Abstract
International students in China were among the first group of individuals to be affected by the COVID-19 pandemic. However, the pandemic’s impact on their mental health is underexplored. This study—utilizing web-based survey data (N = 381), presents preliminary reports using ANOVA and MIMIC analytic approaches. Following the clinical demarcation of the 21-item version of the Depression Anxiety Stress Scales (DASS-21), we found 24.6%, 38.3%, and 43.6% of the students to suffer mild to extreme stress, anxiety, and depression, respectively. Female students reported significantly higher levels of stress and depression than males. Older students’ reports of stress were more substantial than younger students. Students who reported having a relative infected with the virus (vs. those without) experienced significantly higher anxiety and stress. Those who reported having pre-existing chronic health condition(s) (vs. those without) also reported significantly higher stress, anxiety, and depression levels. Moreover, students with an exercise routine (vs. those without) experienced significantly lower levels of stress, anxiety, and depression. Last, our MIMIC model results indicate that foreign students’ age, gender, chronic health status, and having a relative infected with the virus constitute significant risk factors explaining variations in foreign students’ experience of psychological distress. Implications for international students’ management have been thoroughly discussed.
1. Introduction
The COVID-19 pandemic in early 2020 threw the world into chaos. It shook the very foundations of our lives: economic collapse, nationwide quarantine or curfew implementation, and intrusive health checks. The global reach [1] of this invisible “demon” meant that every individual, community, and nation had to grapple with its dramatic ramifications. Adaptation to the sudden and rapid change of events was critical to our survival. One key component that marked adaptation measures at the individual, community, and national, or global level was the need for social distancing [2,3]. Like other service industries such as hospitality, travel, and tourism (HTT) [4,5,6,7,8], universities depend on social interaction, for the most part, to contribute to society. However, the high transmissibility of the disease and the attendant urgency to defeat it through breaking the chain (i.e., social distancing) [9,10] completely transformed the character of academic engagements, especially those between students and their faculty [11,12]. Virtual teaching and learning and research have replaced the in-person face-to-face organization of universities’ life [13,14].
Additionally, students who lived on campus were urged to eschew all forms of socialization. These developments have critical implications on students’ wellbeing and overall quality of life, particularly international students who are away from their families and often other familiar social groups [15]. In 2022, though the chaotic responses have died down a bit, the disease unfortunately still lives amongst us, mutating into more virulent variants in some countries [16,17]. In addition, in most parts of the world, the new normal dictated by the need for social distancing still prevails.
Available evidence on COVID-19 demonstrates that the pandemic has affected the mental health of patients and survivors and health workers, and the general public [18,19]. Preliminary survey studies targeting people with or without quarantine management status demonstrated the pandemic’s effect on mental health [20,21,22]. Importantly, Vindegaard and Benros [18], through a systemic review of 43 studies, synthesized current evidence on mental health. The authors discovered that 20 studies found deteriorating mental health among health workers, including increased depression/depressive symptoms, anxiety, and poor sleep quality. Nineteen of these studies reveal a similar pattern of mental health degradation among the general public. Nonetheless, research into mental health management in times like this is lacking. The authors, therefore, recommend more studies into mental health to inform the design of preventative and treatment measures and the overall mental health care planning in this and future pandemics.
One important group that academics have been silent on is international students. For instance, international students in China have experienced first-hand the drastic measures that had to be taken to curb the spread of the disease. For many, this included severe restrictions on movement, online classes rather than the in-classroom setting, decline or halt in socialization, and frequent health-related tests and checks right from the start of the pandemic. International students might have been faced with immense socio-emotional pressure as a result. Added to the possible anxiety brought about by fear of contracting the disease [23], they are likely to also worry over the welfare of loved ones across the oceans [24]. Generally, research evidence demonstrates the mental health impacts of the pandemic on students [25,26,27,28,29]. Some examples include survey reports of psychological distress among Indian undergraduates and postgraduate students [30], medical students in Pakistan [31], and Chinese university students [32,33,34]. Specifically, Jiang [32] reports a significant increase in scores of somatizations, obsessive-compulsive disorder, interpersonal sensitivity, anxiety, phobic anxiety, and paranoid ideation, among other mental health indices for Chinese students. It is noteworthy that these students possessed limited COVID-19 knowledge and perceived the risk of infection very highly. All these are factors that likely lead to a coping style that is debilitating to mental health. Now, suppose Chinese university students with close family ties [35] are in the throes of COVID-19. In that case, we can safely assume that international students—who may have language challenges, limited mobility, and cultural understanding, may not be spared.
However, scant research exists on international students whose lives, from all indications, may be more susceptible to bouts of stress, anxiety, and depression. Indeed, a systematic review of research on the mental health of international students in China from 2014 to 2021 by Wu [36] found that only two studies examined international students since the pandemic, of which one explored barriers to health science international students’ online education [37] and the other on psychological determinants of depression [38]. These studies are important, but they do not reveal the nature of the incidence of psychological distress across subpopulations of international students. Moreover, Kulyar’s [24] letter to the editor suggests that international students’ concern about infection and safety of their families may impact their mental health. Wang’s preprint [39] with a sample from Central South University’s international students indicates the prevalence of depression and anxiety. These worrying mental health indications are not surprising. Pre-COVID-19 research evidence illustrates the various psychological distresses of adaptation challenges faced by international students in China [40,41,42,43]. Wu [36] therefore concluded that the psychological situation of international students in China is unsatisfying but limited research exists in this area. Manzoor’s [23] recent study on how the fear of COVID-19 induces generalized anxiety disorder among foreign students in China is a welcome contribution.
That notwithstanding, it is important to estimate the extent of mental health incidence among international students. Accordingly, the first objective of this study is to examine the international students’ experience of psychological distress (i.e., stress, anxiety, depression) during the COVID-19 pandemic. Moreover, it is essential to acknowledge that international students are not monolithic. They are some of the most diverse social groups; they have different funding sources, academic majors, and accommodation preferences among other things. To get a comprehensive picture of mental health incidence among international students, our second objective is to analyze international students’ experience of psychological distress across subpopulations using their socio-demographic profiles. Last, we build a multiple indicator-multiple cause (MIMIC) model to examine the predictive capacity of relevant international students’ profiles (i.e., age, sex, chronic condition, and relative infected with COVID-19). In sum, this study examines: (1) the extent of international students’ experience of psychological distress; (2) the levels of this experience across subpopulations; and (3) the risk factors.
2. Materials and Methods
2.1. Participants and Procedure
This study adopts a cross-sectional design, using a questionnaire survey, in assessing international students’ mental health in a time of infectious disease outbreak—the COVID-19 pandemic. The survey was conducted when international students in most schools were still unable to move in and out of campus and were confined to their hostels or dormitories. And the few who could step out of the walls of their universities did so within a strict 1 to 3 h timeframe. Such mobility limitations are currently implemented in universities in certain cities such as Shanghai. The study’s goal and the need for social distancing demanded that an online survey questionnaire design be used for data collection. So, a convenience sampling approach was adopted. The questionnaire items for the constructs (i.e., the DASS-21 variables) and students’ profiles explored in this study were organized on an online platform called Kwiksurvey.com (this platform is used for individual and corporate data collection purposes. For more details, please consult https://kwiksurveys.com/). A hyperlink and a quick response code (i.e., QR code) of the online survey were generated from the platform. To reach a diverse international student population, the authors joined many international student groups on WeChat (a Chinese version of Facebook). Then, we introduced the study along with the hyperlink and the QR code, the study’s purpose, and the supervising institution. To encourage participation, researchers presented a gift packet of money called HongBao to the group members. Data collection took place in July of 2020. The final usable sample for this study came to 381. Eighteen (18) cases were deleted from the data due to incomplete responses, constituting 4.5% of the total data collected.
2.2. Measures
Mental health variables: The three variables measuring international students’ mental health—depression, anxiety, and stress, were captured using the 21-item version of the Depression Anxiety Stress Scales (DASS-21) [44]. These variables were each measured with 7 items on the DASS-21. Example items include: “I was aware of the dryness of my mouth” for anxiety [α = 0.82], “I felt down-hearted and blue” for depression [α = 0.90], and “I found it hard to wind down” for stress [α = 0.84]. The students were instructed to respond to the items in accordance with how best each statement described their feeling in the week prior. Students’ responses were recorded on a 4-point Likert-style scale (0 = did not apply to me at all to 3 = apply to me most of the time).
Students’ demographics and lifestyle variables: By the time of the data collection, COVID-19 had literally enveloped the globe. Therefore, relevant demographic and lifestyle profiles were captured to see where students’ experience of psychological distress differs across these salient indicators. Close- and open-ended questions were used to obtain students’ profiles, consisting of gender (1 = male and 2 = female), age (respondents were asked how old they were at their last birthday and then transformed into categorical variable: 1 = ≤24; 2 = 25–29; 3 = 30–34; 4 = 35 and above), study level (1 = Chinese language study; 2 = college/university; 3 = master; 4 = PhD), residence type (1 = on-campus accommodation and 2 = off-campus accommodation), completion year (1 = 2020; 2 = 2021; 3 = 2022; 4 = 2023; 5 = 2024; 6 = 2025), sponsorship (self-finance; 2 = full scholarship; 3 = other), economic situation (1 = very good; 2 = fairly good; 3 = fairly bad; 4 = very bad), relative on the frontline (1 = yes and 2 = no), relative infected with COVID-19 (1 = yes and 2 = no), chronic health condition (1 = yes and 2 = no), exercise routine (1 = yes and 2 = no), exercise time per week (measured in minutes and then transformed into categories of 1 = ≤2 h; 2 = 2.1–4 h; 3 = >4 h), years of stay (measured in months and then transformed into categories: 1 = ≤3 years; 2 = 3.1–6 years; 3 = >6 years). Please consult Table 1 for details on the descriptive analysis of students’ profiles.

Table 1.
Descriptive analysis of students’ demographic and lifestyle profiles.
2.3. Analytic Approach
This study performed descriptive analysis to obtain frequencies and stacked percentage bar charts for students’ sociodemographic variables and DASS subscales (i.e., anxiety, depression, and stress). Further, a one-way analysis of variance (ANOVA) was used to compare students’ characteristics and psychological states (i.e., anxiety, depression, and stress). Last, we built a multiple indicator-multiple cause (MIMIC) model [45,46] to explore the effect of students’ characteristics (i.e., gender, age, relative with COVID-19, and chronic health conditions) on anxiety, depression, and stress. SPSS version 25 and MS Excel were used to perform all the statistical analyses.
3. Results
3.1. International Students’ Sociodemographic Distribution
The majority of the students surveyed were studying towards a bachelor’s degree or higher (91.8%). Females (50.7%) were only slightly represented more than males. The age distribution of the students showed that they were predominantly below or at 29 years old (73.3%). The greater mass of the students lived in an on-campus accommodation (68.0%), were scheduled to graduate at least by 2021 (64.6%), followed an exercise routine (61.4%), and exercised at least 2 h per week (54.6%). On the other hand, fewer students recorded having a chronic health condition (6.0%), a relative as a frontline worker (25.7%), or a relative with COVID-19 (10.2%). Given that the majority of the students had full scholarship (63.3%), it is unsurprising that the economic situation of the more significant number of the students was at least fairly good (64.5%) (see Table 1 for more details).
3.2. International Students’ Experience of Mental Health during COVID-19
This study took a snapshot of mental health incidence among international students in China. Generally, the findings presented in Figure 1. illustrate a concern for the effects of the COVID-19 pandemic on international students’ wellbeing. The clinical demarcation of mental health experience follows the scoring chart of the DASS-21 scale as detailed in [44]. Overall, over 38 percent of the students surveyed reported experiencing mild to severe anxiety. Moderately anxious feelings were the highest (12.9%), with severe anxiety being the least (6.8%). The percentage of stressed-out students was generally low (24.6%), with only 2.6% of them experiencing extreme stress levels. In terms of depression, the distribution mirrors anxiety, with more (43.6%) of the respondents experiencing varying levels of depression. However, unlike anxiety, the students’ experience of mild (15.0%) and moderate (15.0%) depression was the same (see Figure 1 below).
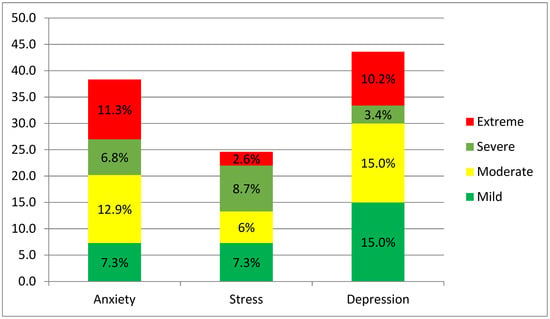
Figure 1.
International students’ experience of anxiety, stress, and depression during COVID-19 pandemic in China.
3.3. ANOVA Results for the Different Groups of Students’ Demographic and Lifestyle Variables
A one-way ANOVA analysis results revealed some sociodemographic groups differ significantly in their experience of stress, anxiety, and depression. Levene’s homogeneity test of variance was significant for gender groups at p = 0.002 for depression but non-significant at p = 0.125 for stress. Female international students reported experiencing significantly higher levels of depression [F = 8.22, p < 0.05] and stress [F = 7.31, p < 0.05] compared to their male counterparts using the Brown–Forsythe test. In respect of age, Levene’s test of homogeneity of variance was observed to have significance at p = 0.022 for stress and p = 0.045 for depression. However, only stress levels differed significantly across the age groups [F = 3.03, p < 0.05]. Levene’s homogeneity test of variance was examined for students’ exercise routine and found significance at p = 0.040 and p = 0.004 for anxiety and depression, respectively, but not stress p = 0.098. Hence, students’ exercise routine status shows itself as a significant differentiating variable in determining the levels of student experience of anxiety [F = 9.67, p < 0.05], depression [F = 9.86, p < 0.05], and stress [F = 4.02, p < 0.05] using the Brown–Forsythe robust test. Further, Levene’s homogeneity test of variance was examined for groups with a relative with COVID-19 and was significant at p = 0.006 and p = 0.005 for anxiety and stress, respectively. A significant difference was found between groups with and without a relative with COVID-19 regarding anxiety [F = 7.33, p < 0.05] and stress [F = 3.94, p < 0.05]. Lastly, significance was found for Levene’s test of homogeneity of variance for groups with and without chronic health conditions at p = 0.002, p = 0.000, and p = 0.016 for anxiety, depression, and stress, respectively. A significant difference was recorded between a student with and without chronic health conditions concerning anxiety [F = 6.97, p < 0.05], depression [F = 11.21, p < 0.05], and stress [F = 12.71, p < 0.05] using the Brown–Forsythe robust test. No statistical significance was found between groups of other sociodemographic variables surveyed in Table 2 with respect to the DASS subscales.

Table 2.
One-way ANOVA analysis result.
3.4. MIMIC Results
MIMIC model was employed to assess the impact of foreign students’ characteristics (i.e., gender, age, relative with COVID-19 and chronic health conditions) on their depression, anxiety, and stress. Prior to the model development, gender (female = 0 and male = 1), relative with COVID-19 (no = 0 and yes = 1), and chronic health conditions (no = 0 and yes = 1) were dummy coded. The model provided a good fit to the data (X2 = 464.70, df = 214, X2/df = 2.17, NFI = 0.89, CFI/TLI = 0.94/0.93, RMSEA = 0.06, SRMR = 0.04). The results revealed that gender had a significant negative effect on anxiety (b = −0.11, SE = 0.03, p < 0.05), depression (b = −0.17, SE = 0.08, p < 0.01), and stress (b = −0.16, SE = 0.05, p < 0.01). Age had a significant positive effect on depression (b = 0.11, SE = 0.01, p < 0.05) and stress (b = 0.16, SE = 0.05, p < 0.01). Moreover, students with relatives infected with COVID-19 significantly predicted anxiety (b = 0.18, SE = 0.06, p < 0.01), depression (b = 0.13, SE = 0.12, p < 0.05), and stress (b = 0.14, SE = 0.10, p < 0.01). Last, chronic health condition had a significant positive effect on anxiety (b = 0.20, SE = 0.08, p < 0.01), depression (b = 0.21, SE = 0.16, p < 0.001), and stress (b = 0.26, SE = 0.13, p < 0.001) (see Figure 2).
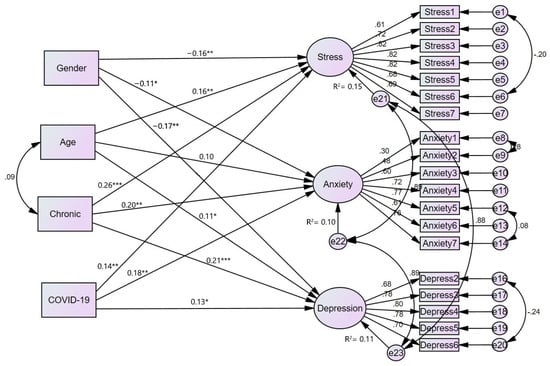
Figure 2.
Structural model examining students’ demographics effect on DASS-21. Note: Chronic = chronic health conditions, COVID-19 = relative with COVID-19. * p < 0.05, ** p < 0.01, *** p < 0.001.
4. Discussion
Sadly, the COVID-19 pandemic has engulfed our globe with unprecedented fear, panic and deaths. It has been over two years now since the disease was declared a global health crisis. Unfortunately, catastrophes of this magnitude are marked to debilitate peoples’ physio-psychological health. In this pandemic, several studies have reported the mental health impact of the COVID-19 pandemic among general populations, medical practitioners, and students. However, scant research [36] exists on one group of university students—the international students—who may be more prone to psychological distress. In particular, international students in China are some of the world’s population to first experience the brunt of the COVID-19 pandemic. Accordingly, the primary aim of this study is to offer a preliminary account of the mental health impacts of the COVID-19 pandemic on international students in China. To achieve our purpose, we employed Lovibond and Lovibond’s (1995) DASS-21 scale and its accompanying clinical scoring chart to map out international students’ experience of psychological distress. Additionally, a one-way analysis of variance (ANOVA) was performed to establish whether differences in mental health experience across international students’ sociodemographic variables were statistically significant. Lastly, a multiple indicator multiple causes (MIMIC) model was developed to explore relevant students’ sociodemographic (i.e., age, gender, chronic condition, and relative with COVID-19) as risk factors. Thus, to the best of our knowledge, this study forms the first assessment of international students’ mental health experience across their profiles and the predictive influence of relevant profiles on their experience.
The results demonstrate that international students’ mental health is a concern. It is noteworthy, however, that a cursory browse through the stacked percentage bar chart indicates that the percentages of students reporting either being anxious, depressed, or stressed out tend to plummet with increasing levels of severity, except anxiety, where the highest rate of students reported feeling moderately (rather than mildly) anxious. This distribution mirrors the distribution of college students’ mental health reports on the DASS-21 scale in prior studies during the COVID-19 pandemic [47]. However, compared to similar studies from China using Chinese university student samples [48], international students report a relatively higher experience of psychological distress. It is also noteworthy that these studies used medical students, who, given the odds, are anticipated to be more psychologically distressed. For example, over 38% of international students in this study reported feeling mild to extreme anxiety compared to 24.9% reported among medical students [48]. Further assessment reveals that a significant part (21.3%) of the 24.9% experienced mild anxiety leaving a small part experiencing moderate (2.7%) and severe (0.9%) anxiety. Moreover, Liu et al. (2020) found that 22.1% and 35.5% of medical students from Hubei province experience anxiety and depression, respectively. In the present study, 43.6% reported feeling depressed. Though Cao et al. [48] and Liu et al. [49] utilized the 7-item Generalized Anxiety Disorder Scale (GAD-7), the exactness of the number of items and the identical rating (thus, the 4-point Likert scale) makes it comparable to the anxiety subscale of the DASS-21.
In terms of biographical data, findings from the ANOVA indicate that female international students are more depressed and stressed out than male international students. This finding is consistent with previous studies using university students’ samples [50,51,52] and even among adolescents [53]. For Hakami et al.’s [51] study, they discovered that junior females who lived alone were particularly at risk of severe to extreme psychological distress. However, not all studies find females to experience significantly different levels of psychological distress in this pandemic. For example, Cao et al. [48] found no difference between males and females in their experience of psychological distress. Further, this study finds that older international students experienced significantly higher stress levels than younger international students. The negative relations between age and stress may be due to the fact that media reports of higher mortality rate among the older population who get infected. In contradistinction, Gaş et al. [50] discovered that younger students were more stressed out than older students.
Regarding international students’ social, pre-existing health condition, and lifestyle data, the results show that the international student group that reported having a relative infected with COVID-19 was significantly more anxious and stressed out than those who had no relative infected with the virus. The higher psychological distress might stem from the worry about losing someone so close. Perhaps, even a sponsor of one’s education. In addition, international students who reported having a pre-existing chronic health condition reported experiencing significantly higher levels of depression, anxiety, and stress than students without a pre-existing chronic health condition. Scientific communication at the initial stages of the virus made clear that the condition of the infected is more likely to deteriorate into a critical emergency if pre-existing chronic health condition exists. This finding supports the empirical reports of individuals with pre-existing psychological conditions suffering more psychological distress than those without [54,55]. Lastly, students with an exercise routine seem to cope better than those without as they reported significantly lower levels of stress, anxiety, and depression compared to students with no exercise routine. This result is consistent with current research evidence [56,57,58,59,60], demonstrating negative relation between physical activity and psychological distress.
Lastly, the findings of the test of whether international students’ age, gender, chronic condition status, and having a relative infected with COVID-19 predicted variations in our three latent variables (i.e., depression, anxiety, and stress) of mental health strengthen the significance of taking foreign students’ unique profiles into account in managing their psychological reaction to the pandemic. Being a female, older age, with a chronic condition, and having a relative with COVID-19 predisposes foreign students to experience higher levels of psychological distress. Some of these findings are consistent with existing studies concerning determinants of psychological distress in this pandemic in other populations, including psychological distress among Israeli and European populations [61,62]. Specifically, the evidence that female international students and those with pre-existing health issues experience higher levels of psychological distress is in line with the findings from the Israeli population [62]. Again, being female was found to induce higher psychological distress in 27 European countries [61]. However, the younger age Israeli population was less impacted by the pandemic contrary to our findings that older students experience higher psychological distress.
4.1. Implications for International Students’ Health Management in Crisis Time
Scholars have suggested the possibility of psychological distress among international students [15]. This study adds to the scant research on international students’ mental health in China [36] by demonstrating the impact of COVID-19 on international students’ mental health, differences in experiencing psychological distress across subpopulations, and the risk factors. The study, therefore, directs the discussion on international students’ mental health from theory-informed speculations to data-driven conclusions. Furthermore, the findings contained in this study possess several practical implications for international students’ mental health management that aligns with the popular proposal of a student-centered approach to international higher education management that nurtures international students’ wellbeing.
First, female international students feeling more depressed and stressed suggest that any interventions designed to manage the international students’ mental health should recognize that not all interventions may work just because they work for male international students. Additionally, interventions on stress management may not work for students of all age groups. We recommend that university managements check the efficacy of preventative or treatment programs across age groups and male and female international students. Second, international students’ lifestyle (exercise routine in this study) is found to have a significant impact on their mental health in this pandemic. We recommend that universities develop physical activity protocols that ensure safe participation in these activities. Third, international students’ management should know which of their students are at a higher risk of psychological distress based on their medical history. Management should quickly move and identify these individuals and, with their contribution, identify ways to support them. Finally, global catastrophes of this nature imply that some relatives of international students may be affected by the situation. The results that students who had a relative infected with the virus reported higher psychological distress implies that international students’ management offices need to know these students to learn about their unique conditions and devise ways, including mindfulness training [63], to alleviate their anguish.
4.2. Limitations of the Study
Despite the valuable insights offered by this study, some limitations are worth pointing out to guide the interpretation of the study’s findings. First, the study’s cross-sectional design with self-reported data raises the possibility of biased reports. However, self-report data on university students’ mental health has been adjudged an adequate assessment as individuals are in the best position to evaluate their subjective wellbeing [48,64]. Second, given that the design was cross-sectional, a comparative analysis of international students’ mental health across different time points during the pandemic is not possible. Therefore, we recommend that future studies adopt a longitudinal design to gain a much richer insight into mental health among international students. Third, self-selection bias may pose a challenge as the data were collected online without probability sampling. We recommend that future research access the sampling frame in a particular university or combine both off- and on-line data collection approaches to monitor self-selection biases in web-based surveys. Fourth, this study did not take into account the origin countries of these students. We recommend future research consider the respective countries of the students. Finally, international students’ sociodemographics are numerous, and we recommend that future studies explore other relevant profiles such as family relationship and economic status that have not been explored in this study.
5. Conclusions
The impact of COVID-19 on international students’ mental health has been underexplored [15,36]. In this study, we report empirical evidence on the mental health impact of the pandemic on international students’ subpopulations. Specifically, the findings show that students who are female, older, with relatives infected with the COVID-19 virus, have pre-existing chronic health condition(s), and are without exercise routine are more susceptible to mental health degradation during the pandemic. We offer a number of practical recommendations to the management of institutions of higher learning with international students’ population to pay attention to the subpopulation of international students that may be more prone to suffer psychological distress from the pandemic as the virus mutates to more or less virulent variants.
Author Contributions
Conceptualization, C.O.A., M.A.B. and J.R.; methodology, M.A.B., C.O.A., E. A-O., M.O.A. and S.Y.N.; investigation, M.A.B., C.O.A., Y.W. and E.A.-O.; resources, C.O.A. and J.R.; data curation, E.A.-O., M.O.A. and S.Y.N.; writing—original draft preparation, M.A.B. and C.O.A.; writing—review and editing, Y.W., E.A.-O., S.Y.N., M.O.A. and J.R.; supervision, J.R.; project administration, M.O.A., Y.W. and J.R.; funding acquisition, C.O.A. and J.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by Grant ZC304020924 from the ZJNUf Postdoctoral Research, Grant PJ103018001 from the Open Research Fund of College of Teacher Education, Zhejiang Normal University, Grant BBA170067 from The National Social Science Fund and supported by China Positive Psychology Research Foundation 2021 Key Projects, Beijing Happiness Foundation. The funders had no involvement in the data collection, analysis and interpretation, as well as the manuscript write-up and the decision to submit the manuscript for publication.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all the students involved in the study.
Data Availability Statement
Data will be supplied upon request from the corresponding author.
Conflicts of Interest
The authors of this manuscript declare that they have no known competing interests, financial or otherwise, that could impact the decisions on the study design, results’ reporting and the choice of publication outlet.
References
- Tian, F.; Li, H.; Tian, S.; Yang, J.; Shao, J.; Tian, C. Psychological Symptoms of Ordinary Chinese Citizens Based on SCL-90 during the Level I Emergency Response to COVID-19. Psychiatry Res. 2020, 288, 112992. [Google Scholar] [CrossRef] [PubMed]
- Taghrir, M.H.; Akbarialiabad, H.; Marzaleh, M.A. Efficacy of Mass Quarantine as Leverage of Health System Governance during COVID-19 Outbreak: A Mini Policy Review. Arch. Iran. Med. 2020, 23, 265–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parmet, W.E.; Sinha, M.S. COVID-19—The Law and Limits of Quarantine. N. Engl. J. Med. 2020, 382, e28. [Google Scholar] [CrossRef]
- Antwi, C.O.; Ren, J.; Owusu-Ansah, W.; Mensah, H.K.; Aboagye, M.O. Airport Self-Service Technologies, Passenger Self-Concept, and Behavior: An Attributional View. Sustainability 2021, 13, 3134. [Google Scholar] [CrossRef]
- Antwi, C.O.; Ntim, S.Y.; Boadi, E.A.; Asante, E.A.; Brobbey, P.; Ren, J. Sustainable Cross-Border Tourism Management: COVID-19 Avoidance Motive on Resident Hospitality. J. Sustain. Tour. 2022, 1–21. [Google Scholar] [CrossRef]
- Antwi, C.O.; Fan, C.J.; Ihnatushchenko, N.; Aboagye, M.O.; Xu, H. Does the Nature of Airport Terminal Service Activities Matter? Processing and Non-Processing Service Quality, Passenger Affective Image and Satisfaction. J. Air Transp. Manag. 2020, 89, 101869. [Google Scholar] [CrossRef]
- Antwi, C.O.; Fan, C.J.; Nataliia, I.; Aboagye, M.O.; Xu, H.; Azamela, J.C. Do Airport Staff Helpfulness and Communication Generate Behavioral Loyalty in Transfer Passengers? A Conditional Mediation Analysis. J. Retail. Consum. Serv. 2020, 54, 102002. [Google Scholar] [CrossRef]
- Boadi, E.A.; He, Z.; Antwi, C.O.; Md Altab, H.; Bosompem, J.; Hinson, R.E.; Atuobuah Boadi, V. Value Co-Creation and Employee Service Behaviours: The Moderating Role of Trust in Employee—Hotel Relationship. J. Retail. Consum. Serv. 2022, 66, 102898. [Google Scholar] [CrossRef]
- Courtemanche, C.; Garuccio, J.; Le, A.; Pinkston, J.; Yelowitz, A. Strong Social Distancing Measures in the United States Reduced the COVID-19 Growth Rate. Health Aff. 2020, 39, 1237–1246. [Google Scholar] [CrossRef]
- Wang, C.; Li, H. Public Compliance Matters in Evidence-Based Public Health Policy: Evidence from Evaluating Social Distancing in the First Wave of COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 4033. [Google Scholar] [CrossRef]
- Hasan, N.; Bao, Y. Impact of “e-Learning Crack-up” Perception on Psychological Distress among College Students during COVID-19 Pandemic: A Mediating Role of “Fear of Academic Year Loss”. Child. Youth Serv. Rev. 2020, 118, 105355. [Google Scholar] [CrossRef] [PubMed]
- Maqableh, M. Evaluation Online Learning of Undergraduate Students under Lockdown amidst COVID-19 Pandemic: The Online Learning Experience and Students’ Satisfaction. Child. Youth Serv. Rev. 2020, 128, 106160. [Google Scholar] [CrossRef]
- Yang, R. China’s Higher Education during the COVID-19 Pandemic: Some Preliminary Observations. High. Educ. Res. Dev. 2020, 39, 1317–1321. [Google Scholar] [CrossRef]
- Chu, Y.; Li, Y. The Impact of Online Learning on Physical and Mental Health in University Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2966. [Google Scholar] [CrossRef]
- Nguyen, O.O.T.K.; Balakrishnan, V.D. International Students in Australia–during and after COVID-19. High. Educ. Res. Dev. 2020, 39, 1372–1376. [Google Scholar] [CrossRef]
- Starr, T.N.; Greaney, A.J.; Addetia, A.; Hannon, W.W.; Choudhary, M.C.; Dingens, A.S.; Li, J.Z.; Bloom, J.D. Prospective Mapping of Viral Mutations That Escape Antibodies Used to Treat COVID-19. Science 2021, 371, 850–854. [Google Scholar] [CrossRef]
- Hoffmann, M.; Krüger, N.; Schulz, S.; Cossmann, A.; Rocha, C.; Kempf, A.; Nehlmeier, I.; Graichen, L.; Moldenhauer, A.S.; Winkler, M.S.; et al. The Omicron Variant Is Highly Resistant against Antibody-Mediated Neutralization: Implications for Control of the COVID-19 Pandemic. Cell 2022, 185, 447–456.e11. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Carmassi, C.; Dell’Oste, V.; Barberi, F.M.; Bertelloni, C.A.; Pedrinelli, V.; Dell’Osso, L. Mental Health Symptoms among General Practitioners Facing the Acute Phase of the COVID-19 Pandemic: Detecting Different Reaction Groups. Int. J. Environ. Res. Public Health 2022, 19, 4007. [Google Scholar] [CrossRef]
- Zhu, S.; Wu, Y.; Zhu, C.Y.; Hong, W.C.; Yu, Z.X.; Chen, Z.K.; Chen, Z.L.; Jiang, D.G.; Wang, Y.G. The Immediate Mental Health Impacts of the COVID-19 Pandemic among People with or without Quarantine Managements. Brain Behav. Immun. 2020, 87, 56. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The Differential Psychological Distress of Populations Affected by the COVID-19 Pandemic. Brain Behav. Immun. 2020, 87, 49. [Google Scholar] [CrossRef] [PubMed]
- Kalok, A.; Sharip, S.; Hafizz, A.M.A.; Zainuddin, Z.M.; Shafiee, M.N. The Psychological Impact of Movement Restriction during the COVID-19 Outbreak on Clinical Undergraduates: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8522. [Google Scholar] [CrossRef] [PubMed]
- Manzoor, F.; Wei, L.; Haq, M.Z. Effect of Coronavirus-19 on Mental Condition of International Students in China. Front. Psychiatry 2022, 12, 2398. [Google Scholar] [CrossRef]
- Fakhar-e-Alam Kulyar, M.; Bhutta, Z.A.; Shabbir, S.; Akhtar, M. Psychosocial Impact of COVID-19 Outbreak on International Students Living in Hubei Province, China. Travel Med. Infect. Dis. 2020, 37, 101712. [Google Scholar] [CrossRef]
- Shafiq, S.; Nipa, S.N.; Sultana, S.; Rahman, M.R.U.; Rahman, M.M. Exploring the Triggering Factors for Mental Stress of University Students amid COVID-19 in Bangladesh: A Perception-Based Study. Child. Youth Serv. Rev. 2021, 120, 105789. [Google Scholar] [CrossRef]
- Khan, A.H.; Sultana, M.S.; Hossain, S.; Hasan, M.T.; Ahmed, H.U.; Sikder, M.T. The Impact of COVID-19 Pandemic on Mental Health & Wellbeing among Home-Quarantined Bangladeshi Students: A Cross-Sectional Pilot Study. J. Affect. Disord. 2020, 277, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Puteikis, K.; Mameniškytė, A.; Mameniškienė, R. Sleep Quality, Mental Health and Learning among High School Students after Reopening Schools during the COVID-19 Pandemic: Results of a Cross-Sectional Online Survey. Int. J. Environ. Res. Public Health 2022, 19, 2553. [Google Scholar] [CrossRef]
- Aolymat, I.; Khasawneh, A.I.; Al-Tamimi, M. COVID-19-Associated Mental Health Impact on Menstrual Function Aspects: Dysmenorrhea & Premenstrual Syndrome, and Genitourinary Tract Health: A Cross Sectional Study among Jordanian Medical Students. Int. J. Environ. Res. Public Health 2022, 19, 1439. [Google Scholar] [CrossRef]
- Da Silva Valadão Fernandes, M.; Martins Vital Da Silva, T.; Rayanne, P.; Noll, S.; Aparecido De Almeida, A.; Noll, M. Depressive Symptoms and Their Associated Factors in Vocational–Technical School Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 3735. [Google Scholar] [CrossRef]
- Kapasia, N.; Paul, P.; Roy, A.; Saha, J.; Zaveri, A.; Mallick, R.; Barman, B.; Das, P.; Chouhan, P. Impact of Lockdown on Learning Status of Undergraduate and Postgraduate Students during COVID-19 Pandemic in West Bengal, India. Child. Youth Serv. Rev. 2020, 116, 105194. [Google Scholar] [CrossRef]
- Sarfraz, M.; Hussain, G.; Shahid, M.; Riaz, A.; Muavia, M.; Fahed, Y.S.; Azam, F.; Abdullah, M.T. Medical Students’ Online Learning Perceptions, Online Learning Readiness, and Learning Outcomes during COVID-19: The Moderating Role of Teacher’s Readiness to Teach Online. Int. J. Environ. Res. Public Health 2022, 19, 3520. [Google Scholar] [CrossRef]
- Jiang, R. Knowledge, Attitudes and Mental Health of University Students during the COVID-19 Pandemic in China. Child. Youth Serv. Rev. 2020, 119, 105494. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Tao, S.; Zhang, Y.; Li, S.; Ma, L.; Yu, Y.; Sun, G.; Li, T.; Tao, F. Geographic Distribution of Mental Health Problems among Chinese College Students during the COVID-19 Pandemic: Nationwide, Web-Based Survey Study. J. Med. Internet Res. 2021, 23, e23126. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xiao, Y.; Liu, Y.; Li, Q.; Shan, C.; Chang, S.; Jen, P.H.S. Mental Health and Psychological Impact on Students with or without Hearing Loss during the Recurrence of the Covid-19 Pandemic in China. Int. J. Environ. Res. Public Health 2021, 18, 1421. [Google Scholar] [CrossRef] [PubMed]
- Affum-Osei, E.; Aboagye, M.O.; Antwi, C.O.; Asante, E.A. Validating the Auckland Individualism–Collectivism Scale (AICS): Testing Factor Structure and Measurement Invariance in Hong Kong and Ghanaian Samples. Psychol. Stud. 2019, 64, 187–199. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, W.; Liu, A.; Lin-Schilstra, L.; Lyu, P. International Students’ Mental Health Care in China: A Systematic Review. Healthcare 2021, 9, 1634. [Google Scholar] [CrossRef]
- Li, W.; Gillies, R.; He, M.; Wu, C.; Liu, S.; Gong, Z.; Sun, H. Barriers and Facilitators to Online Medical and Nursing Education during the COVID-19 Pandemic: Perspectives from International Students from Low- and Middle-Income Countries and Their Teaching Staff. Hum. Resour. Health 2021, 19, 64. [Google Scholar] [CrossRef]
- Li, Y.; Liang, F.; Xu, Q.; Gu, S.; Wang, Y.; Li, Y.; Zeng, Z. Social Support, Attachment Closeness, and Self-Esteem Affect Depression in International Students in China. Front. Psychol. 2021, 12, 399. [Google Scholar] [CrossRef]
- Wang, X.; Hujjaree, K.; Hospital, X.; Wang, F.; Hospital, S.X. Mental Health Impacts for International Students During the COVID-19 Pandemic in China. Prepr. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Shan, C.; Hussain, M.; Sargani, G.R. A Mix-Method Investigation on Acculturative Stress among Pakistani Students in China. PLoS ONE 2020, 15, e0240103. [Google Scholar] [CrossRef]
- Jiang, Q.; Li, Y.; Shypenka, V. Loneliness, Individualism, and Smartphone Addiction Among International Students in China. Cyberpsychol. Behav. Soc. Netw. 2018, 21, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Chen, X.; Li, S.; Liu, Y.; Jacques-Tiura, A.J.; Yan, H. Acculturative Stress and Influential Factors among International Students in China: A Structural Dynamic Perspective. PLoS ONE 2014, 9, e96322. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Yuen, M.; Horta, H. Factors Influencing Life Satisfaction of International Students in Mainland China. Int. J. Adv. Couns. 2020, 42, 393–413. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Lester, L.H. A Multiple Indicators and Multiple Causes (MIMIC) Model of Immigrant Settlement Success. In Paper Presented to the XXVI International Population Conference of the IUSSP; Flinders University: Adelaide, Australia, 2009; pp. 1–44. [Google Scholar]
- Islam, M.S.; Sujan, M.S.H.; Tasnim, R.; Sikder, M.T.; Potenza, M.N.; van Os, J. Psychological Responses during the COVID-19 Outbreak among University Students in Bangladesh. PLoS ONE 2020, 15, e0245083. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The Psychological Impact of the COVID-19 Epidemic on College Students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, Q.; Fan, W.; Makamure, J.; Zheng, C.; Wang, J. Online Mental Health Survey in a Medical College in China During the COVID-19 Outbreak. Front. Psychiatry 2020, 11, 459. [Google Scholar] [CrossRef]
- Gaş, S.; Ekşi Özsoy, H.; Cesur Aydın, K. The Association between Sleep Quality, Depression, Anxiety and Stress Levels, and Temporomandibular Joint Disorders among Turkish Dental Students during the COVID-19 Pandemic. Cranio-J. Craniomandib. Sleep Pract. 2021, 1–6. [Google Scholar] [CrossRef]
- Hakami, Z.; Khanagar, S.B.; Vishwanathaiah, S.; Hakami, A.; Bokhari, A.M.; Jabali, A.H.; Alasmari, D.; Aldrees, A.M. Psychological Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Dental Students: A Nationwide Study. J. Dent. Educ. 2021, 85, 494–503. [Google Scholar] [CrossRef]
- Bermejo-Franco, A.; Sánchez-Sánchez, J.L.; Gaviña-Barroso, M.I.; Atienza-Carbonell, B.; Balanzá-Martínez, V.; Clemente-Suárez, V.J. Gender Differences in Psychological Stress Factors of Physical Therapy Degree Students in the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 810. [Google Scholar] [CrossRef]
- Marie, R.; Journault, A.-A.; Cernik, R.; Welch, P.; Lupien, S.; Mcdermott, B.; Moxon, J.V.; Sarnyai, Z. A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications. Int. J. Environ. Res. Public Health 2022, 19, 4407. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Paluszek, M.M.; Landry, C.A.; Rachor, G.S.; McKay, D.; Taylor, S. Do Pre-Existing Anxiety-Related and Mood Disorders Differentially Impact COVID-19 Stress Responses and Coping? J. Anxiety Disord. 2020, 74, 102271. [Google Scholar] [CrossRef] [PubMed]
- Bendau, A.; Kunas, S.L.; Wyka, S.; Petzold, M.B.; Plag, J.; Asselmann, E.; Ströhle, A. Longitudinal Changes of Anxiety and Depressive Symptoms during the COVID-19 Pandemic in Germany: The Role of Pre-Existing Anxiety, Depressive, and Other Mental Disorders. J. Anxiety Disord. 2021, 79, 102377. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.A.; Chesbro, G.; Larson, R.; Larson, D.; Black, C.D. Short-Term Analysis (8 Weeks) of Social Distancing and Isolation on Mental Health and Physical Activity Behavior During COVID-19. Front. Psychol. 2021, 12, 652086. [Google Scholar] [CrossRef] [PubMed]
- Quintero, M.; Rios, E.; Fuentes-Garcia, A.R.; Gonzalez Sanchez, J.P.; Levels, J.C.; Quintero, A.M.; Rita, A.; Fuentes-Garcia, J.P.; Carlos Gonzalez Sanchez, J. Levels of Physical Activity and Psychological Well-Being in Non-Athletes and Martial Art Athletes during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 4004. [Google Scholar] [CrossRef]
- Radák, Z.; Atalay, M.; Wang, H.; Chen, S.; Chen, T.; Tchounwou, P.B.; de Maio, M.; Bratta, C.; Iannaccone, A.; Castellani, L.; et al. Home-Based Physical Activity as a Healthy Aging Booster before and during COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2022, 19, 4317. [Google Scholar] [CrossRef]
- Friedman, K.; Marenus, M.W.; Murray, A.; Cahuas, A.; Ottensoser, H.; Sanowski, J.; Chen, W. Enhancing Physical Activity and Psychological Well-Being in College Students during COVID-19 through WeActive and WeMindful Interventions. Int. J. Environ. Res. Public Health 2022, 19, 4144. [Google Scholar] [CrossRef]
- Granero-Jiménez, J.; López-Rodríguez, M.M.; Dobarrio-Sanz, I.; Cortés-Rodríguez, A.E. Influence of Physical Exercise on Psychological Well-Being of Young Adults: A Quantitative Study. Int. J. Environ. Res. Public Health 2022, 19, 4282. [Google Scholar] [CrossRef]
- Koch, M.; Park, S. Do Government Responses Impact the Relationship between Age, Gender and Psychological Distress during the COVID-19 Pandemic? A Comparison across 27 European Countries. Soc. Sci. Med. 2022, 292, 114583. [Google Scholar] [CrossRef]
- Horesh, D.; Kapel Lev-Ari, R.; Hasson-Ohayon, I. Risk Factors for Psychological Distress during the COVID-19 Pandemic in Israel: Loneliness, Age, Gender, and Health Status Play an Important Role. Br. J. Health Psychol. 2020, 25, 925–933. [Google Scholar] [CrossRef]
- Antwi, C.O.; Fan, C.J.; Aboagye, M.O.; Brobbey, P.; Jababu, Y.; Affum-Osei, E.; Avornyo, P. Job Demand Stressors and Employees’ Creativity: A within-Person Approach to Dealing with Hindrance and Challenge Stressors at the Airport Environment. Serv. Ind. J. 2019, 39, 250–278. [Google Scholar] [CrossRef]
- Belle, M.A.; Antwi, C.O.; Ntim, S.Y.; Affum-Osei, E.; Ren, J. Am I Gonna Get a Job? Graduating Students’ Psychological Capital, Coping Styles, and Employment Anxiety. J. Career Dev. 2021. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).