Prediction of Mortality in Older Hospitalized Patients after Discharge as Determined by Comprehensive Geriatric Assessment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Setting
2.3. Comprehensive Geriatric Assessment Evaluation
2.4. Outcome
2.5. Statistical Analysis
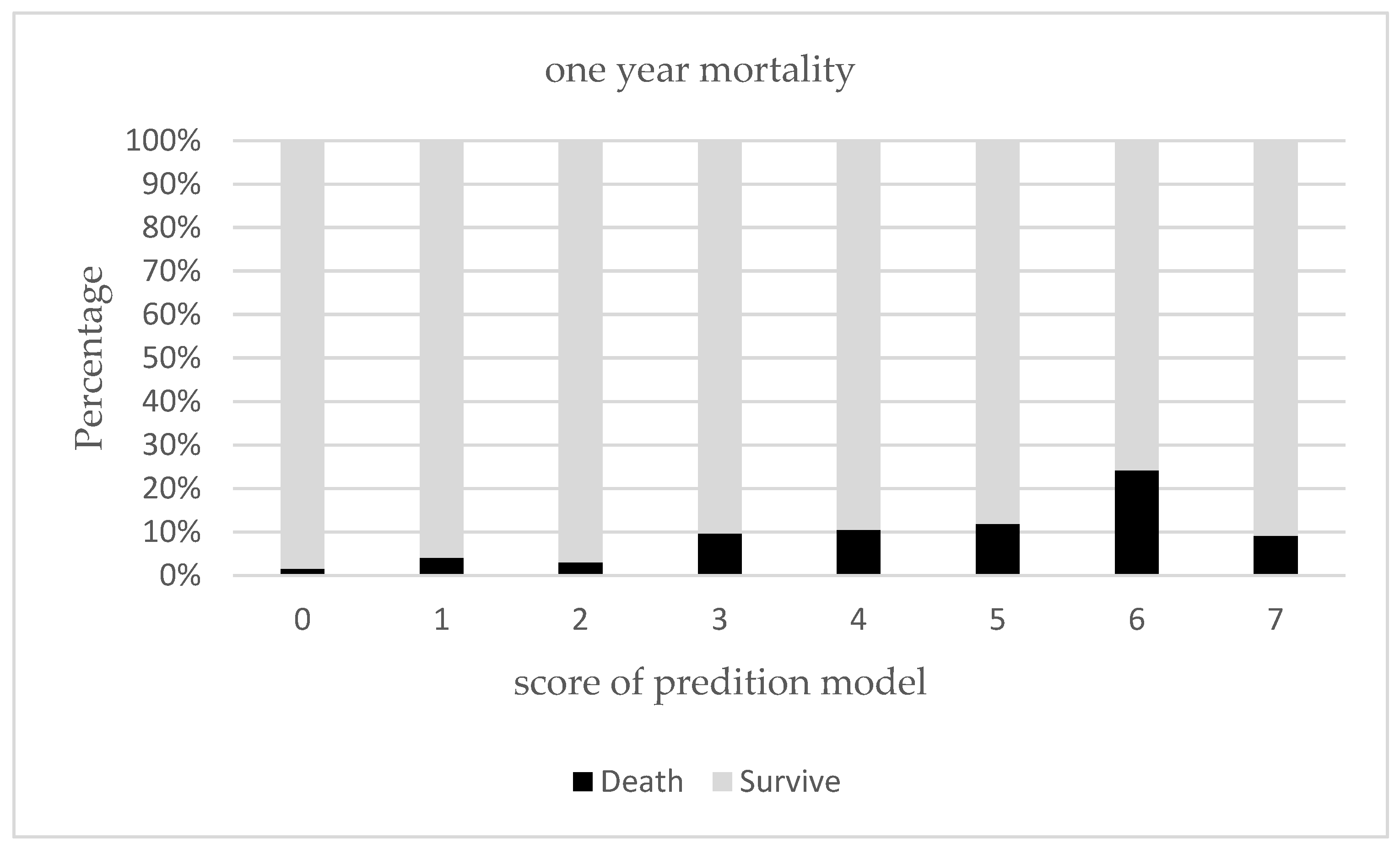
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsuji, M.; Miyahara, S.; Taoka, F.; Teshima, M. An estimation of economic effects of tele-home-care: Hospital cost-savings of the elderly. Stud. Health Technol. Inform. 2001, 84, 858–862. [Google Scholar] [PubMed]
- Lin, Y.Y.; Huang, C.S. Aging in Taiwan: Building a Society for Active Aging and Aging in Place. Gerontologist 2016, 56, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Directorate General of Budget, Executive Yuan: Statistical Review of National Conditions 2022. Available online: https://www.dgbas.gov.tw/public/Data/2328175851DBU1BWDH.pdf (accessed on 28 March 2022).
- Sartelli, M.; Abu-Zidan, F.M.; Labricciosa, F.M.; Kluger, Y.; Coccolini, F.; Ansaloni, L.; Leppäniemi, A.; Kirkpatrick, A.W.; Tolonen, M.; Tranà, C.; et al. Physiological parameters for Prognosis in Abdominal Sepsis (PIPAS) Study: A WSES observational study. World. J. Emerg. Surg. 2019, 14, 34. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, M.; Buurman, B.M.; MacNeil-Vroomen, J.L.; Suijker, J.J.; ter Riet, G.; Moll van Charante, E.P.; de Rooij, S.E. Changes in the in-hospital mortality and 30-day post-discharge mortality in acutely admitted older patients: Retrospective observational study. Age Ageing 2016, 45, 41–47. [Google Scholar] [CrossRef]
- Campbell, S.E.; Seymour, D.G.; Primrose, W.R. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing 2004, 33, 110–115. [Google Scholar] [CrossRef]
- Zanetti, M.; Marzaro, G.; De Colle, P.; Toigo, G.; Bianchini, D.; Nastri, M.; Suriano, C.; Barazzoni, R.; Sanson, G. Predictors of short- and long-term mortality among acutely admitted older patients: Role of inflammation and frailty. Aging Clin. Exp. Res. 2021, 34, 409–418. [Google Scholar] [CrossRef]
- Sullivan, D.H.; Roberson, P.K.; Bopp, M.M. Hypoalbuminemia 3 months after hospital discharge: Significance for long-term survival. J. Am. Geriatr. Soc. 2005, 53, 1222–1226. [Google Scholar] [CrossRef]
- Wang, M.C.; Li, T.C.; Li, C.I.; Liu, C.S.; Lin, W.Y.; Lin, C.H.; Yang, C.W.; Yang, S.Y.; Lin, C.C. Frailty, transition in frailty status and all-cause mortality in older adults of a Taichung community-based population. BMC Geriatr. 2019, 19, 26. [Google Scholar] [CrossRef]
- Jeffery, A.D.; Dietrich, M.S.; Maxwell, C.A. Predicting 1-year disability and mortality of injured older adults. Arch. Gerontol. Geriatr. 2018, 75, 191–196. [Google Scholar] [CrossRef]
- Stuck, A.E.; Siu, A.L.; Wieland, G.D.; Adams, J.; Rubenstein, L.Z. Comprehensive geriatric assessment: A meta-analysis of controlled trials. Lancet 1993, 342, 1032–1036. [Google Scholar] [CrossRef]
- Ellis, G.; Whitehead, M.A.; O’Neill, D.; Langhorne, P.; Robinson, D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst. Rev. 2011, 7, Cd006211. [Google Scholar] [CrossRef]
- Ellis, G.; Gardner, M.; Tsiachristas, A.; Langhorne, P.; Burke, O.; Harwood, R.H.; Conroy, S.P.; Kircher, T.; Somme, D.; Saltvedt, I.; et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst. Rev. 2017, 9, Cd006211. [Google Scholar] [CrossRef] [PubMed]
- Ponzetto, M.; Maero, B.; Maina, P.; Rosato, R.; Ciccone, G.; Merletti, F.; Rubenstein, L.Z.; Fabris, F. Risk factors for early and late mortality in hospitalized older patients: The continuing importance of functional status. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Rankin, A.; Cadogan, C.A.; Patterson, S.M.; Kerse, N.; Cardwell, C.R.; Bradley, M.C.; Ryan, C.; Hughes, C. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst. Rev. 2018, 9, Cd008165. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B.; Garry, P.J. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr. Rev. 1996, 54, S59–S65. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Biggerstaff, B.J. Comparing diagnostic tests: A simple graphic using likelihood ratios. Stat. Med. 2000, 19, 649–663. [Google Scholar] [CrossRef]
- Ghanem, M.; Garthmann, J.; Redecker, A.; Ahrberg-Spiegl, A.B.; Fakler, J.K.M.; Spiegl, U.J.A. Management of pertrochanteric fractures in patients over 90 years: In-hospital mortality rate, complications and associated risk factors. BMC Musculoskelet. Disord. 2021, 22, 799. [Google Scholar] [CrossRef]
- Tomita, Y.; Yamamoto, N.; Inoue, T.; Ichinose, A.; Noda, T.; Kawasaki, K.; Ozaki, T. Preoperative and perioperative factors are related to the early postoperative Barthel Index score in patients with trochanteric fracture. Int. J. Rehabil. Res. 2022, 45, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Guzzo, T.J.; Dluzniewski, P.; Orosco, R.; Platz, E.A.; Partin, A.W.; Han, M. Prediction of mortality after radical prostatectomy by Charlson comorbidity index. Urology 2010, 76, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Shen, S.; Xu, L.; Wang, Y.; Yang, Y.; Chen, L.; Guan, H.; Zhang, J.; Chen, X. The Impact of Intrinsic Capacity on Adverse Outcomes in Older Hospitalized Patients: A One-Year Follow-up Study. Gerontology 2021, 67, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Zekry, D.; Herrmann, F.R.; Vischer, U.M. The association between the body mass index and 4-year all-cause mortality in older hospitalized patients. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Alarcón, T.; Bárcena, A.; González-Montalvo, J.I.; Penãlosa, C.; Salgado, A. Factors predictive of outcome on admission to an acute geriatric ward. Age Ageing 1999, 28, 429–432. [Google Scholar] [CrossRef][Green Version]
- Ryg, J.; Engberg, H.; Anru, P.L.; Pedersen, S.G.H.; Jorgensen, M.G.; Vinding, K.L.; Masud, T.; Andersen-Ranberg, K. Activities of daily living at hospital admission and estimated survival time of older patients. Age Ageing 2021, 50, 1200–1207. [Google Scholar] [CrossRef]
- Tseng, C.L.; Hsu, N.C.; Hsieh, P.I.; Lin, Y.F.; Chen, C.Y.; Wu, C.Y.; Sheng, W.H. Integrated approach for multimorbid patients in a hospitalist setting: Survival analysis of a two-year prospective study. J. Formos. Med. Assoc. 2022, 121, 473–481. [Google Scholar] [CrossRef]
- Lesende, I.M.; Crespo, L.I.M.; Bilbao, I.C.; Rodríguez, J.P.; Manzanares, S.C.; Otter, A.S.D.; Pérez, I.N.; Azcoaga, I.S.; de la Rua Fernández, M.J. Functional decline, mortality and institutionalization after 18 months in multimorbid older persons living in the community: The FUNCIPLUR longitudinal study. Eur. Geriatr. Med. 2019, 10, 523–528. [Google Scholar] [CrossRef]
- Atramont, A.; Lindecker-Cournil, V.; Rudant, J.; Tajahmady, A.; Drewniak, N.; Fouard, A.; Singer, M.; Leone, M.; Legrand, M. Association of Age with Short-term and Long-term Mortality among Patients Discharged from Intensive Care Units in France. JAMA Netw. Open 2019, 2, e193215. [Google Scholar] [CrossRef]
- García-Sanz, M.T.; Cánive-Gómez, J.C.; Senín-Rial, L.; Aboal-Viñas, J.; Barreiro-García, A.; López-Val, E.; González-Barcala, F.J. One-year and long-term mortality in patients hospitalized for chronic obstructive pulmonary disease. J. Thorac. Dis. 2017, 9, 636–645. [Google Scholar] [CrossRef]
- Surme, S.; Balkan, I.I.; Bayramlar, O.F.; Kara Ali, R.; Mete, B.; Tabak, F.; Saltoğlu, N. Predictors of Long-term Outcomes in the Older Adults with Community-Acquired Pneumonia. J. Infect. Dev. Ctries 2021, 15, 1910–1916. [Google Scholar] [CrossRef] [PubMed]
- Bae, H.J.; Yoon, D.S.; Lee, J.; Kim, B.K.; Koo, J.S.; Kwon, O.; Park, J.M. In-hospital medical complications and long-term mortality after ischemic stroke. Stroke 2005, 36, 2441–2445. [Google Scholar] [CrossRef] [PubMed]
- Bellanti, F.; Lo Buglio, A.; Quiete, S.; Vendemiale, G. Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management. Nutrients 2022, 14, 910. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.L.; Ong, K.C.; Chan, Y.H.; Loke, W.C.; Ferguson, M.; Daniels, L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin. Nutr. 2012, 31, 345–350. [Google Scholar] [CrossRef]
- Kyle, U.G.; Kossovsky, M.P.; Karsegard, V.L.; Pichard, C. Comparison of tools for nutritional assessment and screening at hospital admission: A population study. Clin. Nutr. 2006, 25, 409–417. [Google Scholar] [CrossRef]
- Raslan, M.; Gonzalez, M.C.; Dias, M.C.; Nascimento, M.; Castro, M.; Marques, P.; Segatto, S.; Torrinhas, R.S.; Cecconello, I.; Waitzberg, D.L. Comparison of nutritional risk screening tools for predicting clinical outcomes in hospitalized patients. Nutrition 2010, 26, 721–726. [Google Scholar] [CrossRef]
- Bally, M.R.; Blaser Yildirim, P.Z.; Bounoure, L.; Gloy, V.L.; Mueller, B.; Briel, M.; Schuetz, P. Nutritional Support and Outcomes in Malnourished Medical Inpatients: A Systematic Review and Meta-analysis. JAMA Int. Med. 2016, 176, 43–53. [Google Scholar] [CrossRef]
- Hsu, A.T.; Manuel, D.G.; Spruin, S.; Bennett, C.; Taljaard, M.; Beach, S.; Sequeira, Y.; Talarico, R.; Chalifoux, M.; Kobewka, D.; et al. Predicting death in home care users: Derivation and validation of the Risk Evaluation for Support: Predictions for Elder-Life in the Community Tool (RESPECT). CMAJ 2021, 193, e997–e1005. [Google Scholar] [CrossRef]
- Campitelli, M.A.; Bronskill, S.E.; Hogan, D.B.; Diong, C.; Amuah, J.E.; Gill, S.; Seitz, D.; Thavorn, K.; Wodchis, W.P.; Maxwell, C.J. The prevalence and health consequences of frailty in a population-based older home care cohort: A comparison of different measures. BMC Geriatr. 2016, 16, 133. [Google Scholar] [CrossRef]
- Wen, Y.C.; Chen, L.K.; Hsiao, F.Y. Predicting mortality and hospitalization of older adults by the multimorbidity frailty index. PLoS ONE 2017, 12, e0187825. [Google Scholar] [CrossRef]
| Total Patients (N = 1565) | Alive Patients (n = 1455) | Deceased Patients (n = 110) | p Value e | ||||
|---|---|---|---|---|---|---|---|
| Age (years) | 81 | (74.0–86.0) | 81 | (74.0–86.0) | 83 | (76–87) | 0.075 |
| Gender, Male (%) | 966 | (61.7%) | 896 | (61.6%) | 70 | (63.6%) | 0.669 |
| Length of stay (Days) | 9.0 | (6–14) | 9 | (6–14) | 12 | (7–17) | 0.042 |
| Falls in one year (%) | 639 | (40.8%) | 589 | (40.5%) | 50 | (45.5%) | 0.306 |
| Polypharmacy (%) | 1012 | (64.7%) | 930 | (63.9%) | 82 | (74.5%) | 0.025 |
| BI at baseline a | 90 | (60–100) | 90 | (60–100) | 80 | (45–95) | 0.001 |
| BI at admission a | 55 | (20–80) | 55 | (20–80) | 45 | (10–70) | 0.004 |
| IADL at baseline b | 4 | (1–6) | 4 | (1–6) | 2.5 | (0–5) | <0.001 |
| IADL at admission b | 2 | (0–4) | 2 | (0–4) | 1 | (0–3) | 0.004 |
| MNA c | 21.5 | (17.5–24.5) | 22 | (17.5–25.0) | 18.7 | (15–22) | <0.001 |
| CCI d | 2 | (1.0–3.0) | 2 | (1.0–3.0) | 3 | (2.0–4.0) | <0.001 |
| Number of admissions | 0 | (0–0) | 0 | (0–0) | 0 | (0–1.0) | <0.001 |
| Mortality | 110 | (7.0%) | -- | -- | -- | -- | -- |
| Simple Cox Regression Analysis (Original Data) | Simple Cox Regression Analysis (Dichotomized *) | Multiple Cox Regression Model | RISK SCORE | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | p value | HR | 95% CI | p value | Adjusted HR | 95% CI | p value | -- |
| Age | 1.022 | 0.998–1.047 | 0.066 | 1.840 | 1.133–2.986 | 0.014 ** | 1.750 | 1.074–2.853 | 0.025 ** | 1 |
| Gender (male vs. female) | 0.917 | 0.622–1.352 | 0.662 | 0.917 | 0.622–1.352 | 0.662 | -- | -- | -- | -- |
| Length of stay (days) | 1.018 | 1.003–1.032 | 0.016 ** | 1.802 | 1.240–2.619 | 0.002 ** | 1.551 | 1.058–2.275 | 0.024 ** | 1 |
| Polypharmacy | 1.644 | 1.070–2.525 | 0.023 ** | 1.644 | 1.070–2.525 | 0.023 ** | -- | -- | -- | -- |
| BI at baseline | 0.993 | 0.988–0.999 | 0.016 ** | 0.925 | 0.519–1.651 | 0.793 | -- | -- | -- | -- |
| BI at admission | 0.992 | 0.986–0.998 | 0.005 ** | 0.785 | 0.524–1.176 | 0.241 | -- | -- | -- | -- |
| IADL at baseline | 0.887 | 0.829–0.949 | <0.001 ** | 0.616 | 0.408–0.930 | 0.021 ** | -- | -- | -- | -- |
| IADL at admission | 0.882 | 0.811–0.960 | 0.003 ** | 0.657 | 0.448–0.964 | 0.032 ** | -- | -- | -- | -- |
| MNA | 0.913 | 0.881–0.945 | <0.001 ** | 2.141 | 1.449–3.165 | 0.001 ** | 1.508 | 1.002–2.269 | 0.049 ** | 1 |
| CCI | 1.319 | 1.190–1.461 | <0.001 ** | 2.540 | 1.450–4.451 | 0.001 ** | 2.173 | 1.234–3.825 | 0.007 ** | 2 |
| Previous admission history | 1.642 | 1.419–1.899 | <0.001 ** | 2.850 | 1.951–4.162 | <0.001 ** | 2.418 | 1.644–3.557 | <0.001 ** | 2 |
| Cutoff Value | Sensitivity | Specificity | Youden Index | AUC | CI |
|---|---|---|---|---|---|
| Model for 1-year mortality | -- | -- | -- | 0.691 | 0.642–0.740 |
| ≥1 | 0.973 | 0.129 | 0.102 | -- | -- |
| ≥2 | 0.927 | 0.208 | 0.135 | -- | -- |
| ≥3 | 0.791 | 0.535 | 0.326 * | -- | -- |
| ≥4 | 0.509 | 0.736 | 0.245 | -- | -- |
| ≥5 | 0.273 | 0.889 | 0.162 | -- | -- |
| ≥6 | 0.145 | 0.961 | 0.106 | -- | -- |
| ≥7 | 0.009 | 0.993 | 0.002 | -- | -- |
| Model for 30 days mortality | -- | -- | -- | 0.801 | 0.711–0.891 |
| ≥1 | 1.000 | 0.123 | 0.123 | ||
| ≥2 | 1.000 | 0.201 | 0.201 | -- | -- |
| ≥3 | 0.938 | 0.517 | 0.455 * | -- | -- |
| ≥4 | 0.688 | 0.723 | 0.411 | -- | -- |
| ≥5 | 0.500 | 0.882 | 0.382 | -- | -- |
| ≥6 | 0.250 | 0.955 | 0.205 | -- | -- |
| ≥7 | 0.000 | 0.993 | −0.007 | -- | -- |
| Model for 90 days mortality | -- | -- | -- | 0.748 | 0.681–0.814 |
| ≥1 | 1.000 | 0.125 | 0.125 | -- | -- |
| ≥2 | 0.956 | 0.204 | 0.160 | -- | -- |
| ≥3 | 0.867 | 0.524 | 0.391 * | -- | -- |
| ≥4 | 0.622 | 0.729 | 0.351 | -- | -- |
| ≥5 | 0.378 | 0.886 | 0.264 | -- | -- |
| ≥6 | 0.178 | 0.957 | 0.135 | -- | -- |
| ≥7 | 0.000 | 0.993 | −0.007 | -- | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, C.-H.; Lin, S.-Y.; Lee, C.-L.; Lin, C.-S.; Hsu, P.-S.; Lee, Y.-S. Prediction of Mortality in Older Hospitalized Patients after Discharge as Determined by Comprehensive Geriatric Assessment. Int. J. Environ. Res. Public Health 2022, 19, 7768. https://doi.org/10.3390/ijerph19137768
Su C-H, Lin S-Y, Lee C-L, Lin C-S, Hsu P-S, Lee Y-S. Prediction of Mortality in Older Hospitalized Patients after Discharge as Determined by Comprehensive Geriatric Assessment. International Journal of Environmental Research and Public Health. 2022; 19(13):7768. https://doi.org/10.3390/ijerph19137768
Chicago/Turabian StyleSu, Chih-Hsuan, Shih-Yi Lin, Chia-Lin Lee, Chu-Sheng Lin, Pi-Shan Hsu, and Yu-Shan Lee. 2022. "Prediction of Mortality in Older Hospitalized Patients after Discharge as Determined by Comprehensive Geriatric Assessment" International Journal of Environmental Research and Public Health 19, no. 13: 7768. https://doi.org/10.3390/ijerph19137768
APA StyleSu, C.-H., Lin, S.-Y., Lee, C.-L., Lin, C.-S., Hsu, P.-S., & Lee, Y.-S. (2022). Prediction of Mortality in Older Hospitalized Patients after Discharge as Determined by Comprehensive Geriatric Assessment. International Journal of Environmental Research and Public Health, 19(13), 7768. https://doi.org/10.3390/ijerph19137768






