Characteristics of Sleep Paralysis and Its Association with Anxiety Symptoms, Perceived Stress, PTSD, and Other Variables Related to Lifestyle in Selected High Stress Exposed Professions
Abstract
:1. Introduction
Occupations Exposed to Stress and at an Increased Risk of SP
2. Measures and Methods
2.1. Participants and Procedure
- (1)
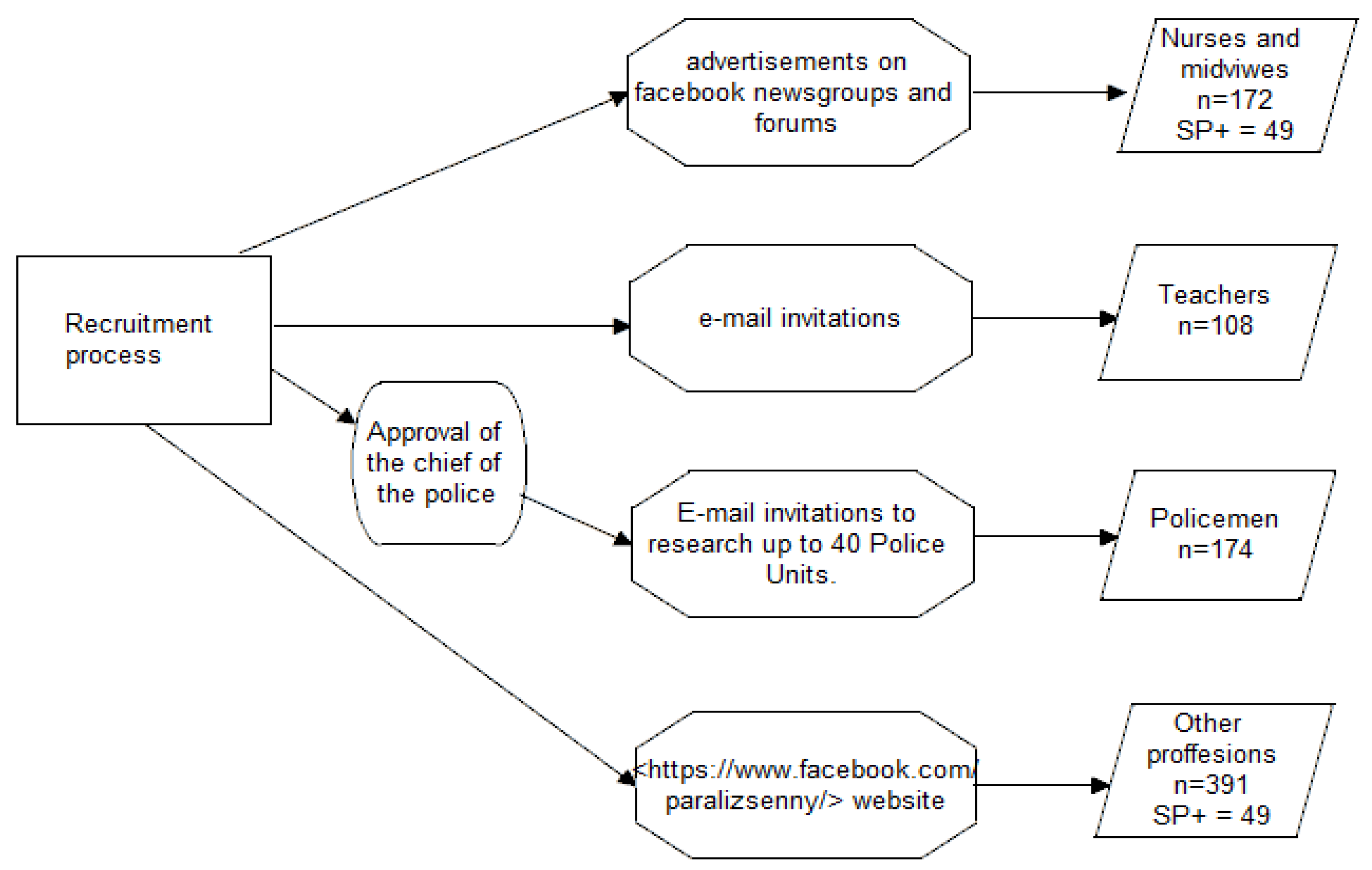
- Nurses and midwives: recruited through advertisements on newsgroups and forums pertaining to these professions more generally. The questionnaire was completed by 172 participants (170 women, 2 men).
- (2)
- Teachers: recruited via an e-mail invitational study sent to schools. The questionnaire was completed by 108 participants (98 women, 10 men).
- (3)
- Policemen: recruited after obtaining consent from the Commander of the Main Headquarters of Police. The research questionnaire was made available to police officers by email to 40 police units located all over Poland. Online research surveys were available by e-mail to policemen working in these units. The questionnaire was completed by 174 participants (49 women, 125 men).
- (4)
- “Other professions”: a battery of questionnaires was made available on the https://www.facebook.com/paralizsenny/website (access date: 21 April 2022) from March 2019 to November 2019. The questionnaire was completed by 391 participants (285 women, 106 men). A list of professions included in the group “other professions” is presented in Supplementary Table S1.
2.2. Measures
2.2.1. Sociodemographic and Health Status Questionnaire
- I.
- personal data, i.e., gender, age, height, weight, size of the city in which they live, profession, and working time (permanent/shift)
- II.
- lifestyle data, i.e., smoking (number of cigarettes smoked during the day and smoking time in years), the average number of hours of sleep during the night, alcohol consumption (type of alcohol and frequency of drinking), the number of cups of coffee or other caffeinated beverages consumed during the day, and physical activity (number of hours a week spent in physical activity).
- III.
- health data, i.e., the presence of chronic diseases (somatic and psychiatric) and medications taken.
2.2.2. Sleep Paralysis Experiences and Phenomenology Questionnaire
2.2.3. The PTSD Checklist (PCL-5)
2.2.4. The State-Trait Anxiety Inventory (STAI)
2.2.5. The Penn State Worry Questionnaire (PSWQ)
2.2.6. The Perceived Stress Scale (PSS-10)
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Group
3.1.1. The Demographic Characteristics, Lifestyle, and Health Status of the Study Participants
3.1.2. Differences between Professions in the Study Group (SP+ and SP−)
Age Differences
Differences in Body Mass Index (BMI)
Differences in Alcohol Consumption
Differences in Sleep Duration
Differences in Time Spent on Physical Activity
Differences in the results of self-written scales (STAI, PCL-5, PSWQ)
3.1.3. Differences between Professions in the Group of Participants Who Experienced at Least One Episode of SP (SP+)
Age Differences
Differences in Body Mass Index (BMI)
Differences in Sleep Duration
Differences in Time Spent on Physical Activity
3.2. Prevalence and Characteristics of SP
3.2.1. Lifetime and Period Prevalence of SP
3.2.2. Characteristics of SP Episodes
3.2.3. Symptomatology of SP
3.3. Relationship between SP and Anxiety Symptoms and Perceived Stress
3.3.1. The Association between Frequency of SP Episodes and Trait Anxiety Symptoms (STAI-T)
3.3.2. The Relationship between the Number of SP Symptoms Reported and Trait Anxiety Symptoms (STAI-T)
3.3.3. The Association between Frequency of SP Episodes and Severity of Symptoms of Post-Traumatic Stress Disorder (PTSD)
3.3.4. Relationship between the Number of SP Symptoms Reported and the Severity of Symptoms of Post-Traumatic Stress Disorder (PTSD)
3.3.5. SP and Tendency to Worry (PSWQ)
3.3.6. SP and Intensity of Perceived Stress (PSS-10)
3.4. Influence of Age, BMI, and Lifestyle Variables on the Frequency and Severity of SP Episodes
3.4.1. Nurses and Midwives
3.4.2. Teachers
3.4.3. Police Officers
3.4.4. “Other Professions”
4. Discussion
5. Conclusions
- The prevalence of SP in each of the researched professional groups was higher than in the general population.
- The lifetime prevalence of SP was the lowest among policemen (15.5%) and the highest in the group of “other professions” (39.4%).
- The course and frequency of SP episodes did not differ in individual professional groups.
- The severity of SP episodes differed between the occupational groups. Hallucination symptoms of SP as well as total symptoms of SP were both more frequently reported among the group of “other professions” as compared to the remaining groups studied.
- An association of SP with symptoms of PTSD and anxiety was confirmed in the group of nurses and “other professions”.
- In the policemen cohort, no relationship was found between SP and PTSD and the severity of anxiety symptoms.
- The frequency and severity of SP, depending on the occupational group, were associated with various lifestyle factors, which may indicate a complex etiology for this sleep disorder.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethics Approval
References
- Sharpless, B.A. A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatr. Dis. Treat. 2016, 12, 1761–1767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Sleep Medicine ICSD-3 Online Version—American Academy of Sleep Medicine (AASM) 2014. Available online: https://learn.aasm.org (accessed on 4 February 2022).
- Cheyne, J.A.; Rueffer, S.D.; Newby-Clark, I.R. Hypnagogic and Hypnopompic Hallucinations during Sleep Paralysis: Neurological and Cultural Construction of the Night-Mare. Conscious. Cogn. 1999, 8, 319–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharpless, B.A.; Kliková, M. Clinical features of isolated sleep paralysis. Sleep Med. 2019, 58, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Wróbel-Knybel, P.; Karakuła-Juchnowicz, H.; Flis, M.; Rog, J.; Hinton, D.E.; Boguta, P.; Jalal, B. Prevalence and clinical picture of sleep paralysis in a Polish student sample. Int. J. Environ. Res. Public Health 2020, 17, 3529. [Google Scholar] [CrossRef] [PubMed]
- Sharpless, B.A.; McCarthy, K.S.; Chambless, D.L.; Milrod, B.L.; Khalsa, S.R.; Barber, J.P. Isolated sleep paralysis and fearful isolated sleep paralysis in outpatients with panic attacksb. J. Clin. Psychol. 2010, 66, 1292–1306. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, C.A. Parasomnias. Dis. -A-Mon. 2011, 57, 364–388. [Google Scholar] [CrossRef]
- Walther, B.W.; Schulz, H. Recurrent Isolated Sleep Paralysis: Polysomnographic and Clinical Findings. Somnologie 2004, 8, 53–60. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 0890425558. [Google Scholar]
- Sharpless, B.A.; Barber, J.P. Lifetime prevalence rates of sleep paralysis: A systematic review. Sleep Med. Rev. 2011, 15, 311–315. [Google Scholar] [CrossRef] [Green Version]
- Wróbel-Knybel, P.; Rog, J.; Jalal, B.; Szewczyk, P.; Karakuła-Juchnowicz, H. Sleep paralysis among professional firefighters and a possible association with PTSD—Online survey-based study. Int. J. Environ. Res. Public Health 2021, 18, 9442. [Google Scholar] [CrossRef]
- Denis, D. Relationships between sleep paralysis and sleep quality: Current insights. Nat. Sci. Sleep 2018, 10, 355–367. [Google Scholar] [CrossRef] [Green Version]
- Denis, D.; French, C.C.; Rowe, R.; Zavos, H.M.S.; Nolan, P.M.; Parsons, M.J.; Gregory, A.M. A twin and molecular genetics study of sleep paralysis and associated factors. J. Sleep Res. 2015, 24, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Denis, D.; French, C.C.; Gregory, A.M. A systematic review of variables associated with sleep paralysis. Sleep Med. Rev. 2018, 38, 141–157. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M. Epidemiological Overview of sleep Disorders in the General Population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Kashani, M.; Eliasson, A.; Vernalis, M. Perceived stress correlates with disturbed sleep: A link connecting stress and cardiovascular disease. Stress 2012, 15, 45–51. [Google Scholar] [CrossRef]
- Rajaratnam, S.M.W.; Barger, L.K.; Lockley, S.W.; Shea, S.A.; Wang, W.; Landrigan, C.P.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Cade, B.E.; et al. Sleep disorders, health, and safety in police officers. JAMA 2011, 306, 2567–2578. [Google Scholar] [CrossRef] [Green Version]
- Carey, M.G.; Al-Zaiti, S.S.; Dean, G.E.; Sessanna, L.; Finnell, D.S. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J. Occup. Environ. Med. 2011, 53, 928–933. [Google Scholar] [CrossRef] [Green Version]
- Weaver, M.D.; Vetter, C.; Rajaratnam, S.M.W.; O’Brien, C.S.; Qadri, S.; Benca, R.M.; Rogers, A.E.; Leary, E.B.; Walsh, J.K.; Czeisler, C.A.; et al. Sleep disorders, depression and anxiety are associated with adverse safety outcomes in healthcare workers: A prospective cohort study. J. Sleep Res. 2018, 27, e12722. [Google Scholar] [CrossRef] [Green Version]
- Garbarino, S.; Guglielmi, O.; Puntoni, M.; Bragazzi, N.L.; Magnavita, N. Sleep quality among police officers: Implications and insights from a systematic review and meta-analysis of the literature. Int. J. Environ. Res. Public Health 2019, 16, 885. [Google Scholar] [CrossRef] [Green Version]
- Zdanowicz, T.; Turowski, K.; Celej-Szuster, J.; Lorencowicz, R.; Przychodzka, E. Insomnia, Sleepiness, and Fatigue Among Polish Nurses. Work. Health Saf. 2020, 68, 272–278. [Google Scholar] [CrossRef]
- Neylan, T.C.; Metzler, T.J.; Best, S.R.; Weiss, D.S.; Fagan, J.A.; Liberman, A.; Rogers, C.; Vedantham, K.; Brunet, A.; Lipsey, T.L.; et al. Critical incident exposure and sleep quality in police officers. Psychosom. Med. 2002, 64, 345–352. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Ruminations and occupational stress as predictors of post-traumatic stress disorder and burnout among police officers. Int. J. Occup. Saf. Ergon. 2021, 28, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; Carey, M.G.; Wagner, S.; Alden, L.E.; Buys, N.; Corneil, W.; Fyfe, T.; Matthews, L.; Randall, C.; White, M.; et al. A systematic review of mental health symptoms in police officers following extreme traumatic exposures. Police Pract. Res. 2021, 22, 225–239. [Google Scholar] [CrossRef]
- Stevelink, S.A.M.; Opie, E.; Pernet, D.; Gao, H.; Elliott, P.; Wessely, S.; Fear, N.T.; Hotopf, M.; Greenberg, N. Probable PTSD, depression and anxiety in 40,299 UK police officers and staff: Prevalence, risk factors and associations with blood pressure. PLoS ONE 2020, 15, e0240902. [Google Scholar] [CrossRef]
- Schuster, M.; Dwyer, P.A. Post-traumatic stress disorder in nurses: An integrative review. J. Clin. Nurs. 2020, 29, 2769–2787. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, S.; Lees, T.; Lal, S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int. J. Environ. Res. Public Health 2019, 16, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watson, R.; Gardiner, E.; Hogston, R.; Gibson, H.; Stimpson, A.; Wrate, R.; Deary, I. A longitudinal study of stress and psychological distress in nurses and nursing students. J. Clin. Nurs. 2009, 18, 270–278. [Google Scholar] [CrossRef]
- Do Valle, L.R.; Do Valle, C.R.; Valle, E.; Malvezzi, S.; Reimão, R. Stress and sleep disorders in teachers—A Brazilian study. Sleep Med. 2013, 14, e292. [Google Scholar] [CrossRef]
- Desouky, D.; Allam, H. Occupational stress, anxiety and depression among Egyptian teachers. J. Epidemiol. Glob. Health 2017, 7, 191–198. [Google Scholar] [CrossRef]
- McCarthy, C.J. Teacher stress: Balancing demands and resources. Phi Delta Kappan 2019, 101, 8–14. [Google Scholar] [CrossRef]
- Johnson, S.; Cooper, C.; Cartwright, S.; Donald, I.; Taylor, P.; Millet, C. The experience of work-related stress across occupations. J. Manag. Psychol. 2005, 20, 178–187. [Google Scholar] [CrossRef] [Green Version]
- Farmer, D. Teacher Attrition: The Impacts of Stress. Delta Kappa Gamma Bull. 2020, 87, 41–50. [Google Scholar]
- De Souza, J.C.; De Sousa, I.C.; Belísio, A.S.; de Azevedo, C.V.M. Sleep habits, daytime sleepiness and sleep quality of high school teachers. Psychol. Neurosci. 2012, 5, 257–263. [Google Scholar] [CrossRef] [Green Version]
- Mollart, L.; Skinner, V.M.; Newing, C.; Foureur, M. Factors that may influence midwives work-related stress and burnout. Women Birth 2013, 26, 26–32. [Google Scholar] [CrossRef]
- Booker, L.A.; Magee, M.; Rajaratnam, S.M.W.; Sletten, T.L.; Howard, M.E. Individual vulnerability to insomnia, excessive sleepiness and shift work disorder amongst healthcare shift workers. A systematic review. Sleep Med. Rev. 2018, 41, 220–233. [Google Scholar] [CrossRef]
- Jalal, B.; Hinton, D.E. Rates and Characteristics of Sleep Paralysis in the General Population of Denmark and Egypt. Cult. Med. Psychiatry 2013, 37, 534–548. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Herman, D.; Huska, J.; Keane, T. PTSD CheckList—Civilian Version (PCL-C); National Center for PTSD: White River Junction, VT, USA, 1994. [Google Scholar]
- Gaudry, E.; Vagg, P.; Spielberger, C.D. Validation of the state-trait distinction in anxiety research. Multivar. Behav. Res. 1975, 10, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.A.; Antony, M.M.; Barlow, D.H. Psychometric properties of the Penn state worry questionnaire in a clinical anxiety disorders sample. Behav. Res. Ther. 1992, 30, 33–37. [Google Scholar] [CrossRef]
- Roberti, J.W.; Harrington, L.N.; Storch, E.A. Further Psychometric Support for the 10-Item Version of the Perceived Stress Scale. J. Coll. Couns. 2006, 9, 135–147. [Google Scholar] [CrossRef]
- Jalal, B.; Romanelli, A.; Hinton, D.E. Sleep paralysis in Italy: Frequency, hallucinatory experiences, and other features. Transcult. Psychiatry 2020, 58, 427–439. [Google Scholar] [CrossRef]
- Jalal, B.; Sevde Eskici, H.; Acarturk, C.; Hinton, D.E. Beliefs about sleep paralysis in Turkey: Karabasan attack. Transcult. Psychiatry 2020, 58, 414–426. [Google Scholar] [CrossRef]
- Ogińska-Bulik, N.; Juczyński, Z.; Lis-Turlejska, M.-K.D. Polska adaptacja PTSD Check List for DSM-5—PCL-5. Doniesienie Wstępne 2018, 61, 281–285. [Google Scholar]
- Wrześniewski, K.; Sosnowski, T.; Jaworowska, A.; Fecenec, D. STAI—Inwentarz Stanu i Cechy Lęku. Polska Adaptacja STAI; Pracownia Testów Psychologicznych PTP: Warszawa, Poland, 2011. [Google Scholar]
- Meyer, T.J.; Miller, M.L.; Metzger, R.L.; Borkovec, T.D. Development and validation of the Penn State Janowski, K. Kwestionariusz Oceny Martwienia się, polska adaptacja PSWQ. Katedra Psychologii Kinane. Lublin: KUL. Behav. Res. Ther. 2007, 28, 487–495. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Skala Odczuwanego Stresu. “PSS-10.” Narzędzia Pomiaru Stresu i Radzenia Sobie ze Stresem; Pracownia Testów Psychologicznych: Warszawa, Poland, 2009; pp. 11–22. [Google Scholar]
- Ferguson, C.J. An Effect Size Primer: A Guide for Clinicians and Researchers. Prof. Psychol. Res. Pract. 2009, 40, 532–538. [Google Scholar] [CrossRef] [Green Version]
- Cheyne, J.A.; Waterloo Unusual Sleep Experiences Questionnaire –VIIIa Technical Report. Department of Psychology University of Waterloo May 2002. 2002. Available online: http://watarts.uwaterloo.ca/~acheyne/spquest01.html (accessed on 13 May 2016).
- Jalal, B. How to make the ghosts in my bedroom disappear? Focused-attention meditation combined with muscle relaxation (MR therapy)-a direct treatment intervention for Sleep Paralysis. Front. Psychol. 2016, 7, 28. [Google Scholar] [CrossRef] [Green Version]
- Soomro, S.; Yanos, P.T. Predictors of Mental Health Stigma among Police Officers: The Role of Trauma and PTSD. J. Police Crim. Psychol. 2019, 34, 175–183. [Google Scholar] [CrossRef]
- Costa, M.; Esteves, M. Cigarette Smoking and Sleep Disturbance. Addict. Disord. Their Treat. 2018, 17, 40–48. [Google Scholar] [CrossRef]
- Munezawa, T.; Kaneita, Y.; Osaki, Y.; Kanda, H.; Ohtsu, T.; Suzuki, H.; Minowa, M.; Suzuki, K.; Higuchi, S.; Mori, J.; et al. Nightmare and sleep paralysis among Japanese adolescents: A nationwide representative survey. Sleep Med. 2011, 12, 56–64. [Google Scholar] [CrossRef]
- Martindale, S.L.; Hurley, R.A.; Taber, K.H. Chronic alcohol use and sleep homeostasis: Risk factors and neuroimaging of recovery. J. Neuropsychiatry Clin. Neurosci. 2017, 29, A6-5. [Google Scholar] [CrossRef]
- Feige, B.; Gann, H.; Brueck, R.; Hornyak, M.; Litsch, S.; Hohagen, F.; Riemann, D. Effects of alcohol on polysomnographically recorded sleep in healthy subjects. Alcohol. Clin. Exp. Res. 2006, 30, 1527–1537. [Google Scholar] [CrossRef]
- Alkerwi, A.; Boutsen, M.; Vaillant, M.; Barre, J.; Lair, M.L.; Albert, A.; Guillaume, M.; Dramaix, M. Alcohol consumption and the prevalence of metabolic syndrome: A meta-analysis of observational studies. Atherosclerosis 2009, 204, 624–635. [Google Scholar] [CrossRef]
- Venkataraman, R.; Satish Kumar, B.P.; Kumaraswamy, M.; Singh, R.; Pandey, M.; Tripathi, P.; Sharath, V.; George, J.V.; Dahal, P. Smoking, alcohol and hypertension. Int. J. Pharm. Pharm. Sci. 2013, 5, 28–32. [Google Scholar]
- Kwon, Y.; Norby, F.L.; Jensen, P.N.; Agarwal, S.K.; Soliman, E.Z.; Lip, G.Y.H.; Longstreth, W.T.; Alonso, A.; Heckbert, S.R.; Chen, L.Y. Association of smoking, alcohol, and obesity with cardiovascular death and ischemic stroke in atrial fibrillation: The Atherosclerosis Risk in Communities (ARIC) study and Cardiovascular Health Study (CHS). PLoS ONE 2016, 11, e0147065. [Google Scholar] [CrossRef] [PubMed]
- Booker, L.A.; Sletten, T.L.; Alvaro, P.K.; Barnes, M.; Collins, A.; Chai-Coetzer, C.L.; Naqvi, A.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M.W.; et al. Exploring the associations between shift work disorder, depression, anxiety and sick leave taken amongst nurses. J. Sleep Res. 2020, 29, e12872. [Google Scholar] [CrossRef] [PubMed]
- Jalal, B.; Hinton, D.E. Sleep paralysis among egyptian college students: Association with anxiety symptoms (PTSD, trait anxiety, pathological worry). J. Nerv. Ment. Dis. 2015, 203, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Horváth, A.; Montana, X.; Lanquart, J.P.; Hubain, P.; Szűcs, A.; Linkowski, P.; Loas, G. Effects of state and trait anxiety on sleep structure: A polysomnographic study in 1083 subjects. Psychiatry Res. 2016, 244, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.C.; Shakoor, B.; Thompson, B.; Dew, D.; Hughley, E.; Mays, R.; Shorter-Gooden, K. Prevalence of isolated sleep paralysis in black subjects. J. Natl. Med. Assoc. 1984, 76, 501–508. [Google Scholar]
- Ikhlaq, A. Association of Sleep Paralysis with PTSD Symptoms, Pathological Worry and Perceived Stress. Int. J. Pulm. Respir. Sci. 2021, 4, 96–99. [Google Scholar] [CrossRef]
- Denis, D.; Poerio, G.L. Terror and bliss? Commonalities and distinctions between sleep paralysis, lucid dreaming, and their associations with waking life experiences. J. Sleep Res. 2017, 26, 38–47. [Google Scholar] [CrossRef]
- McNally, R.J.; Clancy, S.A. Sleep paralysis in adults reporting repressed, recovered, or continuous memories of childhood sexual abuse. J. Anxiety Disord. 2005, 595–602. [Google Scholar] [CrossRef]
- Hinton, D.E.; Pich, V.; Chhean, D.; Pollack, M.H.; McNally, R.J. Sleep paralysis among Cambodian refugees: Association with PTSD diagnosis and severity. Depress. Anxiety 2005, 22, 47–51. [Google Scholar] [CrossRef]
- Fulda, S.; Schulz, H. Cognitive dysfunction in sleep disorders. Sleep Med. Rev. 2001, 5, 423–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheyne, J.A.; Pennycook, G. Sleep paralysis postepisode distress: Modeling potential effects of episode characteristics, general psychological distress, beliefs, and cognitive style. Clin. Psychol. Sci. 2013, 1, 135–148. [Google Scholar] [CrossRef]
- Betscher, E.; Guenter, W.; Langdon, D.W.; Bonek, R. Polish validation of the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS battery): Correlation of cognitive impairment with mood disorders and fatigue. Neurol. Neurochir. Pol. 2021, 55, 59–66. [Google Scholar] [CrossRef] [PubMed]
| Professions: | Nurses and Midwives | Teachers | Policemen | Other Professions | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Type: | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− |
| % (n) | 100 (172) | 27.91 (48) | 72.09 (124) | 100 (107) | 26.17 (28) | 73.83 (79) | 100 (174) | 15.52 (27) | 84.48 (147) | 100 (391) | 39.39 (154) | 60.61 (237) |
| % Female (n) | 98.84 (170) | 100 (48) | 98.39 (122) | 90.65 (97) | 89.29 (25) | 91.14 (72) | 28.16 (49) | 18.52 (5) | 29.93 (44) | 72.89 (285) | 70.13 (108) | 74.68 (177) |
| % Male (n) | 1.16 (2) | 0 (0) | 1.61 (2) | 9.35 (10) | 0 (0) | 8.86 (7) | 71.84 (125) | 81.48 (22.0) | 70.07 (103) | 27.11 (106) | 29.87 (46) | 25.32 (60) |
| Age | ||||||||||||
| M (RNG) | 37.14 (21–63) | 34.04 (21–55) | 38.33 (22–63) | 39.26 (21–62) | 36.36 (23–55) | 40.29 (21–62) | 40.91 (26–59) | 39.63 (30–53) | 41.14 (26–59) | 32.29 (18–67) | 29.34 (18–60) | 34.21 (18–67) |
| Me (Range) | 36 (42) | 30.5 (34) | 39 (41) | 39 (41) | 36.5 (32) | 40 (41) | 40 (33) | 39 (23) | 41 (33) | 29 (49) | 27.5 (42) | 32 (49) |
| % Place of residence (n): | ||||||||||||
| City up to 50, 000 inhabitants | 19.19 (33) | 16.67 (8) | 20.16 (25) | 26.17 (28) | 25.0 (7) | 26.58 (21) | 28.16 (49) | 37.04 (10) | 26.53 (39) | 19.18 (75) | 18.83 (29) | 19.41 (46) |
| City 50,000–100,000 inhabitants | 13.95 (24) | 12.5 (6) | 14.52 (18) | 11.21 (12) | 3.57 (1) | 13.92 (11) | 17.24 (30) | 29.63 (8) | 14.97 (22) | 13.55 (53) | 12.33 (19) | 14.35 (34) |
| City more than 100,00 inhabitants | 46.51 (80) | 51.16 (26) | 43.55 (54) | 37.38 (40) | 35.71 (10) | 37.97 (30) | 37.36 (65) | 25.93 (7) | 39.46 (58) | 42.27 (177) | 52.60 (81) | 40.51 (96) |
| % Village | 20.35 (35) | 16.56 (8) | 21.77 (27) | 25.23 (27) | 35.71 (10) | 21.52 (17) | 17.24 (30) | 7.41 (2) | 19.05 (28) | 21.99 (86) | 16.23 (19) | 25.74 (61) |
| % Type of work (n): | ||||||||||||
| -Shift work | 81.98 (141) | 85.42 (41) | 80.65 (100) | 7.48 (8) | 10.71 (3) | 6.33 (5) | 58.05 (101) | 62.96 (17) | 57.14 (84) | 24.04 (94) | 24.68 (38) | 23.63 (56) |
| -Constant work time | 18.02 (31) | 14.58 (7) | 19.35 (24) | 92.52 (99) | 89.29 (25) | 93.67 | 41.95 (73) | 37.04 (10) | 42.86 (63) | 75.96 (297) | 75.32 (116) | 181 (76.37) |
| Professions: | Nurses and Midwives | Teachers | Policemen | Other Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Type: | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | |
| BMI [kg/m2] | M (RNG) | 25.37 (17.01–41.52) | 24.11 (17.00–40.01) | 25.86 (17.26–41.52) | 25.11 (17.47–44.44) | 25.52 (17.65–44.44) | 24.96 (17.47–42.24) | 27.15 (17.57–40.04) | 27.66 (21.72–35.51) | 27.13 (17.57–40.04) | 24.73 (15.43–43.16) | 24.04 (15.43–51.81) | 25.18 (16.81–58.59) |
| Me (Range) | 24.29 (24.52) | 23.05 (23.05) | 24.67 (24.26) | 24 (26.97) | 23.56 (26.8) | 24.17 (24.76) | 26.59 (22.47) | 26.67 (13.79) | 26.59 (22.47) | 23.46 (43.16) | 23.04 (36.38) | 23.94 (41.79) | |
| % Psychiatric Disorder (n) | 4.07 (7) | 4.17 (2) | 4.03 (5) | 2.8 (3) | 0 | 3.80 (3) | 4.60 (8) | 7.41 (2) | 4.08 (6) | 7.42 (29) | 9.09 (14) | 6.33 (15) | |
| % Somatic disorder (n) | 45.35 (78) | 62.5 (18) | 48.39 (60) | 35.51 (38) | 39.29 (11) | 34.18 (27) | 26.44 (46) | 37.04 (10) | 24.49 (36) | 27.11 (106) | 24.68 (38) | 28.69 (68) | |
| % Medicines taken (n) | 43.02 (74) | 37.5 (18) | 45.16 (56) | 31.78 (34) | 25 (7) | 34.18 (27) | 23.56 (41) | 29.63 (8) | 22.45 (33) | 25.06 (98) | 22.08 (34) | 27.0 (64) | |
| Professions: | Nurses and Midwives | Teachers | Policemen | Other Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Type: | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | |
| Number of cigarettes smoked per day | M (RNG) | 2.87 (0–20) | 3.06 (0–20) | 2.79 (0–20) | 1.13 (0–20) | 1.18 (0–12) | 1.11 (0–20) | 2.97 (0–40) | 3.70 (0–40) | 2.83 (0–40) | 2.48 (0–40) | 2.74 (0–20) | 2.31 (0–40) |
| Me (Range) | 0 (20) | 0 (20) | 0 (20) | 0 (20) | 0 (12) | 0 (20) | 9 (40) | 0 (40) | 0 (40) | 0 (40) | 0 (20) | 0 (40) | |
| Time of cigarette smoking in years | M (RNG) | 4.4 (0–40) | 4.56 (0–35) | 4.34 (0–40) | 2.02 (0–40) | 2.68 (0–28) | 1.78 (0–40) | 3.67 (0–35) | 3.63 (0–30) | 3.68 (0–35) | 2.64 (0–37) | 2.55 (0–28) | 2.70 (0–37) |
| Me (Range) | 0 (40) | 0 (35) | 0 (40) | 0 (40) | 0 (28) | 0 (40) | 0 (35) | 0 (30) | 0 (35) | 0 (37) | 0 (28) | 0 (37) | |
| Number of caffe cup per day | M (RNG) | 2.01 (0–8) | 1.73 (0–5) | 2.12 (0–8) | 1.84 (0–5.5) | 1.68 (0–5) | 1.89 (0–5.5) | 1.98 (0–14) | 1.2 (0–3) | 2.13 (0–14) | 1.55 (0–12) | 1.48 (0–8) | 1.59 (0–12) |
| Me (Range) | 2 (8) | 1.5 (5) | 2 (20) | 2 (5.5) | 1.3 (5) | 2 (5.5) | 2 (14) | 1 (3) | 2 (14) | 1 (12) | 1 (8) | 1.5(12) | |
| Number caffeinated beverages per day | M (RNG) | 0.17 (0–3.5) | 0.08 (0–1) | 0.21 (0–3.5) | 0.19 (0–4) | 0.19 (0–2) | 0.18 (0–4) | 0.22 (0–10) | 0.31 (0–2.5) | 0.2 (0–10) | 0.28 (0–5) | 0.38 (0–5) | 0.22 (0–5) |
| Me (Range) | 0 (3.5) | 0 (1) | 0 (3.5) | 0 (4) | 0 (2) | 0 (4) | 0 (10) | 0 (2.5) | 0 (10) | 0 (5) | 0 (5) | 0 (5) | |
| The frequency of alcohol consumption per month | M (RNG) | 1.22 (0–4) | 1.35 (0–4) | 1.16 (0–4) | 0.55 (0–1) | 1.32 (0–4) | 0.65 (0–5) | 2 (0–5) | 2 (0–4.0) | 2 (0–5) | 1.58 (0–5) | 1.73 (0–5) | 1.49 (0–5) |
| Me (Range) | 1 (4) | 0 (4) | 0 (4) | 1 (1) | 0.5 (4) | 0 (5) | 2 (5) | 2 (4) | 2 (5) | 2 (5) | 2 (0–5) | 2 (5) | |
| Average sleep duration per day (h) | M (RNG) | 6.73 (5–11) | 7.06 (5–10) | 6.6 (5–11) | 6.95 (5–9) | 6.75 (5–8) | 7.03 (5–9) | 6.6 (4–9) | 6.15 (4–8) | 6.68 (4–9) | 7.15 (3–12) | 7.27 (4–12) | 7.08 (3–12) |
| Me (Range) | 7 (6) | 7 (5) | 6.5 (6) | 7 (4) | 7 (3) | 7 (4) | 7 (5) | 6 (4) | 7 (5) | 7 (9) | 7 (8) | 7 (9) | |
| % Satisfaction with the quality of sleep (n) | 22.67 (39) | 31.25 (15) | 19.35 (24) | 45.79 (49) | 28.57 (8) | 51.90 (41) | 38.5 (67) | 22.22 (6) | 41.50 (61) | 44.76 (175) | 49.35 (76) | 41.77 (99) | |
| % The custom of taking naps during the day (n) | 48.84 (84) | 47.92 (23) | 49.19 (61) | 46.73 (50) | 53.57 (15) | 44.30 (35) | 37.93 (66) | 44.40 (12) | 36.73 (54) | 36.83 (144) | 41.56 (64) | 33.76 (80) | |
| number of hours of physical activity per week | M (RNG) | 0.73 (0–8) | 0.9 (0–5) | 0.67 (0–8) | 0.79 (0–8) | 1.21 (0–8) | 0.65 (0–5) | 2.03 (0–10) | 2.52 (0–8) | 1.95 (0–10) | 1.51 (0–10) | 1.51 (0–10) | 1.51 (0–10) |
| Me (Range) | 0 (8) | 0 (5) | 0 (8) | 10 (8) | 0 (8) | 0 (5) | 1 (10) | 3 (8) | 1 (10) | 0 (10) | 0 (10) | 0 (10) | |
| Professions: | Nurses and Midwives | Teachers | Policemen | Other Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Type: | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | Total | SP+ | SP− | |
| The number of points in self-report scales Me (Range): | STAI-T | 48 (52) | 45 (41) | 48 (52) | 48(38) | 52 (34) | 46 (38) | 42 (48) | 46 (44) | 41 (43) | 45 (52) | 45.5 (51) | 45 (51) |
| PCL-5 | 30 (80) | 25 (80) | 31 (80) | 28 (66) | 28 (66) | 28 (63) | 24.5 (78) | 23 (52) | 25 (78) | 23 (71) | 21.0 (71) | 23 (71) | |
| PSWQ | 57 (64) | 52 (56) | 57 (64) | 60 ((56) | 61.5 (44) | 59 (55) | 46.5 (64) | 51 (57) | 46 (64) | 53 (63) | 55 (58) | 53 (63) | |
| PSS-10 | 21 (36) | 20 (31) | 21 (36) | 21(31) | 24 (28) | 20 (28) | 19 (36) | 17 (33) | 19 (36) | 20 (38) | 20 (37) | 19 (37) | |
| Sample Type | SP+ Nurses and Midwives | SP+ Teachers | SP+ Policemen | SP+ Other Professions | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Me | M | Range | Me | M | Range | Me | M | Range | Me | M | Range | |
| Duration of SP episodes (min): | 3 | 5.49 | 99 | 3 | 4.25 | 14 | 1 | 2.78 | 9 | 2.5 | 5.23 | 60 |
| Frequency of SP episodes: | ||||||||||||
| -in the last month: | 0 | 0.65 | 10 | 1 | 1.79 | 18 | 0 | 1.04 | 10 | 0 | 0.99 | 12 |
| -in the last year: | 1 | 5.06 | 80 | 3 | 4.64 | 50 | 2 | 8.74 | 100 | 1 | 7.55 | 150 |
| -throughout the life: | 6 | 28.80 | 499 | 11.5 | 76 | 999 | 12 | 32.73 | 299 | 6 | 87.14 | 6999 |
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |||||
| Time of Occurrence of SP episodes: | ||||||||||||
| -upon falling asleep | 15 | 31.25 (17.6-44.9) | 13 | 46.43 (26.7-66.1) | 11 | 40.74 (20.9-60.5) | 59 | 38.31 (30.6-46.1) | ||||
| -upon awakening | 22 | 44.90 (31.2-60.5) | 9 | 32.14 (13.7-50.6) | 9 | 33.33 (14.3-52.3) | 68 27 | 44.15 (36.2-52.1) | ||||
| -both | 12 | 24.49 (10.6-35.3) | 6 | 21.43 (5.2-37.6) | 7 | 25.93 (8.3-43.6) | 17.53 (11.5-23.6) | |||||
| Body position during SP episodes: | ||||||||||||
| -on back | 33 | 67.35 (55.1–82.3) | 19 | 67.86 (49.4–86.3) | 12 | 44.44 (24.4–64.5) | 79 | 51.30 (43.3–59.3) | ||||
| -on stomach | 2 | 4.08 (−1.7–10) | 1 | 3.57 (−3.8–10.9) | 2 | 7.40 (−3.2–18) | 9 | 5.84 (2.1–9.6) | ||||
| -sleep position makes no difference | 14 | 28.57 (14.0–40.1) | 8 | 28.57 (10.7–46.4) | 13 | 48.15 (28–68.3) | 66 | 42.86 (35–50.1) | ||||
| Sample Type | SP+ Nurses and Midwives | SP+ Teachers | SP+ Policemen | SP+ Other Professions | ||||
|---|---|---|---|---|---|---|---|---|
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |
| At least one symptom | 47 | 97.92 (93.7–102.4) | 25 | 89.29 (77.1–101.1) | 23 | 85.19 (70.7–99.5) | 146 | 94.81 (91.3–98.3) |
| Pressure on chest | 31 | 64.58 (50.6–78.6) | 12 | 42.86 (23.3–62.4) | 10 | 37.04 (17.6–56.5) | 77 | 50 (42.0–57.9) |
| Unable to breathe | 23 | 47.92 (33.3–62.6) | 8 | 28.57 (10.7–46.4) | 9 | 33.33 (14.3–52.3) | 67 | 43.51 (35.6–51.4) |
| Chest pain/discomfort | 19 | 39.58 (25.2–53.9) | 9 | 32.14 (13.7–50.6) | 7 | 25.93 (8.3–43.6) | 54 | 35.06 (27.4–42.7) |
| Feeling of choking | 7 | 14.58 (4.2–24.9) | 4 | 14.29 (0.4–18.5–28.1) | 1 | 3.70 (−3.9–11.3) | 9 | 5.84 (2.1–9.6) |
| Nausea, abdominal distress | 1 | 2.08 (−2.1–6.3) | 0 | 0 | 1 | 3.70 (−3.9–11.3) | 5 | 3.25 (0.4–6.1) |
| Feeling dizzy, unsteady | 18 | 37.50 (23.3–51.7) | 3 | 10.71 (−1.5–22.9) | 5 | 18.52 (2.9–34.2) | 35 | 22.73 (16.0–29.4) |
| Sweating | 24 | 50.0 (35.3–64.7) | 10 | 35.71 (16.8–54.6)) | 15 | 55.56 (35.5–75.6) | 77 | 50 (42.0–58.0) |
| Trembling/shaking | 19 | 39.58 (25.2–53.9) | 10 | 35.71 (16.8–54.6) | 7 | 25.93 (8.3–43.6) | 55 | 35.71 (28.1–43.4) |
| Heart palpitations | 40 | 83.33 (72.4–94.3) | 20 | 71.43 (53.6–89.3) | 15 | 55.56 (35,5–75.6) | 107 | 69.48 (62.1–76.8) |
| Chills or hot flushes | 15 | 31.25 (17.6–44.9) | 8 | 28.57 (10.7–46.4) | 9 | 33.33 (14.3–52.3) | 50 | 32.47 (24.9–39.9) |
| Numbness/tingling | 30 | 62.50 (48.3–76.7) | 18 | 64.29 (45.4–83.2) | 11 | 40.74 (20.9–60.5) | 87 | 56.49 (48.6–64.4) |
| The feeling of body spinning | 10 | 20.83 (8.9–32.7) | 2 | 7.14 (−3.0–17.3) | 5 | 18.52 (2.9–34.2) | 42 | 27.27 (20.2–34.4) |
| Sample Type: | SP+ Nurses and Midwives | SP+ Teachers | SP+ Policemen | SP+ Other Professions | ||||
|---|---|---|---|---|---|---|---|---|
| Type of Hallucinations: | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) |
| Visual | 17 | 35.42 (21.4–49.5) | 8 | 28.57 (10.7–46.4) | 9 | 33.33 (14.3–52.3) | 76 | 49.35 (41.4–57.3) |
| Auditory | 13 | 27.08 (14–40.1) | 6 | 21.43 (5.2–37.6) | 7 | 25.93 (8.3–43.6) | 55 | 35.71 (28.1–43.4) |
| Tactile | 11 | 22.92 (10.6–35.3) | 51 | 35 (20.6–42.9) | 51 | 35 (0.5–29.1) | 51 | 35 (12.6–25.1) |
| Olfactory | 0 | 0 | 1 | 3.57 (−3.8−10.9) | 1 | 3.7 (−3.9–11.3)) | 2 | 1.30 (−0.5−3.1) |
| Intruder | 17 | 35.42 (21.4–49.5) | 10 | 35.71 (16.8−54.6) | 10 | 37.04 (17.6–56.5) | 79 | 51.30 (43.3–59.3) |
| Incubus | 6 | 12.50 (2.8–22.2) | 0 | 0 | 3 | 11.11 (−1.6–23.8) | 19 | 12.34 (7.1–17.6)) |
| Vestibular-motor: | 15 | 31.25 (17.6–44.6) | 3 | 10.71 (−1.5–22.9) | 7 | 25.93 (8.3–43.6) | 56 | 36.36 (28.7–44) |
| -Feeling of body spinning/flying | 10 | 20.83 (8.9–32.7) | 2 | 7.14 (−3–17.3) | 5 | 18.52 (2.9–34.2) | 42 | 22.27 (20.2–34.4) |
| -Autoscopy | 6 | 12.50 (2.8–22.2) | 2 | 7.14 (−3–17.3) | 4 | 14.81 (0.5–29.1) | 18 | 11.69 (6.6–16.8) |
| -OBE | 6 | 12.50 (2.8–22.2) | 3 | 10.71 (−1.5–22.9) | 3 | 11.11 (−1.6–23.8) | 29 | 18.83 (12.6–25.1) |
| Derealization | 7 | 14.58 (4.2–24.9) | 2 | 7.14 (−3–17.3) | 5 | 18.52 (2.9–34.2) | 29 | 18.83 (12.6–25.1) |
| depersonalization | 6 | 12.5 (2.8–22.2) | 1 | 3.57 (−3.8–10.9) | 3 | 11.11 (−1.6–23.8) | 22 | 14.29 (8.7–19.9) |
| Fear | 47 | 97.92 (93.7–102.1) | 26 | 92.86 (82.7–103) | 24 | 88.89 (76.2–101.6) | 146 | 94.81 (91.3–98.3) |
| Fear of death | 27 | 56.3 (41.7–70.8) | 15 | 53.57 (33.9–73.3) | 12 | 44.44 (24.4–64.5) | 86 | 55.84 (47.9–63.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wróbel-Knybel, P.; Flis, M.; Rog, J.; Jalal, B.; Wołkowski, L.; Karakuła-Juchnowicz, H. Characteristics of Sleep Paralysis and Its Association with Anxiety Symptoms, Perceived Stress, PTSD, and Other Variables Related to Lifestyle in Selected High Stress Exposed Professions. Int. J. Environ. Res. Public Health 2022, 19, 7821. https://doi.org/10.3390/ijerph19137821
Wróbel-Knybel P, Flis M, Rog J, Jalal B, Wołkowski L, Karakuła-Juchnowicz H. Characteristics of Sleep Paralysis and Its Association with Anxiety Symptoms, Perceived Stress, PTSD, and Other Variables Related to Lifestyle in Selected High Stress Exposed Professions. International Journal of Environmental Research and Public Health. 2022; 19(13):7821. https://doi.org/10.3390/ijerph19137821
Chicago/Turabian StyleWróbel-Knybel, Paulina, Michał Flis, Joanna Rog, Baland Jalal, Leszek Wołkowski, and Hanna Karakuła-Juchnowicz. 2022. "Characteristics of Sleep Paralysis and Its Association with Anxiety Symptoms, Perceived Stress, PTSD, and Other Variables Related to Lifestyle in Selected High Stress Exposed Professions" International Journal of Environmental Research and Public Health 19, no. 13: 7821. https://doi.org/10.3390/ijerph19137821
APA StyleWróbel-Knybel, P., Flis, M., Rog, J., Jalal, B., Wołkowski, L., & Karakuła-Juchnowicz, H. (2022). Characteristics of Sleep Paralysis and Its Association with Anxiety Symptoms, Perceived Stress, PTSD, and Other Variables Related to Lifestyle in Selected High Stress Exposed Professions. International Journal of Environmental Research and Public Health, 19(13), 7821. https://doi.org/10.3390/ijerph19137821








