1. Introduction
Improving population health and reducing health inequalities are goals of every society, regardless of its current health status level. To ensure a solid basis for making the right decisions to achieve better population health, it should be measured and monitored constantly, using valid, well-constructed indicators. Monitoring health status helps allocate healthcare resources in an adequate way and assess the results of public health activities. Health indicators of population health are used for making comparisons between countries and benchmarking, as well as assessing changes over time within countries [
1].
Comparative health analyses were conducted as long ago as the 17th century, in the area of hospital mortality. In the 1990s, the comparison has been structured as a method of different aspects of healthcare analyses [
2,
3]. Comparisons carried out at different levels and in settings (e.g., regional, international, between hospitals, etc.) make it possible to identify disparities, analyze the reasons for them, and find the best practices possible to improve various aspects of healthcare quality. International comparisons of population health using health-related indicators (including summary measures) make an important contribution to the evaluation of health system performance and enable policymakers to learn from others, helping to direct policy in the right direction [
4,
5,
6]. International comparisons help identify high performers and provide policymakers with a benchmark in order to identify areas that are functioning below expectations [
7,
8].
Any time comparison results or ranking lists are published, especially if they are international and related to health or healthcare, it causes a huge wave of comments and even protests. The comparison results are broadly covered in the media, as issues related to health always attract widespread attention [
4]. Prime examples include the global debate that started after the WHO had announced its health-system performance assessment in 2000, and the comments that have appeared in the media each time the Health Consumer Powerhouse publishes a new Euro Health Consumer Index report [
7,
9,
10].
The rankings of population health, or those in which population health is one of the components, often use values for the total population, not presenting information for any subgroups (for example, the Bloomberg Global Health Index [
11], the OECD Better Life Index [
12], and the Global Health Security Index Ranking [
13]). Meanwhile, older people constitute a growing and more significant group in many populations. In the last 20 years (from 2001 to 2021), the size of the population 65 and above in European Union (EU) countries has increased by over 37% and the share of this population in the total EU population has risen from 15.8% to 20.8% [
14]. People who are older contribute in many ways to societies, and the expectations for the social participation of older groups are increasing, but these opportunities are highly dependent on older people’s health [
15,
16]. In most EU countries the group of people from 15 to 64 years old (that is, of the defined working age) is shrinking: in 16 countries, the size of this group declined between 2001 and 2021, even by nearly 25% in Latvia [
14]. As a result, the older population group is more and more important in the formal and informal labor force [
16]. To plan and implement appropriate actions to ensure healthy and active aging, it is necessary to identify and assess older people’s health status and functioning [
15]. Measuring, monitoring, and understanding the older population’s health is crucial to ensure the best possible functional ability and to build a sufficient long-term care system [
17]. The question arises of whether a comparison analysis using total population health indicators is sufficient in the presented context.
The research question of the study was whether drawing conclusions about older population health based on the health status of the total population is justified in international comparison analyses. To answer this question, international comparisons between European countries were taken into account. A review of population health status indicators available in international databases was also conducted and the construction of these indicators was checked in the context of the older-age population group.
2. Materials and Methods
A review of the five biggest international open-access databases was conducted (Eurostat [
14], WHO Global Health Observatory (WHO GHO) [
18], Global Health Data Exchange (GHDx) [
19], OECD Data [
20], World Bank Open Data [
21]) to identify population health status indicators and gather available values. These databases contain a wide range of health-data collections and declare a statistics comparability, which is one of the essential features in international analyses. The necessity of data comparability was the main reason for relying on international databases, and not on national sources. As a sample for the study, 27 European Union countries + the United Kingdom, Norway, Switzerland and Iceland were chosen. The main rationale for this choice was data availability in the Eurostat database, which is the only one that contains some indicators for assessing population health that are not available elsewhere.
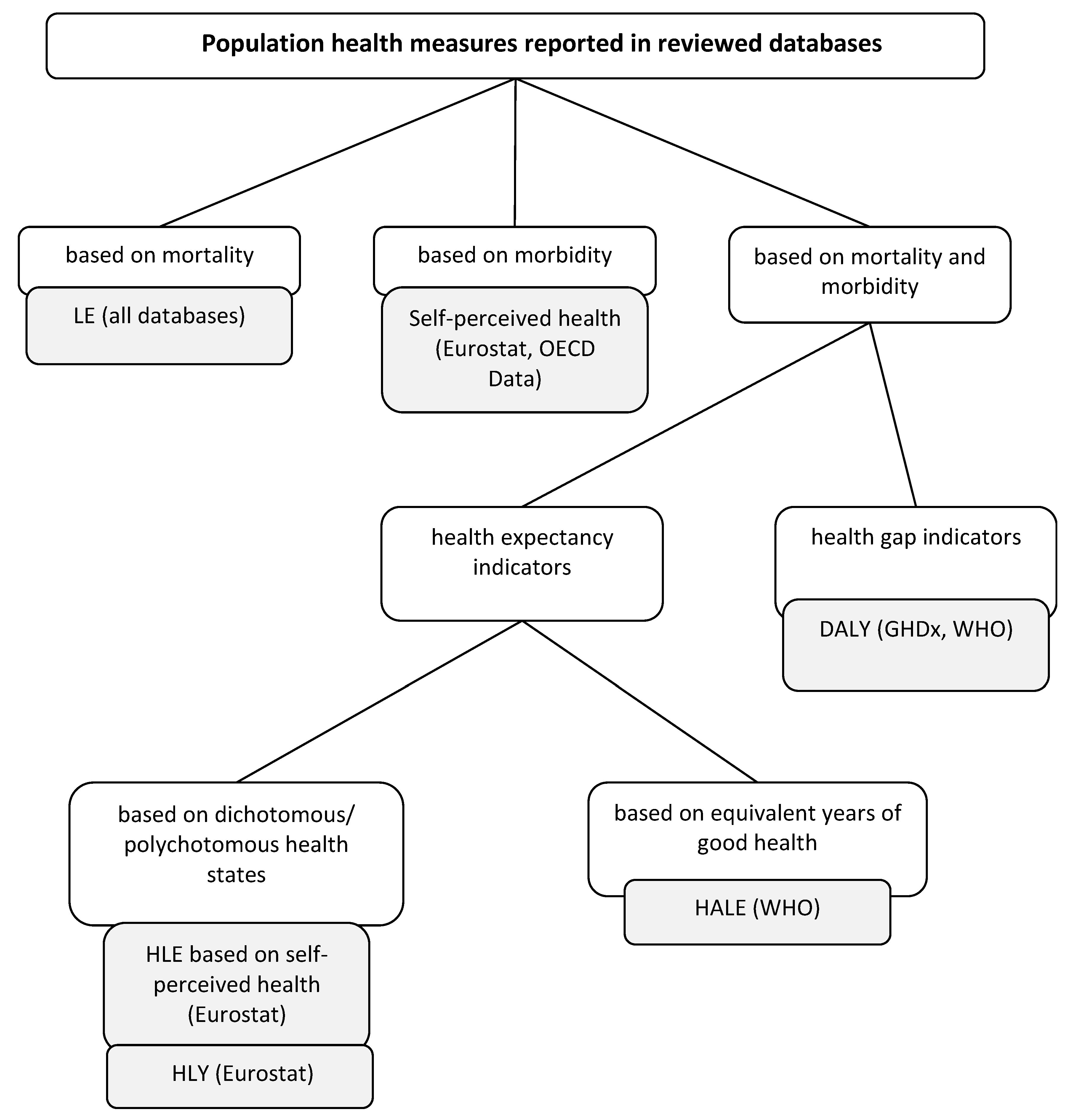
Finally, six indicators were chosen for the analysis: life expectancy (LE), self-perceived health (SPH), healthy life expectancy based on self-perceived health (HLE), healthy life years (HLY), healthy life expectancy (HALE), and disability-adjusted life years (DALY) (
Table 1). The analysis covers the period of 2010–2019, except for the HALE indicator, for which the analysis was carried out for the years 2010, 2015 and 2019 due to the lack of data availability.
For all selected indicators and for each year from 2010–2019, the rankings were created for both the total population and the older subpopulation, and then ranks for these two populations were compared. A higher indicator value means a higher ranking position, excluding DALY, for which a lower value means a higher position (as DALY indicates a burden of diseases). When indicator values are equal, their ranks are the same and equal to the arithmetic mean of their “potential” positions.
The statistical analysis contains the descriptive statistics and then more advanced statistical analyses. Because rankings are an example of ordinal-type data, nonparametric statistical tests were used for the analysis. The sign test and the Wilcoxon signed-rank test were applied to compare the distributions of ranks for the total population and the older subpopulation. The strength of the relationship was assessed using Spearman’s and Kendall’s rank correlation coefficients (the detailed description of methods used in the analysis can be found in the
Supplementary Materials S1). While the sign test is based on the number of signs of differences, the Wilcoxon test takes into account the magnitude of differences in pairs by considering the absolute rank values of these differences. Therefore, the Wilcoxon test is considered more powerful than the sign test.
For all indicators, linear regression models of the dependence of the ranks for the older subpopulation on the ranks for the total population for 2010–2019 were also estimated. The resulting regression coefficient indicates how much the rank of the older subpopulation will increase on average if the rank of the whole population increases by one position. In turn, the coefficient of determination indicates what proportion of the variation in ranks for the older subpopulation is predictable from the ranks for the total population, and the root-mean-square error (RMSE) shows the mean deviation between the observed values and the values predicted by a model. The statistical analyses were performed in STATA.
4. Discussion
The aim of the research was to evaluate whether drawing conclusions about older population health based on the health status of the total population is justified in international comparison analyses. To do this, rankings of countries in terms of the health status of the total and the older population were compared. The analysis was conducted for 31 European countries, and six indicators were used to evaluate population health for the period of 2010–2019.
The statistical analysis did not reject the null hypothesis of equality of the distributions of the total population and the older subpopulation for any of the analyzed indicators (this does not mean that this distributions’ equality has been proven, but we cannot state that it does not exist). The tests also indicate that there is a strong, statistically significant relationship between ranks for the total and the older population. However, looking at the descriptive analysis and visual presentation of data, differences in international rankings of indicator values can be noted. The ranking position of the total population rarely differs from that of the older population by more than 10 items, but sometimes this difference can reach even 15 positions. Thus, in individual cases, the difference is considerable and may affect the conclusions of the ranking analysis. The highest rank differences can be observed for the HLY indicator, and in each year of the analysis period, the SD of rank differences for HLY is higher than 4.7. This value is also exceeded for half of the analyzed years for the SPH indicator, but it occurs very rarely for the remaining ones (only three years for DALY). This suggests that the answer to the research question may depend to some extent on the kind of indicator used, and the analyzing rankings for both total and older populations may be more important for some indicators than for others. The regression analysis also indicates that conclusions drawn from the rankings for the total and the older population may differ more for HLY than, for example, for HLE and HALE; as for the HLY rank variability, for the older group it is explained by the rank variability for the total population only in 66% of cases, while for the last two it is 93%.
International comparisons can be a good measure for identifying potential improvements, but a deep understanding of the reasons for differences between a given country and the best performer is needed [
8]. Due to ranking differences, even when not statistically significant, another country (or countries) can be indicated as examples of “best practices,” looking at total population health and at the older population ranking. As a result, health policy decisions regarding older population health may be based on policies of a country with even worse health outcomes. Looking at health population assessments only through the prism of the entire population may lead to conclusions that do not fully take into account the needs of subpopulations, including older people. For example, in 2019 the HLY indicator ranking for the total population of Cyprus was 10 places higher than Denmark, but in the ranking for the older population, it was 14 places lower. This suggests that analysis regarding the reasons for these differences should be conducted separately for the total and the older populations.
The population health indicator rankings are presented not only as a single comparison, but often constitute one of the components of summary indices in complex assessment frameworks. They may regard not only health-system performance or healthcare-quality evaluation, but also assessments of a wider scope, such as, for example, the Sustainable Development Goals Index, which includes, i.a., life expectancy at birth [
41]. In this index a health indicator for the total population was used, just like in many other cases (Bloomberg Global Health Index [
11], OECD Better Life Index [
12], Global Health Security Index Ranking [
13], and the World Health Report index [
9]), but a good example of the deliberate use of an indicator for the older instead the total population is the Health Care System Performance Rankings published by the Commonwealth Fund. The authors indicate that they are assessing health-system performance, so measures should reflect outcomes that can be modified by health care, while life expectancy at birth may be affected more by socioeconomic conditions than by health-system activities [
42].
Health indicators applicable to all age groups are not easy to construct. Measures evaluating activity limitations may be good for examining the older population’s health status, but may not be good or sensitive enough for the total population [
43]. Measures based on self-perceived health are not used for children, and, for example, in the case of HLY and HLE, the health status of the youngest population is estimated based on the answers of the first interviewed age group, which can impact assessment reliability (assumed to be half of the prevalence for the group 16–19) [
44]. There is also a problem in using these measures for people who, due to their health state, cannot consciously fill questionnaires in (mostly in the older age groups). In HALE construction, disability weights are applied that reflect the severity of a given disease/injury outcome. However, using the same disability weights for every age group may be questionable, as health is perceived differently at different ages. The acceptable level of a health state usually becomes lower with age, so assessment of the burden caused by health problems may be very age-dependent. A health problem greatly lowering a young person’s quality of life can be seen as not so important by an older person. However, an opposite difference is also possible—older people can start to see good health as more important and pay more attention to health [
45,
46,
47,
48,
49]. This may indicate that slightly different methods should be used to measure the health of the older population, or at least that the indicators should be computed partially, paying attention to different age groups [
15,
43]. Meanwhile, there is still a lack of scientific consensus on the key indicators for creating proper health policy and public health interventions for older people [
50].
Population health indicators are often used in international comparisons, sometimes in combination with other kind of measures, to analyze relationships between health and various factors. Some good examples are studies on the relation between GDP and health (e.g., [
51,
52]). Preparing such analyses, especially when their results may have an impact on policy decisions regarding not only the total but also the older population specifically, it is worth checking whether conclusions would be similar if not the total but rather the older population health were taken into account. This would ensure that the decision was being made on a reliable basis.
Regardless of the choice of health indicator, the value for the older population affects more or less the value for the total population. Looking at indicator construction, it may be supposed that this impact is quite strong, but only a detailed analysis could show how significant this impact is depending on the indicator. This kind of analysis would be worth conducting in the future.
This study has been prepared for a small group of countries, all of them situated in Europe. These are countries of a relatively similar level of population health, which may be considered a limitation of the research. A similar analysis should be conducted for other, non-European countries to check the results. Due to data-availability issues, in the case of two indicators, the older population is defined as something other than 65 and over: 60 for HALE and 70 for DALY. This inconsistency can also be seen as a limitation. Additionally, HALE indicator data are only available in the analyzed period for three years.
The results of this research indicate that there are no statistically significant differences between total and older population health assessment in international comparisons. Regardless, despite the lack of statistical confirmation, some differences in EU country rankings may be observed, and they can in some cases affect the conclusions drawn from benchmarking analyses. Every ranking, especially international ones, arouses great interest and emotions. Additionally, taking into account differences in health perception, assessment, expectations and needs in older and younger age groups, it seems justified to recommend presenting the results of population health comparisons not only for the total population, but for the older population as well, at least if it is used as the basis for planning specific health policy and interventions aimed at older people. Data regarding the older population’s health are still insufficient, not systematically collected, analyzed or interpreted [
50].