From Strain toward Hyperdoppler Echocardiographic Evaluation in Sports Medicine
1. Introduction
2. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oxborough, D.; Augustine, D.; Gati, S.; George, K.; Harkness, A.; Mathew, T.; Papadakis, M.; Ring, L.; Robinson, S.; Sandoval, J.; et al. A guideline update for the practice of echocardiography in the cardiac screening of sports participants: A joint policy statement from the British Society of Echocardiography and Cardiac Risk in the Young. Echo Res. Pract. 2018, 5, G1–G10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orlandi, G.; Corsi, M.; Casatori, L.; Stefani, L. Frequency of fragmented QRS in sports activity: A pilot study. J. Sports Med. Phys. Fit. 2022. [Google Scholar] [CrossRef] [PubMed]
- Ollitrault, P.; Pellissier, A.; Champ-Rigot, L.; Junqua, N.; Chequel, M.; Reboursiere, E.; Saloux, É.; Milliez, P.; Hodzic, A. Prevalence and significance of fragmented QRS complex in lead V1 on the surface electrocardiogram of healthy athletes. Europace 2020, 22, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Terho, H.K.; Tikkanen, J.T.; Junttila, J.M.; Anttonen, O.; Kenttä, T.V.; Aro, A.; Kerola, T.; Rissanen, H.A.; Reunanen, A.; Huikuri, H.V. Prevalence and prognostic significance of fragmented QRS complex in middle-aged subjects with and without clinical or electrocardiographic evidence of cardiac disease. Am. J. Cardiol. 2014, 114, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Dandle, M.; Lehmkuhl, H.; Knosalla, C.; Suramelashvili, N.; Hetzer, R. Strain and Strain Rate Imaging by Echocardiography—Basic Concepts and Clinical Applicability. Curr. Cardiol. Rev. 2009, 5, 133–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galanti, G.; Pedrizzetti, G.; Pedri, S.; Stefani, L. 2D longitudinal LV speckle tracking strain pattern in breast cancer survivors: Sports activity vs exercise as prescription model. Intern. Emerg. Med. 2017, 12, 1149–1157. [Google Scholar] [CrossRef] [PubMed]
- Minetti, E.; Klika, R.; Ingletto, C.; Mascherini, G.; Pedrizzetti, G.; Stefani, L. Changes in global longitudinal strain in renal transplant recipients following 12 months of exercise. Intern. Emerg. Med. 2018, 13, 805–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voigt, G.U.; Pedrizzetti, G.; Lysyansky, P.; Tom HMarwick, T.M.; Houle, H.; Baumann, R.; Pedri, S.; Ito, Y.; Abe, Y.; Metz, S.; et al. Definitions for a common standard for 2D speckle tracking echocardiography: Consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, D.R.; Markl, M.; Mur, J.L.M.; Barker, A.; Fernández-Golfín, C.; Lancellotti, P.; Gómez, J.L.Z. Intracardiac flow visualization: Current status and future directions. Eur. Heart J.—Cardiovasc. Imaging 2013, 14, 1029–1038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mele, D.; Smarrazzo, V.; Pedrizzetti, G.; Capasso, F.; Pepe, M.; Severino, S.; Luisi, G.A.; Maglione, M.; Ferrari, R. Intracardiac FlowAnalysis: Techniques and Potential Clinical Applications. J. Am. Soc. Echocardiogr. 2019, 32, 319–332. [Google Scholar] [CrossRef] [PubMed]
- Pedrizzetti, G.; Domenichini, F. Nature optimizes the swirling flow in the human left ventricle. Phys. Rev. Lett. 2005, 95, 108101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef] [Green Version]
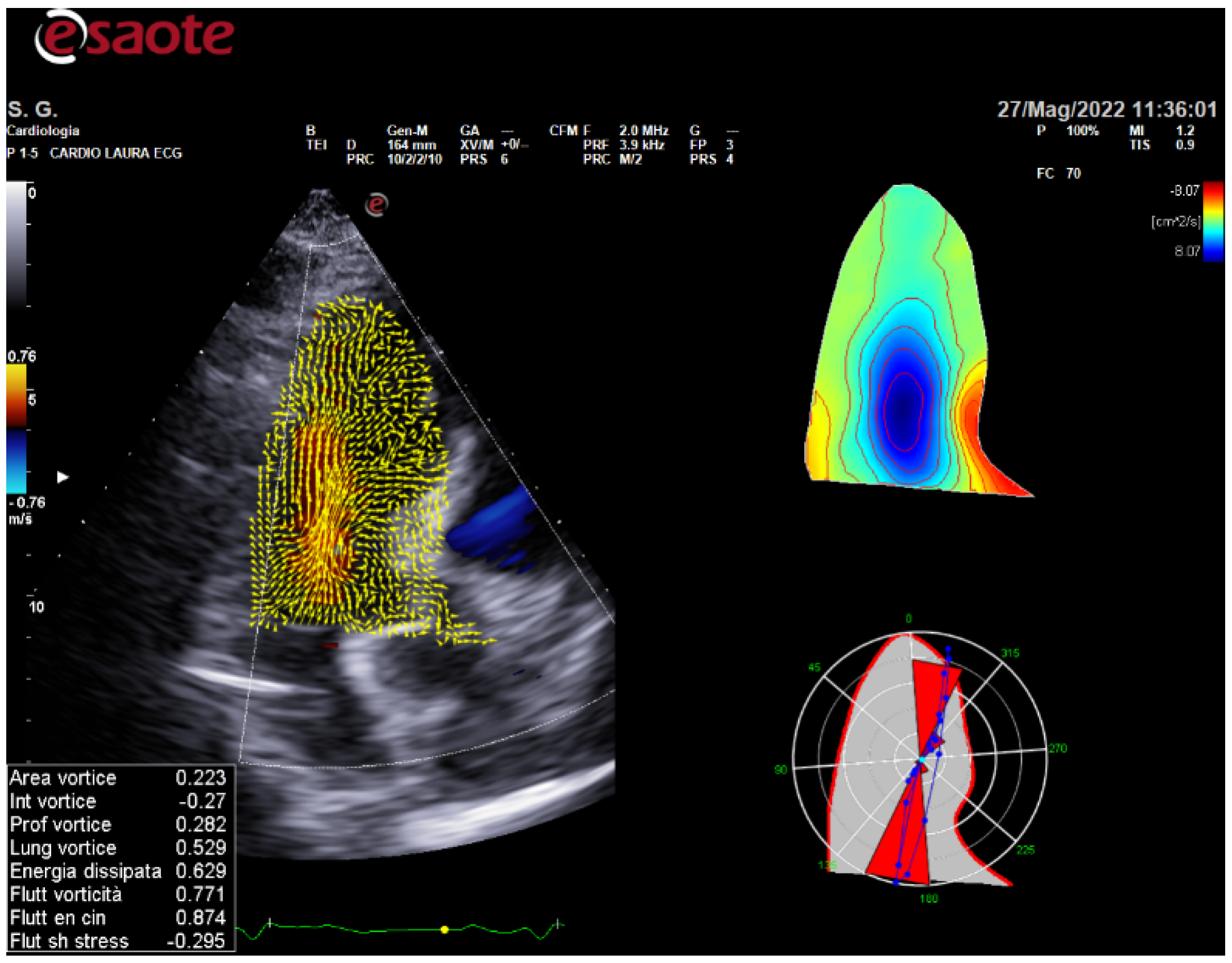
- Fiorencis, A.; Pepe, M.; Smarrazzo, V.; Martini, M.; Severino, S.; Pergola, V.; Evangelista, M.; Incarnato, P.; Previtero, M.; Maglione, M.; et al. Non-invasive Evaluation of Intraventricular Flow Dynamics by the HyperDoppler Technique: First Application to Normal Subjects, Athletes, and Patients with Heart Failure. J. Clin. Med. 2022, 11, 2216. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefani, L. From Strain toward Hyperdoppler Echocardiographic Evaluation in Sports Medicine. Int. J. Environ. Res. Public Health 2022, 19, 7702. https://doi.org/10.3390/ijerph19137702
Stefani L. From Strain toward Hyperdoppler Echocardiographic Evaluation in Sports Medicine. International Journal of Environmental Research and Public Health. 2022; 19(13):7702. https://doi.org/10.3390/ijerph19137702
Chicago/Turabian StyleStefani, Laura. 2022. "From Strain toward Hyperdoppler Echocardiographic Evaluation in Sports Medicine" International Journal of Environmental Research and Public Health 19, no. 13: 7702. https://doi.org/10.3390/ijerph19137702
APA StyleStefani, L. (2022). From Strain toward Hyperdoppler Echocardiographic Evaluation in Sports Medicine. International Journal of Environmental Research and Public Health, 19(13), 7702. https://doi.org/10.3390/ijerph19137702




