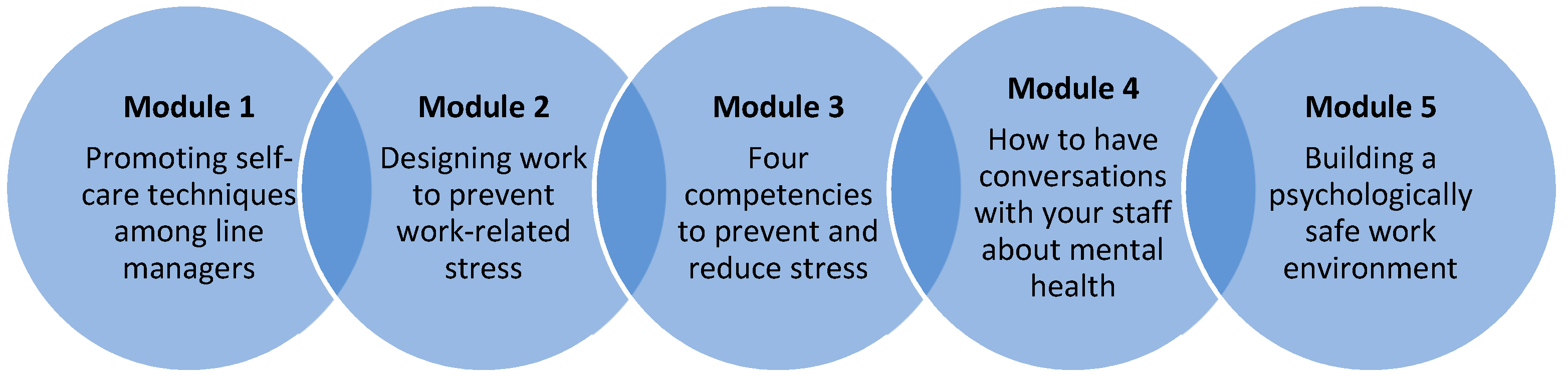
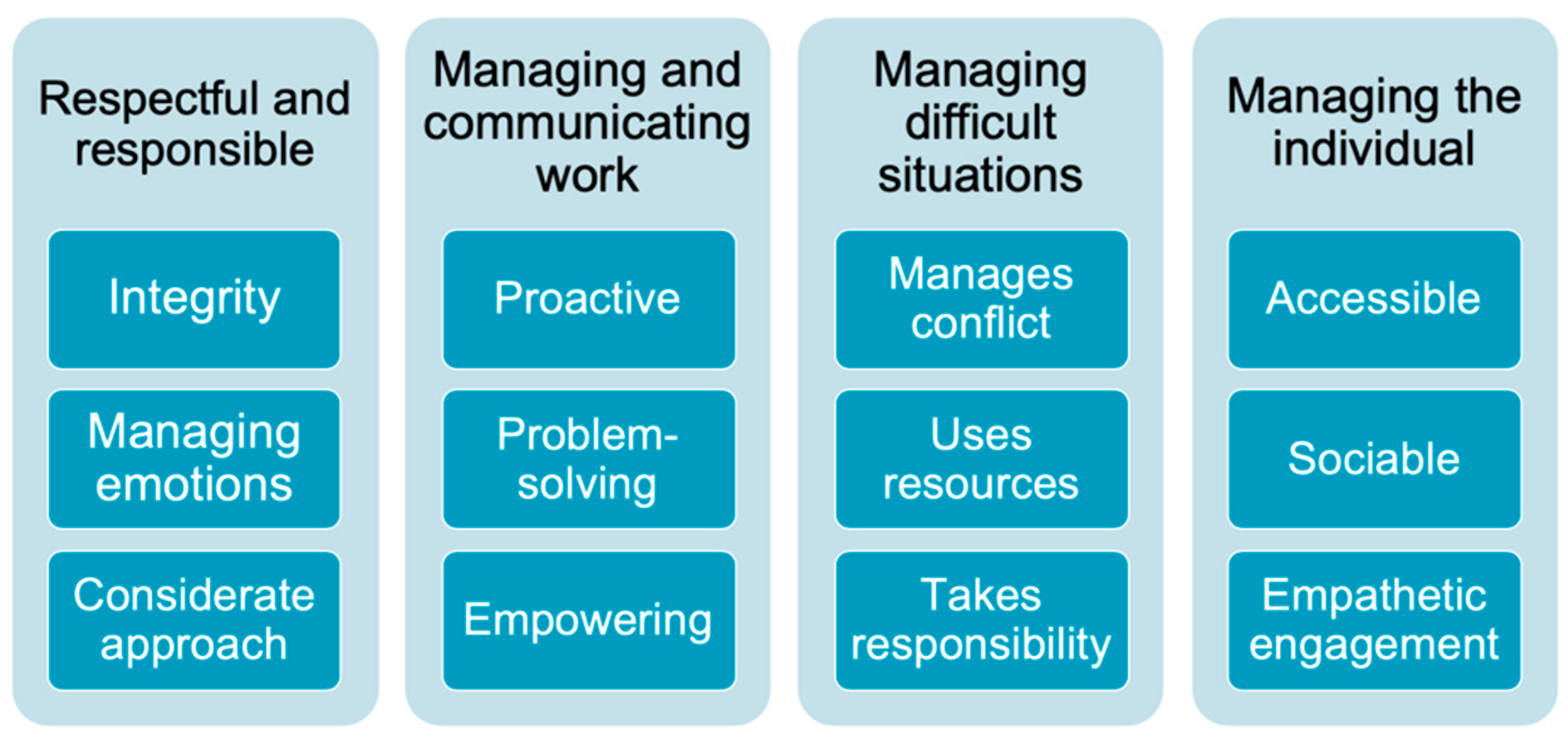
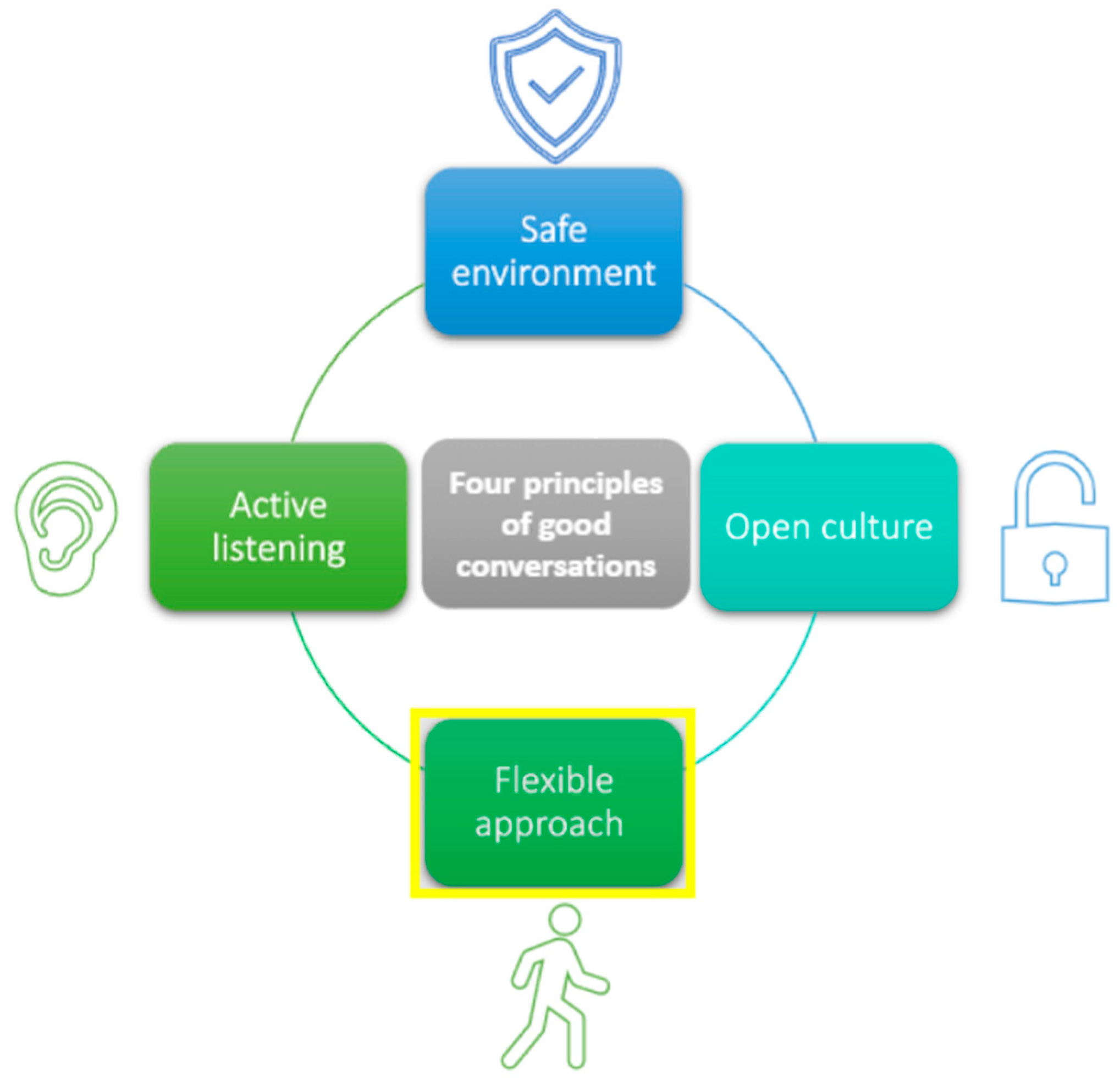
3.1. Managing Minds at Work Intervention
“Managing Minds at Work will develop line manager’s knowledge and confidence in preventing work-related stress and promoting mental health at work. This will be achieved through learning activities to increasing line managers’’ awareness of mental health (including legal requirements and employer responsibilities around work-related stress), encouraging the creation of psychologically safe working environments and work designs that promote mental wellbeing, and increasing managers’ competencies in preventing work-related stress and having open conversations about mental health in the workplace. Ultimately, the longer-term outcomes of this will be to reduce the prevalence of mental ill-health in working-age adults, and related economic burden of presenteeism and sickness absence to individuals, employers, and society”.
3.2. Usability and Pilot Testing Results
“It’s given me a better understanding of the different sources of stress for colleagues and subordinates. I’ll be sure to be more considerate of the different factors in my approach going forward”.
“I have underestimated how important it is that I look after myself. The information in the module makes sense in that you cannot support others if you aren’t in a good place yourself”.
“a good reminder of the need to take care of yourself”.
“It was useful to learn about breaking down the job demands into areas I can easily understand. This will help me to help my team”.
“I think, as the manager I need to have all the answers but it’s important to share problems with the team”.
“I will make an effort to ensure that both my team and I are more conscious about the things we say and how we say them”.
“Made me rethink how to approach people - and the boundaries of things I might ask about”
“I had heard of psychological safety but didn’t really know what it was. I can now make more effort to ensure we have psychological safety in the team”.
“the more conversations I have, the easier it is to talk about mental health”.
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Health and Safety Executive (HSE). Work Related Stress, Anxiety and Depression Statistics in Great Britain. 2019. Available online: https://www.hse.gov.uk/statistics/causdis/stress.pdf (accessed on 23 May 2022).
- Deloitte. Mental Health and Employers: The Case for Investment-Pandemic and Beyond. September–October 2021. Available online: https://www2.deloitte.com/uk/en/pages/consulting/articles/mental-health-and-employers-the-case-for-investment.html (accessed on 5 April 2022).
- Butterworth, P.; Leach, L.S.; Pirkis, J.; Kelaher, M. Poor mental health influences risk and duration of unemployment: A prospective study. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 47, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassard, J.; Teoh, K.; Thomson, L.; Blake, H. Understanding the cost of mental ill-health at work: An integrative framework. In The SAGE Handbook of Organizational Wellbeing; Wall, T., Cooper, C.L., Brough, P., Eds.; SAGE Publications, Ltd.: London, UK, 2021. [Google Scholar]
- Hassard, J.; Teoh, K.R.H.; Visockaite, G.; Dewe, P.; Cox, T. The cost of work-related stress to society: A systematic review. J. Occup. Health Psychol. 2018, 23, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EOSHA. Psychosocial Risks in Europe: Prevalence and Strategies for Prevention; Publications Office of the European Union: Luxembourg, 2014. [Google Scholar]
- Carbone, S.R. Flattening the curve of mental ill-health: The importance of primary prevention in managing the mental health impacts of COVID-19. Ment. Health Prev. 2020, 19, 200185. [Google Scholar] [CrossRef] [PubMed]
- Joyce, J. Facing the challenge of mental ill health in the workplace. J. Public Ment. Health 2013, 12, 93–97. [Google Scholar] [CrossRef]
- Newman, S.A.; Ford, R.C. Five Steps to Leading Your Team in the Virtual COVID-19 Workplace. Organ. Dyn. 2021, 50, 100802. [Google Scholar] [CrossRef]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef] [Green Version]
- Martin, A.; Woods, M.; Dawkins, S. How managers experience situations involving employee mental ill-health. Int. J. Work. Health Manag. 2018, 11, 442–463. [Google Scholar] [CrossRef]
- Davenport, L.J.; Allisey, A.F.; Page, K.M.; LaMontagne, A.D.; Reavley, N.J. How can organizations help employees thrive? The de-velopment of guidelines for promoting positive mental health at work. Int. J. Work. Health Manag. 2016, 9, 411–427. [Google Scholar] [CrossRef]
- Dextras-Gauthier, J.; Marchand, A.; Haines, V., III. Organizational culture, work organization conditions, and mental health: A proposed integration. Int. J. Stress Manag. 2012, 19, 81–104. [Google Scholar] [CrossRef]
- Edmondson, A.D. The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2019. [Google Scholar]
- Nexø, M.A.; Kristensen, J.V.; Grønvad, M.T.; Kristiansen, J.; Poulsen, O.M. Content and quality of workplace guidelines developed to prevent mental health problems: Results from a systematic review. Scand. J. Work. Environ. Health 2018, 44, 443–457. [Google Scholar] [CrossRef] [PubMed]
- Dimoff, J.K.; Kelloway, E.K. With a little help from my boss: The impact of workplace mental health training on leader behaviors and employee resource utilization. J. Occup. Health Psychol. 2019, 24, 4–19. [Google Scholar] [CrossRef] [PubMed]
- Gayed, A.; Milligan-Saville, J.S.; Nicholas, J.; Bryan, B.T.; La Montagne, A.D.; Milner, A.; Madan, I.; Calvo, R.A.; Christensen, H.; Mykletun, A.; et al. Effectiveness of training workplace managers to understand and support the mental health needs of employees: A systematic review and meta-analysis. Occup. Environ. Med. 2018, 75, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Institute for Occupational Safety and Health. White Paper—Workplace Wellbeing: The Role of Line Managers in Promoting Positive Nental Health. Management Today. 2019. Available online: https://iosh.com/media/4174/managing-occ-health-the-role-of-line-managers-in-promoting-positive-mental-health.pdf (accessed on 20 April 2022).
- Weston, D.; Hudson, C.; Carroll, D.; Coomber, S.; Amlôt, R. Evaluating a pilot mental health awareness for managers’ training course. Occup. Med. 2019, 69, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Gayed, A.; Bryan, B.T.; LaMontagne, A.D.; Milner, A.; Deady, M.; Calvo, R.A.; MacKinnon, A.; Christensen, H.; Mykletun, A.; Glozier, N.; et al. A cluster randomized controlled trial to evaluate HeadCoach: An online mental health training programme for workplace managers. Occup. Environ. Med. 2019, 61, 545–551. [Google Scholar] [CrossRef] [Green Version]
- Dimoff, J.K.; Kelloway, E.K.; Burnstein, M.D. Mental health awareness training (MHAT): The development and evaluation of an intervention for workplace leaders. Int. J. Stress Manag. 2016, 23, 167–189. [Google Scholar] [CrossRef]
- Milligan-Saville, J.S.; Tan, L.; Gayed, A.; Barnes, C.; Madan, I.; Dobson, M.; A Bryant, R.A.; Christensen, H.; Mykletun, A.; Harvey, S.B. Workplace mental health training for managers and its effect on sick leave in employees: A cluster randomised controlled trial. Lancet Psychiatry 2017, 4, 850–858. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Kerry, S.; Chandola, T.; Russell, J.; Berney, L.; Hounsome, N.; Lanz, D.; Costelloe, C.; Smuk, M.; Bhui, K. Pilot study of a cluster randomised trial of a guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: GEM Study. BMJ Open 2015, 5, e007981. [Google Scholar] [CrossRef] [Green Version]
- Health and Safety Executive (HSE). Tackling Work-Related Stress Using the Management Standards Approach. 2019. Available online: https://www.hse.gov.uk/pubns/wbk01.htm (accessed on 4 April 2022).
- Jones, M.A. A Study of Satisfaction with Online Learning in Workplace Training. Thesis in Public Policy and Administration. Walden University, 2016. Available online: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=3261&context=dissertations (accessed on 20 April 2022).
- Mitsakis, F.; Karageorgakis, T. E-learning: A Temporary ‘By-Product’ of Covid-19 Pandemic or a Contemporary Solution to Workplace Training and Learning? In The Future of HRD; Loon, M., Stewart, J., Nachmias, S., Eds.; Palgrave Macmillan: Cham, Switzerland, 2020; Volume 1. [Google Scholar] [CrossRef]
- Caudill, J.G. Employee Motivations for Workplace Learning and the Role of Elearning in the Workplace. Internet Learn. 2015, 4. Available online: https://jolrap.scholasticahq.com/article/26908.pdf (accessed on 23 May 2022). [CrossRef]
- David, O.; Salleh, M.; Iahad, N. The impact of elearning in workplace: Focus on organizations and healthcare environments. IAJIT 2012, 2, 203–209. [Google Scholar]
- Cheng, B.; Wang, M.; Yang, S.J.; Kinshuk; Peng, J. Acceptance of competency-based workplace e-learning systems: Effects of individual and peer learning support. Comput. Educ. 2011, 57, 1317–1333. [Google Scholar] [CrossRef] [Green Version]
- Mental Health and Productivity Pilot (MHPP). Supporting Workplace Mental Health Across the East Midlands Engine Region. Available online: https://mhpp.me (accessed on 20 April 2022).
- Blake, H.; Somerset, S.; Greaves, S. The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study. Healthcare 2022, 10, 56. [Google Scholar] [CrossRef]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behavior Change Interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef]
- Mohr, D.C.; Schueller, S.M.; Montague, E.; Burns, M.N.; Rashidi, P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. J. Med. Internet Res. 2014, 16, e146. [Google Scholar] [CrossRef]
- Oinas-Kukkonen, H.; Harjumaa, M. Persuasive systems design: Key issues, process model, and system features. CAIS 2009, 24, 28. [Google Scholar] [CrossRef]
- Blake, H.; Somerset, S.; Evans, C. Development and Fidelity Testing of the Test@Work Digital Toolkit for Employers on Workplace Health Checks and Opt-In HIV Testing. Int. J. Environ. Res. Public Health 2020, 17, 379. [Google Scholar] [CrossRef] [Green Version]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef]
- Thabrew, H.; Fleming, T.; Hetrick, S.; Merry, S. Co-design of eHealth Interventions with Children and Young People. Front. Psychiatry 2018, 9, 481. [Google Scholar] [CrossRef] [Green Version]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- O’Cathain, A.; Croot, L.; Duncan, E.; Rousseau, N.; Sworn, K.; Turner, K.M.; Yardley, L.; Hoddinott, P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019, 9, e029954. [Google Scholar] [CrossRef] [Green Version]
- Skivington, K.; Matthews, L.; Simpson, S.; Craig, P.; Baird, J.; Blazeby, J.; Boyd, K.; Craig, N.; French, D.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ 2021, 374, n2061. [Google Scholar] [CrossRef]
- Bevan Jones, R.; Stallard, P.; Agha, S.S.; Rice, S.; Werner-Seidler, A.; Stasiak, K.; Kahn, J.; Simpson, S.A.; Alvarez-Jimenez, M.; Rice, F.; et al. Practitioner review: Co-design of digital mental health technologies with children and young people. J. Child Psychol. Psychiatry 2020, 61, 928–940. [Google Scholar] [CrossRef]
- Hodson, E.; Dadashi, N.; Delgado, R.; Chisholm, C.; Sgrignoli, R.; Swaine, R. Co-design in mental health; Mellow: A self-help holistic crisis planning mobile application by youth, for youth. Des. J. 2019, 22, 1529–1542. [Google Scholar] [CrossRef] [Green Version]
- Austin, J.; Van Dijk, J.; Drossaert, C. When Theory Meets Users in Co-Design: Four Strategies towards Synergy between Bottom-Up and Top-Down Input. In Proceedings of the Synergy-DRS International Conference, held online, 11–14 August 2020. [Google Scholar]
- Sanders, E.B.-N.; Stappers, P.J. Co-creation and the new landscapes of design. CoDesign 2008, 4, 5–18. [Google Scholar] [CrossRef] [Green Version]
- Saad-Sulonen, J.; Eriksson, E.; Halskov, K.; Karasti, H.; Vines, J. Unfolding participation over time: Temporal lenses in participatory design. CoDesign 2018, 14, 4–16. [Google Scholar] [CrossRef] [Green Version]
- Toledo-Chávarri, A.; Ramos-García, V.; Koatz, D.; Torres-Castaño, A.; Perestelo-Pérez, L.; Ramírez-Puerta, A.B.; Tello-Bernabé, M.-E.; García-García, J.-M.; García-García, J.; Pacheco-Huergo, V.; et al. Co-Design Process of a Virtual Community of Practice for the Empowerment of People with Ischemic Heart Disease. Int. J. Integr. Care 2020, 20, 9. [Google Scholar] [CrossRef]
- Bevan Jones, R.; Thapar, A.; Rice, F.; Beeching, H.; Cichosz, R.; Mars, B.; Smith, D.J.; Merry, S.; Stallard, P.; Jones, I.; et al. A Web-Based Psychoeducational Intervention for Adolescent Depression: Design and Development of MoodHwb. JMIR Ment. Health 2018, 5, e13. [Google Scholar] [CrossRef] [Green Version]
- Köpsel, V.; de Moura Kiipper, G.; Peck, M.A. Stakeholder engagement vs. social distancing—how does the COVID-19 pandemic affect participatory research in EU marine science projects? Marit. Stud. 2021, 20, 189–205. [Google Scholar] [CrossRef]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Powell, A.; Francis-Devine, B.; Clark, H. Coronavirus: Impact on the Labour Market. Research Briefing; House of Commons Library, UK Parliament: London, UK, 2022; Available online: https://commonslibrary.parliament.uk/research-briefings/cbp-8898/ (accessed on 20 April 2022).
- Al Roobaea, R.; Mayhew, P.J. How Many Participants are Really Enough for Usability Studies? In Proceedings of the Science and Information Conference, London, UK, 27–29 August 2014. [Google Scholar]
- Hoffmann, T.; Glasziou, P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention de-scription and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Rad, D.; Rad, G. Theory of Change in Digital Behavior Change Interventions (Dbcis) And Community-Based Change Initiatives —A General Framework. Tech. Soc. Sci. J. 2021, 21, 554–569. [Google Scholar] [CrossRef]
- Yarker, J.; Lewis, R.; Donaldson-Feilder, E.; Flaxman, P. Management Competencies for Preventing and Reducing Stress at Work: Identifying and Developing the Management Behaviors Necessary to Implement the HSE Management Standards; Rr553; HSE Books: London, UK, 2007. [Google Scholar]
- Yarker, J.; Lewis, R.; Donaldson-Feilder, E. Management Competencies for Preventing and Reducing Stress at Work: Identifying the Management Behaviors Necessary to Implement the Management Standards: Phase Two; RR633; HSE Books: London, UK, 2008. [Google Scholar]
- Donaldson-Feilder, E.; Lewis, R.; Yarker, J. Preventing Stress: Promoting Positive Manager Behavior; CPID: London, UK, 2009; Available online: https://www.cipd.co.uk/Images/preventing-stress_2009-promoting-positive-manager-behavior_tcm18-16794.pdf (accessed on 6 April 2022).
- Health and Safety Executive (HSE). Stress Management Competency Indicator Tool. 2009. Available online: http://www.hse.gov.uk/stress/mcit.htm (accessed on 20 April 2022).
- IBM SPSS Statistics for Windows; Version 26.0; IBM Corp.: Armonk, NY, USA, 2019.
- National Institute for Health and Care Excellence (NICE). Mental Wellbeing at Work. NICE Guideline [NG212]. 2022. Available online: https://www.nice.org.uk/guidance/ng212 (accessed on 4 April 2022).
- ISO 45003; Psychological Health in the Workplace. British Standards Institution (BSI): Loughborough, UK, 2022. Available online: https://www.bsigroup.com/en-GB/iso-45003/ (accessed on 4 April 2022).
- Mental Health Commission of Canada (MHCC). National Standard of Canada for Psychological Health and Safety in the Workplace. Available online: https://mentalhealthcommission.ca/national-standard/ (accessed on 4 April 2022).
- Safe Work Australia. Work-Related Psychological Health and Safety: A Systematic Approach to Meeting Your Duties. National Guidance Material. 2019. Available online: https://www.safeworkaustralia.gov.au/system/files/documents/1911/work-related_psychological_health_and_safety_a_systematic_approach_to_meeting_your_duties.pdf (accessed on 4 April 2022).
- World Health Organization. Prevention and Promotion in Mental Health. Mental Health: Evidence and Research; Department of Mental Health and Substance Dependence, World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Michael, J. Where’s the evidence that active learning works? Adv. Physiol. Educ. 2006, 30, 159–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fana, M.; Torrejón Pérez, S.; Fernández-Macías, E. Employment impact of Covid-19 crisis: From short term effects to long terms prospects. J. Ind. Bus. Econ. 2020, 47, 391–410. [Google Scholar] [CrossRef]


| Core Elements | Intervention Development Considerations |
|---|---|
| (i) Context | Context of the employment settings and job role of the line manager may influence the way in which the intervention is accessed and used. Content must be relevant across employment settings (sector, size, and type of organization) for line managers at all levels of the hierarchy. |
| (ii) Developing and refining program theory | Program theory was established prior to intervention development with the involvement of diverse stakeholders and based on evidence and theory from relevant fields. This focused on identifying the key areas of line managers’ influence in preventing poor mental health, specific actions associated with these, and the likely outcomes. Can be refined during successive phases to inform transferability of the intervention across settings. |
| (iii) Engaging stakeholders | Collaborative participatory approach involved stakeholders at every stage: development of program theory, co-creation of intervention content, iterative peer review, and revisions. Multiple methods for stakeholder engagement were triangulated and included individual/group discussion, online data collection, and email feedback to share and develop ideas. Participation must be both emergent and ongoing (long term). |
| (iv) Identifying key uncertainties | Uncertainties related to design and delivery: timescale for development of the intervention, appropriateness of the level of language complexity, most appropriate format for delivery. Potential challenges with engaging stakeholders in research intervention development during a global pandemic. Consideration of the global public health and economic impact of a global pandemic on intervention content and future implementation. |
| (v) Refining the intervention | Using an agile approach, stakeholder consultation and review is an iterative process, allowing for continuous delivery and a resource-efficient approach to toolkit development. |
| (vi) Economic considerations | Stakeholder input supported by charitable bodies and professional input via the wider MHPP program. Specific costs for intervention web-hosting and individual user logins. |
| Category | Summary of Stakeholder Revisions |
|---|---|
| Presentation of materials | cover page, colors, logos, image diversity, balance of text, activities and images, use of bullet points, signposting, typographical errors |
| Functionality | font and illustration size, scrolling, web links, transcript availability, use of hyperlinks, video quality |
| Clarity of information | definition of terms, not assuming prior knowledge or skills, rephrasing, additional explanation, removal of repetition |
| Additional resources | adding confidential helplines, downloadable resources page |
| Incentives for completion | module-by-module completion for flexibility, provision of feedback or explanation for incorrect answers on tasks, encouragement to revisit tasks, observable progression points, confirmation of completion, reminders and encouragement for completion, downloadable certificate |
| Consideration of current context | relevant to virtual and remote working due to the global coronavirus pandemic |
| Question Item (N = 37 Responses +) | TAM Construct | n (%) |
|---|---|---|
| Knowledge attainment | % Yes | |
| Did you learn anything that you did not know before? | U | 24 (64.9) |
| Content Relevance | % Yes | |
| Did you think the module content was relevant to your managerial role? | U | 37 (100) |
| Case example relevance | n (%) strongly disagree, or disagree | |
| The examples provided throughout the module were not relevant to my role as a manager | U | 30 (81.1) |
| Ease of understanding | n (%) strongly disagree, or disagree | |
| I found some of the information presented in the module difficult to understand | E | 36 (97.3) |
| Usability | n (%) strongly agree, or agree | |
| The online module was an appropriate length | E | 37 (100) |
| The online module was easy to navigate | E | 36 (97.3) |
| Barriers to use | n (%) strongly agree, or agree | |
| It was easy to find the time to complete this module | EV | 23 (62.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blake, H.; Vaughan, B.; Bartle, C.; Yarker, J.; Munir, F.; Marwaha, S.; Daly, G.; Russell, S.; Meyer, C.; Hassard, J.; et al. Managing Minds at Work: Development of a Digital Line Manager Training Program. Int. J. Environ. Res. Public Health 2022, 19, 8006. https://doi.org/10.3390/ijerph19138006
Blake H, Vaughan B, Bartle C, Yarker J, Munir F, Marwaha S, Daly G, Russell S, Meyer C, Hassard J, et al. Managing Minds at Work: Development of a Digital Line Manager Training Program. International Journal of Environmental Research and Public Health. 2022; 19(13):8006. https://doi.org/10.3390/ijerph19138006
Chicago/Turabian StyleBlake, Holly, Benjamin Vaughan, Craig Bartle, Jo Yarker, Fehmidah Munir, Steven Marwaha, Guy Daly, Sean Russell, Caroline Meyer, Juliet Hassard, and et al. 2022. "Managing Minds at Work: Development of a Digital Line Manager Training Program" International Journal of Environmental Research and Public Health 19, no. 13: 8006. https://doi.org/10.3390/ijerph19138006
APA StyleBlake, H., Vaughan, B., Bartle, C., Yarker, J., Munir, F., Marwaha, S., Daly, G., Russell, S., Meyer, C., Hassard, J., & Thomson, L. (2022). Managing Minds at Work: Development of a Digital Line Manager Training Program. International Journal of Environmental Research and Public Health, 19(13), 8006. https://doi.org/10.3390/ijerph19138006








