Relationship between Oral Health Knowledge and Maternal Oral Health with Obstetric Risk and Breastfeeding
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Description
2.2. Statistical Analysis
2.3. Ethical Aspects
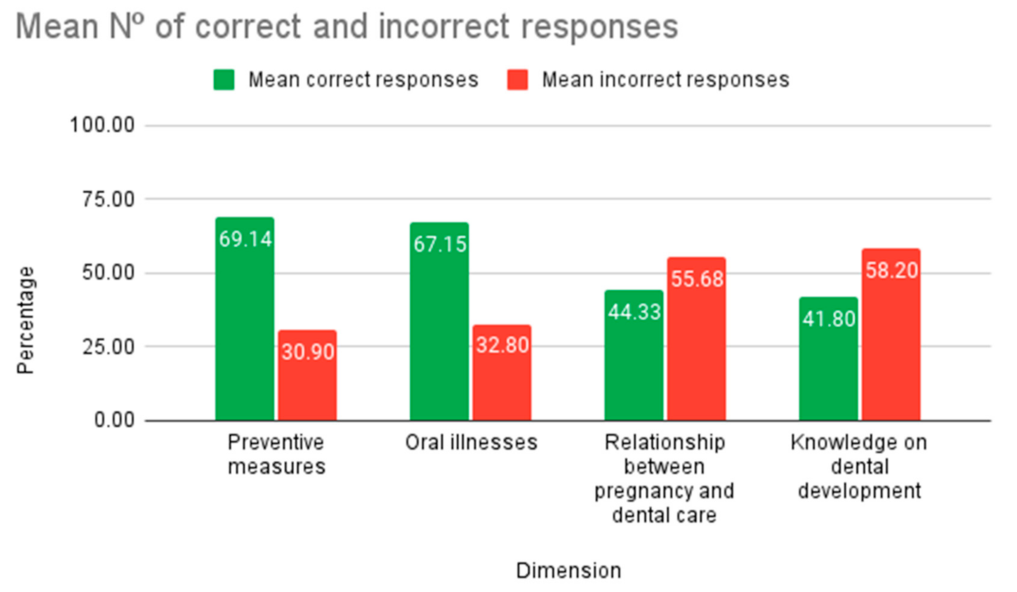
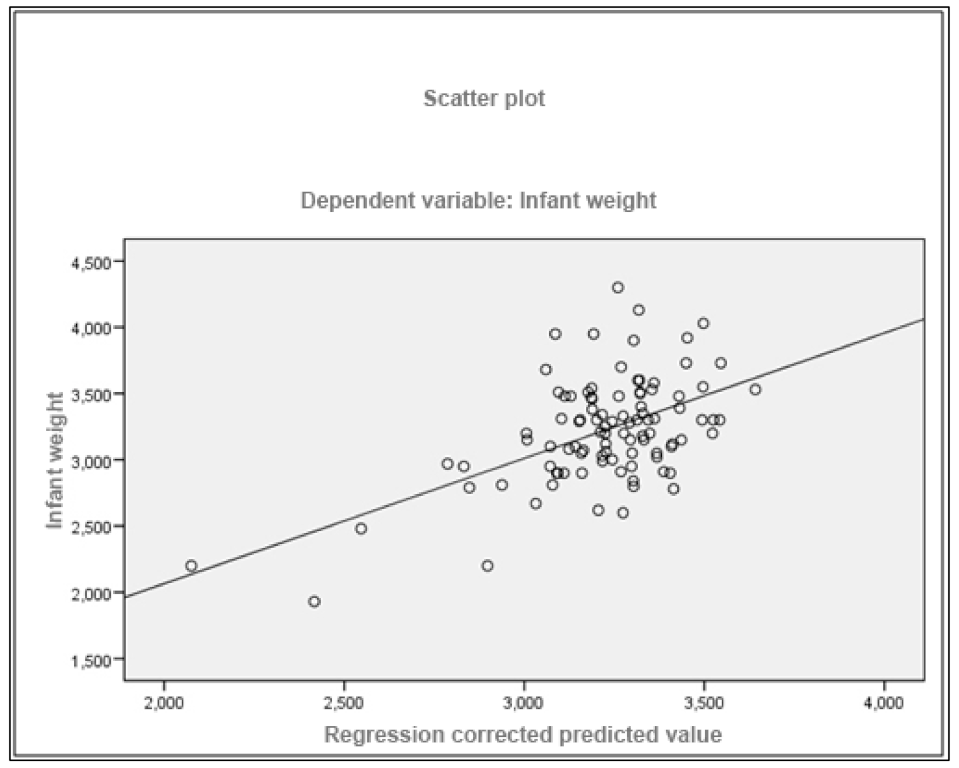
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviations | Significance |
| CAOD | Caries Index |
| CEIC | Clinical Research Ethics Committee |
| CI-S | Simplified Calculus Index |
| DI-S | Simplified Debris Index |
| DW | Durbin–Watson |
| ICU | Intensive Care Unit |
| IHOS | Simplified Oral Hygiene Index |
| IVF | Inflation Variance Factor |
| SESCAM | Health Service of Castilla La Mancha |
| WHO | World Health Organization |
References
- Lamster, I.B.; DePaola, D.P.; Oppermann, R.V.; Papapanou, P.N.; Wilder, R.S. The relationship of periodontal disease to diseases and disorders at distant sites: Communication to health care professionals and patients. J. Am. Dent. Assoc. 2008, 139, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- De Pablo, P.; Chapple, I.L.; Buckley, C.D.; Dietrich, T. Periodontitis in systemic rheumatic diseases. Nat. Rev. Rheumatol. 2009, 5, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, F.B.; Saito, M.T.; Matheus, F.C.; Prediger, R.D.; Yamada, E.S.; Maia, C.S.F.; Lima, R.R. Periodontitis and Alzheimer’s disease: A possible comorbidity between oral chronic inflammatory condition and neuroinflammation. Front. Aging Neurosci. 2017, 10, 327. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, G.; Costi, T.; Alkhamis, N.; Bagattoni, S.; Sadotti, A.; Piana, G. Oral health status in Alzheimer’s disease patients: A descriptive study in an Italian population. J. Contemp. Dent. Pract. 2018, 19, 483–489. [Google Scholar] [CrossRef]
- Michaud, D.S.; Fu, Z.; Shi, J.; Chung, M. Periodontal disease, tooth loss, and cancer risk. Epidemiol. Rev. 2017, 39, 49–58. [Google Scholar] [CrossRef]
- Herrera, D.; Serrano, J.; Roldán, S.; Sanz, M. Is the oral cavity relevant in SARS-CoV-2 pandemic? Clin. Oral. Investig. 2020, 24, 2925–2930. [Google Scholar] [CrossRef]
- Tada, A.; Senpuku, H. The impact of oral health on respiratory viral infection. Dent. J. 2021, 9, 43. [Google Scholar] [CrossRef]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef]
- Figuero-Ruiz, E.; Prieto Prieto, I.; Bascones-Martínez, A. Cambios hormonales asociados al embarazo: Compromiso gingival-periodontal. Av. Perio. Implant. Oral. 2006, 18, 101–113. [Google Scholar]
- Puertas, A.; Magan-Fernandez, A.; Blanc, V.; Revelles, L.; O’Valle, F.; Pozo, E.; León, R.; Mesa, F. Association of periodontitis with preterm birth and low birth weight: A comprehensive review. J. Matern. Fetal Neonatal. Med. 2018, 31, 597–602. [Google Scholar] [CrossRef]
- Carranza, F.N. Periodontología clínica de carranza. In Carranza, Periodontología Clínica de Carranza; Mac Graw-Hill Interamericana: New York, NY, USA, 1998; Chapter 5; p. 73. [Google Scholar]
- Palma, C.; Cahuana, A. Pautas para la salud bucal en los primeros años de vida. Odontol. Pediatr. 2010, 9, 179–189. [Google Scholar] [CrossRef]
- Pirie, M.; Cooke, I.; Linden, G.; Irwin, C. Dental manifestations of pregnancy. Obstet. Gynaecol. 2007, 9, 21–26. [Google Scholar] [CrossRef]
- Guggenheimer, J.; Moore, P.A. Xerostomia: Etiology, recognition and treatment. J. Am. Dent. Assoc. 2003, 134, 61–69. [Google Scholar] [CrossRef]
- Armitage, G.C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef]
- Panadés Alsina, L.; Calvo, X. La importancia de un buen consejo de salud bucodental durante el embarazo. Matronas Profesión. 2014, 15, 73–74. [Google Scholar]
- Bravo-Pérez, M.; Casals-Peidró, E.; Cortés-Martinicorena, F.J.; Llodra-Calvo, J.C.; Álvarez-Arenas Pardina, I.; Hermo-Señariz, P. Encuesta de salud oral en España 2005. RCOE 2006, 11, 409–456. [Google Scholar]
- Polyzos, N.P.; Polyzos, I.P.; Zavos, A.; Valachis, A.; Mauri, D.; Papanikolaou, E.G.; Tzioras, S.; Weber, D.; Messinis, I.E. Obstetric outcomes after treatment of periodontal disease during pregnancy: Systematic review and meta-analysis. BMJ 2010, 29, 341. [Google Scholar] [CrossRef]
- Lorenzo-Pouso, A.I.; Pérez-Sayáns, M.; González-Palanca, S. Relación entre la salud gingival en las gestantes con complicaciones obstétricas. Aten. Prim. 2017, 49, 621–622. [Google Scholar] [CrossRef]
- Romero, R.; Gómez, R.; Chaiworapongsa, T.; Conoscenti, G.; Kim, J.C.; Kim, Y.M. The role of infection in preterm labour and delivery. Paediatr. Perinat. Epidemiol. 2001, 15 (Suppl. 2), 41–56. [Google Scholar] [CrossRef]
- Flores, J.; Oteo, A.; Mateos, L.; Bascones, A. Relación entre enfermedad periodontal y parto prematuro. Bajo peso al nacimiento: Una revisión de la literatura. Av. Periodoncia Implantol. Oral 2004, 16, 93–105. [Google Scholar] [CrossRef]
- Blanco Carrión, J.F.; Gaceta Dental. La Periodontitis en Embarazadas Aumenta el Riesgo de Sufrir un Parto Prematuro. 25 de Noviembre de 2009. Available online: https://gacetadental.com/2009/11/la-periodontitis-en-embarazadas-aumenta-el-riesgo-de-sufrir-un-parto-prematuro-29632/ (accessed on 1 November 2018).
- Madianos, P.N.; Bobetsis, Y.A.; Offenbacher, S. Adverse pregnancy outcomes (APOs) and periodontal disease: Pathogenic mechanisms. J. Clin. Periodontol. 2013, 40 (Suppl. 14), S170–S180. [Google Scholar] [CrossRef] [PubMed]
- Chambrone, L.; Guglielmetti, M.R.; Pannuti, C.M.; Chambrone, L.A. Evidence grade associating periodontitis to preterm birth and/or low birth weight: I. A systematic review of prospective cohort studies. J. Clin. Periodontol. 2011, 38, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Ide, M.; Papapanou, P.N. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes—Systematic review. J. Periodontol. 2013, 84 (Suppl. 4), S181–S194. [Google Scholar] [CrossRef]
- Sanz, M.; Kornman, K. Working group 3 of joint EFP/AAP workshop. Periodontitis and adverse pregnancy outcomes: Consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Clin. Periodontol. 2013, 40 (Suppl. 14), S164–S169. [Google Scholar] [CrossRef]
- Haerian-Ardakani, A.; Eslami, Z.; Rashidi-Meibodi, F.; Haerian, A.; Dallalnejad, P.; Shekari, M.; Moein Taghavi, A.; Akbari, S. Relationship between maternal periodontal disease and low birth weight babies. Iran J. Reprod. Med. 2013, 11, 625–630. [Google Scholar]
- Han, Y.W.; Fardini, Y.; Chen, C.; Iacampo, K.G.; Peraino, V.A.; Shamonki, J.M.; Redline, R.W. Term stillbirth caused by oral Fusobacterium nucleatum. Obstet. Gynecol. 2010, 115 Pt 2, 442–445. [Google Scholar] [CrossRef]
- Huck, O.; Tenenbaum, H.; Davideau, J.L. Relationship between periodontal diseases and preterm birth: Recent epidemiological and biological data. J. Pregnancy 2011, 2011, 164654. [Google Scholar] [CrossRef]
- Offenbacher, S.; Boggess, K.A.; Murtha, A.P.; Jared, H.L.; Lieff, S.; McKaig, R.G.; Mauriello, S.M.; Moss, K.L.; Beck, J.D. Progressive periodontal disease and risk of very preterm delivery. Obstet. Gynecol. 2006, 107, 29–36. [Google Scholar] [CrossRef]
- Bobetsis, Y.A.; Barros, S.P.; Offenbacher, S. Exploring the relationship between periodontal disease and pregnancy complications. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef]
- López, N.J.; Smith, P.C.; Gutierrez, J. Higher risk of preterm birth and low birth weight in women with periodontal disease. J. Dent. Res. 2002, 81, 58–63. [Google Scholar] [CrossRef]
- Ovalle, A. Relación entre enfermedad periodontal, infección bacteriana ascendente y patología placentaria con parto prematuro. Rev. Med. Chile 2009, 137, 504–514. [Google Scholar] [CrossRef][Green Version]
- Corbella, S.; Taschieri, S.; Del Fabbro, M.; Francetti, L.; Weinstein, R.; Ferrazzi, E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta-analysis exploring potential association. Quintessence Int. 2016, 47, 193–204. [Google Scholar] [CrossRef]
- Cetin, I.; Pileri, P.; Villa, A.; Calabrese, S.; Ottolenghi, L.; Abati, S. Pathogenic mechanisms linking periodontal diseases with adverse pregnancy outcomes. Reprod. Sci. 2012, 19, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoat, M.K.; Geurs, N.C.; Reddy, M.S.; Cliver, S.P.; Goldenberg, R.L.; Hauth, J.C. Periodontal infection and preterm birth: Results of a prospective study. J. Am. Dent. Assoc. 2001, 132, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Santa Cruz, I.; Herrera, D.; Martin, C.; Herrero, A.; Sanz, M. Association between periodontal status and pre-term and/or low-birth weight in Spain: Clinical and microbiological parameters. J. Periodontal Res. 2013, 48, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.J.; Lo, A.J.; Pullin, D.A.; Thornton-Johnson, D.S.; Karimbux, N.Y. Scaling and root planing treatment for periodontitis to reduce preterm birth and low birth weight: A systematic review and meta-analysis of randomized controlled trials. J. Periodontol. 2012, 83, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Núñez, J.; Moya, P.; Monsalves, M.J.; Landaeta, M.S. Nivel de conocimiento en salud bucal y uso de GES odontológico en atención ambulatoria en Clínica Privada, Santiago, Chile. Int. J. Odontoestomatol. 2013, 7, 39–46. [Google Scholar] [CrossRef]
- Martignon, S.B. Instrumentos para evaluar los conocimientos, actitudes y prácticas en salud oral para padres/cuidadores de niños menores. Rev. Salud Pública 2008, 10, 308–314. [Google Scholar] [CrossRef][Green Version]
- Penmetsa, G.S.; Meghana, K.; Bhavana, P.; Venkatalakshmi, M.; Bypalli, V.; Lakshmi, B. Awareness, attitude and knowledge regarding oral health among pregnant women: A comparative study. Niger. Med. J. 2018, 59, 70–73. [Google Scholar] [CrossRef]
- Rengifo, H. Creencias acerca de la salud oral en gestantes en tres ciudades colombianas. Rev. Facult. Odont. Univ. Antioquia 2009, 20, 171–178. [Google Scholar]
- Garbero, I.; Delgado, A.; Benito de Cardenas, I. Oral health in pregnant: Knowledge and attitudes. Acta Odontol. 2005, 43, 135–140. [Google Scholar]
- Lindhe, J.L. Periodontología Clínica e Implantología Clínica, 6th ed.; Medica Panamericana: Madrid, Spain, 2017; Chapter 2; p. 75. [Google Scholar]
- Sotomayor, J.S. Nivel de conocimiento en prevención de salud bucal en gestantes que se atienden en dos hospitales nacionales peruanos. Odontol. Sanmarquina 2012, 15, 10–13. [Google Scholar] [CrossRef]
- Correa, M.E. Importancia de revisión odontológica durante el control prenatal. Rev. Odont. Colomb. 2006, 43, 135–140. [Google Scholar]
- Vozza, I.; Capasso, F.; Marrese, E.; Polimeni, A.; Ottolenghi, L. Infant and child oral health risk status correlated to behavioral habits of parents or caregivers: A survey in Central Italy. J. Int. Soc. Prev. Commun. Dent. 2017, 7, 95–99. [Google Scholar] [CrossRef]
- Castro, R.V. Nivel de Conocimiento Sobre Salud Bucal en Gestantes Que Acuden Al Centro de Obrassociales “Maternidad de María” Distrito Chimbote, Provincia Del Santa, región Ancash, Año 2016; Universidad Católica Los Ángeles de Chimbote: Chimbote, Peru, 2017. [Google Scholar]
- Yalcin, F.; Eskinazi, E.; Soydinc, M.; Basegmez, C.; Issever, H.; Isik, G.; Berber, L.; Has, R.; Sabuncu, H.; Onan, U. The effect of sociocultural status on periodontal conditions in pregnancy. J. Periodontol. 2002, 73, 178–1782. [Google Scholar] [CrossRef]
- Santana, A.M. Salud bucodental y embarazo. Rev. Acta Odontoest. 2004, 400, 57–62. [Google Scholar]
- Fuentes Fernández, R.O. Opiniones y creencias de embarazadas en control prenatal relacionadas con salud oral y embarazo. Av. Odontoestomatol. 2009, 25, 147–154. [Google Scholar] [CrossRef][Green Version]
- Keirse, M.J.; Plutzer, K. Women’s attitudes to and perceptions of oral health and dental care during pregnancy. J. Perinat. Med. 2010, 38, 3–8. [Google Scholar] [CrossRef]
- Sousa Araújo, L.C. Pregnant women’s oral health: Knowledge, practices and their relationship with periodontal disease. Rev. Gaúcha Odontol. 2016, 64, 154–163. [Google Scholar] [CrossRef][Green Version]
- García-Martin, J.M.-D.-P. Impacto de la salud oral en la calidad de vida de la gestante. Rev. Salud Públic 2017, 19, 145–152. [Google Scholar] [CrossRef]
- Vera-Delgado, M.M.-B.-L. Nivel de salud oral de la mujer embarazada de la Comunidad Autónoma de la Región de Murcia. Odontol. Preven. 2010, 2, 1–7. [Google Scholar]
- Castaldi, J.B. Enfermedad periodontal: ¿Es factor de riesgo para parto pretérmino, bajo peso al nacer o preeclampsia? Rev. Panam. Salud Pública 2006, 19, 253–258. [Google Scholar] [CrossRef]
- Enabulele, J.; Ibhawoh, L. Resident obstetricians’ awareness of the oral health component in management of nausea and vomiting in pregnancy. BMC Pregnancy Childbirth 2014, 14, 388. [Google Scholar] [CrossRef]
- Jiang, H.; Su, Y.; Xiong, X.; Harville, E.; Wu, H.; Jiang, Z.; Qian, X. Prevalence and risk factors of periodontal disease among pre-conception Chinese women. Reprod. Health 2016, 13, 141. [Google Scholar] [CrossRef]
- Rius, J.M.; Ortuño, J.; Rivas, C.; Maravall, M.; Calzado, M.A.; López, A.; Aguar, M.; Vento, M. Factores asociados al abandono precoz de la lactancia materna en una región del este de España. An. Pediatr. 2014, 80, 6–15. [Google Scholar] [CrossRef]
- Oribe, M. Prevalencia y factores asociados con la duración de la lactancia materna exclusiva durante los 6 primeros meses en la cohorte INMA de Guipúzcoa. Gac. Sanit. 2015, 29, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Santacruz Salas, E.F. Factors Associated with the abandonment of exclusive breastfeeding before three months. Children 2020, 7, 298. [Google Scholar] [CrossRef] [PubMed]
- Cuenca Sala, E.B. Odontología Preventiva y Comunitaria: Principios, Métodos y Aplicaciones; Elsevier Masson: Amsterdam, The Netherlands, 2005; Chapter 5; p. 51. [Google Scholar]
- Piédrola Gil, E. Medicina Preventiva y Salud Pública, 12th ed.; Elsevier Masson: Amsterdam, The Netherlands, 2016; Chapter 66; p. 884. [Google Scholar]
- Rioboo García, R. Odontología Preventiva y Odontología Comunitaria; Avances Médico Dentales: Madrid, Spain, 2002; Volume 1. [Google Scholar]
- Orellana, C. Incidence of Estomatológic program Educaction Program education for prevention and care in pregnant women. Rev. Dent. Chile 2010, 101, 4–7. [Google Scholar]
- Alonso Rosado, A.; Pérez Gómez, R.M.; Criado Pérez, L.; Duque Alonso, N.; Hernández Marcos, C.; Hernández Martín, M.; Lorenzo Rodríguez, V.; Martín Muñoz, F.; Otín Reixa, I. Enfermedades periodontales durante el embarazo y su asociación con parto prematuro y bajo peso al nacimiento: Evidencias y controversias. Avances en Periodoncia e Implantología Oral 2010, 22, 85–89. [Google Scholar] [CrossRef][Green Version]
| Age in Years | 32.5 ± 5.19 Years (Median: 33; Range: 18–45) |
|---|---|
| Educational level | 52 (57.1%) university studies 38 (41.8%) high school education 1 (1.1%) primary education. |
| Number of children | 1.4 ± 0.63 (Median: 1; Range: 1–3) |
| Week of delivery | 39.1 ± 1.36 week (Median: 39; Range: 33–41) |
| Newborn weight | 3221.1 ± 0.39 milligrams (Median: 3200; Range: 1930–4300) |
| Breastfeeding | F Frequency | Mean ± SD | Statistical Significance | |
|---|---|---|---|---|
| Caries Index (CAOD) score | Yes | 82 | 7.18 ± 3.615 | p > 0.05 |
| No | 15 | 6.93 ± 3.515 | ||
| Simplified Oral Hygiene Index (IHOS) score | Yes | 82 | 1.04 ± 0.739 | p > 0.05 |
| No | 15 | 1.17 ± 0.637 | ||
| Week of delivery | Yes | 82 | 39.1 ± 1.44 | p > 0.05 |
| No | 15 | 39.3 ± 0.81 | ||
| Infant’s weight (milligrams) | Yes | 82 | 3221 ± 0.41 | p > 0.05 |
| No | 15 | 3220 ± 0.34 | ||
| Number of Children | Yes | 82 | 1.5 ± 0.63 | p > 0.05 |
| No | 15 | 1.4 ± 0.63 | ||
| Mother’s age in years | Yes | 82 | 33.0 ± 4.80 | p < 0.05 |
| No | 15 | 29.6 ± 6.42 | ||
| Weeks of Pregnancy | Yes | 82 | 31.0 ± 5.35 | p > 0.05 |
| No | 15 | 30.8 ± 6.38 | ||
| Correct answers “Questionnaire for pregnant women. Oral health” | Yes | 82 | 12.8 ± 3.40 | p < 0.05 |
| No | 15 | 10.7 ± 4.02 | ||
| Incorrect answers “Questionnaire for pregnant women. Oral health” | Yes | 82 | 8.5 ± 3.33 | p > 0.05 |
| No | 15 | 10.2 ± 3.26 |
| IHOS Control | Frequency | Mean ± SD | Statistical Significance | |
|---|---|---|---|---|
| Caries index (CAOD) | Suitable | 63 | 6.95 ± 3.674 | p > 0.05 |
| Acceptable | 32 | 7.50 ± 3.538 | ||
| Deficient | 2 | 7.50 ± 0.707 | ||
| Total | 97 | 7.14 ± 3.582 | ||
| Week of delivery | Suitable | 63 | 39.2 ± 1.17 | p > 0.05 |
| Acceptable | 32 | 39.0 ± 1.72 | ||
| Deficient | 2 | 39.5 ± 0.70 | ||
| Total | 97 | 39.1 ± 1.36 | ||
| Infant’s weight (milligrams) | Suitable | 63 | 3333 ± 0.3 | p < 0.05 |
| Acceptable | 32 | 3017 ± 0.3 | ||
| Deficient | 2 | 2960 ± 0.1 | ||
| Total | 97 | 3221 ± 0.3 | ||
| Number of children | Suitable | 63 | 1.5 ± 0.6 | p > 0.05 |
| Acceptable | 32 | 1.5 ± 0.6 | ||
| Deficient | 2 | 1.0 ± 0.0 | ||
| Total | 97 | 1.4 ± 0.6 | ||
| Age | Suitable | 63 | 34.0 ± 4.28 | p < 0.05 |
| Acceptable | 32 | 29.5 ± 5.76 | ||
| Deficient | 2 | 33.0 ± 0.0 | ||
| Total | 97 | 32.5 ± 5.19 | ||
| Weeks of pregnancy | Suitable | 63 | 31.4 ± 5.24 | p > 0.05 |
| Acceptable | 32 | 30.3 ± 5.73 | ||
| Deficient | 2 | 28.0 ± 11.31 | ||
| Total | 97 | 31.0 ± 5.49 |
| Level of Education | Frequency | Mean ± SD | Statistical Significance | |
|---|---|---|---|---|
| Caries index (CAOD) | Primary | 1 | 8.00 | p > 0.05 |
| Secondary | 38 | 7.55 ± 3.562 | ||
| University | 52 | 6.73 ± 3.609 | ||
| Total | 91 | 7.09 ± 3.574 | ||
| Simplified Oral Hygiene Index (IHOS) | Primary | 1 | 1.60 | p < 0.05 |
| Secondary | 38 | 1.39 ± 0.834 | ||
| University | 52 | 0.77 ± 0.509 | ||
| Total | 91 | 1.04 ± 0.729 | ||
| Week of delivery | Primary | 1 | 40.0 | p > 0.05 |
| Secondary | 38 | 39.2 ± 1.38 | ||
| University | 52 | 39.1 ± 1.22 | ||
| Total | 91 | 39.2 ± 1.28 | ||
| Infant weight (mg) | Primary | 1 | 3290 | p > 0.05 |
| Secondary | 38 | 3205 ± 0.3 | ||
| University | 52 | 3253 ± 0.3 | ||
| Total | 91 | 3233 ± 0.3 | ||
| Number of children | Primary | 1 | 1.0 | p > 0.05 |
| Secondary | 38 | 1.5 ± 0.64 | ||
| University | 52 | 1.4 ± 0.64 | ||
| Total | 91 | 1.4 ± 0.63 | ||
| Mother’s age | Primary | 1 | 18.0 | p < 0.05 |
| Secondary | 38 | 31.1 ± 5.91 | ||
| University | 52 | 34.0 ± 3.56 | ||
| Total | 91 | 32.6 ± 5.10 | ||
| Weeks of Pregnancy | Primary | 1 | 28.0 | p > 0.05 |
| Secondary | 38 | 31.0 ± 5.85 | ||
| University | 52 | 31.2 ± 5.56 | ||
| Total | 91 | 31.1 ± 5.63 |
| Dependent Variable: Infant Weight | |||||
|---|---|---|---|---|---|
| Independent Variables | Non-Standardized B Coefficients | Standardized B Coefficients | 95% Confidence Interval | Statistical Significance | |
| Constant | −2.018 | −3.941 | −0.095 | p < 0.05 | |
| Oral Hygiene Index (IHOS) | −0.169 | −0.307 | −0.261 | −0.077 | p < 0.05 |
| Week of delivery | 0.138 | 0.474 | 0.089 | 0.187 | p < 0.05 |
| Smoking Habit | Frequency | Mean ± SD | Statistical Significance | |
|---|---|---|---|---|
| Caries index (CAOD) | Yes | 5 | 8.60 ± 4.615 | p > 0.05 |
| No | 88 | 6.93 ± 3.526 | ||
| Simplified Oral Hygiene Index (IHOS) | Yes | 5 | 1.28 ± 0.715 | p > 0.05 |
| No | 88 | 1.08 ± 0.727 | ||
| Week of delivery | Yes | 5 | 38.6 ± 2.61 | p > 0.05 |
| No | 88 | 39.2 ± 1.30 | ||
| Infant weight (mg) | Yes | 5 | 2798 ± 0.5 | p < 0.05 |
| No | 88 | 3235 ± 0.3 | ||
| Number of Children | Yes | 5 | 1.0 ± 0.0 | p > 0.05 |
| No | 88 | 1.5 ± 0.62 | ||
| Age | Yes | 5 | 30.2 ± 2.38 | p > 0.05 |
| No | 88 | 32.4 ± 5.26 | ||
| Weeks of Pregnancy | Yes | 5 | 32.4 ± 4.82 | p > 0.05 |
| No | 88 | 31.1 ± 5.41 | ||
| Correct Answers | Yes | 5 | 10.0 ± 3.39 | p > 0.05 |
| No | 88 | 12.7 ± 3.49 | ||
| Incorrect Answers | Yes | 5 | 10.8 ± 1.92 | p > 0.05 |
| No | 88 | 8.6 ± 3.41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serrano-Sánchez, S.; González-González, J.; Rodríguez-Martín, B.; Muñoz-Rodríguez, V.; de las Heras-Corrochano, S.; Criado-Alvarez, J.J. Relationship between Oral Health Knowledge and Maternal Oral Health with Obstetric Risk and Breastfeeding. Int. J. Environ. Res. Public Health 2022, 19, 7797. https://doi.org/10.3390/ijerph19137797
Serrano-Sánchez S, González-González J, Rodríguez-Martín B, Muñoz-Rodríguez V, de las Heras-Corrochano S, Criado-Alvarez JJ. Relationship between Oral Health Knowledge and Maternal Oral Health with Obstetric Risk and Breastfeeding. International Journal of Environmental Research and Public Health. 2022; 19(13):7797. https://doi.org/10.3390/ijerph19137797
Chicago/Turabian StyleSerrano-Sánchez, Silvia, Jaime González-González, Beatriz Rodríguez-Martín, Vanesa Muñoz-Rodríguez, Sonia de las Heras-Corrochano, and Juan José Criado-Alvarez. 2022. "Relationship between Oral Health Knowledge and Maternal Oral Health with Obstetric Risk and Breastfeeding" International Journal of Environmental Research and Public Health 19, no. 13: 7797. https://doi.org/10.3390/ijerph19137797
APA StyleSerrano-Sánchez, S., González-González, J., Rodríguez-Martín, B., Muñoz-Rodríguez, V., de las Heras-Corrochano, S., & Criado-Alvarez, J. J. (2022). Relationship between Oral Health Knowledge and Maternal Oral Health with Obstetric Risk and Breastfeeding. International Journal of Environmental Research and Public Health, 19(13), 7797. https://doi.org/10.3390/ijerph19137797








