The Impact of Sport Activity Shut down during the COVID-19 Pandemic on Children, Adolescents, and Young Adults: Was It Worthwhile?
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Positivity to SARS-CoV-2 Test
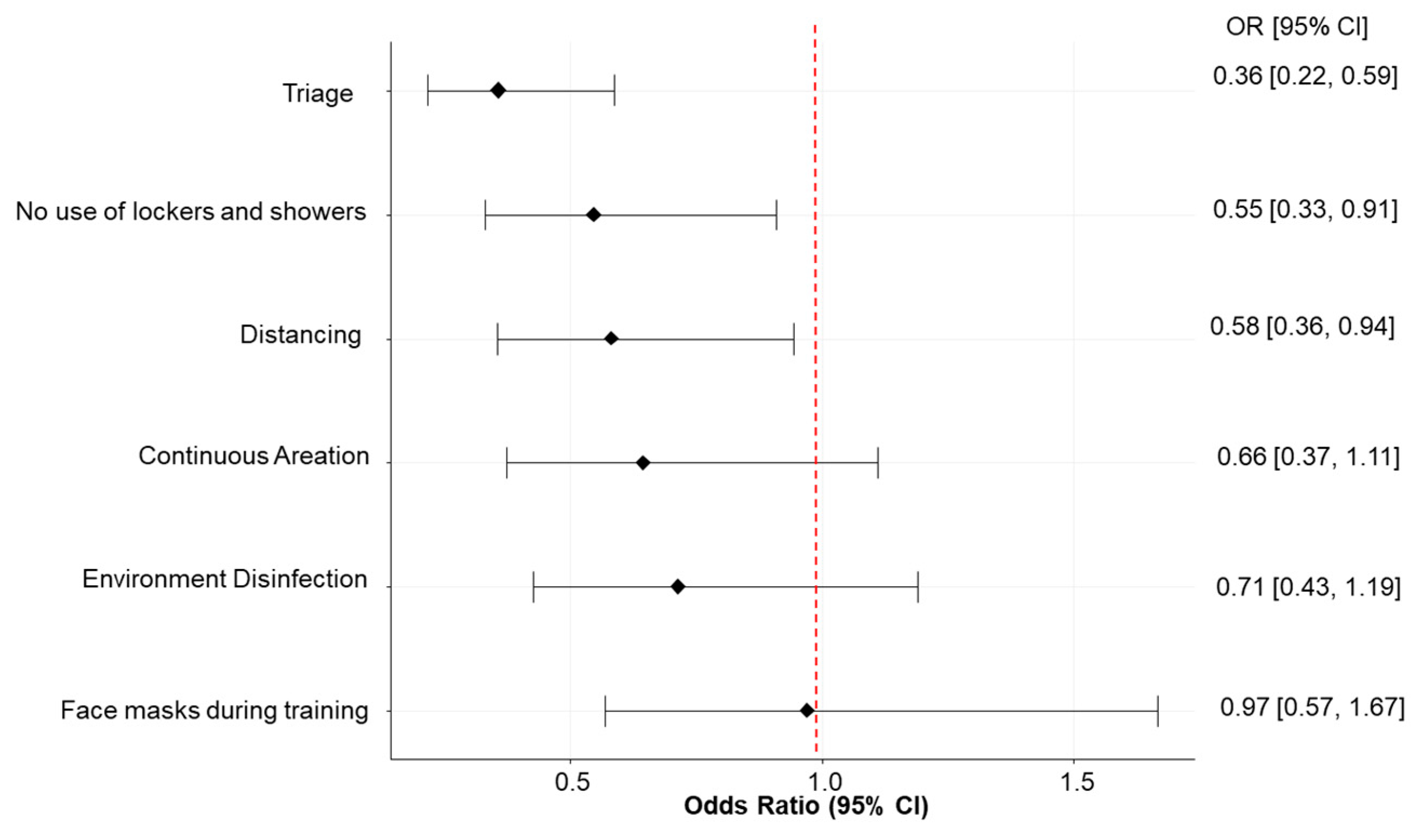
3.2. Preventive Measures
3.3. BMI Change and Adherence to WHO Guidelines for PA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bogoch, I.I.; Watts, A.; Thomas-Bachli, A.; Huber, C.; Kraemer, M.U.G.; Khan, K. Pneumonia of Unknown Aetiology in Wuhan, China: Potential for International Spread via Commercial Air Travel. J. Travel Med. 2020, 27, taaa008. [Google Scholar] [CrossRef] [PubMed]
- Fantini, M.P.; Reno, C.; Biserni, G.B.; Savoia, E.; Lanari, M. COVID-19 and the Re-Opening of Schools: A Policy Maker’s Dilemma. Ital. J. Pediatr. 2020, 46, 79. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Ferran, M.; de la Guía-Galipienso, F.; Sanchis-Gomar, F.; Pareja-Galeano, H. Metabolic Impacts of Confinement during the COVID-19 Pandemic due to Modified Diet and Physical Activity Habits. Nutrients 2020, 12, 1549. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the First COVID-19 Lockdown on Body Weight: A Combined Systematic Review and a Meta-Analysis. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Furukawa, N.W.; Brooks, J.T.; Sobel, J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 while Presymptomatic Or Asymptomatic. Emerg. Infect. Dis. 2020, 26, e201595. [Google Scholar] [CrossRef]
- Sasser, P.; McGuine, T.; Haraldsdottir, K.; Biese, K.; Goodavish, L.; Stevens, B.; Watson, A.M. Reported COVID-19 Incidence in Wisconsin High School Athletes in Fall 2020. J. Athl. Train. 2021, 57, 59–64. [Google Scholar] [CrossRef]
- Atherstone, C.; Siegel, M.; Schmitt-Matzen, E.; Sjoblom, S.; Jackson, J.; Blackmore, C.; Neatherlin, J. SARS-CoV-2 Transmission Associated with High School Wrestling Tournaments—Florida, December 2020–January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 141–143. [Google Scholar] [CrossRef]
- Krug, A.; Appleby, R.; Pizzini, R.; Høeg, T.B. Youth Ice Hockey COVID-19 Protocols and Prevention of Sport-Related Transmission. Br. J. Sports Med. 2022, 56, 29–34. [Google Scholar] [CrossRef]
- Jang, S.; Han, S.H.; Rhee, J.Y. Cluster of Coronavirus Disease Associated with Fitness Dance Classes, South Korea. Emerg. Infect. Dis. 2020, 26, 1917–1920. [Google Scholar] [CrossRef]
- Available online: https://www.Cdc.gov/coronavirus/2019-ncov/science/science-briefs/transmission_k_12_schools.html#sports-Activities (accessed on 5 April 2022).
- Watson, A.M.; Haraldsdottir, K.; Biese, K.; Goodavish, L.; Stevens, B.; McGuine, T. The Association of COVID-19 Incidence with Sport and Face Mask use in United States High School Athletes. J. Athl. Train. 2021. [Google Scholar] [CrossRef]
- Drezner, J.A.; Drezner, S.M.; Magner, K.N.; Ayala, J.T. COVID-19 Surveillance in Youth Soccer during Small Group Training: A Safe Return to Sports Activity. Sports Health 2021, 13, 15–17. [Google Scholar] [CrossRef]
- Schreiber, S.; Faude, O.; Gärtner, B.; Meyer, T.; Egger, F. Risk of SARS-CoV-2 Transmission from on-Field Player Contacts in Amateur, Youth and Professional Football (Soccer). Br. J. Sports Med. 2022, 56, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Seijo Bestilleiro, R.; Suanzes Hernández, J.; Batalla Bautista, D.; Pereira Rodríguez, M.J.; Martín, C.G.; Garcia Rodriguez, M.T.; Pértega Díaz, S. Incidence of COVID-19 in Children and Young People Who Play Federated Football. Sports Health 2022, 14, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R. Physical Education and Sport in Schools: A Review of Benefits and Outcomes. J. Sch. Health 2006, 76, 397–401. [Google Scholar] [CrossRef]
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents Aged 5–17 years: Summary of the Evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef]
- Aubert, S.; Brazo-Sayavera, J.; González, S.A.; Janssen, I.; Manyanga, T.; Oyeyemi, A.L.; Picard, P.; Sherar, L.B.; Turner, E.; Tremblay, M.S. Global Prevalence of Physical Activity for Children and Adolescents; Inconsistencies, Research Gaps, and Recommendations: A Narrative Review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 81. [Google Scholar] [CrossRef]
- Steene-Johannessen, J.; Hansen, B.H.; Dalene, K.E.; Kolle, E.; Northstone, K.; Møller, N.C.; Grøntved, A.; Wedderkopp, N.; Kriemler, S.; Page, A.S.; et al. Variations in Accelerometry Measured Physical Activity and Sedentary Time across Europe—Harmonized Analyses of 47,497 Children and Adolescents. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 38. [Google Scholar] [CrossRef] [Green Version]
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S.; Lancet Physical Activity Series Working Group. The Pandemic of Physical Inactivity: Global Action for Public Health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef] [Green Version]
- Ferrante, G.; Mollicone, D.; Cazzato, S.; Lombardi, E.; Pifferi, M.; Turchetta, A.; Tancredi, G.; La Grutta, S. COVID-19 Pandemic and Reduced Physical Activity: Is there an Impact on Healthy and Asthmatic Children? Front. Pediatr. 2021, 9, 695703. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. The COVID-19 Response must be Disability Inclusive. Lancet Public Health 2020, 5, e257. [Google Scholar] [CrossRef] [Green Version]
- Hemphill, N.M.; Kuan, M.T.Y.; Harris, K.C. Reduced Physical Activity during COVID-19 Pandemic in Children with Congenital Heart Disease. Can. J. Cardiol. 2020, 36, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Golberstein, E.; Wen, H.; Miller, B.F. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatr. 2020, 174, 819–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, R. Projecting the Impact of the Coronavirus Disease-2019 Pandemic on Childhood Obesity in the United States: A Microsimulation Model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.Who.int/tools/growth-Reference-Data-for-5to19-years/indicators/bmi-for-Age (accessed on 5 April 2022).
- Available online: https://www.Who.int/publications/i/item/9789240015128 (accessed on 5 April 2022).
- Matthews, C.E.; Ockene, I.S.; Freedson, P.S.; Rosal, M.C.; Merriam, P.A.; Hebert, J.R. Moderate to Vigorous Physical Activity and Risk of Upper-Respiratory Tract Infection. Med. Sci. Sports Exerc. 2002, 34, 1242–1248. [Google Scholar] [CrossRef]
- Nieman, D.C.; Johanssen, L.M.; Lee, J.W. Infectious Episodes in Runners before and after a Roadrace. J. Sports Med. Phys. Fit. 1989, 29, 289–296. [Google Scholar]
- Chaouachi, A.; Chamari, K.; Wong, P.; Castagna, C.; Chaouachi, M.; Moussa-Chamari, I.; Behm, D.G. Stretch and Sprint Training Reduces Stretch-Induced Sprint Performance Deficits in 13- to 15-Year-Old Youth. Eur. J. Appl. Physiol. 2008, 104, 515–522. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; Abaraogu, U.; Bourgois, J.G.; Dall, P.M.; Darnborough, J.; Duncan, E.; Dumortier, J.; Pavón, D.J.; McParland, J.; Roberts, N.J.; et al. Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis. Sports Med. 2021, 51, 1673–1686. [Google Scholar] [CrossRef]
- Dixon, B.C.; Fischer, R.S.B.; Zhao, H.; O’Neal, C.S.; Clugston, J.R.; Gibbs, S.G. Contact and SARS-CoV-2 Infections among College Football Athletes in the Southeastern Conference during the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2135566. [Google Scholar] [CrossRef]
- Available online: https://www.Aap.org/en/pages/2019-Novel-Coronavirus-Covid-19-infections/clinical-guidance/covid-19-Interim-Guidance-Return-to-Sports/ (accessed on 5 April 2022).
- Pietrabissa, G.; Volpi, C.; Bottacchi, M.; Bertuzzi, V.; Guerrini Usubini, A.; Löffler-Stastka, H.; Prevendar, T.; Rapelli, G.; Cattivelli, R.; Castelnuovo, G.; et al. The Impact of Social Isolation during the COVID-19 Pandemic on Physical and Mental Health: The Lived Experience of Adolescents with Obesity and their Caregivers. Int. J. Environ. Res. Public Health 2021, 18, 3026. [Google Scholar] [CrossRef]
- Abbas, A.M.; Fathy, S.K.; Fawzy, A.T.; Salem, A.S.; Shawky, M.S. The Mutual Effects of COVID-19 and Obesity. Obes. Med. 2020, 19, 100250. [Google Scholar] [CrossRef]
- Holland, S.; Dallos, R.; Olver, L. An Exploration of Young Women’s Experiences of Living with Excess Weight. Clin. Child. Psychol. Psychiatry 2012, 17, 538–552. [Google Scholar] [CrossRef] [PubMed]
- Lachal, J.; Orri, M.; Speranza, M.; Falissard, B.; Lefevre, H.; Qualigramh, M.-R.; Revah-Levy, A. Qualitative Studies among Obese Children and Adolescents: A Systematic Review of the Literature. Obes. Rev. 2013, 14, 351–368. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.L.; Riley, H.; Domoff, S.E.; Gearhardt, A.N.; Sturza, J.; Kaciroti, N.; Lumeng, J.C. Weight Status Moderates Stress-Eating in the Absence of Hunger Associations in Children. Appetite 2019, 136, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Thaker, V.V.; Osganian, S.K.; de Ferranti, S.D.; Sonneville, K.R.; Cheng, J.K.; Feldman, H.A.; Richmond, T.K. Psychosocial, Behavioral and Clinical Correlates of Children with Overweight and Obesity. BMC Pediatr. 2020, 20, 291. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obes. Silver Spring 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Khan, M.A.; Moverley Smith, J.E. "Covibesity", a New Pandemic. Obes. Med. 2020, 19, 100282. [Google Scholar] [CrossRef] [PubMed]
- Nogueira-de-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.L.; Contini, A.A.; Ued, F.D.V. COVID-19 and Obesity in Childhood and Adolescence: A Clinical Review. J. Pediatr. Rio J 2020, 96, 546–558. [Google Scholar] [CrossRef] [PubMed]
- Roland, D.; Harwood, R.; Bishop, N.; Hargreaves, D.; Patel, S.; Sinha, I. Children’s Emergency Presentations during the COVID-19 Pandemic. Lancet Child Adolesc. Health 2020, 4, e32–e33. [Google Scholar] [CrossRef]
- Mitra, R.; Moore, S.A.; Gillespie, M.; Faulkner, G.; Vanderloo, L.M.; Chulak-Bozzer, T.; Rhodes, R.E.; Brussoni, M.; Tremblay, M.S. Healthy Movement Behaviours in Children and Youth during the COVID-19 Pandemic: Exploring the Role of the Neighbourhood Environment. Health Place 2020, 65, 102418. [Google Scholar] [CrossRef]
- Tulchin-Francis, K.; Stevens, W., Jr.; Gu, X.; Zhang, T.; Roberts, H.; Keller, J.; Dempsey, D.; Borchard, J.; Jeans, K.; VanPelt, J. The Impact of the Coronavirus Disease 2019 Pandemic on Physical Activity in U.S. Children. J. Sport Health Sci. 2021, 10, 323–332. [Google Scholar] [CrossRef]
- Kovacs, V.A.; Brandes, M.; Suesse, T.; Blagus, R.; Whiting, S.; Wickramasinghe, K.; Okely, A.D. Are we Underestimating the Impact of COVID-19 on Children’s Physical Activity in Europe?—A Study of 24,302 Children. Eur. J. Public Health 2022, 32, 494–496. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, V.A.; Starc, G.; Brandes, M.; Kaj, M.; Blagus, R.; Leskošek, B.; Suesse, T.; Dinya, E.; Guinhouya, B.C.; Zito, V.; et al. Physical Activity, Screen Time and the COVID-19 School Closures in Europe—An Observational Study in 10 Countries. Eur. J. Sport Sci. 2021, 22, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- McGuine, T.A.; Biese, K.M.; Petrovska, L.; Hetzel, S.J.; Reardon, C.; Kliethermes, S.; Bell, D.R.; Brooks, A.; Watson, A.M. Mental Health, Physical Activity, and Quality of Life of US Adolescent Athletes during COVID-19-Related School Closures and Sport Cancellations: A Study of 13,000 Athletes. J. Athl. Train. 2021, 56, 11–19. [Google Scholar] [CrossRef]
- McGuine, T.A.; Biese, K.M.; Petrovska, L.; Hetzel, S.J.; Reardon, C.L.; Kliethermes, S.; Bell, D.R.; Brooks, A.; Watson, A.M. Changes in the Health of Adolescent Athletes: A Comparison of Health Measures Collected before and during the COVID-19 Pandemic. J. Athl. Train. 2021, 56, 836–844. [Google Scholar] [CrossRef]
- Pombo, A.; Luz, C.; Rodrigues, L.P.; Ferreira, C.; Cordovil, R. Correlates of Children’s Physical Activity during the COVID-19 Confinement in Portugal. Public Health 2020, 189, 14–19. [Google Scholar] [CrossRef]
- Sooriyaarachchi, P.; Francis, T.V.; King, N.; Jayawardena, R. Increased Physical Inactivity and Weight Gain during the COVID-19 Pandemic in Sri Lanka: An Online Cross-Sectional Survey. Diabetes Metab. Syndr. 2021, 15, 102185. [Google Scholar] [CrossRef]
- Bell, A. Designing and testing questionnaires for children. J. Res. Nurs. 2007, 12, 461–469. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Gnagnarella, P.; Dragà, D.; Misotti, A.M.; Sieri, S.; Spaggiari, L.; Cassano, E.; Baldini, F.; Soldati, L.; Maisonneuve, P. Validation of a short questionnaire to record adherence to the Mediterranean diet: An Italian experience. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1140–1147. [Google Scholar] [CrossRef]

| Characteristics | All (N = 1750) $ | At Least One Positive SARS-CoV-2 Test (N = 192, 11%) | No Positive SARS-CoV-2 Test (N = 1558, 89%)- | p-Value * |
|---|---|---|---|---|
| Age ∞ | 12 (9, 15) | 13 (10, 18) | 12 (9, 15) | <0.001 |
| Gender | 0.34 | |||
| Female | 780 (45%) | 78 (10%) | 702 (90%) | |
| Male | 944 (55%) | 109 (12%) | 835 (88%) | |
| Education | <0.001 | |||
| Elementary school or lower | 719 (41%) | 53 (7%) | 666 (93%) | |
| Middle school | 427 (24%) | 50 (12%) | 377 (88%) | |
| High school | 297 (17%) | 23 (8%) | 274 (92%) | |
| Professional high school | 77 (4%) | 14 (18%) | 63 (82%) | |
| University | 152 (9%) | 28 (18%) | 124 (82%) | |
| Other or no school | 75 (4%) | 21 (28%) | 54 (72%) | |
| Any training | 0.31 | |||
| No | 492 (28%) | 59 (12%) | 433 (88%) | |
| Yes | 1258 (72%) | 133 (11%) | 1125 (89%) | |
| Training by closure period ^ | 0.55 | |||
| No | 492 (28%) | 59 (12%) | 433 (88%) | |
| At least one in opening period | 305 (17%) | 29 (10%) | 276 (90%) | |
| At least one in closure period | 953 (54%) | 104 (11%) | 849 (89%) | |
| Weekly training sessions | 0.10 | |||
| No | 492 (28%) | 59 (12%) | 433 (88%) | |
| Up to two | 853 (49%) | 80 (9%) | 773 (91%) | |
| More than two | 405 (23%) | 53 (13%) | 352 (87%) | |
| Baseline BMI ∞ | 18.9 (16.7–21.3) | 19.6 (17.6–22.0) | 18.9 (16.6–21.3) | <0.001 |
| Geographical area | 0.65 | |||
| North | 1127 (66%) | 113 (10%) | 1014 (90%) | |
| Center | 277 (16%) | 26 (9%) | 251 (91%) | |
| South and Islands | 272 (16%) | 33 (12%) | 239 (88%) | |
| Abroad | 30 (2%) | 4 (13%) | 26 (87%) | |
| Number of SARS-CoV-2 tests ∞ | 1 (0–3) | 2 (1–5) | 1 (0–2) | <0.001 |
| Outdoor physical activity | 0.05 | |||
| No | 549 (32%) | 48 (9%) | 501 (91%) | |
| Yes | 1194 (67%) | 143 (12%) | 1051 (88%) | |
| Highest parents’ education | <0.001 | |||
| Middle school or lower | 50 (3%) | 17 (34%) | 33 (66%) | |
| High school | 560 (33%) | 67 (12%) | 493 (88%) | |
| University or higher | 1112 (64%) | 103 (9%) | 1009 (91%) | |
| Parents’ workplace | 0.03 | |||
| Home | 345 (20%) | 26 (8 %) | 319 (92%) | |
| At least partially outside | 1383 (80%) | 161 (12%) | 1222 (88%) | |
| Mediterranean Diet | <0.001 | |||
| Adherence | 523 (47%) | 38 (7%) | 485 (93%) | |
| No adherence | 898 (63%) | 121 (13%) | 777 (87%) |
| Overall Analysis (n = 1732) | Enrolled in Sport Centers (n = 1669) | |
|---|---|---|
| OR [95% CI] | OR [95% CI] | |
| Training by closure period ^ | ||
| No | 1.00 [reference] | 1.00 [reference] |
| At least one in opening period | 1.00 [0.60, 1.65] | 0.93 [0.56, 1.55] |
| At least one in closure period | 0.89 [0.61, 1.30] | 0.62 [0.41, 0.93] |
| Gender | ||
| Female | 1.00 [reference] | 1.00 [reference] |
| Male | 1.47 [1.05, 2.07] | 1.42 [0.98, 2.04] |
| Number of SARS-CoV-2 tests * | 1.16 [1.11, 1.21] | 1.19 [1.13, 1.24] |
| Education | ||
| Elementary school or lower | 1.00 [reference] | 1.00 [reference] |
| Middle school | 1.22 [0.80, 1.88] | 1.19 [0.76, 1.87] |
| High school | 0.79 [0.46, 1.36] | 0.83 [0.47, 1.44] |
| Professional high school | 2.16 [1.09, 4.27] | 1.95 [0.94, 4.06] |
| University | 2.30 [1.32, 4.01] | 1.57 [0.85, 2.89] |
| Other or no school | 3.31 [1.75, 6.28] | 1.81 [0.86, 3.81] |
| Highest parents’ education | ||
| University or higher | 1.00 [reference] | 1.00 [reference] |
| High school | 1.22 [0.86 1.73] | 1.21 [0.83, 1.75] |
| Middle school or lower | 3.63 [1.82, 7.27] | 3.85 [1.81, 7.97] |
| Parents’ workplace | ||
| Home | 1.00 [reference] | 1.00 [reference] |
| At least partially outside | 1.57 [1.00, 2.42] | 1.63 [1.00, 2.67] |
| Overall Analysis (n = 1730) | Enrolled in Sport Centers (n = 1668) | |||
|---|---|---|---|---|
| N (% at Least One Positive Test among Cohabitants) | OR [95% CI] | N (% at Least One Positive Test among Cohabitants) | OR [95% CI] | |
| Training by closure period ^ | ||||
| No | 488 (18%) | 1.00 [reference] | 488 (18%) | 1.00 [reference] |
| At least one in opening period | 304 (18%) | 1.20 [0.80, 1.80] | 284 (18%) | 1.09 [0.72, 1.64] |
| At least one in closure period | 938 (19%) | 0.98 [0.71, 1.35] | 896 (17%) | 0.78 [0.56, 1.08] |
| Gender | ||||
| Female | 772 (17%) | 1.00 [reference] | 741 (16%) | 1.00 [reference] |
| Male | 934 (19%) | 1.22 [0.93, 1.59] | 903 (18%) | 1.20 [0.90, 1.60] |
| Geographical area | ||||
| North | 1116 (18%) | 1.00 [reference] | 1082 (17%) | 1.00 [reference] |
| Center | 273 (14%) | 0.61 [0.40, 0.90] | 267 (14%) | 0.64 [0.42, 0.96] |
| South and Islands | 270 (19%) | 1.13 [0.79, 1.62] | 255 (17%) | 1.00 [0.68, 1.48] |
| Abroad | 29 (24%) | 1.01 [0.37, 2.75] | 27 (26%) | 1.19 [0.44, 3.28] |
| Number of SARS-CoV-2 tests * | - | 1.20 [1.15, 1.25] | - | 1.21 [1.16, 1.27] |
| Education | ||||
| Elementary school or lower | 717 (14%) | 1.00 [reference] | 691 (13%) | 1.00 [reference] |
| Middle school | 424 (21%) | 1.25 [0.89, 1.74] | 410 (21%) | 1.28 [0.91 1.81] |
| High school | 289 (12%) | 0.62 [0.40, 0.96] | 284 (12%) | 0.64 [0.41, 1.00] |
| Professional high school | 78 (29%) | 1.82 [1.03, 3.21] | 75 (28%) | 1.84 [1.02, 3.33] |
| University | 147 (24%) | 1.64 [1.01, 2.66] | 141 (21%) | 1.29 [0.77, 2.18] |
| Other or no school | 72 (40%) | 3.09 [1.74, 5.49] | 65 (34%) | 2.16 [1.15, 4.07] |
| Number of cohabitants | - | 1.17 [1.02, 1.33] | - | 1.16 [1.01, 1.33] |
| Highest parents’ education | ||||
| University or higher | 1102 (17%) | 1.00 [reference] | 1067 (16%) | 1.00 [reference] |
| High school | 555 (20%) | 1.14 [0.86, 1.51] | 533 (20%) | 1.11 [0.83, 1.50] |
| Middle school or lower | 48 (38%) | 2.29 [1.17, 4.45] | 45 (18%) | 2.25 [1.13, 4.50] |
| Parents’ workplace | ||||
| Home | 339 (14%) | 1.00 [reference] | 328 (12%) | 1.00 [reference] |
| At least partially outside | 1369 (19%) | 1.60 [1.11, 2.30] | 1318 (18%) | 1.68 [1.14, 2.46] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raimondi, S.; Cammarata, G.; Testa, G.; Bellerba, F.; Galli, F.; Gnagnarella, P.; Iannuzzo, M.L.; Ricci, D.; Sartorio, A.; Sasso, C.; et al. The Impact of Sport Activity Shut down during the COVID-19 Pandemic on Children, Adolescents, and Young Adults: Was It Worthwhile? Int. J. Environ. Res. Public Health 2022, 19, 7908. https://doi.org/10.3390/ijerph19137908
Raimondi S, Cammarata G, Testa G, Bellerba F, Galli F, Gnagnarella P, Iannuzzo ML, Ricci D, Sartorio A, Sasso C, et al. The Impact of Sport Activity Shut down during the COVID-19 Pandemic on Children, Adolescents, and Young Adults: Was It Worthwhile? International Journal of Environmental Research and Public Health. 2022; 19(13):7908. https://doi.org/10.3390/ijerph19137908
Chicago/Turabian StyleRaimondi, Sara, Giulio Cammarata, Giovanna Testa, Federica Bellerba, Federica Galli, Patrizia Gnagnarella, Maria Luisa Iannuzzo, Dorotea Ricci, Alessandro Sartorio, Clementina Sasso, and et al. 2022. "The Impact of Sport Activity Shut down during the COVID-19 Pandemic on Children, Adolescents, and Young Adults: Was It Worthwhile?" International Journal of Environmental Research and Public Health 19, no. 13: 7908. https://doi.org/10.3390/ijerph19137908
APA StyleRaimondi, S., Cammarata, G., Testa, G., Bellerba, F., Galli, F., Gnagnarella, P., Iannuzzo, M. L., Ricci, D., Sartorio, A., Sasso, C., Pravettoni, G., & Gandini, S. (2022). The Impact of Sport Activity Shut down during the COVID-19 Pandemic on Children, Adolescents, and Young Adults: Was It Worthwhile? International Journal of Environmental Research and Public Health, 19(13), 7908. https://doi.org/10.3390/ijerph19137908










