Abstract
The aim of this study is to estimate the association between employment conditions and mental health status in the working population of Iberoamerica. In this cross-sectional study, we pooled individual-level data from nationally representative surveys across 13 countries. A sample of 180,260 workers was analyzed. Informality was assessed by social security, health affiliation, or contract holding. Mental health was assessed using several instruments. We used Poisson regression models to estimate the contribution of informality to poor mental health by sex and country, adjusted by sociodemographic and work-related characteristics. Then, we performed a meta-analysis pooling of aggregate data using a random-effects inverse-variance model. Workers in informal employments showed a higher adjusted prevalence ratio (aPR) of poor mental health than those in formal employment in Peru (aPR men 1.5 [95% confidence intervals 1.16; 1.93]), Spain (aPR men 2.2 [1.01; 4.78]) and Mexico (aPR men 1.24 [1.04; 1.47]; women 1.39 [1.18; 1.64]). Overall estimates showed that workers in informal employment have a higher prevalence of poor mental health than formal workers, with it being 1.19 times higher (aPR 1.19 [1.02; 1.39]) among men, and 1.11 times higher prevalence among women (aPR 1.11 [1.00; 1.23]). Addressing informal employment could contribute to improving workers’ mental health.
1. Introduction
Paid work is a social determinant of health that can act to either promote or hinder wellness. It provides financial security, personal identity, and an opportunity to make a meaningful contribution to community life [1]. However, there are stressful characteristics of work related to demands, control, and support that can act to the detriment of workers’ health [2].
Informal employment is defined as a non-regulated placement in the labor market that involves an undocumented arrangement between employee and employer in which there is no labor regulation, income taxation, social protection or entitlement to certain benefits, such as advance notice of dismissal, or unemployment and sick leave benefits [3]. Workers in informal employment may be exposed, to a greater extent, to the stressful characteristics of work and this may be reflected in their mental health status.
Underemployment [4,5], an unfavorable psychosocial environment with high demands and low control or an effort-reward imbalance [6,7,8], low procedural or relational justice [9,10,11], and non-permanent work have been associated with mental disorders [12,13,14,15,16,17]. However, evidence of the impact of informality on mental health is limited [18] and most previous studies were conducted in upper income countries [16,19,20,21].
The Iberoamerican community is composed of 22 Spanish- and Portuguese-speaking countries (19 Latin American countries, plus Spain, Portugal and Andorra). The relations between Iberoamerican countries have been intensifying, especially multilateral agreement on social security, which has been led by the Ibero-American Social Security Organisation (OISS by its acronym in Spanish) [22]. The current and foreseen trade agreements between the European Union and Latin America require the guarantee of conditions of equality and basic elements for sustainability, including policies that ensure decent and productive work [23]. Evidence from Iberoamerica is scarce and controversial. Previous studies showed that Brazilian workers in informal employment (categorized as self-employed and underemployed) have a higher prevalence of common mental disorders than those in formal employment, and that this association is stronger among women [16,24]. In Central America, workers lacking social security coverage showed a higher prevalence of poor mental health [25]. On the contrary, results from Colombia show that most informal workers perceive their health as normal, good, or very good and are satisfied with their quality of life. However, these results have not been compared to those of workers in formal employment [26]. Results from Chile show that the prevalence of poor mental health is higher among informal workers when compared to formal workers only in the case of male dependent workers, and that there are no differences among women [18].
The aim of this study is to assess the relationship between poor mental health and informal employment among a sample of workers from 13 Iberoamerican countries.
2. Materials and Methods
2.1. Study Design
Cross-sectional.
2.2. Data Source and Study Participants
Nationally representative surveys of household, health, or working conditions were identified for 13 Iberoamerican countries (Table 1). These 13 countries were selected for the study because data could be found that met the following criteria. Eligible surveys were performed after 2012 and included individual-level data on employment conditions and mental health assessed by a valid instrument. When more than one survey for a country complied with inclusion criteria, the most recent was chosen.

Table 1.
Data source and mental health measurement tool.
According to methodological reports from these surveys, all interviews were performed face-to-face at the interviewees’ houses. Our sample was restricted to those who had worked during the week preceding the interview, or were absent from work whether due to leave, illness, strike or attendance at a work-related course. This resulted in a sample of 180,260 workers aged 15 and over.
2.3. Variables
2.3.1. Outcome
Mental health status was assessed by five different instruments. For the World Health Organization—Five Well-Being Index (WHO-5), poor mental health was defined as a score under 13 [27]; for the 9-item Patient Health Questionnaire (PHQ-9), as a score of 10 or more [28]; for the psychological domain of the Abbreviated World Health Organization Quality of Life questionnaire (WHOQOL-Bref), as a score under 60 [29]; for the 12-item General Health Questionnaire (GHQ-12) following the GHQ usual scoring method (0–0–1–1), as a score of 3 or more [30]; and for the affect domain of the Washington Group Extended Set on Functioning (WG-ES), as a score of 4 in either depression or anxiety scales [31].
2.3.2. Work-Related Variables
Regarding employment conditions, in order to operationalize the variable of informal employment, according to the ILO approach [32], social security or health affiliation, or having a contract, were the criteria used based on the information available. Workers were classified according to their social security affiliation as either formal (affiliated) or informal (not affiliated). This was the case for Argentina, countries in Central America, and Peru. When information on social security was not available, classification was based on affiliation with a health system: workers who were entitled to health services as holders were considered formal and those not entitled or entitled as beneficiaries for other family members were considered informal. This was the case for Brazil. In the case of Chile, Mexico, Portugal, and Spain, due to data availability, employment status was based on contract holding. Workers holding a contract were considered formal and those working without a contract were considered informal (Supplementary Table S1).
Regarding labor relationship, workers were classified as an employee, self-employed or an employer. Occupational category was first transformed from local classification into the International Standard Classification of Occupation (ISCO-08) [33] and then grouped into four categories: non-manual skilled (managers, professionals, technicians and associate professionals), non-manual non-skilled (clerical support and services and sales workers), manual skilled (skilled agricultural, forestry and fishery workers, craft and related trades workers, and plant and machine operators and assemblers), and manual non-skilled (elementary occupations). Further aggrupation into manual and non-manual was performed. Workers in the armed forces were excluded from the analysis.
2.3.3. Socio-Demographic Variables
Age comprised four categories (younger than 24; 25–44; 45–64; and over 65 years old). Highest educational level achieved was categorized into less than primary school; primary school; middle school; and higher education. Marital status comprised two categories: married or cohabiting; and single, separated, or widowed.
2.4. Analysis
At the country level, we describe the population distribution by frequencies and weighted proportions (N%). We estimated the prevalence of poor mental health with a 95% confidence interval (95% CI) by work-related and socio-demographic characteristics, and estimated the association between employment condition and poor mental health by crude prevalence ratios (cPR) using Poisson regression with robust variance. Models were adjusted by age, marital status, education, occupational category, and labor relationship in the case of Argentina, Chile, Peru, Brazil and countries in Central America. Models for Spain and Portugal were adjusted by age, marital status, education, and occupational category, and models for Mexico were adjusted by age, marital status, and education due to data availability. Country-specific survey weights were applied. All analyses were stratified by sex.
Second, a meta-analysis [34] pooling of aggregate data from each country using a random-effects inverse-variance model was performed to assess the overall effect of employment condition on mental health status in the region. The analysis was stratified by a mental health measurement tool.
3. Results
3.1. Population Characteristics
Workers in informal employment represent more than 40% (N = 83,781) of the working population in Iberoamerica according to the surveys included in this study. Informality was highest in Guatemala (men: 88.0% [85.1; 90.4]; women: 88.3% [85.0; 91.0]) and lowest in Spain (men: 3.9% [2.70; 5.10]; women: 6.8% [5.27; 8.25]). Spain also showed the lowest proportion of workers in manual occupations (men: 43.5% [40.6; 46.3]; women: 23.6% [21.2; 25.9]), while Honduras showed the highest (men: 82.5% [79.6; 85.0]; women: 57.3 [52.6; 61.9]). Men showed higher rates of working in manual occupations than women across all countries. Approximately 17% of workers (N = 31,135) did not finish primary school, this figure being below 3% in Spain and Portugal and above 25% for Brazil. Women represented a lower proportion of unschooled workers than men, except for in the cases of Peru and Guatemala (Supplementary Table S2).
3.2. Mental Health Distribution
Among the countries using GHQ-12, the lowest prevalence of poor mental health was found in Guatemalan men (8.1% [5.94; 11.0]) and Salvadoran women (11.0% [8.5; 13.4]), while the highest was found in Peruvian workers (men 27.9% [25.5; 30.4); women 32.5% [29.9; 35.3]). Among the countries using WHO-5, Argentine workers showed a considerably higher prevalence of poor mental health (men: 15.6% [14.4; 16.8]; women: 21.9 [20.2; 23.5]) than workers in Spain (men 9.9% [8.4; 11.8]; women 13.7% [11.8; 15.9]) and Portugal (men: 11.6% [8.44; 15.8]; women 14.1% [11.1; 17.7]). Women consistently showed a higher prevalence of poor mental health than men across countries, except for Costa Rica (men 15.1% [10.7; 19.6]; women 14.8 [11.0; 18.7]).
The differences between the sexes were greater for Brazil, with a prevalence ratio of women: men (W:M) of 2.89 and an absolute difference of 8.70 percentage points (pp) (men 4.6% [4.2; 5.0]; women 13.3% [12.6; 14.1]), followed by Mexico and Guatemala, regarding relative difference (W:M Mexico 1.76 Guatemala 1.65), and by Argentina and Chile, regarding absolute differences (Argentina 6.30 pp, Chile 6.0 pp).
The least educated workers showed a higher prevalence of poor mental health than the most educated across regions, except for Panamanian and Brazilian male workers. Differences in the prevalence of poor mental health between the lowest and highest educational categories were greater for women than for men, except in the cases of El Salvador (men 4.8 pp, women 2.3 pp) and Spain (men 10.2 pp, women 7.2 pp) (Table 2 and Table S3).

Table 2.
Prevalence of poor mental health (%) according to work and sociodemographic variables, by questionnaire, country, and sex.
3.3. Informality and Poor Mental Health
Informal workers showed a higher prevalence of poor mental health than their counterparts across most countries and both sexes. However, formal male workers from Panama (27.0% vs. 19.2%), Portugal (11.1% vs. 10.7%), and Brazil (4.8% vs. 4.5%) and formal female workers from El Salvador (14.5% vs. 10.5%) showed a higher prevalence of poor mental health than informal workers (Table 2 and Table S3).
The prevalence ratios of poor mental health between informal and formal workers were significant in the case of male workers from Costa Rica (cPR 1.80 [1.00; 3.25]), Peru (cPR 1.63 [1.31; 2.01]), and Mexico (cPR 1.17 [1.00; 1.37]) and female workers from Peru (cPR 1.45 [1.15; 1.83]), Chile (cPR 1.51 [1.10; 2.06]), Brazil (cPR 1.17 [1.02; 1.34]), and Mexico (cPR 1.55 [1.34; 1.79]). Overall crude estimates show that men and women in informal employment had a 22% and 27% higher prevalence of poor mental health than their formal counterparts, respectively (cPR men 1.22 [1.03; 1.39]; women 1.27 [1.12; 1.43]) (Table 3).

Table 3.
Prevalence ratio of poor mental health between formal (Ref.) and informal workers by country and sex.
In adjusted models, men in informal employment showed a higher prevalence of poor mental health than formal workers in Peru (aPR 1.5 [1.16; 1.93]), Spain (aPR 2.2 [1.01; 4.78]), and Mexico (aPR 1.24 [1.04; 1.47]). In the case of women, the results are statistically significant only in the case of Mexico (aPR 1.39 [1.18; 1.64]). Overall adjusted estimates continue to show a higher prevalence or poor mental health in informal workers when compared with formal workers, although these values are lower than the crude estimates. Overall, among men, informal workers showed a 1.19 times higher prevalence of poor mental health than formal workers (aPR 1.19 [1.02; 1.39]). Among women, informal workers showed a 1.11 higher prevalence than formal workers (aPR 1.11 [1.00; 1.23]) (Table 3 and Figure 1).
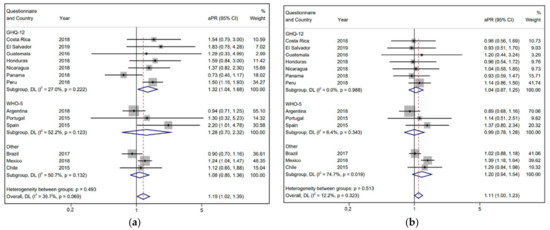
Figure 1.
Forest plots showing adjusted prevalence ratios (aPR) of poor mental health between informal and formal workers of Iberoamerica, by country and mental health questionnaire, and overall estimates from the meta-analysis. (a) Men. (b) Women. The dashed red line shows the overall result.
4. Discussion
Our results show that, overall, Iberoamerican workers in informal employment have a higher prevalence of poor mental health than workers in formal employment. However, the results are heterogeneous among countries and, in most cases, we could not establish a robust association between informality and poor mental health. These results may be due to various reasons: The inaccurate measurement of mental health status; the inaccurate measurement of informality; unobserved confounding factors concealing a real association; or a non-existing association between informality and poor mental health. It is important to note that informal employment is related not only to poor working and employment conditions, but also to poor living conditions, social and economic vulnerability, and poor environmental conditions. All of these factors could affect the association. Previous studies showed that national indicators of GDP, CO2 emissions, educational attainment, life expectancy, rates of poverty, and women’s labor market participation are strongly associated with the rate of informality [35].
4.1. Mental Health Status Measurement
Regarding the prevalence of poor mental health, the information found was heterogeneous, with poorly standardized records, making it difficult to establish accurate regional comparisons. The mental health questionnaires used in each survey measure different concepts of health. Take, for example, PHQ-9 and WHO-5. The former scores each of the nine DSM-IV criteria for depression with questions such as “Have you felt depressed or hopeless?”, while the latter assesses psychological well-being with statements such as “I have felt cheerful and in good spirit”. However, other studies have established measurement similarities between PHQ-9 and GHQ-12 [36,37], WHO-5 and GHQ-12 [38], WHO-5 and PHQ-9 [39], and PHQ-9 and the depression domain of WG-ES [40]. Besides differences across questionnaires, differences in social, cultural and historical background across countries may influence workers’ perception of their mental health and quality of life, both being closely related to one’s expectations. Thus, even when using the same questionnaire, mental health evaluation requires a country-specific analysis, and questionnaire validation in each country is encouraged [41].
In addition, estimates of poor mental health may be underestimated for two reasons: first, the prevalence of somatic symptom in Latin America is high, while mood symptoms are underrepresented [42]. Hence, we would expect low rates of self-identified depression. Second, GHQ-12, although used extensively, may not be the best screening tool [43].
The prevalence of poor mental health in Mexico is remarkably low; however, the case definition refers to mental conditions causing high disability. Other studies have already reported similar rates when severity is considered [44,45].
4.2. Exposure Measurement
Informality was defined according to ILO specifications, and rates of informal employment described hereby are similar to those depicted by ILO [46], implying general measurement accuracy, except for El Salvador and Brazil where we found higher rates, and Spain and Chile where we found lower rates. Nevertheless, other authors have already argued that this definition may be insufficient to analyze the context of the Latin American working population [47]. Furthermore, employment conditions on the main job are used to depict informality, but a person can simultaneously have two or more formal and/or informal jobs. The proportion of workers holding multiple jobs varied in the sample, from 3% in Mexico to around 19% in Argentinian women and Peruvian men, and was not available for Chile. The characteristics of these other jobs could not be ascertained.
Formal workers may not be as protected as we would expect, diminishing the differences between formal and informal workers. Workers at formal jobs may also be exposed to other work-related risk factors for poor mental health, such as an increased number of working hours, unpaid overtime, poor job security, poor satisfaction with one’s work culture and a feeling of a lack of support, low income, shift work, and night work [48,49]. Moreover, the provision of mental health services represents less than 1% of government health spending in low- and middle-income countries, and rates of availability and uptake for mental health services remain very low [50]. Therefore, health and social services may not meet the mental health needs of formal workers in the region. On the other hand, workers may have other support systems outside social security and state resources.
4.3. Unobserved Confounders
Other life circumstances may have a greater impact on mental health than employment condition and may act as unobserved confounders. Exposure to poverty, food insecurity, trauma, housing instability, and decreased social support have all been proven to affect one’s physical and mental well-being [51,52]. Race and migrant status have also been proven to highly affect mental health. Information on these circumstances could not be ascertained for each country and was, therefore, not included in the analysis. Future studies should explore the effect of these living conditions on the association between informality and poor mental health.
4.4. Education
When adjusting for the highest education level achieved, the magnitude of the association between informality and poor mental health decreased, implying that part of that association was explained by education. Low education may be associated with poor mental health in two ways: early onset disorders have been shown to impact school dropout, and school dropout has been proposed as a cause of internalizing disorders [53,54,55].
4.5. Gender
The association between informality and poor mental health was higher and stronger for men than for women when adjusting for sociodemographic and other work-related variables. The unequal involvement of women in unpaid labor can wield deleterious effects on their mental health and may explain some of the differences found between the sexes [56]. Information on care load and domestic work was only available for questionnaires from Brazil and Chile. In Brazil, women were in charge of caring for dependents (children, the elderly, the sick or people with special needs) more frequently than men, and those in charge of care showed a higher prevalence of poor mental health. In Chile, the results were similar, with a larger percentage of women in charge of caring for dependents and domestic work than men. Women with double presence showed a significantly higher prevalence of poor mental health.
4.6. Strengths and Limitations
The findings should be considered in light of the limitations of this study. First, in all cases, survey participants were limited to those with permanent residence and sufficient proficiency in the official language (Spanish or Portuguese), and therefore the prevalence of poor mental health may be underestimated by the exclusion of the most vulnerable workers, such as immigrants. Second, the surveys included relied solely on retrospective self-reports; hence, the data are subject to recall bias and the willingness to disclose information truthfully. Given the generally stigmatizing nature of mental health disorders, it is likely that reporting bias leads to an underestimation of prevalence. The cross-sectional design of the study prevented us from making inferences regarding causality or directionality between socio-demographic and work-related correlates and mental health status. To operationalize informal employment, and according to the ILO approach [32], different criteria were used for each country, depending on the information available: affiliation with social security, with a health system or with having a contract. However, in many countries, workers with a contract must be affiliated with a pension or health system, and thus not being affiliated with social security or a health system is tantamount to the same concept: informality. Another important limitation is that mental health status was assessed using five different instruments. However, all instruments used were validated, widely recognized and reliable measures of mental health. In addition, we measured the prevalence ratio of poor mental health between formal and informal workers within countries using the same instrument. Finally, given that the data come from different countries and therefore from different sources, the methodologies might have differed slightly. In addition, the surveys were conducted in different years, between 2012 and 2018. However, this study used data from each country to measure the difference between the mental health of informal and formal workers within countries. All these limitations encourage caution when interpreting the results.
Despite these limitations, to our knowledge this is the first study to report on the mental health status of the working population of Iberoamerica as a whole and to highlight the deleterious effect of informality on workers’ mental health, regardless of other sociodemographic and work-related characteristics. In this study, we provide evidence, based on the most recent data available, for local occupational health planning and a starting point for further surveillance in the region.
5. Conclusions
Addressing informal employment could contribute to improving the mental health of workers in Iberoamerica. Work is a key determinant of workers’ mental health, but other determinants such social and living conditions should be included in prevention policies. Given the great heterogeneity among surveys in the region, we recommend further research to incorporate common indicators of mental health and informality in order to enable comparisons. Additionally, variables such as hours dedicated to unpaid work at home and care for dependents should be included to better analyze the interaction between work, gender, and mental health.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijerph19137883/s1. Table S1: Definition of employment condition by questionnaire. Table S2: Population distribution by questionnaire, country and sex. Table S3: Prevalence of poor mental health (% (95% CI)) according to work and sociodemographic variables, by questionnaire, country, and sex.
Author Contributions
Conceptualization, F.G.B. and M.S.-P.; methodology, P.S.; validation, M.S.-P.; formal analysis, P.S.; investigation, M.S.-P. and P.S.; data curation, P.S.; writing—original draft preparation, P.S.; writing—review and editing, M.S.-P. and F.G.B.; visualization, P.S.; supervision, F.G.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its characteristics. The datasets analyzed were properly anonymized and informed consent was obtained at the time of the original data collection, in which the researchers took no part.
Informed Consent Statement
Informed consent was obtained at the time of the original data collection.
Data Availability Statement
In this study, the datasets analyzed were publicly available from some countries, while others were obtained from third parties. Restrictions may apply to the availability of these latter datasets. Datasets are available at the following addresses: Argentina: https://www.argentina.gob.ar/srt/observatorio-srt/encuestas-salud-trabajo/ECETSS-2018 (accessed on 14 January 2022); Brazil: https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=microdados (accessed on 14 January 2022); Chile: http://epi.minsal.cl/bases-de-datos/ (accessed on 14 January 2022); Centro America: The University of Texas Health Science Center at Houston (UTHealth) https://sph.uth.edu/research/centers/swcoeh/central-america/ (accessed on 14 January 2022) Available under request; Peru: Instituto Nacional de Salud: https://web.ins.gob.pe/ (accessed on 14 January 2022) Available under request; Mexico: https://www.inegi.org.mx/programas/enh/2017/#:~:text=La%20Encuesta%20Nacional%20de%20los.y%20las%20comunicaciones%20en%20los (accessed on 14 January 2022); Spain and Portugal: European Foundation for the Improvement of Living and Working Conditions. (2020). European Working Conditions Survey Integrated Data File. 1991–2015. [data collection]. 8th Edition. UK Data Service. SN: 7363. DOI: 10.5255/UKDA-SN-7363-8. Available under request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fact Sheet Library|NAMI: National Alliance on Mental Illness. Available online: https://www.nami.org/About-Mental-Illness/Mental-Health-by-the-Numbers/Infographics-Fact-Sheets (accessed on 14 January 2022).
- Harnois, G.; Gabriel, P.; WHO; ILO. Mental Health and Work: Impact, Issues and Good Practices; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- ILO. Informality and Non-Standard Forms of Employment; ILO: Geneva, Switzerland, 2018. [Google Scholar]
- Dooley, D.; Prause, J.; Ham-Rowbottom, K.A. Underemployment and Depression: Longitudinal Relationships. J. Health Soc. Behav. 2000, 41, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Friedland, D.S.; Price, R.H. Underemployment: Consequences for the Health and Well-Being of Workers. Am. J. Commun. Psychol. 2003, 32, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Van Der Doef, M.; Maes, S. The Job Demand-Control(-Support) Model and Psychological Well-Being: A Review of 20 Years of Empirical Research. Work. Stress 1999, 13, 87–114. [Google Scholar] [CrossRef]
- Paterniti, S.; Niedhammer, I.; Lang, T.; Consoli, S.M. Psychosocial Factors at Work, Personality Traits and Depressive Symptoms: Longitudinal Results from the GAZEL Study. Br. J. Psychiatry 2002, 181, 111–117. [Google Scholar] [CrossRef] [Green Version]
- Stansfeld, S.A.; Fuhrer, R.; Shipley, M.J.; Marmot, M.G. Work Characteristics Predict Psychiatric Disorder: Prospective Results from the Whitehall II Study. Occup. Environ. Med. 1999, 56, 302–307. [Google Scholar] [CrossRef] [Green Version]
- Ylipaavalniemi, J.; Kivimäki, M.; Elovainio, M.; Virtanen, M.; Keltikangas-Järvinen, L.; Vahtera, J. Psychosocial Work Characteristics and Incidence of Newly Diagnosed Depression: A Prospective Cohort Study of Three Different Models. Soc. Sci. Med. 2005, 61, 111–122. [Google Scholar] [CrossRef]
- Kivimäki, M.; Elovainio, M.; Vahtera, J.; Virtanen, M.; Stansfeld, S.A. Association between Organizational Inequity and Incidence of Psychiatric Disorders in Female Employees. Psychol. Med. 2003, 33, 319–326. [Google Scholar] [CrossRef] [Green Version]
- Kivimäki, M.; Elovainio, M.; Vahtera, J.; Ferrie, J.E. Organisational Justice and Health of Employees: Prospective Cohort Study. Occup. Environ. Med. 2003, 60, 27. [Google Scholar] [CrossRef] [Green Version]
- Bardasi, E.; Francesconi, M. The Impact of Atypical Employment on Individual Wellbeing: Evidence from a Panel of British Workers. Soc. Sci. Med. 2004, 58, 1671–1688. [Google Scholar] [CrossRef] [Green Version]
- Liukkonen, V.; Virtanen, P.; Kivimäki, M.; Pentti, J.; Vahtera, J. Social Capital in Working Life and the Health of Employees. Soc. Sci. Med. 2004, 59, 2447–2458. [Google Scholar] [CrossRef]
- Virtanen, P.; Liukkonen, V.; Vahtera, J.; Kivimäki, M.; Koskenvuo, M. Health Inequalities in the Workforce: The Labour Market Core-Periphery Structure. Int. J. Epidemiol. 2003, 32, 1015–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Virtanen, M.; Kivimäki, M.; Elovainio, M.; Vahtera, J.; Ferrie, J.E. From Insecure to Secure Employment: Changes in Work, Health, Health Related Behaviours, and Sickness Absence. Occup. Environ. Med. 2003, 60, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Ludermir, A.B.; Lewis, G. Informal Work and Common Mental Disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Bjarnason, T.; Sigurdardottir, T.J. Psychological Distress during Unemployment and beyond: Social Support and Material Deprivation among Youth in Six Northern European Countries. Soc. Sci. Med. 2003, 56, 973–985. [Google Scholar] [CrossRef]
- Ruiz, M.E.; Vives, A.; Martínez-Solanas, È.; Julià, M.; Benach, J. How Does Informal Employment Impact Population Health? Lessons from the Chilean Employment Conditions Survey. Saf. Sci. 2017, 100, 57–65. [Google Scholar] [CrossRef]
- Cai, Y.; Kong, W.; Lian, Y.; Jin, X. Depressive Symptoms among Chinese Informal Employees in the Digital Era. Int. J. Environ. Res. Public Health 2021, 18, 5211. [Google Scholar] [CrossRef]
- Sołtys, A.; Tyburski, E. Predictors of Mental Health Problems in Formal and Informal Caregivers of Patients with Alzheimer’s Disease. BMC Psychiatry 2020, 20, 435. [Google Scholar] [CrossRef]
- Santana, V.S.; Loomis, D.; Newman, B.; Harlow, S.D. Informal Jobs: Another Occupational Hazard for Women’s Mental Health? Int. J. Epidemiol. 1997, 26, 1236–1242. [Google Scholar] [CrossRef]
- Organización Iberoamericana de Seguridad Social OISS—Organización Iberoamericana de La Seguridad Social. Available online: https://oiss.org/medidas-tomadas-por-los-gobiernos-de-iberoamerica-en-relacion-con-el-covid-19/ (accessed on 25 September 2021).
- Organizacion Iberoamericana de Seguridad Social. III Estrategia Iberoamericana de Seguridad y Salud En El Trabajo; OISS: Madrid, Spain, 2021. [Google Scholar]
- Giatti, L.; Barreto, S.M.; Comini César, C. Household Context and Self-Rated Health: The Effect of Unemployment and Informal Work. J. Epidemiol. Commun. Health 2008, 62, 1079–1085. [Google Scholar] [CrossRef]
- López-Ruiz, M.; Artazcoz, L.; Martínez, J.M.; Rojas, M.; Benavides, F.G. Informal Employment and Health Status in Central America Health Behavior, Health Promotion and Society. BMC Public Health 2015, 15, 698. [Google Scholar] [CrossRef] [Green Version]
- Vélez Álvarez, C.; Del Pilar, M.; Potes, E.; Eugenia, M.; Merchán, P. Quality of Life and Informal Labor among Elderly Persons in an Intermediate Colombian City, 2012–2013. Rev. Bras. Geriatr. Gerontol. 2016, 19, 415–427. [Google Scholar] [CrossRef] [Green Version]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.A.B.; Soares, S.M.; Santos, J.F.G.; Silva, L.B. Cut-off Point for WHOQOL-Bref as a Measure of Quality of Life of Older Adults. Rev. Saude Publica 2014, 48, 390–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The Validity of Two Versions of the GHQ in the WHO Study of Mental Illness in General Health Care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Washington Group on Disability Statistics (WG). Development of Disability Measures for Surveys: The Extended Set on Functioning; Organización Iberoamericana de Seguridad Social: Madrid, Spain, 2021. [Google Scholar]
- International Labour Organization (ILO). Measuring Informality: A Statistical Manual on the Informal Sector and Informal Employment; International Labour Organization (ILO): Turin, Italy, 2013; ISBN 9789221273882. [Google Scholar]
- International Labour Office. International Standard Classification of Occupations. Available online: https://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/@publ/documents/publication/wcms_172572.pdf (accessed on 14 January 2022).
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Özgür, G.; Elgin, C.; Elveren, A.Y. Is Informality a Barrier to Sustainable Development? Sustain. Dev. 2021, 29, 45–65. [Google Scholar] [CrossRef]
- Grunauer, M.; Schrock, D.; Fabara, E.; Jimenez, G.; Miller, A.; Lai, Z.; Kilbourne, A.; McInnis, M.G. Tablet-Based Screening of Depressive Symptoms in Quito, Ecuador: Efficiency in Primary Care. Int. J. Fam. Med. 2014, 2014, 845397. [Google Scholar] [CrossRef] [Green Version]
- Martin, A.; Rief, W.; Klaiberg, A.; Braehler, E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the General Population. Gen. Hosp. Psychiatry 2006, 28, 71–77. [Google Scholar] [CrossRef]
- Mergl, R.; Seidscheck, I.; Allgaier, A.K.; Möller, H.J.; Hegerl, U.; Henkel, V. Depressive, Anxiety, and Somatoform Disorders in Primary Care: Prevalence and Recognition. Depress. Anxiety 2007, 24, 185–195. [Google Scholar] [CrossRef]
- Hajos, T.R.S.; Pouwer, F.; Skovlund, S.E.; Den Oudsten, B.L.; Geelhoed-Duijvestijn, P.H.L.M.; Tack, C.J.; Snoek, F.J. Psychometric and Screening Properties of the WHO-5 Well-Being Index in Adult Outpatients with Type 1 or Type 2 Diabetes Mellitus. Diabet. Med. 2013, 30, e63–e69. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M. WG Mental Health Work Group Update WG Mental Health Work Group; The Washington Group on Disability Statistics, University College London: London, UK, 2017. [Google Scholar]
- Benítez-Borrego, S.; Mancho-Fora, N.; Farràs-Permanyer, L.; Urzúa-Morales, A.; Guàrdia-Olmos, J. Differential Item Functioning of WHOQOL-BREF in Nine Iberoamerican Countries. Rev. Iberoam. Psicol. Salud 2016, 7, 51–59. [Google Scholar] [CrossRef] [Green Version]
- Muñoz, R.A.; McBride, M.E.; Brnabic, A.J.M.; López, C.J.; Hetem, L.A.B.; Secin, R.; Dueñas, H.J. Major Depressive Disorder in Latin America: The Relationship between Depression Severity, Painful Somatic Symptoms, and Quality of Life. J. Affect. Disord. 2005, 86, 93–98. [Google Scholar] [CrossRef]
- Hankins, M. The Reliability of the Twelve-Item General Health Questionnaire (GHQ-12) under Realistic Assumptions. BMC Public Health 2008, 8, 355. [Google Scholar] [CrossRef] [Green Version]
- Medina-Mora, M.E.; Borges, G.; Lara, C.; Benjet, C.; Blanco, J.; Fleiz, C.; Villatoro, J.; Rojas, E.; Zambrano, J. Prevalence, Service Use, and Demographic Correlates of 12-Month DSM-IV Psychiatric Disorders in Mexico: Results from the Mexican National Comorbidity Survey. Psychol. Med. 2005, 35, 1773–1783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demyttenaere, K.; Bruffaerts, R.; Posada-Villa, J.; Gasquet, I.; Kovess, V.; Lepine, J.P.; Angermeyer, M.C.; Bernert, S.; de Girolamo, G.; Morosini, P.; et al. Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys. JAMA 2004, 291, 2581–2590. [Google Scholar] [CrossRef]
- International Labour Office. Women and Men in the Informal Economy: A Statistical Picture; ILO: Geneva, Switzerland, 2018; ISBN 9221131033. [Google Scholar]
- Ruiz, M.E.; Tarafa Orpinell, G.; Jódar Martínez, P.; Benach, J. ¿Es Posible Comparar El Empleo Informal En Los Países de América Del Sur? Análisis de Su Definición, Clasificación y Medición. Gac. Sanit. 2015, 29, 65–71. [Google Scholar] [CrossRef] [Green Version]
- Kevric, J.; Papa, N.; Perera, M.; Rashid, P.; Toshniwal, S. Poor Employment Conditions Adversely Affect Mental Health Outcomes Among Surgical Trainees. J. Surg. Educ. 2018, 75, 156–163. [Google Scholar] [CrossRef]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Burton, N.W.; Kolbe-Alexander, T.L. Shift Work and Poor Mental Health: A Meta-Analysis of Longitudinal Studies. Am. J. Public Health 2019, 109, E13–E20. [Google Scholar] [CrossRef]
- Patel, V.; Chisholm, D.; Parikh, R.; Charlson, F.J.; Degenhardt, L.; Dua, T.; Ferrari, A.J.; Hyman, S.; Laxminarayan, R.; Levin, C.; et al. Addressing the Burden of Mental, Neurological, and Substance Use Disorders: Key Messages from Disease Control Priorities, 3rd Edition. Lancet 2016, 387, 1672–1685. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, K.H. Social Determinants of Health: The How, Who, and Where Screenings Are Occurring; a Systematic Review. Soc. Work. Health Care 2019, 58, 719–745. [Google Scholar] [CrossRef] [PubMed]
- Molarius, A.; Berglund, K.; Eriksson, C.; Eriksson, H.G.; Lindén-Boström, M.; Nordström, E.; Persson, C.; Sahlqvist, L.; Starrin, B.; Ydreborg, B. Mental Health Symptoms in Relation to Socio-Economic Conditions and Lifestyle Factors a Population-Based Study in Sweden. BMC Public Health 2009, 9, 302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esch, P.; Bocquet, V.; Pull, C.; Couffignal, S.; Lehnert, T.; Graas, M.; Fond-Harmant, L.; Ansseau, M. The Downward Spiral of Mental Disorders and Educational Attainment: A Systematic Review on Early School Leaving. BMC Psychiatry 2014, 14, 237. [Google Scholar] [CrossRef] [Green Version]
- Borges, G.; Mora-Icaza, M.E.M.; Benjet, C.; Lee, S.; Lane, M.; Breslau, J. Influence of Mental Disorders on School Dropout in Mexico. Rev. Panam. De Salud Publica Pan Am. J. Public Health 2011, 30, 477–483. [Google Scholar] [CrossRef]
- Lee, S.; Tsang, A.; Breslau, J.; Aguilar-Gaxiola, S.; Angermeyer, M.; Borges, G.; Bromet, E.; Bruffaerts, R.; De Girolamo, G.; Fayyad, J.; et al. Mental Disorders and Termination of Education in High-Income and Low- and Middle-Income Countries: Epidemiological Study. Br. J. Psychiatry 2009, 194, 411–417. [Google Scholar] [CrossRef]
- Jung, A.K.; O’Brien, K.M. The Profound Influence of Unpaid Work on Women’s Lives: An Overview and Future Directions. J. Career Dev. 2019, 46, 184–200. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).