Effects of Subjective Health Perception on Health Behavior and Cardiovascular Disease Risk Factors in Patients with Prediabetes and Diabetes
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants and Data Collection
2.3. Instruments
2.3.1. Subjective Health Status
2.3.2. Health-Related Behaviors
2.3.3. Cardiovascular Disease Risk-Related Indicators
2.3.4. Body and Blood Indices
3. Data Analysis
Ethical Considerations
4. Results
4.1. General Characteristics of the Participants
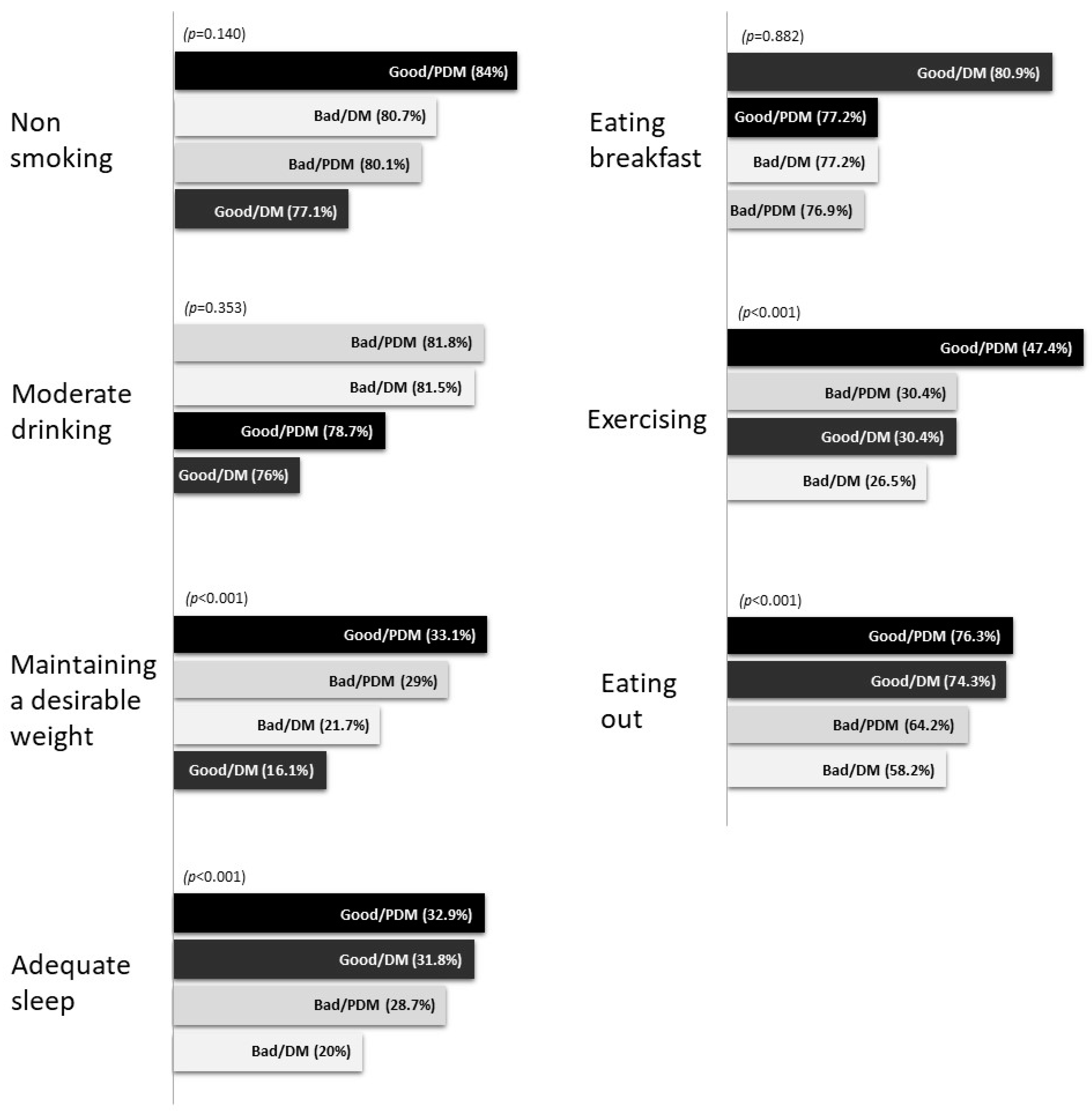
4.2. Health Behaviors
4.3. Cardiovascular Disease-Related Indices
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- L’heveder, R.; Nolan, T. International diabetes federation. Diabetes Res. Clin. Pract. 2013, 101, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Korean Diabetes Association. Diabetes Fact Sheet 2020; Korean Diabetes Association: Seoul, Korea, 2021. [Google Scholar]
- Snoek, F.J.; Skinner, T.C.; Steed, L. Diabetes. In Chronic Physical Illness: Self-Management and Behavioural Interventions; Newman, S., Steed, L., Mulligan, K., Eds.; McGraw-Hill: New York, NY, USA, 2009; pp. 169–188. [Google Scholar]
- Savage, P.J. Cardiovascular complications of diabetes mellitus: What we know and what we need to know about their prevention. Ann. Intern. Med. 1996, 124, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Booth, G.L.; Kapral, M.K.; Fung, K.; Tu, J.V. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: A population-based retrospective cohort study. Lancet 2006, 368, 29–36. [Google Scholar] [CrossRef]
- Jylhä, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009, 69, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Shin, K.R.; Kim, J.S. A study on health concern, self-rated health, health status, and health promotion behavior of elderly women in urban area. J. Korean Acad. Nurs. 2004, 34, 869–880. [Google Scholar] [CrossRef]
- Shin, K.R.; Kim, J.S.; Kim, J.Y. A comparison on self-rated health, health status, and health promotion behaviors between low income and non-low income elderly women. Korean J. Adult Nurs. 2005, 17, 732–742. [Google Scholar]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. BMC Public Health 2013, 13, 320. [Google Scholar] [CrossRef]
- Badawi, G.; Pagé, V.; Smith, K.J.; Gariépy, G.; Malla, A.; Wang, J.; Boyer, R.; Strychar, I.; Lesage, A.; Schmitz, N. Self-rated health: A predictor for the three year incidence of major depression in individuals with Type II diabetes. J. Affect. Disord. 2013, 145, 100–105. [Google Scholar] [CrossRef]
- Wennberg, P.; Rolandsson, O.; Jerdén, L.; Boeing, H.; Sluik, D.; Kaaks, R.; Teucher, B.; Spijkerman, A.; de Mesquita, B.B.; Dethlefsen, C.; et al. Self-rated health and mortality in individuals with diabetes mellitus: Prospective cohort study. BMJ Open 2012, 2, e000760. [Google Scholar] [CrossRef]
- Bishwajit, G.; Tang, S.; Yaya, S.; He, Z.; Feng, Z. Lifestyle behaviors, subjective health, and quality of life among Chinese men living with type 2 diabetes. Am. J. Men’s Health 2017, 11, 357–364. [Google Scholar] [CrossRef]
- Marte, J.L.C.; Javier, A.; Ruiz-Matuk, C.; Paulino-Ramirez, R. Quality of Life and Nutritional Status in diabetic patients on hemodialysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 576–580. [Google Scholar] [CrossRef] [PubMed]
- Boehme, S.; Geiser, C.; Renneberg, B. Functional and self-rated health mediate the association between physical indicators of diabetes and depressive symptoms. BMC Fam. Pract. 2014, 15, 157. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S. The Factors Affecting Self-Rated Health Status in the Aged with Diabetes. J. Korean Data Anal. Soc. 2012, 14, 3075–3086. [Google Scholar]
- Seo, Y.M.; Choi, W.H. Self efficacy and self care behavior in type 2 diabetes mellitus: The mediating effect of subjective health status. J. Korean Data Anal. Soc. 2017, 19, 453–556. [Google Scholar] [CrossRef]
- Park, J.Y. A Study on Self Management, Hemoglobin A1c(HbA1c), and Perceived Health Status for the Type II Diabetes Patients. J. Korean Biol. Nurs. Sci. 2010, 12, 106–113. [Google Scholar]
- Nam, S.I.; Choi, K.H.; Yi, H.J. Self-perceived health status, Depression, and Suicidal Behavior among People with Diabetes. Korean J. Soc. Welf. Stud. 2014, 45, 231–254. [Google Scholar]
- Jang, U.M.; Kim, G.Y. The Relationship between Self-Rated Health Status and Mental Health among Korean Older Adults: The Moderating Role of Self-Rated Socio-Economic Levels. J. Soc. Sci. 2021, 10, 121–144. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care 2010, 33 (Suppl. S1), S11–S61. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Sarwar, N.; Gao, P.; Kondapally Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar]
- Testa, M.A.; Simonson, D.C. Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: A randomized, controlled, double-blind trial. JAMA 1998, 280, 1490–1496. [Google Scholar] [CrossRef] [PubMed]
- Vijan, S.; Hofer, T.P.; Hayward, R.A. EStimated benefits of glycemic control in microvascular complications in type 2 diabetes. Ann. Intern. Med. 1997, 127, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Skyler, J.S.; Bergenstal, R.; Bonow, R.O.; Buse, J.; Deedwania, P.; Gale, E.A.; Howard, B.V.; Sue Kirkman, M.; Kosiborod, M.; Sherwin, R.S.; et al. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA diabetes trials. Circulation 2009, 119, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Nam, Y.H.; Nam, J.R. A Study of the Factors Affecting the Subjective Health Status of Elderly People in Korea. Korean J. Fam. Welf. 2011, 16, 145–162. [Google Scholar]
- Kim, J.S.; Cho, B.L. Association between self-Preceived Health Status and Health Related Behavior in Routine Health Examinees. Korean J. Fam. Med. 2010, 31, 688–696. [Google Scholar] [CrossRef]
- Kwon, Y.M.; Yeun, E.J. The self related health status and related factors in the urban elderly. J. Korean Data Anal. Soc. 2009, 11, 1289–1306. [Google Scholar]
- Kang, Y.H.; Kim, M.Y.; Lee, E. The Relationship of Perceived Health Status, Activities of Daily Living and Nutrition Status in the Community-Dwelling Korean Elderly. J. Korean Acad. Nurs. 2008, 38, 122–130. [Google Scholar] [CrossRef]
- Bailis, D.S.; Segall, A.; Mahon, M.J.; Chipperfield, J.G.; Dunn, E.M. Perceived control in relation to socioeconomic and behavioral resources for health. Soc. Sci. Med. 2001, 52, 1661–1676. [Google Scholar] [CrossRef]
- Haddock, C.K.; Poston, W.S.; Pyle, S.A.; Klesges, R.C.; Vander Weg, M.W.; Peterson, A.; Debon, M. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health Qual. Life Outcomes 2006, 4, 57. [Google Scholar] [CrossRef]
- Kim, N.J. The Effect of Regular Exercise on the Subjective Health and Social Activity of the Elderly. Korean J. Phys. Educ. 2000, 39, 149–158. [Google Scholar]
- Kim, N.J. A Study on Correlations among Menopausal Symptoms, Exercise Performance and Subjective Health Conditions of Middle-aged Women. J. Korean Soc. Health Educ. Promot. 2002, 19, 133–147. [Google Scholar]
- Seib, C.; Parkinson, J.; McDonald, N.; Fujihira, H.; Zietek, S.; Anderson, D. Lifestyle interventions for improving health and health behaviours in women with type 2 diabetes: A systematic review of the literature 2011–2017. Maturitas 2018, 111, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.Y.; Park, J.A. Effect of Health status and Health Behavior on the Diabetes Mellitus Prevalence of Korean Adults. J. Korea Contents Assoc. 2014, 14, 198–209. [Google Scholar] [CrossRef]
- Sung, M.J.; Kim, E.J.; Lee, H.J.; Noh, J.W. Analysis of the prevalence of diabetes mellitus and related factors for the local seniors. J. Korea Contents Assoc. 2014, 14, 244–250. [Google Scholar] [CrossRef]
- Kim, S.H. The association between expectation regarding aging and health-promoting behaviors among korean older adults. J. Korean Acad. Nurs. 2007, 37, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Esteban, C.; Quintana, J.M.; Aburto, M.; Moraza, J.; Egurrola, M.; Pérez-Izquierdo, J.; Aizpiri, S.; Aguirre, U.; Capelastegui, A. Impact of changes in physical activity on health related quality of life among patients with COPD. Capelastegui Eur. Respir. J. 2010, 36, 292–300. [Google Scholar] [CrossRef]
- Song, H.Y. The Airflow Obstruction and Subjective Health Status among Stable Chronic Obstructive Pulmonary Disease Patients Residing in the Community. J. Korean Acad. Nurs. 2017, 19, 38–47. [Google Scholar]
- Kim, H.R. Quality of Life and Its’ Correlates among Older Adults in One Urban Community in Korea: Mediating Effects of Ego Integrity. Korea Gerontol. Soc. 2012, 32, 223–236. [Google Scholar]
- Oh, Y.J.; Kwon, Y.H. Factors Infuencing perceived health status and life satisfaction in rural residents. J. Agric. Med. Community Health 2012, 37, 145–155. [Google Scholar] [CrossRef][Green Version]
- Ngetich, E.; Pateekhum, C.; Hashmi, A.; Nadal, I.P.; Pinyopornpanish, K.; English, M.; Quansri, O.; Wichit, N.; Kinra, S.; Angkurawaranon, C. Illness Perceptions, Self-Care Practices, and Glycemic Control among Type 2 Diabetes Patients in Chiang Mai, Thailand. Arch. Public Health 2022, 80, 134. [Google Scholar] [CrossRef]
| Good/PDM | Bad/PDM | Good/DM | Bad/DM | Total | χ2/F | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||||
| Sex | M | 524 | 53.1 | 312 | 28.6 | 88 | 7.8 | 131 | 10.5 | 1055 | 100.0 | 35.061 | <0.001 |
| F | 599 | 43.5 | 592 | 39.8 | 63 | 4.6 | 176 | 12.1 | 1430 | 100.0 | |||
| Total | 1123 | 48.1 | 904 | 34.5 | 151 | 6.1 | 307 | 11.3 | 2485 | 100.0 | |||
| Weight | 65.3 ± 0.4 (1) | 63.4 ± 0.5 | 68.7 ± 1.1 | 67.3 ± 1.0 | 64.0 ± 0.1 | 10.36 (2) | <0.001 | ||||||
| BMI | 24.3 ± 0.1 | 24.8 ± 0.1 | 26.0 ± 0.3 | 26.4 ± 0.3 | 24.2 ± 0.1 | 26.06 (2) | <0.001 | ||||||
| Age | 40–59 year | 558 | 58.7 | 265 | 27.6 | 52 | 5.5 | 84 | 8.2 | 959 | 100.0 | 80.523 | <0.001 |
| >60 year | 565 | 38.1 | 639 | 40.9 | 99 | 6.7 | 223 | 14.3 | 1526 | 100.0 | |||
| Total | 1123 | 48.1 | 904 | 34.5 | 151 | 6.1 | 307 | 11.3 | 2485 | 100.0 | |||
| Marital status | Single | 28 | 34.7 | 38 | 47.5 | 3 | 3.2 | 11 | 14.6 | 80 | 100.0 | 51.754 | <0.001 |
| Married (living together) | 911 | 52.9 | 602 | 31.0 | 121 | 6.1 | 202 | 10.0 | 1836 | 100.0 | |||
| Married (living apart) | 184 | 33.5 | 264 | 44.4 | 27 | 6.5 | 94 | 15.6 | 569 | 100.0 | |||
| Total | 1123 | 48.1 | 904 | 34.5 | 151 | 6.1 | 307 | 11.3 | 2485 | 100.0 | |||
| Household income | Q1 | 161 | 22.9 | 356 | 51.5 | 43 | 6.7 | 144 | 18.9 | 704 | 100.0 | 193.434 | <0.001 |
| Q2 | 268 | 48.1 | 229 | 34.1 | 32 | 5.1 | 73 | 12.7 | 602 | 100.0 | |||
| Q3 | 319 | 58.7 | 170 | 28.5 | 36 | 5.2 | 49 | 7.6 | 574 | 100.0 | |||
| Q4 | 372 | 62.3 | 145 | 24.6 | 38 | 6.7 | 39 | 6.4 | 594 | 100.0 | |||
| Total | 1120 | 48.2 | 900 | 34.5 | 149 | 6.0 | 305 | 11.3 | 2474 | 100.0 | |||
| Employment | Yes | 736 | 57.3 | 412 | 28.2 | 96 | 6.7 | 116 | 7.8 | 1360 | 100.0 | 103.950 | <0.001 |
| No | 386 | 34.5 | 489 | 43.8 | 55 | 5.2 | 190 | 16.5 | 1120 | 100.0 | |||
| Total | 1122 | 48.1 | 901 | 34.5 | 151 | 6.1 | 306 | 11.3 | 2480 | 100.0 | |||
| Education level | Elementary school | 219 | 24.8 | 440 | 50.5 | 51 | 6.4 | 149 | 18.3 | 859 | 100.0 | 264.604 | <0.001 |
| Junior high school | 124 | 35.3 | 136 | 41.1 | 28 | 9.4 | 57 | 14.3 | 345 | 100.0 | |||
| High school | 379 | 55.7 | 209 | 29.7 | 38 | 4.8 | 75 | 9.8 | 701 | 100.0 | |||
| University | 400 | 70.6 | 115 | 19.5 | 34 | 5.7 | 24 | 4.2 | 573 | 100.0 | |||
| Total | 1122 | 48.1 | 900 | 34.4 | 151 | 6.1 | 305 | 11.3 | 2478 | 100.0 | |||
| Menopause | No | 156 | 62.4 | 72 | 27.5 | 5 | 1.8 | 18 | 8.2 | 251 | 100.0 | 44.015 | <0.001 |
| Yes | 432 | 38.1 | 508 | 43.2 | 56 | 5.4 | 155 | 13.3 | 1151 | 100.0 | |||
| Total | 588 | 43.5 | 580 | 39.8 | 61 | 4.6 | 173 | 12.2 | 1402 | 100.0 | |||
| Good/PDM | Bad/PDM | Good/DM | Bad/DM | Total | χ2 | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % (1) | n | % | n | % | n | % | n | % | |||
| Non-smoking | 980 | 84.0 | 756 | 80.1 | 119 | 77.1 | 248 | 80.7 | 2103 | 81.9 | 5.477 | 0.140 |
| Moderate drinking | 896 | 78.7 | 760 | 81.8 | 116 | 76.0 | 255 | 81.5 | 2027 | 79.9 | 3.259 | 0.353 |
| Maintaining a desirable weight | 389 | 33.1 | 268 | 29.0 | 28 | 16.1 | 64 | 21.7 | 749 | 29.4 | 24.155 | <0.001 |
| Adequate sleep | 359 | 32.9 | 263 | 28.7 | 45 | 31.8 | 71 | 20.0 | 738 | 29.9 | 15.694 | 0.001 |
| Eating breakfast | 901 | 77.2 | 722 | 76.9 | 126 | 80.9 | 244 | 77.2 | 1993 | 77.3 | 0.915 | 0.822 |
| Exercising | 520 | 47.4 | 263 | 30.4 | 43 | 30.4 | 80 | 26.5 | 906 | 38.1 | 62.357 | <0.001 |
| Eating out | 713 | 58.2 | 725 | 76.3 | 104 | 64.2 | 241 | 74.3 | 1783 | 66.6 | 58.032 | <0.001 |
| Good/PDM | Bad/PDM | Good/DM | Bad/DM | F | p | |
|---|---|---|---|---|---|---|
| SBP | 120.88 ± 0.52 | 124.44 ± 0.62 | 126.4 ± 1.27 | 128.88 ± 1.4 | 15.53 | <0.001 |
| DBP | 77.06 ± 0.34 | 76.21 ± 0.42 | 77.92 ± 1.07 | 75.84 ± 0.83 | 1.73 | 0.160 |
| TC | 202.61 ± 1.28 | 193.08 ± 1.65 | 194.49 ± 4.39 | 181.6 ± 2.89 | 18.62 | <0.001 |
| HDL-C | 50.18 ± 0.4 | 47.88 ± 0.43 | 43.87 ± 1.04 | 44.8 ± 0.86 | 19.14 | <0.001 |
| LDL-C | 122.43 ± 2.80 | 120.39 ± 3.65 | 126.28 ± 5.76 | 105.44 ± 4.95 | 3.43 | 0.017 |
| CVD score | 10.75 ± 0.15 | 12.24 ± 0.16 | 12.59 ± 0.33 | 13.41 ± 0.26 | 35.53 | <0.001 |
| TG | 141.99 ± 3.79 | 155.64 ± 5.82 | 199.56 ± 15.43 | 197.14 ± 15.44 | 9.16 | <0.001 |
| Glucose | 100.55 ± 0.44 | 101.88 ± 0.58 | 147.78 ± 4.17 | 150.54 ± 3.25 | 111.59 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwak, S.; Lee, Y.; Baek, S.; Shin, J. Effects of Subjective Health Perception on Health Behavior and Cardiovascular Disease Risk Factors in Patients with Prediabetes and Diabetes. Int. J. Environ. Res. Public Health 2022, 19, 7900. https://doi.org/10.3390/ijerph19137900
Kwak S, Lee Y, Baek S, Shin J. Effects of Subjective Health Perception on Health Behavior and Cardiovascular Disease Risk Factors in Patients with Prediabetes and Diabetes. International Journal of Environmental Research and Public Health. 2022; 19(13):7900. https://doi.org/10.3390/ijerph19137900
Chicago/Turabian StyleKwak, Sungjung, Yoonmi Lee, Seunghui Baek, and Jieun Shin. 2022. "Effects of Subjective Health Perception on Health Behavior and Cardiovascular Disease Risk Factors in Patients with Prediabetes and Diabetes" International Journal of Environmental Research and Public Health 19, no. 13: 7900. https://doi.org/10.3390/ijerph19137900
APA StyleKwak, S., Lee, Y., Baek, S., & Shin, J. (2022). Effects of Subjective Health Perception on Health Behavior and Cardiovascular Disease Risk Factors in Patients with Prediabetes and Diabetes. International Journal of Environmental Research and Public Health, 19(13), 7900. https://doi.org/10.3390/ijerph19137900






